The Parkinsons Disease News Today Forums Are A Place To Connect With Other Patients Share Tips And Talk About The Latest Research Check Them Out Today

• Don’t focus on the what-ifs. They’ll defeat you most every time. Do focus on “now.” It may seem like a tremendous struggle at the moment, but things could be worse. Today may be one of the harder days, but when the clock strikes 12, it’s a new day. Something wonderful could be ahead, waiting to happen. Your patient may turn into a pumpkin! Don’t lose hope.
• If you don’t have one already, get a sense of humor. Without one, you’ll often despair. Find something funny in every day. You need to laugh.
• Get yourself into a support group locally or online. You may not think you need it, but you do. Especially as the road becomes bumpier. And it will get bumpier. Get some support in place now, as it will make things easier to deal with later.
• You need your friends. Don’t alienate them by thinking you can do this by yourself. Accept their invitations to help. Accept an hour off, washing the dishes, picking up some groceries, dropping the kids off at practice, or cooking your family a meal. Give yourself some slack and let your friends feel needed, because if they are offering to help before you have even asked, they may see your need better than you can.
• Try to think ahead. Your loved one’s mental faculties may not be so great anymore. A daily schedule may be useful, with a reminder for doctor’s appointments, visitors, special occasions, etc.
***
Im In Pain But I Dont Want To Take Carbidopa/levodopa Yet Because My Doctor Says It Will Only Work For Five Years Any Advice
It is true that as time passes and your disease progresses, you will have to take higher doses to replace the dopamine your body can no longer produce. However, the rate of dopamine loss is different for everyone. What your doctor may be telling you is that after taking carbidopa/levodopa for some time, you may begin to experience side effects like dyskinesia. It is important to understand that while you may experience this unwanted side effect, for example, you still benefit from the carbidopa/levodopa. If you believe your pain is Parkinson’s-related, and you have already tried other medications and complementary therapies without relief, it is probably time to try carbidopa/levodopa.
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half “of the patients were described as unable to make any decisions in the last month of life.” 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Stage Four: Symptoms Are Severe And Disabling And You Often Need Assistance To Walk Stand And Move
Stage Four Parkinson’s disease is often called advanced Parkinson’s disease. People in this stage experience severe and debilitating symptoms. Motor symptoms, such as rigidity and bradykinesia, are visible and difficult to overcome. Most people in Stage Four aren’t able to live alone. They need the assistance of a caregiver or home health aide to perform normal tasks.
Stage Three: Symptoms Are More Pronounced But You Can Still Function Without Assistance

The third stage is considered moderate Parkinson’s disease. In this stage, you’ll experience obvious difficulty with walking, standing, and other physical movements. The symptoms can interfere with daily life. You’re more likely to fall, and your physical movements become much more difficult. However, most patients at this stage are still able to maintain independence and need little outside assistance.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
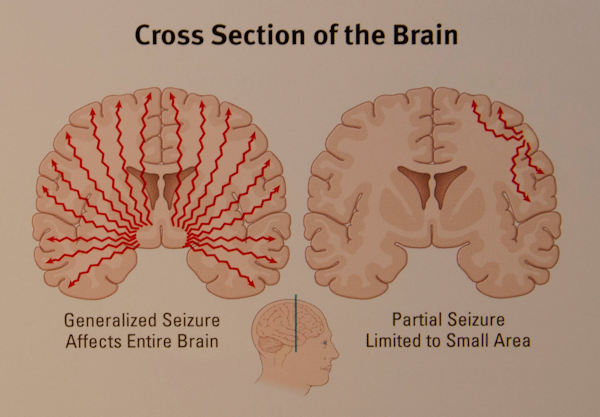
Relationship Between Disrupted Neuronal Connectivity And Epileptic Seizures
Epilepsy is considered a disease of network dysfunction.47,48 At a microscopic level, both simple and complex partial seizures involve disruptions in the excitatory interactions between cerebral cortex pyramidal cells.49 From a neurophysiology view, the EEG-graphic representation of an epileptic event is characterized by the paroxysmal onset of hyper-synchronized sharp waves disrupting the neuronal background activity. This activity is often multifocal, reflecting a broader network dysfunction.50,51 Moreover, TMS studies demonstrate similar neurophysiologic features between epilepsy and PD characterized by a state of increased cortical excitability as indicated by reduced intra-cortical inhibition and increased intra-cortical facilitation observed in both patient populations.25,52–55 As mentioned before, in PD, cortical neurons innervating the basal ganglia become hyperexcitable, possibly as a compensatory mechanism following the incremental rise in the output threshold of striatal dopaminergic neurons. As such, it would not be surprising if this putatively maladaptive phenomenon may eventually lead to the generation of epileptiform activity. While epidemiologically, epilepsy-increased comorbidity in patients with PD remains questioned,13,56 our group published the largest case series of patients with PD with concomitant epilepsy57 raising the possibility that epileptic activity in these patients may indeed be under-diagnosed and under-recognized.
Directions Of Deep Brain Stimulation For Epilepsy And Parkinsons Disease
- 1Department of Computer Science and Information Engineering, National Cheng Kung University, Tainan, Taiwan
- 2Institute of Basic Medical Science, National Cheng Kung University, Tainan, Taiwan
- 3Institute of Medical Informatics, National Cheng Kung University, Tainan, Taiwan
- 4Department of Psychology, National Cheng Kung University, Tainan, Taiwan
Background: Deep brain stimulation is an effective treatment for movement disorders and neurological/psychiatric disorders. DBS has been approved for the control of Parkinson disease and epilepsy.
Objectives: A systematic review and possible future direction of DBS system studies is performed in the open loop and closed-loop configuration on PD and epilepsy.
Methods: We searched Google Scholar database for DBS system and development. DBS search results were categorized into clinical device and research system from the open-loop and closed-loop perspectives.
Results: We performed literature review for DBS on PD and epilepsy in terms of system development by the open loop and closed-loop configuration. This study described development and trends for DBS in terms of electrode, recording, stimulation, and signal processing. The closed-loop DBS system raised a more attention in recent researches.
What Are The Important Points Regarding Apomorphine At The End Of Life

Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
Subclinical Or Atypical Epileptic Seizures Could Masquerade As Non
While the non-motor questionnaire and non-motor symptoms scale 73,74 allow improved detection and tracking of NMD-PD, the symptoms often remain under-recognized and under-appreciated by clinicians and caretakers. Recently, six different clinical phenotypes of PD were recognized on the basis of prevalent NMS-PD.75 These non-motor signatures included cognitive impairment, apathy, depression/anxiety, REM behavioral disorder , lower limb pain, and weight loss/olfactory dysfunction. This distinction may help in promoting the incorporation of NMS-PD into routine assessments, emphasizing the importance of these features for an adequate appreciation of the patient’s clinical picture. On the other hand, a rigid categorization may challenge the flexible and consistent monitoring of these dynamic and overall nonspecific symptoms along the disease course.
In the following section, we will focus on clinical features frequently displayed by patients with PD that may signal an ongoing subclinical or non-motor epileptic event masquerading as NMS-PD.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Which Medications Can Make Confusion And Hallucinations Worse

As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a “last in, first out approach.” 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patient’s medication history should be considered.29
Visual Hallucinations: Differential Diagnosis And Treatment Copyrightcited by
Have you ever encountered a patient who reported isolated visual hallucinations but did not have any other symptoms of delirium or psychosis? Have you wondered which medical and neurologic illnesses may present with visual hallucinations? Have you deliberated about how best to work up and treat patients with visual hallucinations?
If you have, then the following questions and answers should serve to frame the differential diagnosis of visual hallucinations and to explore the available options for diagnostic testing and treatment.
How Can The Etiology Of Visual Hallucinations Be Determined
Given the broad variety of potential etiologies of visual hallucinations outlined previously, it is clear that an accurate diagnosis is required before effective treatment can be initiated. A thorough history and clinical examination are the most vital elements of a workup for visual hallucinations. Associated symptoms and characteristics of the visual hallucinations themselves may help direct diagnosis . The elicitation of signs or symptoms of psychosis, inattention, parkinsonism, impaired vision, or headache will narrow the diagnosis and prompt further diagnostic studies. An EEG is potentially the most revealing diagnostic study, since it can not only highlight seizure activity, but also detect delirium , delirium tremens , and CJD .54,55 An MRI of the brain can uncover tumors or infarcts that may be responsible for Anton’s syndrome or peduncular hallucinosis, and may also show the characteristic “pulvinar sign” associated with CJD.
Epileptic Seizures In Neurodegenerative Dementia Syndromes AJ Larner*
Consultant Neurologist. Cognitive Function Clinic, Walton Centre for Neurology and Neurosurgery, Liverpool, United Kingdom
- *Corresponding Author:
- Cognitive Function Clinic, Walton Centre for Neurology and Neurosurgery, Lower Lane, Fazakerley, Liverpool, UKTel: 151 529 5727FAX: 151 529 8552
Visit for more related articles at Journal of Neurology and Neuroscience
What To Do With Deep Brain Stimulation At The End Of Life

Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patient’s handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue with someone who is experiencing a hallucination or delusion. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Chauncey Spears, Movement Disorders Fellow at the University of Florida, a Parkinson’s Foundation Center of Excellence.
Antiepileptic Drug Shows Neuroprotection In Parkinsons
REPORTING FROM ICPDMD 2018
NEW YORK – The loss of dopaminergic neurons is known to be a pivotal mechanism in Parkinson’s disease , but early research into the anticonvulsant drug valproic acid has found it may produce antioxidant and neuroprotective actions that enhance the effects of levodopa, as reported at the International Conference on Parkinson’s Disease and Movement Disorders.
Dr. Ece Genc
“Levodopa had better activity than valproic aside, but when they are used together, they have really very effective results,” said Ece Genç, PhD, of Yeditepe University in Istanbul, who reported on the research conducted in her laboratory.
Dr. Genç noted her research in rats has focused on the possible mechanisms of neurodegeneration in Parkinson’s disease: mitochondrial dysfunction, oxidative stress and tissue damage, disruption in protein organization, and cell death caused by inflammatory changes. “Dopamine metabolism can itself be a toxic compound for the neurons,” she said, explaining that dopamine is critical for stabilizing nerve synapses, but its dysregulation can cause oxidative stress of the neurons, leading to cell death.
Previous research that has shown the rotenone model of valproic acid provided neuroprotection helped drive her research, she said .
One of the drawbacks of valproic acid is that it affects so many different channels in the body. “We have to find some drugs with more targeted action.” Dr. Genç said.
Dr. Genç did not report any relevant disclosures.
Stage One: Symptoms Affect Only One Side Of Your Body
The initial phase of Parkinson’s disease typically presents with mild symptoms. Some patients will not even detect their symptoms in the earliest phases of this stage. Typical motor symptoms experienced in Stage One include tremors and shaking limbs. Family members and friends may begin to notice other symptoms including tremor, poor posture, and mask face or loss of facial expression.
What Drug Treatments Are Commonly Prescribed For Pain

Dopamine agonists are often the neurologist’s first weapon to alleviate Parkinson’s-related pain. Levodopa is used to treat many types of pain due to Parkinson’s because it treats the motor symptoms such as rigidity and dystonia that are causing them. Other medicines called analgesics can also be used to treat pain. When talking with your doctor, it is critical to let her know about all of the medications you are taking– including over the counter drugs, herbs, vitamins and mineral supplements. Without complete information, your doctor may prescribe a drug that could have serious adverse effects.
Parkinson Disease And The Risk Of Epileptic Seizures
Boston Collaborative Drug Surveillance Program, Lexington, MA
Boston University School of Public Health, Boston, MA
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Boston Collaborative Drug Surveillance Program, Lexington, MA
Hospital Pharmacy, University Hospital Basel, Basel, Switzerland
Search for more papers by this author
Boston Collaborative Drug Surveillance Program, Lexington, MA
Boston University School of Public Health, Boston, MA
Basel Pharmacoepidemiology Unit, Division of Clinical Pharmacy and Epidemiology, Department of Pharmaceutical Sciences, University of Basel, Basel, Switzerland
Boston Collaborative Drug Surveillance Program, Lexington, MA
Hospital Pharmacy, University Hospital Basel, Basel, Switzerland
Search for more papers by this author
To assess the association between incident Parkinson disease and subsequent incident epileptic seizures.
What Are The Different Categories Or Types Of Tremor
Tremor is most commonly classified by its appearance and cause or origin. There are more than 20 types of tremor. Some of the most common forms of tremor include:
Essential tremor
Essential tremor is one of the most common movement disorders. The exact cause of essential tremor is unknown. For some people this tremor is mild and remains stable for many years. The tremor usually appears on both sides of the body, but is often noticed more in the dominant hand because it is an action tremor.
The key feature of essential tremor is a tremor in both hands and arms, which is present during action and when standing still. Additional symptoms may include head tremor without abnormal posturing of the head and a shaking or quivering sound to the voice if the tremor affects the voice box. The action tremor in both hands in essential tremor can lead to problems with writing, drawing, drinking from a cup, or using tools or a computer.
Tremor frequency may decrease as the person ages, but the severity may increase, affecting the person’s ability to perform certain tasks or activities of daily living. Heightened emotion, stress, fever, physical exhaustion, or low blood sugar may trigger tremor and/or increase its severity. Though the tremor can start at any age, it most often appears for the first time during adolescence or in middle age . Small amounts of alcohol may help decrease essential tremor, but the mechanism behind this is unknown.
Dystonic tremor
Cerebellar tremor
Parkinsons As A Disease Of Neuronal Connectivity
The clinical manifestations of neurodegenerative disorders have been traditionally described from an impaired neuronal circuitry perspective.14 Technological advancements have led to a surge of studies investigating the impact PD has on neural excitability and connectivity utilizing electroencephalogram , neuromodulation techniques, imaging modalities, and graph-analytical methods. Although the field of PD has been somewhat slower to incorporate these concepts compared to other disease models, clinicians now generally acknowledge the complex, multifaceted nature of the disease and the need to pursue multidimensional approaches to study it.
To further establish the clinical applicability of connectome network dysfunction, studies have demonstrated that circuit-specific modulatory therapies, such as repetitive TMS, can alleviate various symptoms of PD, from memory and motor symptoms to depression in PD.31–34 Although from a therapeutic standpoint, there is much to streamline and corroborate with respect to repetitive TMS paradigms and methodologies, there is no denying the potential to providing individualized circuit-specific modulatory therapies.35
What Type Of Pain Occurs With Parkinsons Disease

The types of pain associated with Parkinson’s include: aching or burning pain from muscles or skeleton, sharp pain from a nerve or nerve root, numbness or “pins and needles” pain also radiating from a nerve or nerve root, pulsing or aching pain that results from tightness or ongoing twisting and writhing movements , restlessness caused from akathisia, and sudden, sharp burning pain that occurs for no known reason.
How Is Psp Different From Parkinson’s Disease
PSP is often misdiagnosed as Parkinson’s disease, especially early in the disorder, as they share many symptoms, including stiffness, movement difficulties, clumsiness, bradykinesia , and rigidity of muscles. The onset of both diseases is in late middle age. However, PSP progresses more rapidly than Parkinson’s disease.
- People with PSP usually stand exceptionally straight or occasionally tilt their heads backward . This is termed “axial rigidity.” Those with Parkinson’s disease usually bend forward.
- Problems with speech and swallowing are much more common and severe in PSP than in Parkinson’s disease and tend to show up earlier in the disease.
- Eye movements are abnormal in PSP but close to normal in Parkinson’s disease.
- Tremor is rare in PSP but very common in individuals with Parkinson’s disease.
Although individuals with Parkinson’s disease markedly benefit from the drug levodopa, people with PSP respond minimally and only briefly to this drug.
People with PSP show accumulation of the protein tau in affected brain cells, whereas people with Parkinson’s disease show accumulation of a different protein called alpha-synuclein.
What Symptoms Can Be Expected In Advanced Pd
- Pain – 86%
- Shortness of breath – 54%
- Problems in swallowing – 40%14
In an analysis of 339 death certificates and medical notes in the UK, pneumonia was found to be a “terminal event in 45%”.13
Caregiver distress with choking and the risk of “choking to death” is also mentioned in a separate study in to experiences regarding all stages of PD.4
In a survey of symptoms and their association with quality of life, in those patients with advanced disease, uncontrolled pain, anxiety and hallucinations were significantly associated with poor quality of life.9
Seizures are also noted in a description of the last phase of Parkinsonian syndromes,15 and in retrospective studies of PD patients’ overall.16,17
These above symptoms often occur on the background of weight loss, pain, and cognitive impairment. It is important therefore to note which medications given at the end of life may exacerbate these symptoms, and which should be considered in anticipation of them.
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinson’s report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include “delirium,” in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and “isolated minor symptoms” or “minor hallucinations,” including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinson’s. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinson’s not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinson’s is a complex disease and as it progresses the percentages and risk of symptoms will change.
Parkinsons Disease And Cryptogenic Epilepsy

Milton C. Biagioni
1The Marlene and Paolo Fresco Institute for Parkinson’s & Movement Disorders, NYU Langone Medical Center, New York University School of Medicine, New York, NY, USA
2Department of Neurology, Baylor Scott & White Healthcare, Austin, TX, USA
Abstract
Epilepsy is an uncommon comorbidity of Parkinson’s disease and has been considered not directly associated with PD. We present five patients who had concomitant PD and cryptogenic epilepsy. Although rare, epilepsy can coexist with PD and their coexistence may influence the progression of PD. While this may be a chance association, an evolving understanding of the neurophysiological basis of either disease may suggest a mechanistic association.
1. Introduction
Parkinson’s disease is traditionally considered primarily a subcortical disorder with late cortical involvement. There is, however, mounting evidence of considerable cortical involvement, even in the early stages of PD . The damage seems to involve, at least in part, the simultaneous processes of both the diffuse progressive deposition of alpha-synuclein and the secondary biological changes that disrupt neural connectivity . These processes reinforce the concept of dysfunctional neural networks as a potential basis of symptomatology in PD .
2. Methods
3. Cases
| 1 | |
| H&Y stage at PD Dx | 1 |
| H&Y stage at epilepsy Dx | N/A |
| H&Y stage at last visit | 3 |
| 796 | 780 |
3.1. Patient 1
3.2. Patient 2
3.3. Patient 3
3.4. Patient 4
3.5. Patient 5
4. Discussion
Competing Interests
Potential Therapeutic Implications For Non
Current available therapies for treating NMS-PD include pharmaceutical therapies, exercise, and brain stimulation to improve various NMS-PD.88,89 Cognitive deficits contribute largely to the morbidity of NMS-PD and have remained without efficient therapy. AEDs have been proposed to prevent the cellular death and cognitive worsening associated with the presence of epileptic seizures in AD.90 In light of the aforementioned similarities between PD and AD constructs, we believe that the long-term impact and therapeutic implications of AEDs on the natural course of PD should indeed be adequately investigated through properly designed clinical trials in the future.
Many mechanisms of cognitive decline and other NMS-PD have been proposed in PD. These include progressive alpha-synuclein disease, affected neurotransmitter systems, synaptic changes, inflammation, mitochondrial dysfunction, genetic risk factors,91 white matter lesions,92 and network dysfunction.93,94 While studies in AD have begun to support the role of connectome dysfunction in accelerating cognitive decline through recurrent epileptic events, this possibility remains to be investigated in patients with PD. As such, properly designed studies should be conducted to better characterize these phenomena in this specific population.
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinson’s disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
Medications Used For Treating Psychosis
Antipsychotic agents are designed to balance abnormal chemical levels in the brain. Up until the 1990s, the use of antipsychotics in PD was controversial because the drugs used until that time work by reducing excess dopamine. This alleviated psychosis but caused dramatic worsening of PD motor symptoms.
Fortunately, medications that are better tolerated by people with PD are now available. Today, there are three antipsychotic medications considered relatively safe for people with PD: quetiapine , clozapine and the newest agent, pimavanserin . They cause limited worsening of PD while treating hallucinations and delusions.
What Is Progressive Supranuclear Palsy
Progressive supranuclear palsy is a rare brain disorder that causes problems with movement, walking and balance, and eye movement. It results from damage to nerve cells in the brain that control thinking and body movement. The disorder’s long name indicates that the disease worsens and causes weakness by damaging certain parts of the brain above nerve cell clusters called nuclei that control eye movements.
PSP is different than Parkinson’s disease—another movement disorder—although they share some symptoms . Currently there is no effective treatment for PSP, but some symptoms can be managed with medication or other interventions.
Clinical Effectiveness Of Zonisamide
Murata et al. incidentally found that ZNS was effective in treating PD patients. Since then, several clinical trials have been performed to explore the effectiveness of ZNS for the treatment of PD. Based on adequate randomized controlled trials , ZNS is efficacious and safe as an adjunctive therapy in patients with PD . Additionally, the 2018 guideline has supported the use of ZNS for motor symptoms, especially for treating motor fluctuations . We review the clinical trials below; further details are summarized in Table 2.
Table 2. Clinical trials on zonisamide effectiveness in the treatment of PD.
