Parkinsons Disease Late Stages: What Will Happen To Me
With advanced Parkinsons disease, stage 5 life expectancy can be months or years depending on how your condition presents. You are likely to need round-the-clock care at this stage, and you may not be able to move around independently. Patients with late-stage Parkinsons disease are more susceptible to pneumonia, sepsis, pyelonephritis and decubitus ulcers. Late-stage Parkinsons also leads to Parkinsons disease dementia in 50% of cases. For all of these reasons, many late-stage Parkinsons patients are cared for by loved ones or in a hospice.
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this w
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
Stage 5 The Most Advanced Stage Of Parkinsons Disease
This is the late stage of Parkinsons disease where the patient completely depends on others for functioning. The patient finds it difficult to move and need a . This stage is also accompanied by behavioral symptoms such as delusions and hallucinations. Moreover, the patient becomes sensitive to infections such as pneumonia.
One main limitation of the Hoehn and Yahr scale is that it entirely relies on motor symptoms and doesnt take into account the cognitive or other non-motor symptoms. Due to this, some physicians may prefer to use an alternative method known as the Unified Parkinsons disease Rating Scale. This scale is more inclusive as it covers both the motor symptoms and the non-motor symptoms, including mental functions, mood, behavior.
Disclaimer: The information shared here should not be taken as medical advice. The opinions presented here are not intended to treat any health conditions. For your specific medical problem, consult with your health care provider.
Neuropsychiatric Symptoms And Dementia
Visual hallucinations and illusions are common in PD and reportedly occur in a third to 40% of patients . Although virtually all anti-parkinsonian medications have been reported to induce hallucinations and psychosis, visual hallucinations have also been reported to occur prior to drug treatment . Neuropathological changes in the amygdala and hippocampus caused by the disease process seem to be implicated in the aetiology . Frequently, images of people, small animals or objects are conceived or the hallucinations may have multiple content. The images may be familiar or not. They last from seconds to minutes, and may recur over the day . Usually, non-demented patients retain insight and the hallucinations are usually not threatening. Less commonly, the hallucinations are olfactory , auditory and tactile . One study showed that visual component was lacking in 10% of cases . Minor visual phenomena such as sense of presence and visual illusions affect 1772% of patients and delusions about 5% . Higher load of dopaminergic treatment may be related to the hallucinations, but disease severity, cognitive impairment, depression, older age and worse visual acuity may also be important .
Caregiver Burden And Questionnaire Assessment
The mean ZBI score shows a tendency to be lower in LCIG group compared to CSAI or CU group, even if no statistically significant difference was found among groups . The boxplot of the ZBI Score showed that LCIG and CU populations have a very similar distribution . The CSAI ZBI boxplot distribution is slightly wider but not statistically different . The aggregated results on ZBI scores never/rarely vs. sometimes/quite frequently/nearly always did not show a significant difference between groups for each question, except for the question number 6, regarding the negative influence of the assistance on the relationship with other relatives or friends; in this case, a difference was found between LCIG and CSAI . The following variables were correlated with the ZBI score: caregivers change in capability to perform family duties and leisure activities,caregivers change in work,need of professional assistance,patients judgment on QoL, and caregivers judgment on QoL. The analysis of the distribution of these significant associations is described in Figure 2A and . The UPDRS-IV item 39 and the H&Y stage did not show any association with the ZBI score .
|
Figure 1 Frequency of symptoms reported by caregivers and kind of mood change in each group. |
|
Table 3 Aggregated Results for ZBI Scores in the Three Groups of Treatment. The Total Percentage in Each Group Were Computed Excluding the Missing Data |
Parkinsons Disease: Is Death Inevitable
Death is inevitable for us all, but Parkinson’s disease in itself is not a death sentence. Your prognosis will depend on your age, general health, and how your Parkinson’s has progressed. However, there is no reason to assume that you won’t continue to live a full and productive life with the condition.
Scientists are performing new medical trials and research all the time to look for a cure for Parkinsons disease, while our understanding of medications and treatments is better than it has ever been. Therefore, there are plenty of ways you can control the symptoms of Parkinsons disease and make changes to your lifestyle as necessary. Many Parkinsons patients take up yoga, gardening, swimming and walking to improve their strength, flexibility and mental health. Others use physical therapy, massage and meditation to help keep symptoms at bay. These are great ways to extend your life expectancy with or without Parkinsons disease.
APA ReferenceSmith, E. . Is Parkinsons Disease Fatal? Life Expectancy for Parkinsons, HealthyPlace. Retrieved on 2021, August 25 from https://www.healthyplace.com/parkinsons-disease/information/is-parkinsons-disease-fatal-life-expectancy-for-parkinsons
Stage 4 The Advanced Stage Of Parkinsons Disease
This is considered the advanced stage of the disease during which the symptoms become severe and problematic. Loss of balance is common that can lead to falls and result in serious injuries. The patient can still stand and walk but may need a all the time. The patient increasingly depends on others for functioning. Depression-like symptoms may also appear in some patients.
What Are The Stages Of Parkinsons
Doctors sometimes use five stages to describe the progress of Parkinsons disease. Each stage presents changing or new symptoms that a person is likely to encounter.
It is worth noting that not everyone will reach the advanced stages. For some people, the symptoms remain mild, and they can continue to live independently and be mobile.
Dividing the condition into stages helps doctors and caregivers understand and address some of the challenges a person is experiencing as it progresses.
Your Home And Lifestyle
- Modify your activities and your home. For example, simplify your daily activities, and change the location of furniture so that you can hold on to something as you move around the house.
- Eat healthy foods, including plenty of fruits, vegetables, grains, cereals, legumes, poultry, fish, lean meats, and low-fat dairy products.
- Exercise and do physiotherapy. They have benefits in both early and advanced stages of the disease.
What Are The Symptoms Of End
Stage four for Parkinsons disease is often called advanced Parkinsons disease because people in this stage experience severe and incapacitating symptoms. This is when medication doesnt help as much and serious disabilities set in.
Theres an increased severity in:
- How you speak a softer voice that trails off.
- Falling and trouble with balance and coordination.
- Freezing a sudden, but temporary inability to move, when you start to walk or change direction.
- Moving without assistance or a wheelchair.
- Other symptoms such as constipation, depression, loss of smell, low blood pressure when going to stand up, pain, and sleep issues.
Many times someone with advanced PD cant live on their own and needs help with daily tasks.
Stage five is the final stage of Parkinsons, and assistance will be needed in all areas of daily life as motor skills are seriously impaired. You may:
- Experience stiffness in your legs. It may make it impossible to walk or stand without help.
- Need a wheelchair at all times or are bedridden.
- Need round-the-clock nursing care for all activities.
- Experience hallucinations and delusions.
As Parkinsons disease progresses into these advanced stages, its symptoms can often become increasingly difficult to manage. Whether you or your loved one with end-stage Parkinsons lives at home, in an assisted living facility or a nursing home, hospice services can optimize your quality of life and that of your family members as well.
Stooping Or Hunched Posture
People who have Parkinsons disease may notice changes in their posture due to other symptoms of the disease, such as muscle rigidity.
People naturally stand so that their weight is evenly distributed over their feet. However, people who have Parkinsons disease may start bending forward, making them appear hunched or stooped over.
My Parkinson’s Story: Advanced Parkinsons

This 10-minute video alternates between an interview with a man and his wife and his palliative care team, including a doctor, nurse, clerg and social worker. The man and his wife shares his experience with late stage Parkinson’s. The palliative care team explains that their job is to support the best physical, emotional and spiritual wellbeing of the immediate family as well as help the family make end of life decisions.
Combining Tests Into A Two
Two-stage screening where the first test is relatively inexpensive, but sensitive and moderately specific is an approach that reduces the number of expensive confirmatory tests. Using imaging as the second test in a two-step process reduces costs by lowering the number of scansthat need to be performed. To have a high overall accuracy rate, the first-stage test must be at least as sensitive as imaging. As a secondary screen, imaging can weed-out false positive tests, but it cannot re-capture false-negative cases that were not referred for imaging. The primary screen must also be reasonably specific, because the number of scans that needs to be performed depends on the false positive rate of the primary screening test.
To Support The Diagnosis Your Healthcare Provider Will Also Look For Other Symptoms:
- Micrographia
- Reduced facial expression
- Decreased arm swing or leg drag on one side of the body while walking
Symptoms such as shoulder pain, depression, sleep problems, constipation and loss of sense of smell can begin long before any of the motor symptoms appear. Because symptoms like these can be subtle at first, they are not always evident or meaningful before diagnosis. It is common after being diagnosed with Parkinsons to look back and realize symptoms had been coming on gradually for months or even years. Often people explore other treatment avenues for early symptoms, like physical therapy or even surgery for pain, only to discover later it was actually connected to Parkinsons.
Since doctors diagnose other medical conditions using sophisticated technology, many are surprised to learn a Parkinsons diagnosis is based on your medical history and a simple examination. While your healthcare provider may take other steps, such as order blood and urine tests, check copper levels and order a brain scan, such as an MRI or CT or DaTscan that measures dopamine, these tests do not diagnose Parkinsons. They are used to either confirm the diagnosis or determine if another medical condition is causing your symptoms.
Everyones experience of Parkinsons will be unique, and a person with YOPD may have similar symptoms as someone diagnosed later in life.
Whats The Relationship Between Parkinsons And Sleep
Parkinsons disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinsons disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinsons disease. These signs may include things like thrashing while youre asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinsons disease, a restful nights sleep can be hard to find.
Braaks Hypothesis On How Parkinsons Disease Begins
Braaks hypothesis, named for professor Heiko Braak, MD, who outlined the theory in 2003, suggests that rather than beginning in the brain, Parkinsons disease begins in the periphery of the body. Braaks hypothesis proposes that the earliest signs of PD are found in the gut and the olfactory bulb, an area of the brain involved in the sense of smell.2-4
The accumulation of the protein is believed to begin in the gastrointestinal tract or the olfactory bulb before progressing to other areas of the brain. After the aggregates of alpha-synuclein have formed, they appear to be capable of growing and spreading from nerve cell to nerve cell across the brain.2-4
The appearance of alpha-synuclein aggregates coincides with the appearance of symptoms: alpha-synuclein aggregates in the brainstem correlates with the onset of motor symptoms. Appearance of alpha-synuclein aggregates in the cortex correlates with dementia and cognitive dysfunction.2-4
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinsons Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting both” to stay best informed on the Foundation’s work and the latest in PD news.
What Is And Isnt Parkinsons Disease
I am often asked if Parkinsons Disease is a form of Alzheimers. is not Alzheimers, or a brain tumor, and the prognosis for Parkinsons, though not a perfect scenario, leaves room to live a productive life.
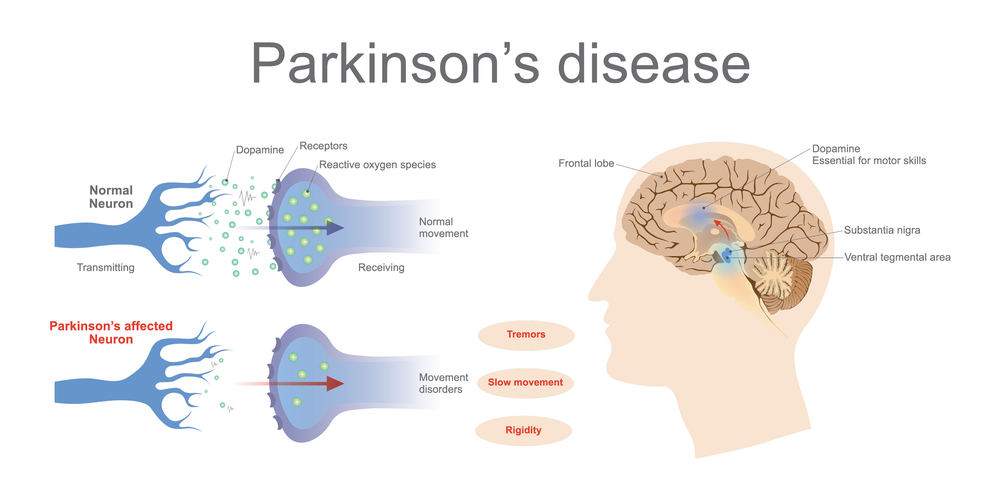
PD is a progressive and chronic neurological disease that often begins with mild symptoms that advance gradually over time. Symptoms can be so subtle in the early stages that they go unnoticed, leaving the disease undiagnosed for years. For patients with Parkinsons, there is a reduction in the body chemical , which controls movement and mood so simple activities like walking, talking and writing can be impacted.
Due to the complexity of PD, diagnosis is based on a variety of factors. The best diagnosis is made by an expert doing a careful history and exam followed by tracking responses to therapy. There is no blood or laboratory test to diagnose Parkinsons disease.
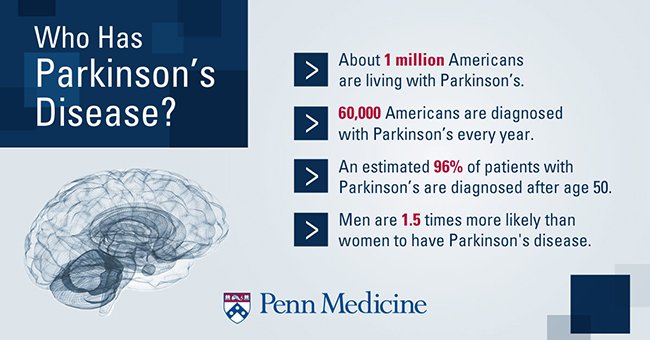
While Parkinsons reaches all demographics, the majority of people with PD are age 60 or older. Men and people with a family history of the disease have an increased risk.
Patient And Caregiver Selection
Advanced PD patients already in treatment with optimized CSAI, LCIG, or CU since at least 6 months up to 3 years were enrolled in this study. The inclusion criteria to verify the advanced stage included the presence of at least 3 hours OFF period per day or >25% of daily time spent in OFF as assessed by United Parkinsons Disease Rating Scale -IV item 39. Further inclusion criteria were the presence of a family adult carer who had provided regular daily assistance to the patient for at least 6 months.
The history or presence of any severe condition that might interfere with caregiver burden assessments, previous treatment with LCIG, CSAI, or DBS, mild to severe cognitive dysfunction/dementia , and Hoehn & Yahr stage 5 in OFF condition in the previous 12 months were considered as exclusion criteria.
The present study was approved by the Ethics Committee of each local health authority and each patient had to be able to understand and provide their informed consent as well as their care partners provided informed consent. Patients with mild to severe cognitive dysfunction/dementia, were excluded in order not to interfere with the capacity consent. The study was conducted according to the International Conference on Harmonization Good Clinical Practices.
New Diagnostic Standards For Parkinsons
Until recently, the gold-standard checklist for diagnosis came from the U.K.s Parkinsons Disease Society Brain Bank. It was a checklist that doctors followed to determine if the symptoms they saw fit the disease. But thats now considered outdated. Recently, new criteria from the International Parkinson and Movement Disorder Society have come into use. This list reflects the most current understanding of the condition. It allows doctors to reach a more accurate diagnosis so patients can begin treatment at earlier stages.
Do People Actually Lose Their Sense Of Smell With Parkinsons
A: Yes. Its a condition called anosmia, and if you have it with no other disease , you have at least a 50 percent chance of developing Parkinsons disease in the next five to 10 years. What happens is that alpha-synuclein, the protein that clumps in the part of the brain that regulates dopamine and leads to Parkinsons disease, also aggregates in the olfactory bulb, the part of the brain responsible for your sense of smell. This happens well before the protein accumulations cause motor symptoms.
Interdisciplinary Palliative Care For People With Advanced Parkinsons Disease: A View From The Home
Jori E. Fleisher1, Ellen C. Klostermann1, Serena P. Hess1, Jeanette Lee1, Erica Myrick1, Joshua Chodosh2,3
1Department of Neurological Sciences, New York University School of Medicine , 3Medicine Service, VA New York Harbor Healthcare System, New York, NY , USA
Contributions: Conception and design: JE Fleisher, J Chodosh; Administrative support: EC Klostermann, SP Hess, J Lee, E Myrick; Provision of study materials or patients: JE Fleisher; Collection and assembly of data: JE Fleisher, EC Klostermann, SP Hess, J Lee, E Myrick; Data analysis and interpretation: JE Fleisher, SP Hess, J Lee, EC Klostermann, J Chodosh; Manuscript writing: All authors; Final approval of manuscript: All authors.
Correspondence to:
Background: Advanced Parkinsons disease is a multidimensional neurodegenerative condition with motor and non-motor symptoms contributing to increasing disability and decreasing quality of life. As the disease progresses, patients may become homebound and estranged from neurological care, with dire consequences. We describe the increasing epidemiologic burden of and individual risks faced by patients with palliative-stage PD and their caregivers.
Keywords: Home visits; interdisciplinary; neurodegenerative disease; Parkinsons disease
Submitted Aug 12, 2019. Accepted for publication Sep 09, 2019.
doi: 10.21037/apm.2019.09.12
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinsons disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
Other Treatments Of Lower Back Pain
NSAIDs which include medications such as ibuprofen and naproxen, as well as acetaminophen, can be very beneficial for pain in PD, as they are for the general population. These medications do not typically have neurologic side effects, so they are well tolerated in people with PD. They can have other side effects though, so as always, discuss all medications that you are taking, including over-the-counter medications, with your doctor. If these medications do not provide sufficient back pain relief, your doctor may prescribe a pain medication. In addition, he/she may refer you for a procedure such as an epidural injection to help with lower back pain. Rarely, surgery may be recommended if a specific structural reason for pain is identified.
Message From Our Podcast Sponsor:
The content of this podcast was up to date and accurate at the time of recording in June 2021. The views expressed in this episode represent the speakers own opinions and experiences. Speakers may express personal opinions that are not necessarily shared by Britannia Pharmaceuticals. Content from this episode has been reviewed by Britannia to ensure compliance with the ABPI and EFPIA Codes of Practice for the Pharmaceutical Industry.
This article and podcast episode is sponsored by Britannia Pharmaceuticals. All interviewees have received a donation for their time. The information in this article is given for information purposes only and does not represent an endorsement by the European Parkinsons Disease Association of any particular treatments, products or companies. This article and podcast episode is not a substitute for advice from your doctor, pharmacist or other healthcare professional. Parkinsons Life makes no representations or warranties of any kind, express or implied, about the completeness or accuracy of information provided.
Read more:
How Is Parkinson’s Disease Diagnosed
Your doctor will ask questions about your symptoms and your past health and will do a neurological examination. This examination includes questions and tests that show how well your nerves are working. For example, your doctor will watch how you move, check your muscle strength and reflexes, and check your vision.
Your doctor will also ask questions about your mood.
In some cases, your doctor may have you try a medicine. How this medicine works may help your doctor know if you have Parkinson’s disease.
There are no lab or blood tests that can help your doctor know whether you have Parkinson’s. But you may have tests to help your doctor rule out other diseases that could be causing your symptoms. For example, you might have an to look for signs of a or brain tumour.
What Else Can I Do To Sleep Better With Parkinsons Disease

Practicing healthy sleep hygiene habits may also promote more restful .
Do:
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as , within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
