Constipation Linked To Increased Risk Of Developing Parkinsons Disease
The American Academy of Neurology is the world’s largest association of neurologists and neuroscience professionals, with 36,000 members. The AAN is dedicated to promoting the highest quality patient-centered neurologic care. A neurologist is a doctor with specialized training in diagnosing, treating and managing disorders of the brain and nervous system such as Alzheimer’s disease, stroke, migraine, multiple sclerosis, concussion, Parkinson’s disease and epilepsy.
Did You Know Parkinson’s Disease Could Be A Reason For Constipation
Constipation is usually a result of irregular food habits, sedentary lifestyle and everything that counts to be unhealthy. Most of the time a little change in your lifestyle habits and improving physical activity can help you get over the symptoms of the condition. However, there are times when the cause might not be just this. There could be an underlying medical condition that can lead to constipation. However, this happens mostly to the elderly population. Here Dr Jayshri Shah Consultant-Hepatologist, Gastroenterologist and Therapeutic Endoscopist at Jaslok Hospital & Research Centre tell us about the medical conditions which could lead to constipation.
1. Hypothyroidism: Of the many symptoms an underactive thyroid gives rise to, constipation is one of them. Hypothyroidism slows down many physiological conditions of the body and it could also do the same to the digestive track making it difficult for an individual to pass stool. Read to know what happens if you miss a thyroid dose.
2. Polypharmacy: Having more than four medications for various ailments is a very common scenario in elderly. But this could have an influence on the stool pattern and lead to constipation. The common medications that can give rise to constipation are antidepressants, painkillers, certain vitamin , blood pressure and allergy medications, etc. Sometimes even some antacids could give you the same problem. Know what happens when you keep popping antacids regularly.
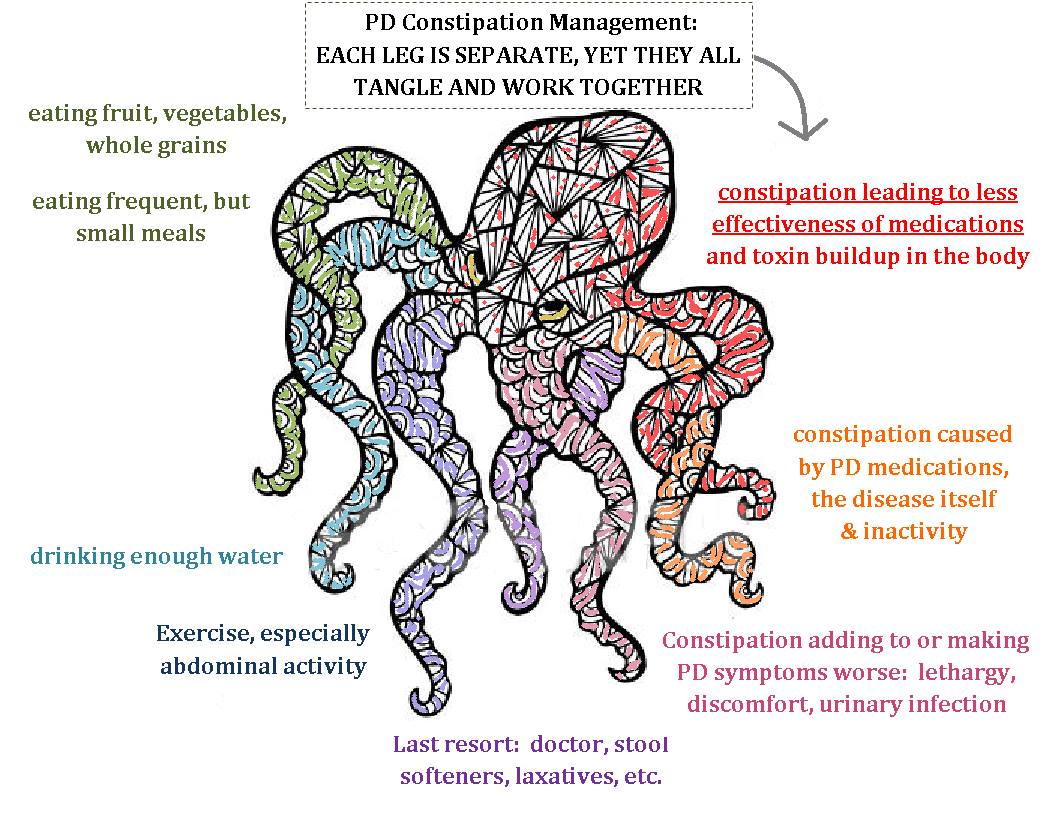
What Causes Constipation In People With Parkinson’s Disease
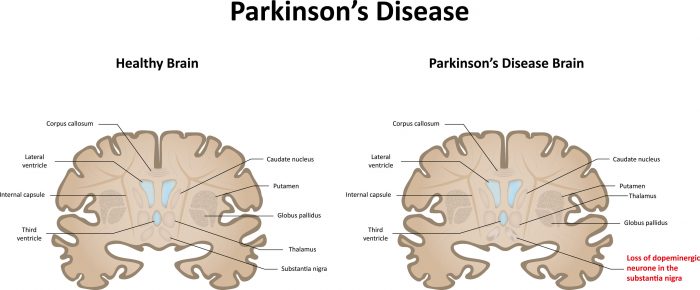
In some people with Parkinson’s disease, constipation may occur due to the improper functioning of the autonomic nervous system. The autonomic nervous system is responsible for regulating smooth muscle activity. If this system is not working properly, the intestinal tract may operate slowly, causing constipation.
Also, medications used to treat Parkinson’s disease can cause constipation.
When Parkinsons Interferes With Gastrointestinal Function
This 63-minute audio with slides by Dr. Peter A. LeWitt discusses the effect of Parkinson’s disease on the gastrointestinal system, with particular focus on constipation. Improving GI function can have a positive impact on the consistency of benefit from Parkinson’s disease medications. Highlights of recent research into Parkinson’s disease originating in the GI tract, developing biomarkers for early diagnosis, and others.
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
Dietary Fibre For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Choose easy-to-eat fibrous foods such as soft fruits. Consider mashing or pureeing fruits to make them easier to eat. Make sure to include the skin, where most of the fibre is found.
- Eat at least two pieces of fruit and five serves of vegetables every day.
- Eat homemade vegetable soups.
- Sprinkle a tablespoon of bran, psyllium husks or chia seeds on your breakfast cereal or add the bran to baked products such as cakes. However, avoid bran if you have swallowing problems.
- Fibre supplements may be helpful, but you must drink enough fluids for these to work properly. Avoid fibre supplements if you have problems swallowing.
- Don’t increase dietary fibre too quickly or you’ll risk bloating and abdominal cramps. If discomfort occurs, cut back your fibre intake, increase your fluid intake, apply a hot water bottle to your abdomen and see your doctor.
Toilet Habits And Constipation In Parkinsons Disease
Suggestions for good toilet habits include:
- Go to the toilet as soon as you feel the urge to pass a bowel motion. Hanging on can contribute to constipation.
- Use the correct posture on the toilet to help you pass a bowel motion – place your elbows on your knees, bulge out your stomach, straighten your spine and put your feet on a footstool.
- Avoid holding your breath and don’t strain when you are on the toilet. Allow yourself plenty of time.
- Use a warm washcloth pressed against your back passage or gently massage with one or two fingers to help to relax the muscles.
- Talk to your doctor or pharmacist about medicines to help soften your bowel motions.
Addressing Practical Aspects Of Eating And Drinking
Some people with Parkinson’s have problems chewing and swallowing. This can make it difficult to eat a diet with plenty of fibre. A speech and language therapist can give advice about this. Ask your GP, specialist or Parkinson’s nurse for a referral. If it takes a long time to eat and your meal goes cold, eat smaller portions and go back for seconds that have been kept warm. You can also get special plates that keep your meals hot – the Disabled Living Foundation has more information.
An occupational therapist will also be able to give you some tips and practical advice.
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
Fecal incontinence can also be related to nerve dysfunction of the anal sphincter, or the ring of muscle that controls when feces is released. Cognitive dysfunction and mobility issues may further interfere with getting to the bathroom in time. Some treatment options are similar to urinary incontinence including the use of bedside equipment to minimize mobility issues and introduction of pelvic floor exercises to strengthen the musculature that keeps feces in place.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dr. Rebecca Gilbert
How About Using Supplements In Parkinsons Disease
Some patients prefer using food supplements. Nutrition supplements like coenzyme Q10, fish oil, and vitamin D have been linked to reducing disease progression and some studies suggest that taking these supplements may benefit the patients. However, research in this direction is still limited and we can’t advise you to take any supplements at this stage. We recommend you discuss it with your healthcare provider first before considering any supplements.
Treatment For Constipation In Parkinsons Disease
Your doctor may suggest various treatments to help combat constipation, including:
- dietary changes, including more fibre rather than refined or highly processed foods, and water
- moderate exercise
- good toilet habits
- avoidance of unnecessary medicines that contain substances known to cause constipation
- laxatives, particularly agents that bulk and lubricate the stools
- treatment for any other medical problem that may be contributing to your constipation, such as haemorrhoids .
Background: The Stomach Parkinson’s And Levodopa
Levodopa is not absorbed from the stomach, but the stomach plays an important role in controlling how levodopa reaches the parts of the small intestine where it is absorbed. Some medicines, including dopamine agonists and anticholinergics, can also delay gastric emptying, as can severe stomach acidity, although over-treatment of this problem can also prevent the break-down of levodopa tablets, leading to incomplete absorption.
Unfortunately, gastric emptying can be delayed by Parkinson’s itself or by constipation caused by the colon-gastric reflex. Levodopa tablets may remain in the stomach for a long time, leading to delayed absorption in the small intestine and a delayed response to the treatment.
An enzyme called dopa-decarboxylase that is present in the stomach lining can convert levodopa trapped in the stomach into dopamine, making it unavailable to the central nervous system. Also, dopamine formed in the stomach may stimulate gastric dopamine receptors, leading to stomach relaxation and reduced gastric motility, and this can worsen the problem.
Liquid levodopa may improve motor fluctuations by ensuring better absorption than standard preparations, especially when taken after meals. Subcutaneous infusion of the dopamine agonist apomorphine is effective in controlling motor fluctuations by bypassing the gastrointestinal tract.
Diagnosis Of Constipation In Parkinsons Disease
Diagnosis of constipation may include:
- medical history
- detailed description of symptoms
- physical examination.
Medical problems other than Parkinson’s disease can also cause constipation. Your doctor may wish to do tests to rule out other possible causes. The tests depend on the medical condition under investigation.
Exercise For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Talk with your doctor, physiotherapist, exercise physiologist or healthcare professional when planning your exercise program.
- Aim for at least 30 minutes of exercise every day.
- Spend a few minutes warming up and cooling down. This could include marching in place or stretching.
- Start with the easiest exercises first. Slowly introduce the more difficult exercises as your fitness increases.
- Only exercise when other people are at home who can help if necessary.
- Remember: too little exercise and fluid intake with an increase in dietary fibre can worsen constipation for some people.
Why Might Constipation Be A Parkinson’s Symptom
This 62-minute audio with slides is presented as an interview of two neurologists and explains how the gastrointestinal musculature is well enervated and, therefore, affected by the loss of dopamine and deposits of alpha synuclein, just as the brain is. Management options are discussed, and recent research into the microbiome and the gut/brain connection in Parkinson’s disease.
What Are Those Common Triggers Of Constipation
Fluids For Constipation In Parkinsons Disease

Be guided by your doctor, but general suggestions include:
- Try to drink six to eight glasses of fluid every day. Water is best, but you can also include fluid in the form of soup, juice, tea and coffee.
- Limit drinks that cause dehydration such as alcohol, tea and coffee.
- Spread your drinks throughout the day.
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
Causes Of Constipation In Parkinsons Disease
The ways in which Parkinson’s disease can increase the risk of constipation include:
- lack of dopamine in the brain – impairs control of muscle movement throughout the body. Bowel muscles can become slow and rigid
- uncoordinated bowel motions – the bowel muscles may be weak and unable to contract, or they may clench instead of relaxing when trying to pass a motion
- eating problems – dietary fibre containing insoluble fibre adds bulk to your bowel motions and can help prevent constipation. However, if a person with Parkinson’s disease finds it difficult to chew or swallow, they may avoid eating fibrous foods
- drinking problems – you need water to plump up the dietary fibre in your bowel motions. Swallowing difficulties may discourage a person with Parkinson’s disease from drinking enough fluids
- sedentary lifestyle – lack of exercise slows the passage of food through your intestines. Parkinson’s disease reduces muscle control, so lack of exercise is common
- medications – many different medications can cause constipation. Medications used in the treatment of Parkinson’s disease may slow bowel movements or cause a decrease in appetite.
Follow A Squatty Potty Posture In The Toilet
A proper posture while sitting on the commode in the toilet is very important for controlling constipation. But this is ignored by most people.
We usually follow a slump posture while sitting in the toilet. This position is not good for proper elimination as it makes a kink in the rectum and restrains the outward movement of bowel which makes the constipation more worsen.
To avoid this, researchers recommend following a squatty potty posture. In this posture, your sitting position makes an angle in a way where your knees are above your hips, the same like you do squats. This position makes the rectum like a shoot that allows the bowel to eliminate out the stool more easily.
Using a western toilet commode can make it very hard to get into squatty potty position. However, a toilet stool can make it easier for you. So use a small stool available in your house that allows to raise your knees above your hips and make it to a squatty position when sitting in the toilet. You can also buy a , which is especially designed for squatty potty position.
Parkinsons Disease: Combating Constipation

In Part 2 of this 3-part blog series we discuss constipation related to Parkinson’s disease and the gut-brain connection.
In patients with Parkinson’s disease, the major cause of constipation is that the nervous system control of the gut slows down due to the effects of the disease, resulting in the slowing down of gut movement and leading to constipation.
Alpha-synuclein refers to the abnormal protein that is also seen in the brains of patients with PD. These same protein deposits have been observed in the gut prior to development of motor symptoms, up to 20 years prior to diagnosis. These abnormalities have also been found in the parasympathetic neurons of the vagus and sacral nerves that connect the brain to the visceral organs and are involved in the autonomic nervous system. The term parasympathetic refers to the side of the autonomic nervous system that allows the gut to move . Basically as the nervous system control of the gut slows, gut function slows and constipation results.
Interestingly, patients’ self-reports of constipation may not paint the full picture of the severity of constipation. One study found that objective measurements of colon transit time revealed higher rates of constipation than subjectively reported by patients. This is known as slow transit constipation.
Patients with PD should be aware of their bowel movements and remain vigilant to the development of constipation and should do the following to improve bowel regularity:
Urinary Difficulties In Parkinsons Disease
The most common urinary difficulty experienced by people with PD is a frequent and urgent need to urinate. Urinary incontinence, the involuntary loss of urine, is also a symptom of PD. This may occur even when the bladder is not full. Recent research studies estimate approximately 27-39% of people with PD experience urinary difficulties, although urinary incontinence only develops in about 15% of those with PD. Bladder issues usually develop in the later stages of PD.2
There are several medications that can help manage urinary difficulties, such as tolterodine, oxybutynin, darifenacin, and solifenacin. These medications work to block or reduce overactivity in the bladder. However, these medications may make the symptoms of PD worse. It is recommended to discuss these treatments with a movement disorders specialist who has been trained to understand the effects of various medications on the disease.2
Does High Dose Thiamine Cause Constipation 16 Replies
I know that some people have reported that high dose thiamine helps with constipation issues.
I have been gradually increasing my dose weekly having started at 100 mg a day and it seems to be causing constipation. I am currently at 200 mg twice a day.
Has anyone else found that high dose B1 causes constipation?
I am hoping I won’t have to discontinue it.
Thanks!
Yes, I’ve heard it can really help.
In my experience thiamine b1 doesn’t cause constipation. I had constipation before I started thiamine. A short time after I started thiamine my constipation was greatly reduced. Though it didn’t disappear completely
Thanks for your input, Grumpy. It’s great that B1 helped you.
Constipation is a symptom of Parkinson’s. I take a level teaspoon of Mannitol, an osmotic diuretic which helps constipation and for some Parkinson’s.
Thank you for your reply.
I didn’t have a problem with it before I started B1. I discontinued B1 for a week and the constipation improved. I’m now trying B1 again.
I experienced just the opposite – my constipation improved after some time on B1 injections. This was actually the only improvement I observed ……………..
How long before you saw the improvement?
About a month I think……………but due to Corona, I had to stop injections after 3 months and am now taking tablets but my constipation is worse again……….
The Gastrointestinal Tract And Parkinsons
As promised in a previous blog, I now return to the topic of the gastrointestinal tract and Parkinson’s disease . As most of you know, GI symptoms are very common in PD. We will discuss what those symptoms are, why they occur, and the current research that links what is happening in the gut to theories as to why PD occurs at all. Many of you have suggested gut-related topics for this blog including a discussion of symptoms such as bloating and constipation, and a discussion of the use of probiotics in PD. I will address these issues as well. Submit additional topics that you would like to read about here.
GI symptoms can be among the most bothersome of the non-motor symptoms of PD. Constipation is the most common of these symptoms, affecting 80-90% of people with PD. APDA has a helpful brochure with practical tips to prevent and treat constipation in PD.
GI pathology in Parkinson’s disease however, can involve the entire GI tract and includes sialorrhea and dysphagia . In addition, delayed gastric emptying, in which the digestive contents are held up in the stomach and do not move normally into the small intestine, can cause sensations of nausea and bloating.
The gut has its own nervous system
The gut as a biomarker
Entry to the brain
How do Lewy bodies propagate?
How Can It Affect People With Parkinsons
- Constipation can impact the absorption and effectiveness of levodopa .
- Constipation can disturb bladder function. An over-full bowel due to constipation can press on your bladder, reducing the amount of urine it can hold.
- Straining due to constipation can weaken your pelvic floor muscles. Pelvic floor muscle strength is important for both bladder and bowel control.
- Severe constipation is the most common cause of bowel incontinence. Bowel incontinence is the inability to control your bowel motions. It can range from soiling your underwear to the loss of a full bowel motion.
Impact Of Diet On Parkinsons Medications
Taking certain foods may interfere with the efficacy of drugs used in Parkinson’s disease. This is especially true for high-protein foods. Their consumption may affect the body’s ability to absorb levodopa, which is the most prescribed drug in Parkinson’s disease. It’s therefore good to take levodopa 30 – 60 minutes before eating the high-protein foods.
However, for some patients it causes nausea, and taking levodopa on an empty stomach might not be a good idea. In that case, taking levodopa with a small snack can enhance the absorption of the drug in the blood.
How Might Parkinson’s Affect The Bowels
Bowel problems can occur in anyone, but some problems, especially reduced bowel movement or constipation, are particularly common in Parkinson’s. This tends to be as a result of slowness of movement and muscle rigidity, both of which are visible symptoms of the condition. But Parkinson’s also muscles we cannot see – including the bowel muscles – which in turn causes a reduction or slowness of bowel movements.
Poor bowel function may be exacerbated if chewing and swallowing food is difficult, which is quite common in Parkinson’s. This may make it harder to eat a diet that is rich in fibre – for example fruit, vegetables and whole grains – which helps form soft, bulky stools and aids bowel function.
Exercise is also thought to play a role in efficient bowel function, but if Parkinson’s makes activities more difficult, the bowel may be less stimulated and the intestines can become sluggish.
Constipation is thought to affect up to 65% of people with Parkinson’s – the bowel symptoms may predate the neurological ones . Tremor and a fear of spilling drinks can mean some people unintentionally reduce their fluid intake which can make stools hard and more difficult to pass. When stools remain unpassed for a long time, they become harder as the body absorbs more water from them. If stools build up in the rectum they can become impacted and block the rectum. They may also overflow as lumps of stool or watery mucus.
Avoid Eating White Rice And White Bread
While brown rice may help relieve constipation, white rice may have the opposite effect. Unlike brown rice, white rice lacks fibers and nutrients. It’s rather rich in starch content, which is slowly digested and cause significant bloating.
Similar is the case with white bread. It is made of wheat that lacks most of its fiber content. This caused the stool hard and makes it difficult for the colon to remove it from the body. Therefore, try to avoid using white bread or anything made from white floor like cakes, cookies, donuts, and bagels.
Want More Practical Articles Like This
Much more can be found in?our?Every Victory Counts®?manual.?It’s packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action.?Request your free copy of the?Every Victory Counts?manual by clicking the button below.
Thank you to our 2021 Peak Partners,? Adamas, Amneal, Kyowa Kirin, and Sunovion, for helping us make printing, distribution, and shipping of the Every Victory Counts manual possible.
Final Thoughts: What Has Worked For Me
Some of the prescription medications that have helped me include: Amitiza, Linzess, Movantik, Relistor, Symproic, and Trulance. Plus I made sure to exercise, massage my stomach in a circular motion at least once a day, drink warm/hot water in the morning before eating, and use probiotics. I also tried to do things that helped make me feel more relaxed. In my experience, a combination of these things is what truly helps maintain a healthy bowel, which results in better PD symptom control by allowing medication to be maximally absorbed.
How Does Parkinson’s Affect The Bowel
April 11 2020
Two out of three people with Parkinson’s disease suffer from constipation, and the symptom can occur long before the diagnosis is made. Constipation is one of the most common non-motor symptoms of this condition.
Many patients find it embarrassing to talk about their bowel problems, but it is important to seek help in managing constipation. Left untreated, constipation can lead to other problems. You may feelunwell and nauseous, exacerbating the constipation as you don’t feel like eating or drinking.Constipation can also cause overactive bladder and urinary incontinence due to mechanical pressure on the bladder. Sometimes constipation makes it difficult to empty your bladder, and when urineremains in the bladder there is a risk of urinary tract infections.
We spoke to Ethan and Susan about their symptoms and how they manage it – here’s an excerpt from our free guides: “Bladder and Bowel dysfunction when you have Parkinson’s Disease”
Ethan’s story
Susan’s story
Female and male anatomy are different, and the effects of Parkinson’s disease may have different effects when it comes to bladder and bowel dysfunction.
The bladder and bowel also interact and effect the functioning of these processes. In these free guides, we look at the symptoms, effects and therapies available to manage this condition.
Bladder and Bowel dysfunction when you have Parkinson’s Disease
Treating And Managing Bowel Problems
The first step in dealing with bowel disorders is to talk to your doctor. He or she will probably review your medication to see if this is a contributory factor. Whilst it is usually possible to control any difficulties with diet, fluid intake and exercise, your doctor, or Parkinson’s nurse specialist if you have one, will be able to advise further, and may, for example, prescribe laxatives in severe cases of constipation. If you have any “alarm features” such as unintentional weight loss or rectal bleeding, then you may need to be referred for specialist assessment.
The following healthcare professionals can also advise on aspects of bowel care:
- A dietician will be able to advise on diet and fluid.
- A physiotherapist may be able to help with advice and abdominal exercises which will help in passing stools.
- A speech and language therapist can help with swallowing problems. They may be able to advise on ways of relaxing your throat, and give guidance on posture and exercises to help overcome any difficulties you have.
- An occupational therapist may also be able to suggest practical ways to overcome any difficulties you have with eating and drinking.
What Examinations May I Need To Have

Your GP or specialist will probably ask a series of questions to find out what the problem is. These may include:
- When did the trouble start?
- How often does it happen?
- Can you feel when your bladder or bowel is full?
- Are you having difficulty emptying your bladder or bowel?
- How often are you using the toilet?
Parkinson’s symptoms, such as slowness of movement and rigid muscles, affect the muscles in the bowel wall. This can make it harder to push stools out of the body. You may be asked to keep a chart for several days of how often you use the toilet and how much you drink.
Bladder or bowel problems can be complex in Parkinson’s, so sometimes specialist tests or X-rays may be needed. All of these can usually be done in an outpatient department or clinic.
How Can I Avoid Getting Constipated
- Eat a well-balanced diet with plenty of fiber. Good sources of fiber are fruits, vegetables, legumes, and whole grain bread and cereal. Most of the fiber in fruits is found in the skins. Fruits with edible seeds, such as strawberries, have the most fiber. Eat bran cereal or add bran cereal to other foods, such as soup.
- Drink 1½ to 2 quarts of water and other fluids a day. Liquids that contain caffeine, such as coffee and soft drinks, seem to have a dehydrating effect and may need to be avoided until your bowel habits return to normal.
- Move your bowels when you feel the urge.
Medication Side Effects And The Gut
The interactions between PD medication ingestion and the gut can play a major role in motor fluctuations – the phenomenon in which a patient’s response to Levodopa varies widely during the day. A recent APDA webinar helps to explain this interplay.
Delayed gastric emptying
Delayed gastric emptying can interfere with medication absorption. Medication doses that are ingested by mouth may sit in the stomach before being transported to the small intestine where they are absorbed. Delayed gastric emptying could be responsible for dose failures – when a dose of medication does not have a robust enough effect.
Protein effect
Levodopa crosses the wall of the small intestine via a molecule in the intestinal wall that transports amino acids, the building blocks of protein. When dietary protein is also present in the small intestine, then there are fewer transporters available for Levodopa to use. A patient may therefore experience the “protein effect”, in which he or she feels that medication is not as effective after a high-protein meal. Sources of dietary protein include: beef, chicken, pork, fish, eggs, nuts and dairy.
Helicobacter pylori and small intestinal bacterial overgrowth
About a third of PD patients are infected with Helicobacter pylori, a common bacteria which can cause gastritis and ulcers. Infection with Helicobacter pylori has been linked to worsened motor fluctuations. It can be diagnosed with a urea breath test that analyzes exhaled air.
