#9: If You Dont Experience The Same Symptoms As Your Relatives Who Are Diagnosed With Celiac Disease Then You Dont Have The Condition
This isn’t true. Celiac disease symptoms vary from person to person. This is also true among related people with celiac disease. You may be surprised that a younger sibling has symptoms, while other family members have none.
If you have celiac disease, your 1st and 2nd degree relatives are more likely to develop the condition. That’s why celiac disease specialists recommend that you get tested as soon as possible if you have a relative with the disorder.  The presence of the disease in a family is the first step towards a proactive diagnosis.
Because the symptoms and onset of the disease vary from individual to individual, it is recommended that you get tested as soon as a relative is diagnosed. Then undergo another screening every two to three years. It is not uncommon for a family member to test negative during one blood test, but then have a positive test result later. In such a case, the best option is to carry out a gene test for celiac disease.
�
Parkinson’s Disease May Manifest In The Gastrointestinal Tract May Begin In The Gut Long Before Any Motor Symptoms Show Up Caption:
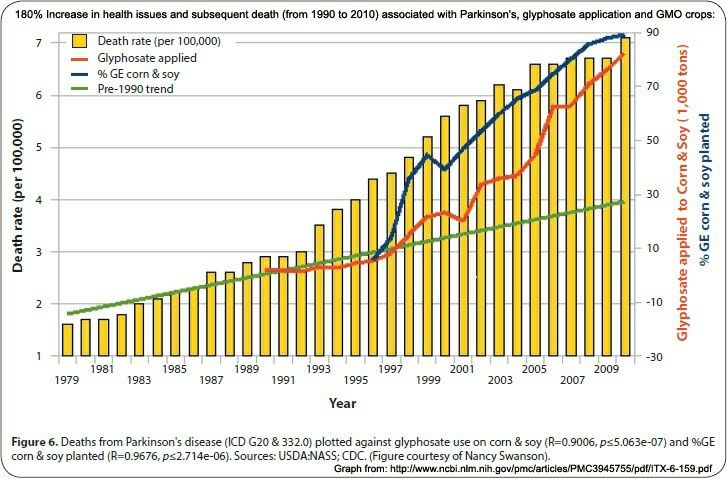
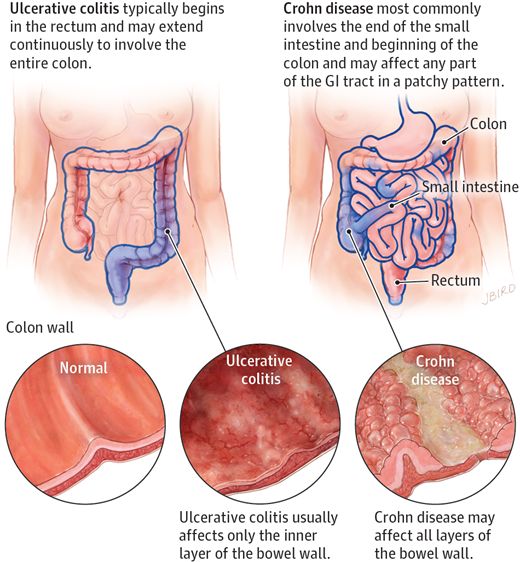
Celiac.com 12/02/2019 – Parkinson’s development can take many paths, with factors like genetics, aging, and environmental conditions all playing roles. Most people with Parkinson’s disease experience non-motor-symptoms, such as chronic constipation and/or impairment of gastrointestinal transit, long before the disease manifests clearly. Researcher Tomasza Brudek recently reviewed available medical literature for a possible link between Inflammatory Bowel Disease and Parkinson’s Disease.
Brudek is affiliated with both the Research Laboratory for Stereology and Neuroscience, Copenhagen University Hospital, Bispebjerg-Frederiksberg Hospital in Copenhagen, Denmark; and the Copenhagen Center for Translational Research, Copenhagen University Hospital, Bispebjerg and Frederiksberg Hospital in Copenhagen, Denmark.
Celiac.com Sponsor :Build-up of ?-synuclein protein in the form of Lewy bodies and Lewy neurites, and degeneration of substantia nigra dopamine neurons are classic clinical markers of Parkinson’s Disease.
Major features of Parkinson’s Disease include inflammatory responses manifested by glial reactions, T cell infiltration, and increased expression of inflammatory cytokines, along with other toxic mediators derived from activated glial cells.
Because gastrointestinal pathology can play such an important role in Parkinson’s Disease development, there’s good reason to believe that IBD and IBD treatments can influence Parkinson’s Disease risk.
When You Reintroduce Foods You Need To Be On The Lookout For Various Symptoms Which May Return
Your reactions may be delayed by as long as 72 hours. And, symptoms are not limited to the digestive system.
Pay close attention to the following symptoms which may indicate you are gluten intolerant.
And, if severe enough, warrants special follow up with your physician for additional testing.
- diarrhea and constipation
- Elana’s Pantry for amazing recipes
- Against All Grain for gluten and grain-free recipes and meal plans
Association Between Microscopic Colitis And Parkinson’s Disease In A Swedish Population
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Correspondence to: Xiaoying Kang, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, SE-171 77 Stockholm, Sweden; E-mail: xiaoying.kang@ki.se
Massachusetts General Hospital, Crohn’s and Colitis Center and Harvard Medical School, Boston, Massachusetts, USA
Division of Clinical Epidemiology, Department of Medicine Solna, Karolinska Institutet, Stockholm, Sweden
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
MRC Unit for Lifelong Health and Ageing, University College London, London, United Kingdom
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Department of Pediatrics, Örebro University Hospital, Örebro, Sweden
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Department of Clinical Neuroscience, Karolinska Institutet, Stockholm, Sweden
Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, Stockholm, Sweden
Correspondence to: Xiaoying Kang, Department of Medical Epidemiology and Biostatistics, Karolinska Institutet, SE-171 77 Stockholm, Sweden; E-mail: xiaoying.kang@ki.se
Massachusetts General Hospital, Crohn’s and Colitis Center and Harvard Medical School, Boston, Massachusetts, USA
https://doi.org/10.1002/mds.28594
Mayo Clinic Discovers Potential Link Between Celiac Disease And Cognitive Decline
- Date:
- Mayo Clinic
- Summary:
- Mayo Clinic researchers have uncovered a new link between celiac disease, a digestive condition triggered by consumption of gluten, and dementia or other forms of cognitive decline.
Mayo Clinic researchers have uncovered a new link between celiac disease, a digestive condition triggered by consumption of gluten, and dementia or other forms of cognitive decline. The investigators’ case series analysis — an examination of medical histories of a group of patients with a common problem — of 13 patients will be published in the October issue of Archives of Neurology.
“There has been very little known about this connection between celiac disease and cognitive decline until now,” says Keith Josephs, M.D., Mayo Clinic neurologist and study investigator. “This is the largest case series to date of patients demonstrating cognitive decline within two years of the onset of celiac disease symptom onset or worsening.”
Says Joseph Murray, M.D., Mayo Clinic gastroenterologist and study investigator, “There has been a fair amount written before about celiac disease and neurological issues like peripheral neuropathy or balance problems, but this degree of brain problem — the cognitive decline we’ve found here — has not been recognized before. I was not expecting there would be so many celiac disease patients with cognitive decline.”
The next step in the research will be to investigate the measure and nature of the connection between the two conditions.
#13: A Gluten Free Diet Is Great For Everyone Not Just People With Celiac Disease
The gluten-free diet movement is all the rage right now, and with good reason. Most people believe it will help them lose weight and keep it off. While this might have a grain of truth, going on a gluten-free diet without having celiac disease can come with a battery of risks.
Wheat, barley, oats, rye, and other gluten-rich grains are loaded with much-needed dietary fiber. This helps digestion and prevents complications like bloating and constipation. When you stay away from gluten foods, you are essentially removing fiber from your diet. That’s a big no-no.
Yes, a gluten-free diet may seem attractive to those who want to shed a few unwanted pounds. However, this diet can have a negative effect. Did you know that most gluten-free cookies, brownies, and other baked items are jam-packed with sugar, calories, and other undesirable ingredients?
A gluten-free diet can also translate into less mineral and vitamin intake. However you look at it, you should think twice before you go gluten-free if you don’t actually have celiac disease. Besides, when you finally return to consuming gluten after a long hiatus, the results might not be pleasant.
�
What Is Parkinsons Disease Symptoms Causes Diagnosis Treatment And Prevention
The causes and symptoms of Parkinson’s disease can vary from person to person. While there is no cure, there are medications and treatments to help manage the condition.
Parkinson’s disease is a movement disorder that happens when nerve cells in a certain part of the brain are no longer making the chemical dopamine.
The condition is also sometimes known as paralysis agitans or shaking palsy.
The Parkinson’s Foundation estimates that 60,000 Americans are diagnosed with Parkinson’s every year. However, the true number of people who develop the disease may be much higher.
Research Is Underway To Further Understand The Cardiac Effects Of Parkinsons
It is possible to image the sympathetic nervous system of the human heart by injecting a radioactive tracer, meta-iodo-benzyl-guanidine, . Development of this technique, known as MIBG cardiac imaging, holds much promise as a test to confirm the diagnosis of PD , to identify those who are at risk of developing PD in the future, and to distinguish PD from related disorders. MIBG cardiac imaging is still considered an experimental procedure for detection of PD and is not yet in use as a clinical tool for this purpose.
A recent research study was conducted in monkeys in which the destruction of the sympathetic nerves of the heart was chemically induced to mimic the changes that are seen in PD. The cardiac system was then imaged using a number of new-generation radioactive tracers, which bind to markers of inflammation and oxidative stress. This model system may help to shed light on the molecular changes that accompany the loss of the sympathetic nerves of the heart and can also be used to track the response of the cardiac system to therapeutic agents.
Is Paralysis An Accurate Term For Muscle Weakness During Parkinsons Disease
Paralysis is defined as the loss of muscle function of the body and is a curable condition. Stroke or injury such as spinal cord injury is considered as common and major causes of Parkinson’s disease. Attack of paralysis may also occur in cases of cerebral palsy, post-polio syndrome, brain injury, etc.
Brain Stimulation Therapies for Mental Illnesses
In some cases, paralysis is a birth defect. Parkinson’s attack is not a paralysis attack but because the symptoms for both are similar, people often cannot distinguish between the two.
Patients of Parkinson’s disease also suffer from muscle weakness but it is not justified to categorize this muscle weakness as paralysis. In 1962, researcher Denny-Brown explained the difference between the two conditions. He stated that paralysis agitans occur with tremors and arteriosclerotic Parkinsonism is characterized by muscle rigidity and slowness of movement.
Paralysis is in itself is a disorder but there are some chances that patients of Parkinson’s disease might suffer from it.
Although paralysis occurs due to some severe injury which results in cutting blood supply to the brain and Parkinson’s disease is the degeneration of neurons, but in some cases, the main cause i.e. dopamine loss can correlate these conditions. Some patients experience “internal tremors” which might be vaguely stated as Parkinson’s paralysis. If these tremors are severe and long-term then it is a serious concern among Parkinson’s patients.
Can Gluten Sensitivity Mimic Neurological Diseases For Example: Parkinson’s
My mom was diagnosed with Parkinson’s Disease in 2006. She has been told by her physicians that she has a very mild case of the disease. She has no tremor. When looking over the symptom checker page for gluten sensitivity, I checked quite a few symptoms my mom has been showing.
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
The Heart Of The Matter: Cardiovascular Effects Of Parkinsons Disease
It has long been understood that Parkinson’s disease does not just cause movement symptoms, but also causes a litany of non-motor symptoms with effects throughout the body. One of the organ systems that is affected is the cardiac system, encompassing the heart, as well as the major and minor blood vessels. I received this topic as a suggestion from a blog reader and we will be discussing this important issue today. Please feel free to .
#7: You Can Treat Celiac Disease With Drugs Or A Gluten Free Diet
As we’ve seen, this is not exactly true because there is no true cure for celiac disease. Yes, only a gluten-free regimen can help, but the condition is not treatable or curable in the long run. In fact, celiac disease is a life-long condition, which means you have to stick to a strict diet that’s free of gluten for the rest of your life.
You have probably heard that there are some drugs and medications that can help with celiac disease. These can only treat other conditions caused by your celiac disease, ranging from diarrhea to stomach complications.
Simply speaking, a gluten-free diet doesn’t cure celiac disease; it just helps you to manage it.
�
Neurological Complications Of Celiac Disease: A Brief Overview
Nowadays, it is widely accepted that the typical disease represents a small proportion of the so-called “CD iceberg,” because 5–6 fold more patients present with atypical or silent forms . Neurological manifestations may either precede or follow the disease, or be present at its onset . Therefore, a sensitive and specific diagnostic method able to recognize early disease process, progression, and complication would be desirable.
To date, both the causative factors and pathophysiological mechanisms of neurological involvement in CD remain a matter of debate. According to the literature, the nervous system may be one of the elective sites of gluten-mediated pathogenesis, including cross-reacting antibodies, immune-complex deposition, direct neurotoxicity, other immune-mediated factors, and deficiency of vitamin and other nutrients secondary to chronic malabsorption . Recently, studies using single photon emission computed tomography showed regional changes in cerebral perfusion, with regression after institution of a GFD . The authors argued that the cerebral hypoperfusion might be related to intestinal hyperemia from immune-mediated or endothelial damage due to immune-complex deposition likely involving antibodies against gliadin . Alternatively, cortical brain hypoperfusion could reflect focal vasculitis secondary to perivascular inflammation .
Celiac Disease Might Hold The Clue To How Other Diseases Work
Photos by Lloyd Fox.
In his small office at the Johns Hopkins Bloomberg School of Public Health in Baltimore, Noel Rose, M.D., sits surrounded by stacks of books and papers—his groundbreaking lab research and the several textbooks he’s edited on autoimmune diseases.
Rose, 87, known nationally as the “father of autoimmune disease,” is a giant in the field. But as director of Hopkins’ Autoimmune Disease Research Center, he has other work he takes just as seriously: answering calls for help from patients.
For decades, he has gotten letters, emails and phone calls from people around the country with autoimmune problems like celiac disease. Many have been ill for several years and visited multiple physicians without getting any answers. Instead, because the symptoms can be vague, these patients are often labeled chronic complainers.
“They want desperately to have some idea of what is wrong with them,” Rose says.
Understanding The Neurologic Control Of The Cardiac System
Before we explore this issue, let’s first learn a bit about the autonomic nervous system and about the cardiac system’s place within it. The ANS is part of the peripheral nervous system, a network of nerves throughout the body. The ANS exerts control over functions that are not under conscious direction such as respiration, heart function, blood pressure, digestion, urination, sexual function, pupillary response, and much more. The ANS is further subdivided into the parasympathetic nervous system and the sympathetic nervous system. Both the parasympathetic and sympathetic nervous systems regulate most major organs. Often, they have opposite effects, with the sympathetic nervous system activating a system and the parasympathetic system calming it down.
One of the systems controlled by the ANS is cardiac regulation. Blood pressure sensors, known as baroreceptors, reside in the heart as well as in the carotid artery, the major artery in the neck. If the baroreceptors sense a change in the blood pressure, a signal is sent to particular areas in the brain. From there, the autonomic nervous system sends signals to the heart to control heart rate and cardiac output. Signals are also sent to the blood vessels to change the size of their diameter, thereby regulating blood pressure.
#10: Food Labeled As Gluten Free Doesnt Include Any Gluten
No, that’s not always true. It is very difficult to get rid of all gluten from food. Today, gluten can be detected using specialized tests that can measure the quantity of the protein down to 3ppm . More crucially, experts say that people with celiac sprue can tolerate gluten levels of up to 20 parts per million.
Sadly, labeling items “gluten-free� is voluntary for food manufacturers. Even if you find a food item labeled as such don’t take their word for it. It doesn’t even mean that the food has zero gluten in it. When a manufacturer labels food “gluten free� it means is that the food contains less than 20 parts per million of gluten. As such, if you are extremely sensitive to gluten, you might still experience mild to acute symptoms of celiac disease. Remember that food designated ‘gluten-free’ can still be contaminated with gluten during processing, packing or distribution. Our article on what to expect when you are living with celiac disease will help you know what makes certain foods great for a gluten-free diet.
�
Newly Diagnosed With Celiac Heres A Gluten Free Meal Plan
Here is a sample 3-day gluten-free meal plan to get you started. Feel free to mix and match. Adjust according to your tastes and preferences. Each of these meals is 100% gluten free and delicious!
Day 1:
Breakfast
½ cup cooked certified gluten-free oatmeal with sea salt, 2 TBS almond milk 1 tsp each of chia, pumpkin and sunflower seeds, drizzle of raw honey, and ½ cup of fresh fruit
Lunch
2-3 cups of salad with mixed greens, sprouts, red or green peppers, cucumbers, 5 oz. of cooked shrimp, ½ avocado, ½ cup of garbanzo beans.
Dressing: 2 tablespoons olive oil mixed with 1 teaspoon of apple cider vinegar and season with salt and pepper to taste
Dinner
5 oz. grilled bison burger patty with tomato and gluten-free condiment of your choice . Serve with unlimited roasted asparagus with olive oil and sea salt.
Baked sweet potato with Kerrygold butter and sea salt
Snack
½ apple sliced, with 2 TBS almond butter
Day 2:
Breakfast
2 scrambled pasture-raised eggs and 1 ounce of crumbled goat or feta cheese over 2 cups mixed greens with arugula, splash of apple cider vinegar and olive oil, sea salt and pepper to taste
Lunch
Soup – Kettle & Fire beef bone broth blended with leftover baked sweet potato .
Serve with small side salad with avocado slices, lemon wedge and olive oil
Dinner
5 oz. of broiled wild-caught salmon with unlimited steamed green beans with Kerrygold butter.
Serve with ½ cup of cooked quinoa.
Snack
Day 3:
Breakfast
Serve with Applegate organic chicken sausage
Lunch
Dinner
How To Prevent Parkinsons Disease With Diet And Lifestyle
The number of people diagnosed with Parkinson’s disease and living with this condition is on the rise, with researchers estimating that over 1 million Americans will have this devastating illness by 2020.
Unfortunately, the conventional treatments available for Parkinson’s disease are limited to surgical interventions and medications that come with numerous side effects. But a growing body of research indicates that there are many modifiable risk factors associated with the condition, providing us with clues as to what measures we can take to prevent the onset of the disease. Read on to learn how to prevent Parkinson’s disease by using evidence-based dietary and lifestyle interventions.
Scientists Link Immune Cells To Parkinson’s Disease Onset
- Date:
- La Jolla Institute for Immunology
- Summary:
- A new study adds increasing evidence that Parkinson’s disease is partly an autoimmune disease. In fact, the researchers report that signs of autoimmunity can appear in Parkinson’s disease patients years before their official diagnosis.
A new study co-led by scientists at the La Jolla Institute for Immunology adds increasing evidence that Parkinson’s disease is partly an autoimmune disease. In fact, the researchers report that signs of autoimmunity can appear in Parkinson’s disease patients years before their official diagnosis.
The research could make it possible to someday detect Parkinson’s disease before the onset of debilitating motor symptoms — and potentially intervene with therapies to slow the disease progression.
The study, published in the April 20, 2020, issue of Nature Communications, was co-led by LJI professor Alessandro Sette, Dr. Biol. Sci, and Professor David Sulzer, Ph.D., of the Columbia University Medical Center.
Scientists have long known that clumps of a damaged protein called alpha-synuclein build up in the dopamine-producing brain cells of patients with Parkinson’s disease. These clumps eventually lead to cell death, causing motor symptoms and cognitive decline.
The researchers hope to study more Parkinson’s patients and follow them over longer time periods to better understand how T cell reactivity changes as the disease progresses.
Story Source:
Early Signs You Have Celiac Disease According To Experts

One of the most widespread health problems in the U.S. are autoimmune disorders, which the American Autoimmune Related Diseases Association estimated affects close to 50 million Americans. To make matters complicated, there are over 100 types of autoimmune disorders that someone can be diagnosed with that all affect different areas of the body, and, that are all accompanied by unique symptoms. Among those, one of the most common kinds of autoimmune diseases is celiac disease, which the Celiac Disease Foundation reported affects at least one percent of people in the U.S.
Celiac disease is triggered by ingesting gluten food products — such as wheat, barley, and rye — and the disorder is so much more than simply having a slight sensitivity or upset stomach. According to Healthline, people with celiac disease can experience painful digestive issues, bloating, nausea, depression, and even iron-deficiency anemia. What’s more, The Mayo Clinic reported in 2012 that if celiac disease goes undetected, or is left untreated, “a range of problems may develop as a result of the body’s reaction to gluten — from skin rashes and lactose intolerance to infertility, bone weakness, and nerve damage.”
Living Gluten Free For Your Best Health With Hashimotos
So, you’ve decided to go gluten free for good?
You have Hashimoto’s and you know you are not making the progress you want to see taking medication alone.
You get the science I have explained here in this article.
You recognize the connection between gluten and your thyroid.
But, if, even after reading the above, you still feel stuck on the actual implementation of a gluten free meal plan – you are normal.
It’s not easy to commit to giving up gluten for the rest of your life.
We love our pizza, cakes, cookies, baked goods, beer, etc.
Even when I knew that gluten was my #1 food problem, it took me a good FIVE MONTHS to quit it altogether.
But, you know how I finally figured it out?
I never wanted to feel sick again.
And, after the first few weeks of GLUTEN ZERO, I said to myself “So this is how normal people feel?!”
It was wonderful!
That feeling was better than any piece of pizza or plate of pasta or slice of bread.
Feeling good for the first time in my life was a slice of heaven.
And, it still is.
Researchers Confirm Celiac Disease Can Damage The Brain
People living with celiac disease have a higher risk of neurological damage according to a new study from the University of Sheffield.
The study found that the brains of people living with CD showed evidence of damage to brain matter and cognitive deficit in the form of slowed reaction times.
Alongside this neurological damage, this group of people also had indications of worsened mental health compared to matched healthy control subjects.
The researchers hope the study will help clinicians to tailor their care to CD patients who may present even the mildest cognitive changes; providing reassurance and motivation for the maintenance of a strict gluten-free diet , and eradicate any skepticism in the clinical community.
People living with CD have increased sensitivity to gluten and are advised to follow a strict GFD, the only current method of minimizing exposure and the immediate risk of damage to their digestive system.
As a result of repeated or uncontrolled exposure, this autoimmune response to gluten can also lead to serious complications and longer term health problems for people living with CD. These include a higher risk of coronary artery disease, small bowel cancers, deterioration of bone health and damage to the nervous system.
There has long been debate amongst neurologists and gastroenterologists about whether this neurological damage is caused as a result of people having CD, with previous studies finding conflicting evidence.
Explore further
The Missing Link Between Celiac Disease And Hashimotos
Celiac Disease and Hashimoto’s share a common genetic link – the HLA-DQ2 allele.
So, someone who has the HLA-DQ2 allele is at risk to develop Celiac disease.
In order for Celiac disease to fully develop, other environmental triggers need to be present .
When leaky gut co-occurs with gluten exposure and genetic predisposition, the perfect storm is created for Celiac disease.
This largely holds true for the development of Hashimoto’s. They are like two sides of the same coin.
In a nutshell…
- You need the genetic predisposition .
- You need gluten, which is sticky and invasive and increases zonulin production leading to leaky gut.
- You need the immune system to kick in.
- Your immune system is so overworked the immune cells lose self tolerance.
- Your immune system starts attacking your own tissue.
Neurophysiology Of The Celiac Brain: Disentangling Gut
- 1Spinal Unit, Ospedale Cannizzaro, Catania, Italy
- 2Centro Neurolesi Bonino Pulejo , Messina, Italy
- 3Department of Neurology IC, Oasi Maria SS , Troina, Italy
- 4Department of Surgery and Medical-Surgical Specialties, University of Catania, Catania, Italy
- 5Section of Neurosciences, Department of Medical and Surgical Sciences and Advanced Technology, University of Catania, Catania, Italy
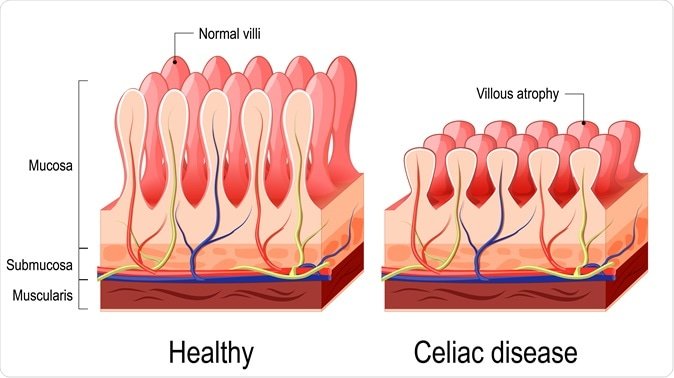
#8: Celiac Disease Is Only A Gastrointestinal Disease
Yes, gastrointestinal symptoms like diarrhea, bloating and stomach pain are very common with celiac disease. These apparent symptoms can make you believe that the disease only affects the GI.
Although the digestive system bears the brunt of the problems, celiac disease can adversely affect a host of organs and body systems. For instance, severe inflammation can damage the bile duct, leading to pancreatic malfunction, liver problems, and kidney disease.
Don’t forget that most autoimmune diseases go hand-in-hand, so celiac disease usually occurs in conjunction with thyroid disorders, type 1 diabetes, multiple sclerosis, and so forth. One study published by researchers at the University of Padua in Italy showed that celiac children are 4.5x and 2.5x likely to develop autoimmune thyroid disorder and type 1 diabetes respectively.
Plus, celiac disease can lead to an array of other non-GI symptoms, such as itchy skin rashes, drastic weight loss, joint pain, migraines, anemia, and fatigue. Some people may suffer from infertility and irregular menstrual periods, or experience pregnancy complications, including preterm delivery and miscarriage.
�
Table 1 Neurologic Complications Identified In Gluten
|
Conditions |
|
Pseudotumor cerebri |
Cerebellar ataxia. Cerebellar ataxia is the most commonly reported neurologic complication of gluten-related disorder. Up to 68% of patients with idiopathic ataxias test positive for gliadin, transglutaminase, or endomysial antibodies, suggesting that gluten-related disorder plays an important role in the pathophysiology of ataxia . In 2 other series of idiopathic ataxia, the frequency of antigliadin or antiendomysium antibodies was lower . In observational studies, patients often present with ataxia even in the absence of gastrointestinal symptoms, with up to two thirds of these patients demonstrating normal small intestinal mucosa .
Patients between the ages of 18 and 75 years have been observed to experience gluten ataxia, with a mean age of onset in the early 50s. Although the ataxia is progressive and primarily affects stance and gait, patients may also exhibit limb ataxia, dysarthria, and nystagmus. As discussed in more detail in the following section, about 60% of patients with gluten ataxia also have peripheral neuropathy. Rarer coincident symptoms include myoclonus, palatal tremor, opsoclonus, chorea, and cognitive impairment . In cases associated with dementia, celiac disease has been linked to hereditary forms of spinocerebellar ataxia .
The forms of peripheral neuropathy exhibited by patients with ataxia vary and include axonal, mononeuritis multiplex, sensorimotor polyneuropathy , motor, sensory, and small-fiber .
Celiac Disease Statistics And The Link To Hashimotos
- The increased risk is true despite treatment with a gluten-free diet or thyroid medications and may be due to overlapping genetic predispositions.
- In a recent study by Alessio Fasano, MD, a recognized Celiac disease expert, one half of the people newly diagnosed with Celiac disease also had Hashimoto’s thyroid disease.
Additionally, a 2008 study by Naiyer et al explored the connection between Hashimoto’s and Celiac disease. This is what they discovered:
- Anti-tissue transglutaminase antibodies are present in patients with active Celiac disease.
- These antibodies will decrease and eventually disappear on a gluten-free diet.
- These anti-tTG antibodies bind and react to thyroid tissue as well, which may contribute to Hashimoto’s development.
- Antithyroid antibodies were observed more often in patients with Celiac disease than in either controls or patients with another autoimmune condition .
This basically means, if you are suffering with symptoms of Celiac disease, but undiagnosed for any length of time, your risk for developing Hashimoto’s is imminent.
It was a few years later that I was found to have anti-tTG antibodies and finally received a diagnosis for Celiac disease.
What Is Parkinsonism Is It Different From Parkinsons

Parkinson’s disease is the most common cause of parkinsonism, a category of neurological diseases that cause slowed movement.
No quick or easy diagnostic tests exist for Parkinson’s disease, so a patient may receive an initial diagnosis of parkinsonism without a more specific condition being confirmed.
Classic Parkinson’s disease — referred to as idiopathic because it has no known cause — is the most common and most treatable parkinsonism.
About 15 percent of people with parkinsonism have atypical variants, which are also known as Parkinson’s plus syndromes.
