Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed

In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half “of the patients were described as unable to make any decisions in the last month of life.” 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Identifying Newly Diagnosed Pd Patients And Matched Controls For Each Pd Patient
The study population comprised newly diagnosed patients with PD and their matched controls. First, we identified PD patients using the registration code for PD in the program for rare, intractable disease from January 1, 2004, to December 31, 2006, and we defined the index date as the date of the earliest claim with the V124 code. To remove any prevalent cases, we excluded patients who had PD diagnostic codes or PD registration codes before January 1, 2004. As the V124 registration criteria did not exclude atypical Parkinsonian syndromes, we excluded patients diagnosed with atypical parkinsonism during the entire study period, from 2002 to 2017. Moreover, we excluded patients under 40 years of age. Lastly, we excluded patients whose total number of days of antiparkinsonian medications was less than 180 days. The list of the antiparkinsonian medications used in this study is given in Supplementary Table S1.
Then, we selected up to four controls for each PD patient matched by sex and age at the index date. Previous studies reported that matching 4 controls to 1 patient can minimize the bias in measuring treatment effect in the maximum number of matched controls12,13. Individuals who had the registration code for rare, intractable disease for PD , had any diagnostic code for Parkinsonism , or had been prescribed an antiparkinsonian drug during the study period were not recruited as controls.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Can I Support Someone With Parkinson’s At The Advanced Or Palliative Stage
In the advanced stages of Parkinson’s, your patient’s care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the ‘whole person’ to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinson’s may be supported by a number of professionals, including a Parkinson’s nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinson’s should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the person’s wishes and preferences are for their care in the future. They may include decisions on any treatments the person doesn’t want to have in the future – this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
What Other Conditions Have Similar Symptoms And Signs Of Parkinsons Disease

Other neurological diseases may cause symptoms similar to Parkinson’s disease. The term Parkinsonism refers to a patient that has symptoms similar to Parkinson’s.
Early in the disease process, it can be tough to make an assertive diagnosis and difference between Parkinson’s and Parkinson-like diseases.
Often the correct diagnosis is made after further symptoms develop, and the physician can monitor the course of the disease.
The development of additional symptoms and the course of the illness generally points towards the correct diagnosis. These are the most common neurological diseases that can produce Parkinson-like symptoms.
- Progressive Supranuclear Palsy
- Lewy Body disease or Dementia with Lewy bodies
- Corticobasal degeneration or corticobasal ganglionic degeneration
Nonetheless, doctors should think of other causes rather than Parkinson’s disease when events like this happen.
- Poor response to dopamine
- Early loss of balance or vision problems
- Prominent intellectual decline – dementia
- Rapid onset or progression of the disease
Actually, though it is a disease that is not clearly understood, there are specific organizations like Parkinson’s UK that dedicate themselves to doing research.
These organizations look forward to following the natural course of the disease and developing clinical trials for patients in an attempt to find a cure.
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
How Can Parkinson’s Affect Someone At The Advanced Or Palliative Stage
Parkinson’s progresses in stages: diagnosis, maintenance, advanced and palliative. Professionals should have talk to people with Parkinson’s about advance care planning in the earlier stages of the disease. This can allow them to express their wishes and preferences for their care in the later stages of the disease and make plans for the future.
Although the condition progresses differently and at a different speed for each person, the advanced stage can potentially cover a long period of time.
Problems that affect someone with advanced Parkinson’s may include:
- medicines being less effective at managing symptoms than before
- having to take lots of medicines to manage symptoms and side effects
- more ‘off’ periods – when the effects of medication are reduced, and people experience movement fluctuations and involuntary movements
- increased mobility problems and falls
- swallowing difficulties
- less control of their Parkinson’s symptoms, which become less predictable
- pain.
Some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection, such as pneumonia. People with Parkinson’s most often die because of an infection or another condition, usually caused by Parkinson’s.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
What Is The Prognosis And Life Expectancy For Parkinson’s Disease

The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a “last in, first out approach.” 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patient’s medication history should be considered.29
How Is Parkinsons Dementia Different From Alzheimers Disease
The advanced cognitive changes that impact daily living in Alzheimer’s and Parkinson’s disease are both types of dementia.
Parkinson’s disease dementia can occur as Parkinson’s advances, after several years of motor symptoms. Dementia with Lewy Bodies is diagnosed when cognitive decline happens first, or when Parkinson’s motor symptoms and cognitive decline occur and progress closely together. Cognitive impairments in PDD, combined with the movement symptoms of the disease, produce a greater impact on social and occupational functioning than Alzheimer’s.
Alzheimer’s, a fatal brain disease, causes declines in memory, thinking and reasoning skills. Physicians can diagnose Alzheimer’s. Visit the Alzheimer’s Association to learn the 10 signs Alzheimer’s disease.
Fortunately for people with PD, Parkinson’s disease dementia is less disabling than Alzheimer’s disease. People with Alzheimer’s have language difficulties earlier than people with Parkinson’s, and no new memories are formed. People with PD also have more ability to compensate and adjust based on cues.
Two Areas In Which Parkinsons Disease May Bring About Death
I. Falls
PD patients are at an increased risk of falling and bad falls can lead to death. This usually occurs as a complication of a fall that requires hospitalization, particularly if it involves surgery. While most people do not fracture their hips when they fall, some do, and hip surgery, while routine, is still major surgery. It carries the risk of infection, delirium related to pain medications and anesthesia, heart failure, pneumonia, blood clots in the legs that then go to the lungs, and general weakness from immobility. Hip fractures are probably the main cause for death for those who fall, but people can fracture other bones and require surgery. They may fracture their ribs, which leads to reduced coughing, because of the pain, and an increased risk of lung infections . It is surprisingly uncommon for Parkinson’s Disease patients to die from brain injuries related to falls, but it still may occur.
II. Pneumonia
PD patients also may develop pneumonias completely unrelated to difficulties with swallowing, just like their non-PD friends and relatives.
Standard Protocol Approval Registration And Patient Consent
The study protocol was assessed and determined to be exempt from review by the Institutional Review Board of Seoul National University Hospital . Furthermore, the NHIS approved the use of its database and provided data after excluding all possible patient identification information . The requirement for informed consent was waived by the Institutional Review Board of the Seoul National University, because the database was anonymized. All methods were carried out in accordance with relevant guidelines and regulations.
What Is The Best Way To Communicate With A Person With Pdd
PD-related mood and motor changes can impact communication; cognitive changes and Parkinson’s disease dementia can further these difficulties.
- It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. Stay calm and be patient. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- You may find acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior: the person may be hungry, thirsty, tired, in pain, frustrated, lonely or bored.
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- It’s OK to use humor to diffuse stressful situations but avoid negative humor or sarcasm ? these can be misunderstood.
Page reviewed by Dr. Jori Fleisher, MSCE, Assistant Professor, Department of Neurological Sciences at Rush University Medical Center, a Parkinson’s Foundation Center of Excellence.
What To Do With Deep Brain Stimulation At The End Of Life

Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patient’s handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
Janet Reno’s Death: How Does A Person Die Of Parkinson’s
Former U.S. Attorney General Janet Reno has died at age 78 from complications of Parkinson’s disease, her family announced today. But how do people die from this disease?
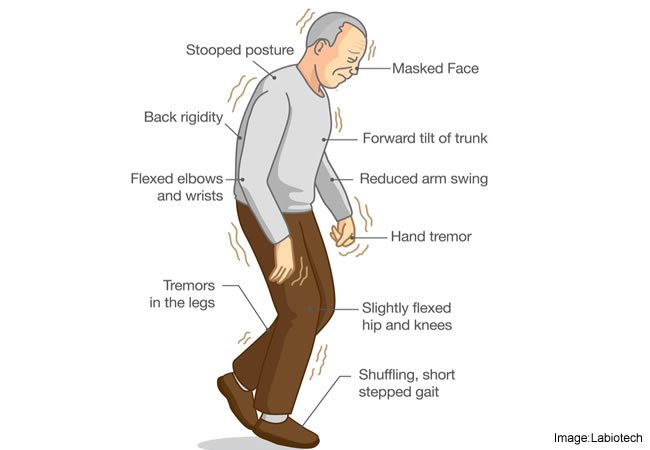
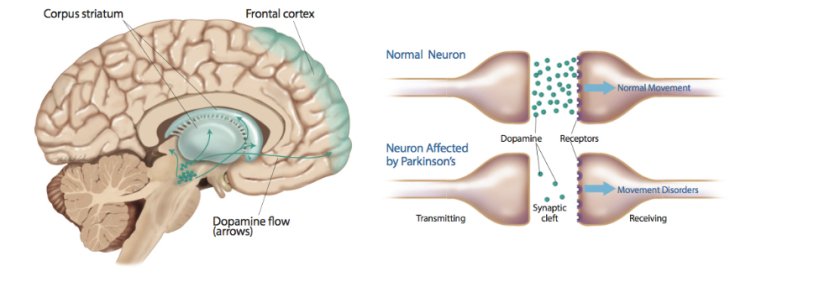
In patients with Parkinson’s disease, the brain cells that produce a chemical called dopamine start to die off. It’s not clear what triggers the death of these cells, but researchers do know that dopamine is important for the control of muscle movement. Parkinson’s patients experience symptoms such as tremors, slowed movements, muscle stiffness and impaired balance.
Parkinson’s itself is usually not considered a deadly disease, and many people with the disease have a life expectancy that’s close to the average life expectancy in the general population, according to the Parkinson’s Disease Foundation.
“You die with Parkinson’s disease, not from it,” according to the Michael J. Fox Foundation for Parkinson’s Research. Reno’s family did not release any further details about her death.
But in some cases, advanced symptoms of Parkinson’s disease can lead to complications that result in death, the Michael J. Fox Foundation says. For example, patients can have problems swallowing because they have a loss of control over the muscles in their throat.
Patients also may have impaired balance, which can result in falls that lead to serious or even fatal injuries, the Michael J. Fox Foundation says.
New Clues On Why Some People With Parkinson’s Die Sooner
- Date:
- American Academy of Neurology
- Summary:
- New research shows how old people are when they first develop Parkinson’s disease is one of many clues in how long they’ll survive with the disease.
New research shows how old people are when they first develop Parkinson’s disease is one of many clues in how long they’ll survive with the disease. The research is published in the October 5, 2010, print issue of Neurology®, the medical journal of the American Academy of Neurology.
The 12-year study included 230 people with Parkinson’s disease, of whom 211 died by the end of the research. “Remarkably, time to death for these people took anywhere from two to 37 years from diagnosis so it’s important we try to identify those risk factors that lead to an early death so we can find ways to increase a person’s life expectancy,” said Elin Bjelland Forsaa, MD, with Stavanger University Hospital in Norway and a member of the American Academy of Neurology.
The average time from the appearance of movement problems to death was 16 years. The average age at death was 81.
The study found that the risk of earlier death was increased about 1.4 times for every 10-year increase in age when symptoms began. People with psychotic symptoms, such as delusions and hallucinations, were also 1.5 times more likely to die sooner compared to those without these symptoms.
The study also found that taking antipsychotic drugs or drugs for Parkinson’s disease had no negative effect on survival.
Story Source:
How Can Falls Resulting From Parkinsons Disease Be Fatal
Patients with Parkinson’s disease are seen to be at an increased risk of bad falls which can lead to death. Generally it is seen that death results from hip fractures that require hospitalization because surgery would be required. Hip surgery is a major operation which carries the risk of infection, heart failure and blood clots. Such clots become dangerous if they reach the lungs. Sometimes fall may even lead to fatal brain injuries if not taken care properly.
Complications Related To Parkinson’s Can Affect Survival

Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Parkinson’s is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinson’s disease in the United States. During the six-year period, 64% of the participants with Parkinson’s disease passed away.
The risk of death of those with Parkinson’s was then compared to Medicare beneficiaries who did not have Parkinson’s or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinson’s was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinson’s disease was similar to those with hip fracture, Alzheimer’s dementia, or a recent heart attack—although it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
New Clues On Why Some People With Parkinsons Die Sooner
The American Academy of Neurology, an association of more than 22,000 neurologists and neuroscience professionals, is dedicated to promoting the highest quality patient-centered neurologic care. A neurologist is a doctor with specialized training in diagnosing, treating and managing disorders of the brain and nervous system such as epilepsy, dystonia, migraine, Huntington’s disease, and dementia.For more information about the American Academy of Neurology, visit http://www.aan.com.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
What Medications Are Used To Treat Parkinsons Disease

Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Can A Person With Parkinsons Have A Normal Life Span
When people first hear about a Parkinson’s diagnosis, their thoughts often go to the worst-case scenario. However, it’s important to keep a positive perspective about your senior loved one’s diagnosis. While you can expect your loved one to develop some symptoms such as tremors, there are many things that can be done to give him or her an excellent prognosis for a long and happy life.
How To Take Care Of Patients With Parkinsons Disease
The condition of Parkinson’s disease progress with time and demands care from a care giver. The disease affects the motor abilities of the patient and the gradual loss of independence can be disheartening. Care givers should-
Emotional Support: Try maintaining the quality of life of the patient with proper mental support.
Follow-Up: It is the responsibility of the caregiver to take the patient for proper follow-ups to the doctor.
Diet: The care giver should keep an eye on the diet of the patient. He should have a balanced and nutritious diet. He should also be motivated to exercise regularly.
Learn More About the Disease:The care giver should make attempts to learn about the symptoms of Parkinson’s disease in order to provide sufficient empowerment to the patient.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
How Does The Parkinsons Disease Progress Over Time
Although slow, Parkinson’s disease is progressive in nature where the condition keeps worsening at every stage.
In the initial stage, the symptoms are seen to be mild in nature. The symptoms do not really interfere with the daily tasks and the lifestyle of the patient. The tremors and problems with balance, movement starts from one side of the body.
The next phase is characterized by moderate form of the symptoms which are distinctively noticed by people. The muscles become stiff and posture is likely to be irregular. Exercise may be recommended by the doctor to ease out the stiffness. However, balance of the patient is not much impaired.
The next stage is considered to be the turning point of the symptoms because the patient may start to lose control over his balance of the posture. He may also experience decreased reflex and is more prone to fall down while his movements become slower. In this stage, occupational therapy is required to help the patient with the stiffness and fine motor abilities.
In the second last stage the patient may not even be able to stand without help. The patient should not live alone because daily activities cannot be done independently. It is extremely important to have the assistance if a care giver at this stage.
Also Read:
How Long Can A Person Live With Stage 5 Parkinson
When patients reach stage five – the final stage of Parkinson’s disease – they will have severe posture issues in their back, neck, and hips. In end–stage of Parkinson’s disease, patients will also often experience non-motor symptoms. These can include incontinence, insomnia, and dementia.
Additionally, what do Parkinson’s patients usually die from? But the most common cause of death in those with Parkinson’s is pneumonia, because the disease impairs patients‘ ability to swallow, putting them at risk for inhaling or aspirating food or liquids into their lungs, leading to aspiration pneumonia.
Also asked, what happens in stage 5 Parkinson’s?
Stage Five of Parkinson’s Disease –Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
How quickly can Parkinson’s progress?
While symptoms and disease progression are unique to each person, knowing the typical stages of Parkinson’s can help you cope with changes as they occur. Some people experience the changes over 20 years or more. Others find the disease progresses more quickly.

