Treatment Of Parkinsons Disease/is There A Cure For Parkinsons Disease
Although there is no cure for Parkinson’s disease, medicines, surgical treatment, and other therapies can often relieve some symptoms.
Medicines for Parkinson’s Disease
Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapy—such as nausea, vomiting, low blood pressure, and restlessness—and reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinson’s symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements-
- Anticholinergic drugs to reduce tremors and muscle rigidity
Quarter Of Parkinsons Sufferers Were Wrongly Diagnosed Says Charity
Poll of more than 2,000 people found 26% of respondents were told they had something else
More than a quarter of people with Parkinson’s disease were initially misdiagnosed, new research has found.
The poll of more than 2,000 people found 26% were first told they had something else, while 21% saw their GP three or more times before being referred to a specialist.
Of those who were misdiagnosed, 48% were given treatment for their nonexistent condition, with 36% receiving medication, 6% undergoing operations or procedures and a further 6% given both medication and operations or procedures.
Of those who received unnecessary treatment, 34% said their health had got worse as a result.
The poll, for the charity Parkinson’s UK, also found that women were more likely to be misdiagnosed than men, and errors were most common in people aged 51 to 60.
Katie Goates of Parkinson’s UK said: “Parkinson’s is an incredibly complex condition with more than 40 symptoms, and it affects everyone differently.
“One of the biggest challenges for Parkinson’s research is that there is no definitive test for Parkinson’s, and as a result we’ve heard of people being misdiagnosed with anything from a frozen shoulder or anxiety to a stroke.
“Our survey has shown that because of this, people are being left in limbo and seeing their health deteriorate, which is unacceptable.
About 145,000 people in the UK are diagnosed with Parkinson’s every year.
Signs of Parkinson’s can include:
Results
What Does It Mean?
Difficulties In Diagnosing Depression In Patients With Parkinson’s
- Certain symptoms of depression overlap with symptoms of PD ? for example, sleep problems and feeling slowed down occur in both conditions.
- Some experts think that depression in PD often involves frequent, shorter changes in mood versus a constant state of sadness daily.
- Many people with PD express less emotion due to the effect the disease has on the muscles of the face. This symptom, called facial masking, makes a person unable to express emotion through facial expressions.
- Many people with Parkinson’s do not seek treatment because they often do not recognize they have a mood problem or are unable to explain symptoms. For these reasons, it is helpful to ask a caregiver or loved one if he or she has noticed any changes commonly reported in depression.
Blood Test May Distinguish Parkinsons From Multiple System Atrophy
A highly sensitive and specific blood test has been developed that can distinguish Parkinson’s disease from multiple system atrophy , a team at the University of California, Los Angeles Health reported.
The test examines the levels of a protein called alpha-synuclein in exosomes — tiny vesicles released by cells that end up in the blood. In Parkinson’s, alpha-synuclein comes from neuron-derived exosomes, while in MSA it comes from exosomes released by oligodendrocytes, another type of brain cell.
Based on the content and origin of the exosomes, this test can help discriminate between Parkinson’s disease and MSA.
“This is a major breakthrough, because it allows us to analyze what’s going on in the brain using a blood test,” Gal Bitan, PhD, the study’s senior author and a professor of neurology at the David Geffen School of Medicine at UCLA, said in a university press release.
The study, “?-Synuclein in blood exosomes immunoprecipitated using neuronal and oligodendroglial markers distinguishes Parkinson’s disease from multiple system atrophy,” was published in Acta Neuropathologica.
Parkinson’s and neurodegenerative diseases such as MSA have several symptoms in common, including muscle rigidity and tremors. Because of this overlap in symptoms, many cases are misdiagnosed.
Incorrect diagnoses can also affect clinical trial results, as potential treatments would be tested in people without the disorder under evaluation.
Results
What Does It Mean?
References
What Is The Prognosis And Life Expectancy For Parkinson’s Disease

The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
Simple Blood Tests For Parkinsons Disease Derived From Genome
The diagnosis of Parkinson’s disease relies on expert opinion. Autopsy studies, however, have demonstrated that even experienced neurologists misdiagnose Parkinson’s disease in about a quarter out of a hundred cases. Diagnostic accuracy at disease onset, when neuroprotective treatment is anticipated to be most effective, is even lower. Thus, there is a crucial need for biomarkers that are disease-specific and which precisely identify early disease stages.
Traditional studies of blood from Parkinson’s disease patients have analyzed expression levels of one gene or gene product at a time. We plan to take advantage of ‘gene chip’ technology allowing expression analysis of up to 22,000 genes on a single glass slide, known as microarray. We hypothesize that a comparison of the gene chip analyses of blood samples from Parkinson’s disease patients and normal controls or patients with other neurological diseases will identify a set of signature genes with characteristic expression in patients with Parkinson’s disease. These key genes will provide a ‘molecular fingerprint’ of Parkinson’s disease in blood.
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
Helping diagnose Parkinson’s with DaTscan and other tests
Why Genetic Testing For Parkinsons Disease Is Complex:
In addition to the above, it is important to realize that not all genes associated with PD contribute to disease in the same way:
Blood Test Aims To Detect Parkinson’s In Early Stages
Explore further
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Global Problem: Lack Of Diagnosis Negates Treatment Impact
Search
Methodological Limitations Of The Diagnostic Studies
Poll Finds 1 In 4 People With Parkinson Disease Misdiagnosed
In a poll of people with Parkinson disease, more than 1 in 4 participants reported having been misdiagnosed, with a further 21% having to see their general provider 3 times before being referred to a specialist.
In a poll of people with Parkinson disease , more than 1 in 4 participants reported having been misdiagnosed, with a further 21% having to see their general provider 3 times before being referred to a specialist, according to a report published by The Guardian.
The poll, for the charity Parkinson’s UK, included more than 2000 patients with PD . Results showed that among participants who were misdiagnosed, 48% were given treatment for their nonexistent condition, with 36% receiving medication, 6% undergoing operations or procedures, and 6% given both medication and operations/procedures. A decline in health was reported in 34% of those misdiagnosed, and women were shown to be more likely to be misdiagnosed than men.
Katie Goates, MSc, BSc, professional communications and engagement program manager at Parkinson’s UK, highlighted the difficulty in diagnosing PD, which is a complex condition of more than 40 symptoms, as one of the chief reasons behind the poll’s findings. “One of the biggest challenges for Parkinson’s research is that there is no definitive test for Parkinson’s, and as a result we’ve heard of people being misdiagnosed with anything from a frozen shoulder or anxiety to a stroke,” said Goates.
Characteristics Of Atypical Msa: Parkinsons Disease Mimics

Case illustration
A 67-year-old female : presented with a 1-year history of worsening dexterity of her left hand. Examination revealed an asymmetrical tremor of the hand at rest with cogwheel rigidity and bradykinesia. Her symptoms and signs improved with levodopa therapy . Over the next 3 years, she developed motor fluctuations, generalized peak-dose dyskinesia, worsening dysarthria, urinary frequency and constipation. She also reported intermittent mild non-threatening visual hallucinations. Orofacial dystonia and urinary incontinence then became more intrusive. She died aged 75. The final clinical diagnosis was Parkinson’s disease. Autopsy confirmed the pathological diagnosis of MSA . There were frequent depositions of neuritic plaques but no neurofibrillary tangles were found in the brain. Key clinical features of all Parkinson’s disease mimics are provided in Supplementary Table 2.
Atypical MSA versus typical MSA or Parkinson’s disease
Red flag features in atypical MSA versus typical MSA or Parkinson’s disease
| Pathological diagnosis . |
|---|
Open in new tab Open in new tabOpen in new tab
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Read more about Parkinson’s tremors
Rigidity
Bradykinesia
mask-like expression of the face
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Conditions That Mimic Shuffling Gait Seen In Parkinsons:
Please read the article on shuffling gait. It describes 5 causes of shuffling of gait.
The most crucial mimic to remember is Normal Pressure Hydrocephalus .
The person with NPH feels like he is stuck to the ground. This is a “magnetic gait”. It is easy to mistake this for Parkinson’s disease.
For example, see this video posted by the Hydrocephalus Association of America on youtube:
NPH can be treated by implanting a small shunt pipe. This shunt drains excess water around the brain into the abdomen.
What Are The Symptoms Of Atypical Parkinsonian Disorders
Like classic Parkinson’s disease, atypical Parkinsonian disorders cause muscle stiffness, tremor, and problems with walking/balance and fine motor coordination.
Patients with atypical Parkinsonism often have some degree of difficulty speaking or swallowing, and drooling can be a problem. Psychiatric disturbances such as agitation, anxiety or depression may also be part of the clinical picture.
Dementia with Lewy bodies can cause changes in attention or alertness over hours or days, often with long periods of sleep during the day. Visual hallucinations — typically of small animals or children, or moving shadows in the periphery of the visual field — are common in DLB. DLB is second only to Alzheimer’s disease as a cause of dementia in the elderly, and it most commonly affects patients in their 60s.
Patients with progressive supranuclear palsy may have difficulties with eye movements, particularly when looking downward, and with balance — when descending stairs, for instance. Backward falls are common and may occur during the early course of the disease. PSP is not usually associated with tremor, unlike Parkinson’s disease.
Parkinson’s Disease and Movement Disorders Center
What Are The Early Warning Signs Of Parkinsons Disease
Parkinson’s disease typically causes a one-sided tremor, most obvious when at rest rather than engaged in an active task. The slowness of movement and muscle stiffness are also typical. The symptoms are often initially quite subtle and emerge slowly over a period of months. It is not unusual in my experience for someone with early-stage PD to have seen a rheumatology specialist for something like a “frozen shoulder” that is actually related to the muscle stiffness caused by PD.The typical clinical signs of PD that a neurologist will look for are slowness of repetitive movements , difficulty in initiation of movement , and a progressive reduction in the speed and amplitude of sequential movements , with muscular rigidity and a slow “pill-rolling” resting tremor.An early sign can be a reduced arm swing on walking, reduced facial expressiveness, a quietening of the voice and smaller handwriting. So-called “non-motor” signs can precede the problems with movement by months or even years and include depression, anxiety, constipation and a particular sleep disorder called “REM sleep behaviour disorder,” whereby an individual may “act out” dreams or start talking in their sleep.
Conditions That Can Cause Tremors Besides Parkinsons:
The tremor of Parkinson’s disease occurs even at rest. Hence it is called a rest tremor. Very few other conditions produce rest tremor.
But, many other diseases produce a tremor which is seen only when moving, for example when writing. This is called an Action tremor or posturokinetic tremor. Even these diseases are sometimes misdiagnosed as Parkinson’s disease.
| Causes of Rest Tremor |
|---|
|
2. Excessive stress, coffee or smoking 3. Medications such as bronchodilators, valproate and lamotrigine 4. Chromosomal problems such as Fragile-X syndrome 5. Parkinson’s disease itself! And many others… |
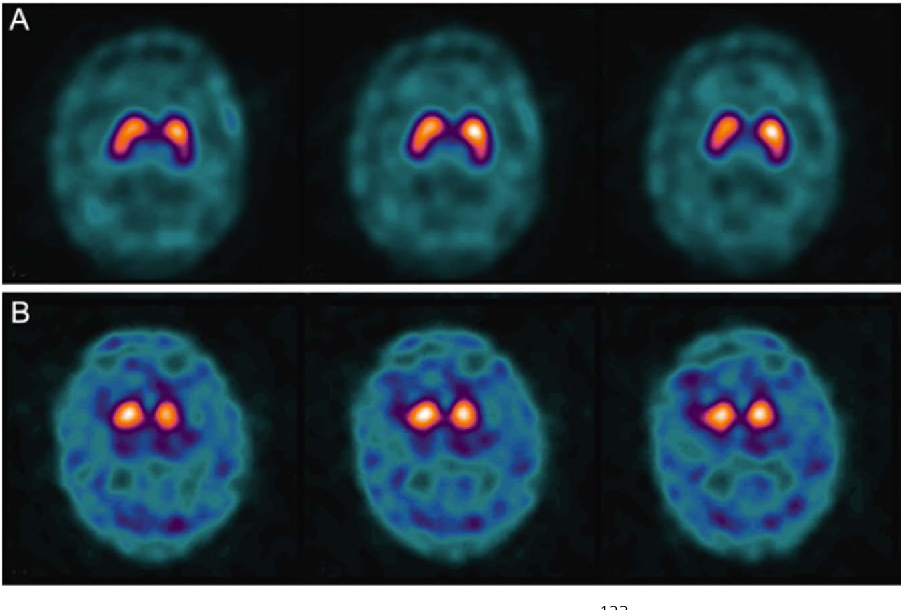
Which Test Can Be Done When The Diagnosis Is In Doubt
I request a small set of tests on almost all patients I diagnose with Parkinson’s. These detect some mimics of Parkinson’s disease.
Some doctors don’t request all these tests. And for a good reason.
The diagnosis of Parkinson’s mimics is primarily based on a careful history and examination. Even in my practice, these tests change the diagnosis only in a minority of patients.
I like the additional confirmation provided by these tests. They also have other benefits. For example, they help me determine the proper dosages of medications like Amantadine.
| Simple tests to detect Parkinson’s Mimics |
|---|
| 1. MRI-Brain – with size measurements of brain parts called the midbrain and pons. I usually also request a unique picture called SWI, which shows iron inside the brain.
2. Blood tests: |
But when the diagnosis s really in doubt, there is another brain scan that can be done.
A Trodat scan. Or even better – an F-DOPA scan. Both these scans measure dopamine activity inside the brain.
You can read more about Trodat & F-DOPA scans by clicking here.
These scans are not perfect. Let me tell you why very quickly:
In Parkinson’s disease, dopamine activity inside the brain is deficient. This deficiency produces an abnormal scan. If the Trodat/F-DOPA scan is normal, it is unlikely that you have Parkinson’s disease.
Drugs And Medication Used To Treat Parkinsons Disease
A number of different drugs can be used to treat Parkinson’s.
Levodopa
Levodopa is the most common treatment for Parkinson’s. It helps to replenish dopamine.
About 75 percent of cases respond to levodopa, but not all symptoms are improved. Levodopa is generally given with carbidopa.
Carbidopa delays the breakdown of levodopa which in turn increases the availability of levodopa at the blood-brain barrier.
Dopamine agonists
Dopamine agonists can imitate the action of dopamine in the brain. They’re less effective than levodopa, but they can be useful as bridge medications when levodopa is less effective.
Drugs in this class include bromocriptine, pramipexole, and ropinirole.
Anticholinergics
Anticholinergics are used to block the parasympathetic nervous system. They can help with rigidity.
Benztropine and trihexyphenidyl are anticholinergics used to treat Parkinson’s.
Amantadine
Amantadine can be used along with carbidopa-levodopa. It’s a glutamate-blocking drug . It offers short-term relief for the involuntary movements that can be a side effect of levodopa.
COMT inhibitors
Catechol O-methyltransferase inhibitors prolong the effect of levodopa. Entacapone and tolcapone are examples of COMT inhibitors.
Tolcapone can cause liver damage. It’s usually saved for people who do not respond to other therapies.
Ectacapone does not cause liver damage.
Stalevo is a drug that combines ectacapone and carbidopa-levodopa in one pill.
MAO-B inhibitors
Whats The Outlook For People With Parkinsons Plus
Although there currently isn’t a treatment to halt the progression of Parkinson’s plus syndrome, there are treatments that can help you manage your symptoms and improve your quality of life.
The exact outlook for Parkinson’s plus syndrome depends on the person and the specific condition they have. Someone who is otherwise healthy when they’re diagnosed will typically have a longer life expectancy than someone who is already facing other health conditions when they’re diagnosed. Your doctor will monitor your condition over time and can let you know how it’s progressing.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
Diagnosis Of Parkinson Disease: Motor Symptoms
Katarzyna Kaczy?ska, Kryspin Andrzejewski, inGenetics, Neurology, Behavior, and Diet in Parkinson’s Disease, 2020
How Do You Know You Have Parkinsons Disease
What Are Signs And Symptoms Of Parkinsons Disease
Early diagnosis can greatly increase the effectiveness of Parkinson’s treatment. However, Parkinson’s symptoms are easy to dismiss as normal signs of aging or other conditions such as stroke or head trauma. For these reasons, people may ignore symptoms or doctors may have a harder time with diagnosis.
Who Should Consider A Genetic Test For Parkinsons
There are two groups of people who might consider getting genetic testing and we will discuss each group separately.
Genetic testing for PD is a common request and a number of commercial labs perform panels of genetic testing for PD. You may ask: “How can I test myself for Parksinon’s?” Whether you’re considering getting a genetic test through your doctor, or performing one at home, it’s important to note that at-home test don’t map the entire gene for mutations. Genetic testing through your doctor will test for GBA, PARK7, SNCA, LRRK2, parkin and PINK1.
Both groups are faced with two questions: Should I get genetic testing? And if so, what should I do with the results? Before we address these two questions, we need to learn more about the complexity of genetic testing in PD.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
Once the patient is at the doctor’s office, the physician:
Is It Parkinson’s Disease Blood Test Might Tell
Conditions Misdiagnosed As Parkinson’s Disease
Parkinsons disease, especially in its early stages when symptoms are mild, is not an easy disease to diagnose. The non-specific, and easily overlooked nature of the signs of Parkinsons make it difficult to spot, and unlike many illnesses, there is no one laboratory test or radiological exam that will provide a definitive diagnosis of Parkinsons disease.
Patients exhibiting Parkinsons-like symptoms may undergo blood and urine tests, or CT or MRI scans to exclude other conditions, but none of these will provide a diagnosis of Parkinsons disease. The best way to test for Parkinsons disease is to conduct a systemic neurological examination that includes tests to gauge a patients reflexes, muscle strength, coordination, balance, gait, and overall movement. Even so, according to information presented on The Michael J. Fox Foundation for Parkinsons Research, up to 25 percent of Parkinsons disease diagnoses are incorrect.
So, why is there confusion about diagnosing Parkinsons disease? The simple answer is that symptoms of Parkinsons disease are not clear cut, and therefore, it is easy to mistake them for other conditions, or to classify them as parkinsonian when they are not.
Here is a brief overview of the top ten conditions mistaken for Parkinsons disease:
Beyond those top three, there are other conditions that are often confused with Parkinsons disease, including:
What Are The Five Stages Of Parkinsons Disease

Neurologists use a number of scales and criteria to describe stages of PD. In my experience whilst these have clear utility in the context of observational research studies as well as prospective trials of treatment, on an individual basis they are not especially useful in day to day clinical practice. The key is to understand what the main symptoms affecting a person’s quality of life are and to adjust treatment to try to improve those symptoms.If you are worried that either you or your loved one is showing early signs of Parkinson’s disease, do not hesitate to book an appointment with Dr Paviour now for an assessment.
Review Guide To Diseases Similar To Parkinsons
Some movement disorders have PD symptoms
Parkinson’s disease is not related to other well-known neurological conditions such as multiple sclerosis, muscular dystrophy, or Lou Gehrig’s disease . However, there is a variety of syndromes and diseases that look like PD but have other clinical features and pathology. The American Parkinson Disease Asso ciation in Staten Island, NY, describes 14 such diseases, as follows:
• Benign essential tremor: Essen tial tremor is commonly mistaken for PD, but the tremor quality is different. It is primarily at its worst during action, less severe during posture-holding, and rare at rest. The hands are affected, and there may be a tremor of the head and neck, usually a head nod. Also, the voice has a tremulous quality, which is not seen in PD. The legs are rarely affected, and there is no slowness, stiffness, or other features of PD. Some patients with presumed essential tremor eventually may develop PD.
• Multiple systems atrophy: This term refers to three main disorders, called olivopontocerebellar atrophy , Shy-Drager syndrome , and striatonigral degeneration . All of these may be characterized by parkinsonism, although rest tremor is slight or absent. Again, the course is more rapid than PD, and treatment is usually not productive. Distinguishing features are:
What Diseases Can Be Mistaken For Parkinson’s
This is the list of different diseases that may be mistaken with Parkinson’s disease:
- Progressive supranuclear palsy.
Alzheimer’s disease and primary lateral sclerosis can also be mistaken for Parkinson’s disease. Other similar conditions include essential tremor, dystonic tremor, vascular Parkinsonism, and drug-induced Parkinsonism.
One may also ask, what are the four cardinal signs of Parkinson’s disease? Cardinal symptoms. Four symptoms are considered cardinal in PD: bradykinesia, tremor, rigidity, and postural instability also referred to as parkinsonism. Tremor is the most apparent and well-known symptom.
Moreover, what is similar to Parkinsons?
Progressive Supranuclear Palsy: An Atypical Parkinsonian Syndrome. Progressive supranuclear palsy is not Parkinson’s disease , but is a Parkinsonian-like syndrome. PSP is a rare brain disorder that causes serious and progressive problems with gait and balance, as well as eye movement and thinking problems.
Does stress cause Parkinson’s disease?
Research suggests that stressful life events may increase the risk of Parkinson’s disease. In addition, animal studies indicate that stress damages dopamine cells, resulting in more severe parkinsonian symptoms. In humans, acute stress can worsen motor symptoms, including bradykinesia, freezing, and tremor.
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
What Are The Treatment Options For Depression
Just as the symptoms and causes of depression can differ from person to person, so too can suitable treatment approaches. There are two main types of treatment options for depression: antidepressant medications and psychological counseling .
The Parkinson’s Foundation recommends a holistic, comprehensive approach to depression. Although antidepressants are often effective in reducing symptoms, they should seldom be used alone. In most cases, the best approach is a combination of antidepressant medication, counseling, exercise and social support.
How can you ease depression in PD? First, share your concerns with your doctor. Many movement disorders specialists now include questions about depression in their exams. If your doctor does not, raise the topic. He or she may recommend medical or nonmedical coping strategies, including the following:
What Are The Different Forms Of Parkinsonism
There are three main forms of parkinsonism, as well as other related conditions.
Most people with parkinsonism have idiopathic Parkinson’s disease, also known as Parkinson’s. Idiopathic means the cause is unknown.
The most common symptoms of idiopathic Parkinson’s are tremor, rigidity and slowness of movement.
Vascular parkinsonism affects people with restricted blood supply to the brain. Sometimes people who have had a mild stroke may develop this form of parkinsonism.
Common symptoms include problems with memory, sleep, mood and movement.
Some drugs can cause parkinsonism.
Neuroleptic drugs , which block the action of the chemical dopamine in the brain, are thought to be the biggest cause of drug-induced parkinsonism.
The symptoms of drug-induced parkinsonism tend to stay the same – only in rare cases do they progress in the way that Parkinson’s symptoms do.
Drug-induced parkinsonism only affects a small number of people, and most will recover within months – and often within days or weeks – of stopping the drug that’s causing it.
Cause Of Loss Of Smell In Parkinsons Disease
It’s unclear why olfactory dysfunction occurs in Parkinson’s disease. Experts have found that smell loss correlates with a lower number of cholinergic neurons in the nucleus basalis of Meynart—a region of the brain that projects to the primary olfactory cortex where you get the sensation of smell.
With this information, smell tests that focus on detecting cholinergic dysfunction may be ideal. It’s still too early to tell, though, so more investigation needs to be done.
Additionally, some researchers have suggested that Parkinson’s disease may actually begin in the digestive system and the olfactory bulb , and not the substantia nigra . This may be why early symptoms, like constipation and loss of smell, begin years prior to motor symptoms like resting tremor and muscle stiffness.
Blood Test For Parkinson’s: Study Details
When brain cells die, Nagele says, they explode ”like a water balloon breaking.”
The contents of those dying cells spill partially back into the blood. “Their debris is released and your body will sense it and develop autoantibodies to clear that debris,” he says.
The new test looks for these autoantibodies in the blood specific to the disease. The researchers narrowed down a list of more than 100 of these autoantibodies to 10 that looked most promising. When these antibodies rise to a certain level, it signals disease, Nagele says.
To evaluate the Parkinson’s test, Nagele’s team looked at more than 150 blood samples, including:
