Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
The exact cause of Parkinson’s disease is unknown, but researchers think it’s a combination of environmental factors, genetics and the presence of a protein in the nerve cells called “lewy bodies.” There is no cure for Parkinson’s disease, but there are treatments that can help improve quality of life and manage the symptoms of the disease.
MORE: This woman proves you can live a good life with Parkinson’s disease.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Autonomic Dysfunction: Implications For The Pathophysiology And Treatment Of Parkinson Disease
Both pathologic and physiologic studies demonstrate widespread involvement of the autonomic nervous system in PD . Several excellent reviews discuss treatment of autonomic symptoms which is currently limited and symptom-based. The American Academy of Neurology’s practice parameter for non-motor features in PD recommends only two medications for autonomic dysfunction: Sildenafil for erectile dysfunction and polyethylene glycol for constipation. This highlights the lack of evidence for specific treatments and the need for research in this area. Understanding PD pathophysiology of autonomic dysfunction would allow more mechanistically based treatments to be developed.
The Effect Of Dopaminergic Medications On Autonomic Measures In Parkinson Disease
Human autopsies reveal dopamine receptors to be in the nucleus tractus solitarius and the dorsal motor nucleus of the vagus, suggesting that dopaminergic signals regulate visceral autonomic function. Epidemiologic studies observe higher doses of dopaminergic medications and higher disease severity to be related to more autonomic problems, independent of one another. Levodopa can be further metabolized to small amounts of epinephrine and norepinephrine which may lead to sympathomimetic effects. Some studies have found a positive correlation of levodopa and norepinephrine concentrations, while others have not. Constipation in PD may improve with dopaminergic treatment. Although treatment with levodopa has been thought to cause OH, this has not been consistently supported in physiological studies.
Distinguishing Parkinson Disease From Other Parkinsonian And Lewy Body Syndromes
Pathologically, PD is categorized as a synucleinopathy along with dementia with Lewy Bodies, pure autonomic failure and multiple system atrophy . The first three of these disorders are all Lewy body disorders given their Lewy-related pathology. MSA is not a Lewy body disorder as it is characterized by glial cytoplasmic inclusions. Given the pathological overlap of Lewy body disorders, some have suggested that PD, dementia with Lewy bodies and pure autonomic failure may be considered Lewy body synucleinopathies with distinct but overlapping motor, cognitive and autonomic features. Clinical manifestations depend on the predominant sites of Lewy body formation and neuronal loss. Such a proposition is far from certain, however, given that the biological significance of Lewy-related pathology and its impact on neurodegeneration remains unclear. It is possible Lewy-related pathology interferes with normal cell function or that they are the result of a protective response to cytotoxic proteins.
The clinical and pathological overlap of Lewy body disorders is still being resolved and whether PD falls within the spectrum of Lewy body disorders or is truly distinct from pure autonomic failure or dementia with Lewy bodies remains to be seen.
Research Is Underway To Further Understand The Cardiac Effects Of Parkinsons
It is possible to image the sympathetic nervous system of the human heart by injecting a radioactive tracer, meta-iodo-benzyl-guanidine, . Development of this technique, known as MIBG cardiac imaging, holds much promise as a test to confirm the diagnosis of PD , to identify those who are at risk of developing PD in the future, and to distinguish PD from related disorders. MIBG cardiac imaging is still considered an experimental procedure for detection of PD and is not yet in use as a clinical tool for this purpose.
A recent research study was conducted in monkeys in which the destruction of the sympathetic nerves of the heart was chemically induced to mimic the changes that are seen in PD. The cardiac system was then imaged using a number of new-generation radioactive tracers, which bind to markers of inflammation and oxidative stress. This model system may help to shed light on the molecular changes that accompany the loss of the sympathetic nerves of the heart and can also be used to track the response of the cardiac system to therapeutic agents.
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
The Heart Of The Matter: Cardiovascular Effects Of Parkinsons Disease
It has long been understood that Parkinson’s disease does not just cause movement symptoms, but also causes a litany of non-motor symptoms with effects throughout the body. One of the organ systems that is affected is the cardiac system, encompassing the heart, as well as the major and minor blood vessels. I received this topic as a suggestion from a blog reader and we will be discussing this important issue today. Please feel free to .
Parkinson Disease Neuropathology In The Autonomic Nervous System
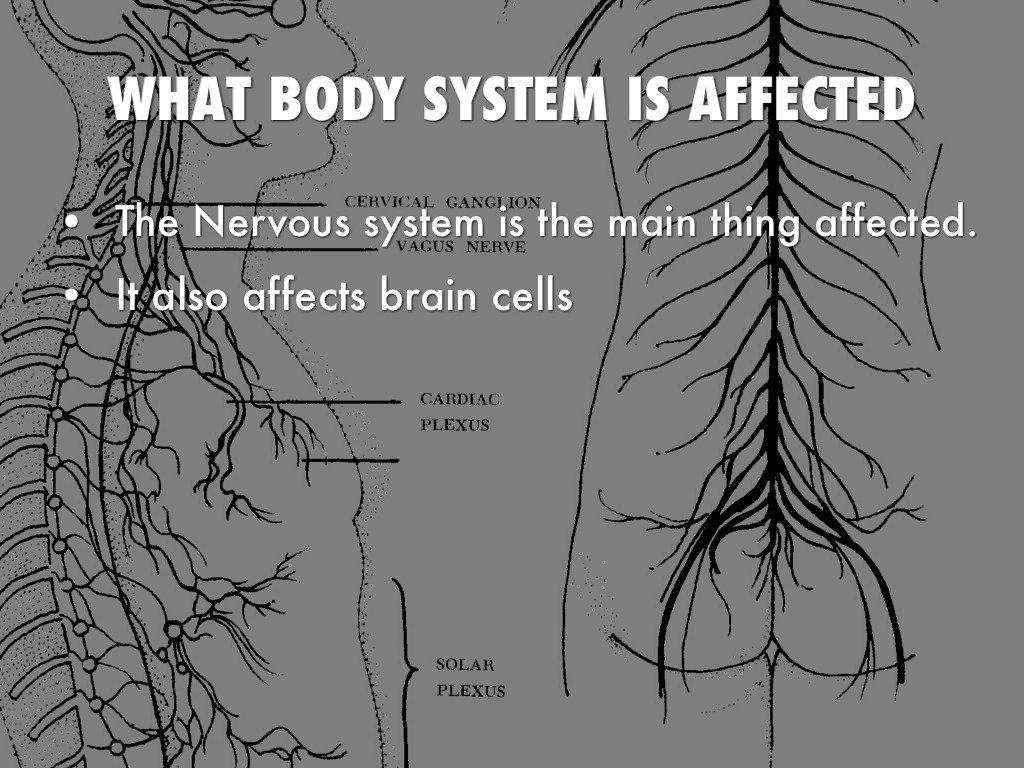
Anatomically, the autonomic nervous system can be divided into central autonomic networks, sympathetic pathways, parasympathetic pathways and the enteric nervous system. Central autonomic networks integrate autonomic function, linking the neocortex, diencephalon and brainstem. At its core is the nucleus tractus solitarius which integrates somatic and autonomic nervous systems and maintains homeostasis with projections to the hypothalamus, limbic structures and descending autonomic tracts. PD pathology has been characterized by intraneuronal inclusions which contain ?-synuclein known as Lewy neurites or Lewy bodies . ?-synuclein is a presynaptic protein thought to maintain synaptic integrity and be involved with regulation of dopamine synthesis. Although often seen in the absence of neuronal loss, evidence suggests that ?-synuclein aggregation is a precursor to neurodegeneration. PD pathology has been observed in a chain of neurons forming autonomic pathways including: the hypothalamus, preganglionic parasympathetic projection neurons in the dorsal motor nucleus of the vagus and pre-ganglionic and post-ganglionic sympathetic projection neurons . PD pathology has also been found in several end-organs including the submandibular gland, lower esophagus, duodenum, pancreas, bronchus, larynx, epicardium, adrenal medulla, parathyroid and ovary. Figure 1 illustrates most areas within autonomic pathways where PD pathology has been found.
What Body Systems And Organs Are Affected By Parkinson Disease
5/5Parkinson’s diseasebodyorgan systemsaffectedsystem
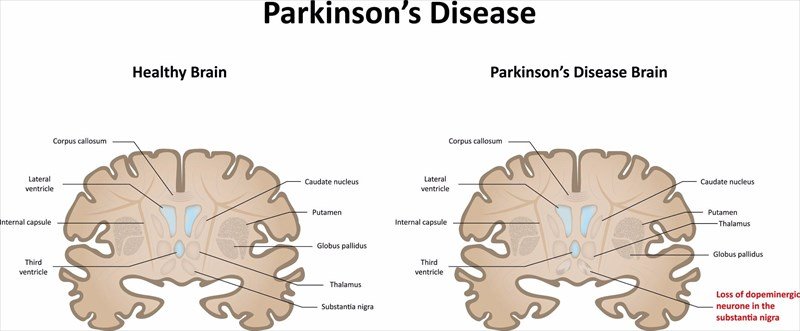
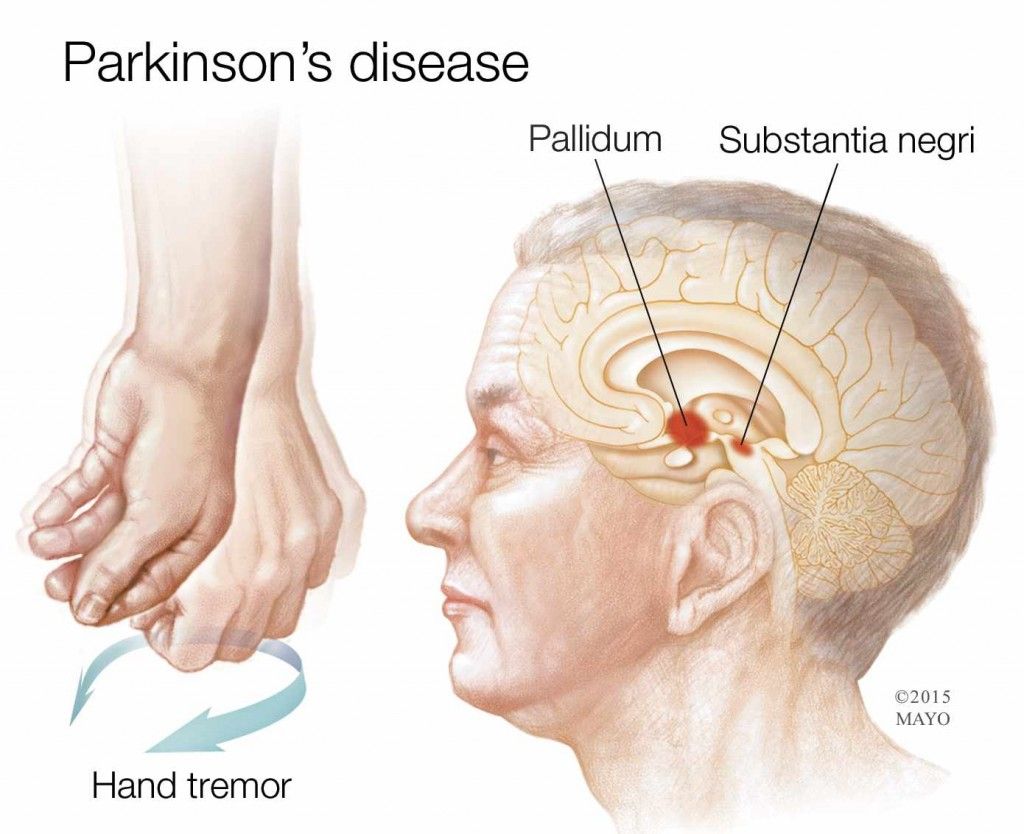
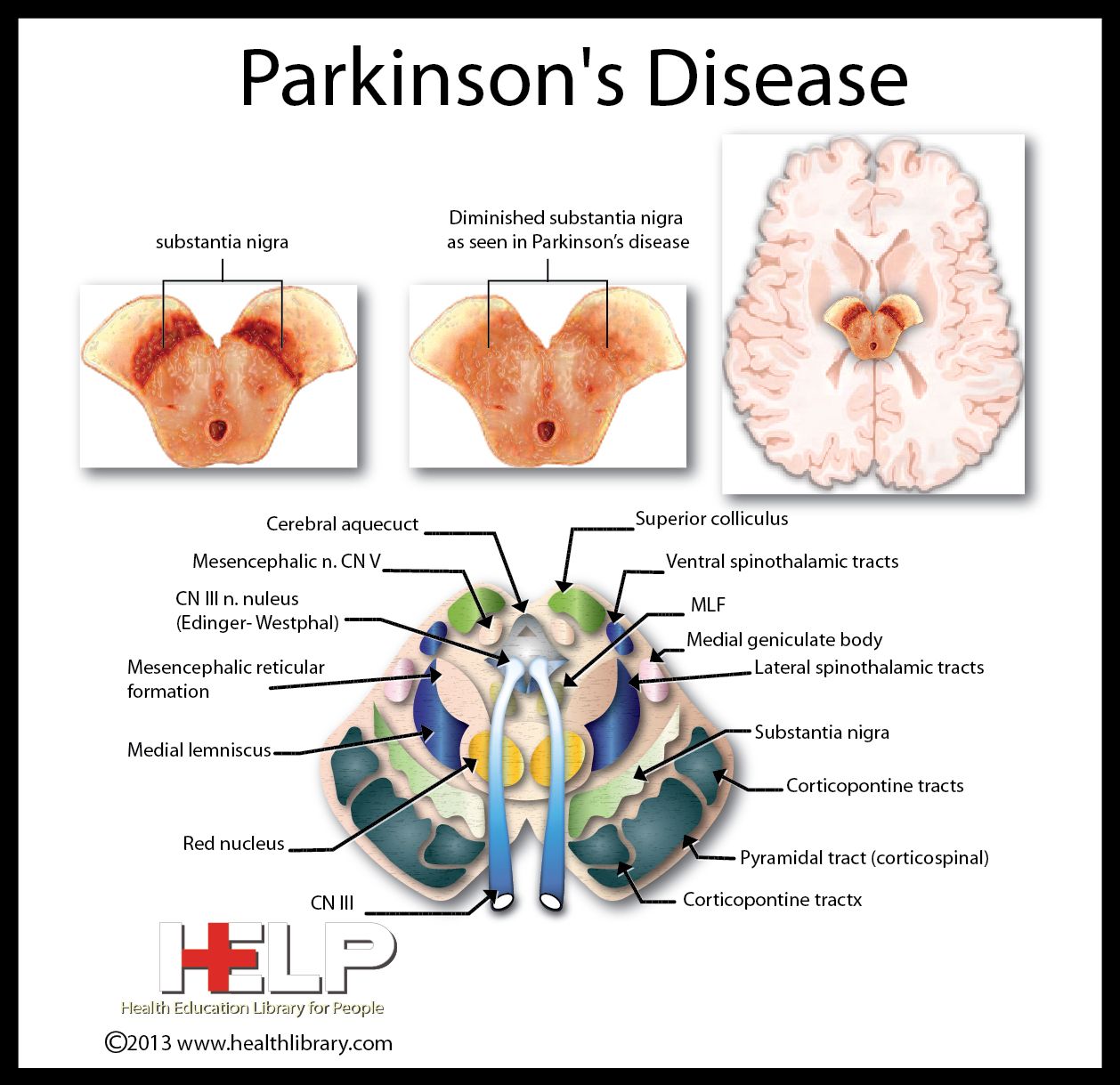
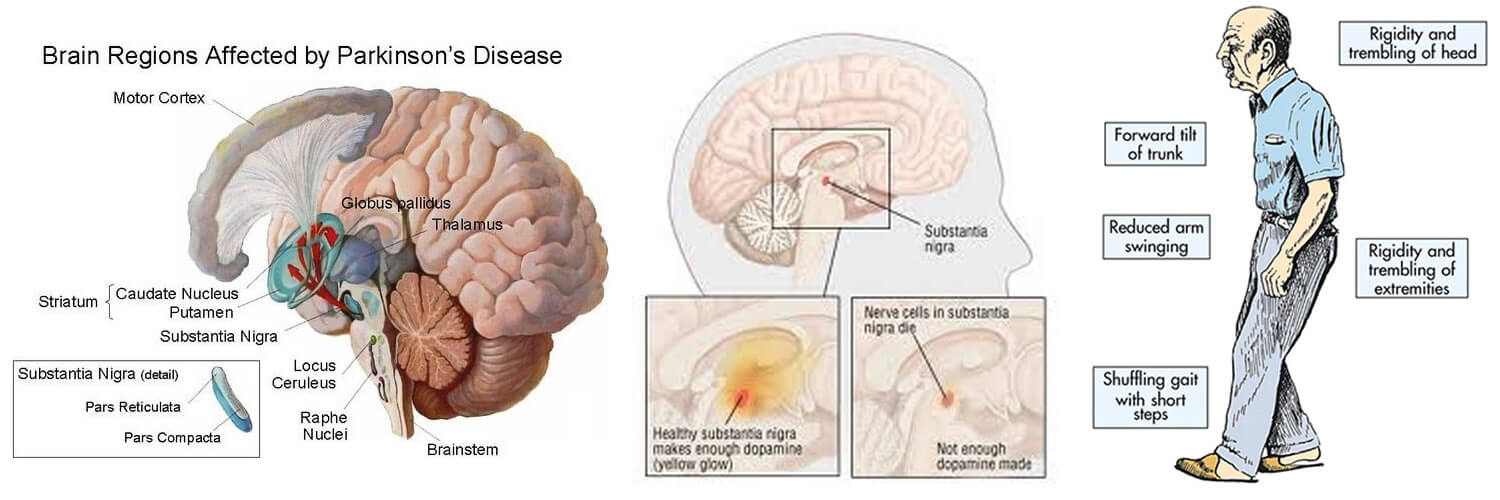
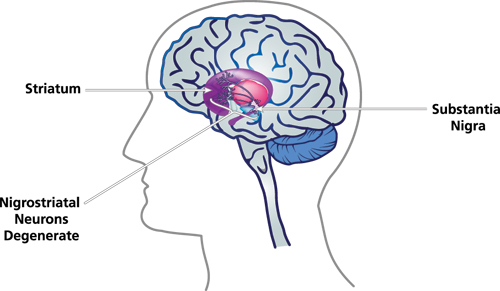
Parkinson’s disease is a degenerative, progressive disorder that affects nerve cells in deep parts of the brain called the basal ganglia and the substantia nigra. Nerve cells in the substantia nigra produce the neurotransmitter dopamine and are responsible for relaying messages that plan and control body movement.
Also, what foods should Parkinson’s patients avoid? Eat too many sugary foods and drinks as these can negatively impact your immune system. Opt for naturally sweetened food and reduce your sugar intake to manage Parkinson’s symptoms. Eat too much protein. Consuming lots of beef, fish, or cheese may affect the effectiveness of certain Parkinson’s medications.
Just so, how does Parkinson disease affect the muscular system?
Unlike some neurological conditions which affect muscle tone, the rigidity in Parkinson’s disease affects flexor and extensor muscles equally. Rigidity in Parkinson’s disease can prevent you from moving easily, and this lack of easy movement can lead to more stiffness in a downward cycle.
How does Parkinson start?
PD starts with the brain cells, called neurons, which control movement. Neurons produce a substance called dopamine. PD sets in when the neurons die and the levels of dopamine in the brain decrease. Early signs of Parkinson’s disease can be easy to miss, especially if they occur sporadically.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Parkinsons Disease Effects On The Body Tremor Motor Symptoms Emma-Marie Smith
The Parkinson’s tremor affects 80% of people with Parkinson’s disease. Sadly, it is also one of the more difficult symptoms to treat. The PD tremor is characterized by a quivering movement or shakes that occurs at rest, but it presents differently in everyone. People in the early stages of PD usually experience tremors starting in one hand, leg or foot, but the tremor may eventually progress to both sides of the body. Find out the effects of Parkinson’s tremor on the body and explore ways to treat motor symptoms of the disease.
Understanding The Neurologic Control Of The Cardiac System
Before we explore this issue, let’s first learn a bit about the autonomic nervous system and about the cardiac system’s place within it. The ANS is part of the peripheral nervous system, a network of nerves throughout the body. The ANS exerts control over functions that are not under conscious direction such as respiration, heart function, blood pressure, digestion, urination, sexual function, pupillary response, and much more. The ANS is further subdivided into the parasympathetic nervous system and the sympathetic nervous system. Both the parasympathetic and sympathetic nervous systems regulate most major organs. Often, they have opposite effects, with the sympathetic nervous system activating a system and the parasympathetic system calming it down.
One of the systems controlled by the ANS is cardiac regulation. Blood pressure sensors, known as baroreceptors, reside in the heart as well as in the carotid artery, the major artery in the neck. If the baroreceptors sense a change in the blood pressure, a signal is sent to particular areas in the brain. From there, the autonomic nervous system sends signals to the heart to control heart rate and cardiac output. Signals are also sent to the blood vessels to change the size of their diameter, thereby regulating blood pressure.
Treatment For The Motor Symptoms Of Parkinson’s Disease
There are many ways to deal with Parkinson’s disease motor symptoms, including medications, occupational therapy and lifestyle adjustments. You may find that tremors make you more susceptible to accidents – such as tripping, falling or spilling hot liquids – so you must take care and ask for the help and support you need.
In Parkinson’s disease, freezing of gait is characterized by hesitation before stepping forward, or a feeling like your feet have frozen to the floor. Frozen gait usually only lasts for a step or two, but you will need to be careful when crossing busy streets and try to minimize your risk of falling wherever possible.
You can talk to your doctor about medications to try, as well your surgical and homeopathic options. However, there is no cure for Parkinson’s disease and no way to stop the symptoms entirely, but scientists are working to change that.
APA ReferenceSmith, E. . Parkinson’s Disease Effects on the Body? Tremor, Motor Symptoms, HealthyPlace. Retrieved on 2021, August 11 from https://www.healthyplace.com/parkinsons-disease/symptoms/parkinsons-disease-effects-on-the-body-tremor-motor-symptoms
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
How Does Neuron Dysfunction Affect Parkinsons Patients
Parkinson’s disease is a disorder that affects the brain and the nervous system of its sufferers.
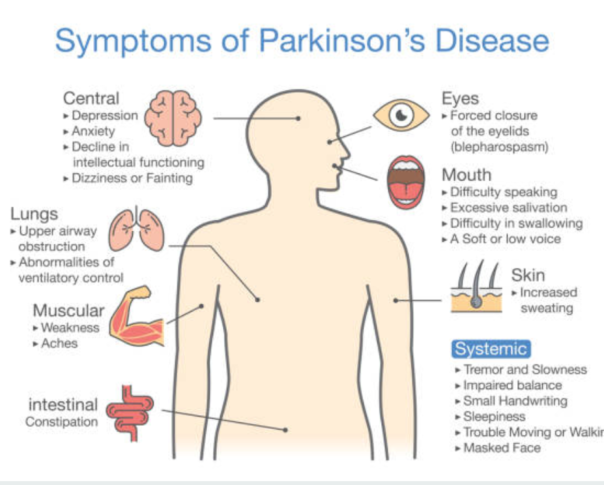
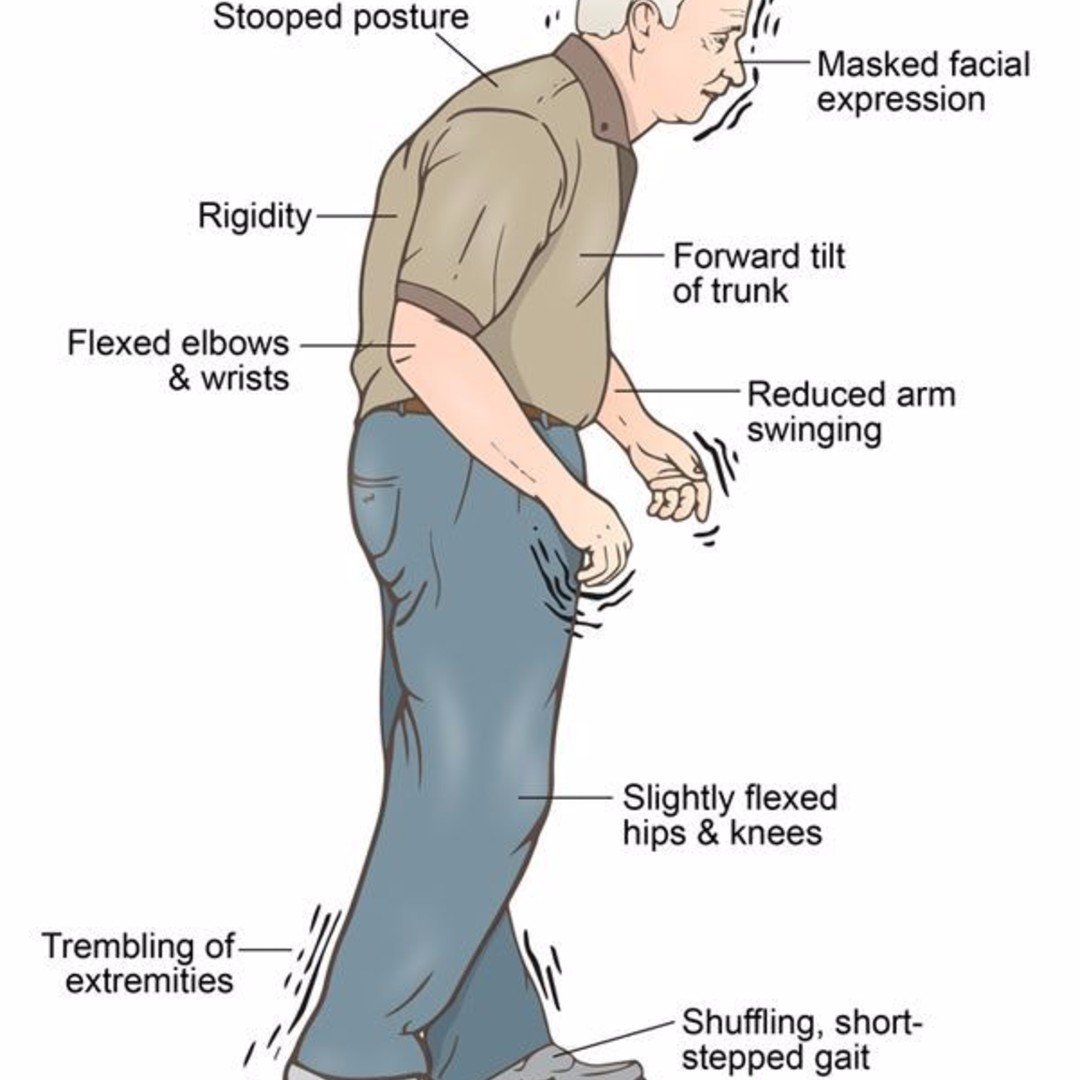
Over time, neurons in the regions of the brain that control movement degenerate, leading to a loss of motor control and a host of primary and secondary symptoms. People with Parkinson’s disease often experience tremors and shaking, a slow, shuffling walk, and an occasional sensation of being frozen in place, incapable of voluntary movement. Parkinson’s sufferers also routinely experience other, more subtle, motor symptoms, such as very small, cramped handwriting, a rigid, mask-like facial expression, and difficulty controlling the tone and volume of their voice.
These symptoms are caused by dysfunction in the neurons that control movement. These densely packed nerve endings in the brain and throughout the body send and receive chemical signals relating to movement. In Parkinson’s, these neurons lose their ability to produce dopamine, a chemical messenger essential to transmitting these signals. This leads to random firing of the neurons and compromised movement. Eventually, Parkinson’s often effects other body systems, causing digestive, urinary, skin, and psychiatric problems.
Edison Home Health Care is happy to advise and assist you or any loved one seeking a home attendant for Parkinson’s related issues. Give us a call at 888-311-1142, or fill out a contact form and we will respond shortly.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Tips For Dealing With Parkinsons Disease Tremor
Because the Parkinson’s tremor appears at rest, many people find that exercise helps control their symptoms. Here are some tips to help you limit the effects of Parkinson’s tremor:
- If the tremor presents in your jaw, try chewing gum to keep the area moving.
- Foot tremors present when you are sitting or lying down, and they always disappear when you stand up. Therefore you should try to avoid long periods of inactivity, as staying still may worsen your tremor symptoms.
- Finger twitching and the “pill roll” tremor refer to tremors in the thumb and fingers. You may find hand exercises such as rotating your hands, moving your fingers or squeezing a stress ball will help ease your symptoms. If you feel self-conscious about your tremor, you can always hide your hands in your pockets or place them under a table until the shaking subsides.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
How Parkinsons Disease Affects The Human Body
More than one million people live with Parkinson’s disease in the U.S., but no two experiences are the same. Parkinson’s affects individuals in vastly different ways: for some, Parkinson’s may first show up as slight hand tremors, and in others, it might appear as an unusual level of stiffness. For one person it may progress slowly, and in someone else, it may spread frighteningly fast.
There are some consistencies in how the disease works, however, and understanding these similarities can help prepare for what to expect if you or a loved one is diagnosed with Parkinson’s disease. From how it starts to how it progresses through its five stages, here are some of the ways Parkinson’s affects the human body.
What Are The Symptoms Of Parkinson’s Disease
The symptoms of Parkinson’s disease include tremors or trembling ; difficulty maintaining balance and coordination; trouble standing or walking; stiffness; and general slowness.
Over time, a person with Parkinson’s may have trouble smiling, talking, or swallowing. Their faces may appear flat and without expression, but people with Parkinson’s continue to have feelings — even though their faces don’t always show it. Sometimes people with the disease can have trouble with thinking and remembering too.
Because of problems with balance, some people with Parkinson’s fall down a lot, which can result in broken bones. Some people with Parkinson’s may also feel sad or depressed and lose interest in the things they used to do.
The symptoms of Parkinson’s disease appear gradually and get worse over time. But because Parkinson’s disease usually develops slowly, most people who have it can live a long and relatively healthy life.
How Does Parkinson Affect The Nervous System What Is Parkinson’s?Parkinson’s Effect On The Nervous System And Dopamine.The Two Types Of Parkinson’s Related To The Nervous Systemdistinct subtypesAutonomic Nervous System And Parkinson’s
Autonomic dysfunctionHow To Keep Your Nervous System Healthy?healthyHere are some important recommendations:
How Does Parkinsons Disease Affect The Body
Recognising the signs
A combination of signs can help a doctor make an early diagnosis. If Parkinson’s disease is diagnosed early, the chances of being able to treat and manage the condition are greater. Individual signs may not be an indication of Parkinson’s disease. Some signs such as loss of smell could be caused by an infectious illness, or joint stiffness by conditions like arthritis.
Parkinson’s is most commonly diagnosed with a very physical examination and assessment of a person’s medical history. There are very specific markers for diagnosis which doctors use to assess for possible Parkinson’s disease. These markers have a lot to do with a combination of very specific signs and symptoms and if recognised early enough, can be better managed.
1. Primary motor symptoms
2. Secondary motor symptoms
Other motor symptoms include:
Some individuals may also experience the following:
- Hunched over / stooped posture – When standing, the body may begin to slouch or lean inwards, causing a hunched over appearance.
- Impaired gross motor coordination
- Impaired fine motor dexterity and motor coordination
- Difficulties with swallowing or chewing
- Cramping
- Production of excess saliva and drooling
- Sexual dysfunction
- Dystonia
- Akathisia
3. Non-motor symptoms
Symptoms that do not involve physical movement or coordination, and often precede motor problems, can include:
Symptoms are initially mild, even if they develop suddenly, and typically affect one side of the body at first.
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinson’s disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Decreased facial expressions: You may not smile or blink as often as the disease worsens; your face lacks expression.
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Innate Immunity In Pd: Microglia Activation
Microglial cells are the principal actors of innate immunity in the CNS responsible for the protection and restoration of neurons . They can be activated by various external or internal insults such as neuronal dysfunction, trauma or certain toxin. Also, a wide range of molecules including viral or bacterial proteins, ?-syn, cytokines and antibodies are able to induce the activation of microglia . Consequently, microglial cells produce different molecular mediators with chemotactic and immunomodulatory functions. One of them is tumor necrosis factor which in PD plays important roles contributing to the regulation of synaptic plasticity . PD brains are characterized by the presence of HLA-DR+ microglial cells and raised levels of CD68, an activation marker for microglia and macrophages, having a direct relation with ?-syn aggregations and the duration of disease . Moreover, an increased expression of MHC-II molecules in microglial cells has been observed in chronic neuroinflammation but not in the CNS of healthy subjects . Individuals with single nucleotide polymorphism at MCH-II locus are prone to develop PD, which indirectly proves the importance of adaptive immunity in these patients .
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
How Parkinson’s Affects The Nervous System
Parkinson’saffects nerveNerve
It has long been understood that Parkinson’s disease does not just cause movement symptoms, but also causes a litany of non-motor symptoms with effects throughout the body. One of the organ systems that is affected is the cardiac system, encompassing the heart, as well as the major and minor blood vessels.
Additionally, what are the changes to the brain caused by Parkinson’s disease? The brain changes caused by Parkinson’s disease begin in a region that plays a key role in movement, leading to early symptoms that include tremors and shakiness, muscle stiffness, a shuffling step, stooped posture, difficulty initiating movement and lack of facial expression.
Regarding this, does Parkinson’s affect your spine?
Low back pain and back of the neck pain are probably the most common pain conditions in PD. The reason Parkinson’s Disease patients have so many problems with their low back and their neck is their posture. Because of the stooped posture, the muscles in the lower back have to pull much harder to keep the spine upright.
Does stress cause Parkinson’s?
Research suggests that stressful life events may increase the risk of Parkinson’s disease. In addition, animal studies indicate that stress damages dopamine cells, resulting in more severe parkinsonian symptoms. In humans, acute stress can worsen motor symptoms, including bradykinesia, freezing, and tremor.
