Stage Four: Symptoms Are Severe And Disabling And You Often Need Assistance To Walk Stand And Move

Stage Four Parkinson’s disease is often called advanced Parkinson’s disease. People in this stage experience severe and debilitating symptoms. Motor symptoms, such as rigidity and bradykinesia, are visible and difficult to overcome. Most people in Stage Four aren’t able to live alone. They need the assistance of a caregiver or home health aide to perform normal tasks.
Stage Three: Symptoms Are More Pronounced But You Can Still Function Without Assistance
The third stage is considered moderate Parkinson’s disease. In this stage, you’ll experience obvious difficulty with walking, standing, and other physical movements. The symptoms can interfere with daily life. You’re more likely to fall, and your physical movements become much more difficult. However, most patients at this stage are still able to maintain independence and need little outside assistance.
Mayo Clinic Q And A: Rate Of Progression Of Parkinsons Disease Hard To Predict
DEAR MAYO CLINIC: My father is 64 and was diagnosed with Parkinson’s last year. So far his symptoms are very mild, but I’m wondering what the typical progression of the disease is like. I have read that deep brain stimulation is sometimes recommended. When is this type of treatment usually considered? Is it safe?
ANSWER: The symptoms of Parkinson’s disease, or PD, tend to begin very gradually and then become progressively more severe. The rate of progression is hard to predict and is different from one person to another. Treatment for PD includes a variety of options, such as exercise, medication and surgery. Deep brain stimulation is one surgical possibility for treating PD, but it’s usually only considered in advanced cases when other treatments don’t effectively control symptoms.
Parkinson’s disease is a syndrome which typically has no known cause. The diagnosis is based on symptoms. Neurologists who specialize in movement disorders typically have the most experience with PD diagnosis and treatment. There are many symptoms of parkinsonism. The most common include excessive slowness and lack of movement, as well as shaking or tremor.
As in your father’s situation, symptoms are often mild at the outset. How quickly they get worse varies substantially, perhaps because there may be multiple underlying causes of the disease. In most cases, symptoms change slowly, with substantive progression taking place over the space of many months or years.
Life Expectancy Of Parkinsonism Patients In The General Population license
Absolute life expectancy estimates of parkinsonism are easy to translate to patients.
- •
-
Patients with parkinsonism have a reduced life expectancy compared to matched controls.
- •
-
The most prominent decrease in life expectancy is observed if parkinsonism is diagnosed before the age of 70.
- •
-
The number of years lived with parkinsonism in the general population is relatively low.
What Is The Prognosis And Life Expectancy For Parkinson’s Disease

The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
Why It Is Hard To Detect The Progression Of Parkinsons Disease
As we stated above that Parkinson’s disease is not basic, it becomes difficult to detect it in its early stage due to 2 symptoms – it affects motor issues such as the rigid muscles and tremors, and the other is the development of non-motor symptoms such as dementia, pain, and loss of smell.
Although one cannot see that a person suffering from Parkinson’s disease will show all the symptoms, you cannot even tell or predict which symptoms will be present and their severity. For instance, one patient may show severe dementia with slight tremors. Another patient displays a critical condition of tremors but does not have any problem related to memory or thinking. In another case, the patient can show a severe state of all the symptoms. Therefore, it is difficult to predict the progression of the condition.
In addition to this, the medicines that help in treating Parkinson’s disease also make it difficult to predict the results because a few patients show positive results while others do not show any improvement.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
How Is Parkinsons Dementia Different From Alzheimers Disease
The advanced cognitive changes that impact daily living in Alzheimer’s and Parkinson’s disease are both types of dementia.
Parkinson’s disease dementia can occur as Parkinson’s advances, after several years of motor symptoms. Dementia with Lewy Bodies is diagnosed when cognitive decline happens first, or when Parkinson’s motor symptoms and cognitive decline occur and progress closely together. Cognitive impairments in PDD, combined with the movement symptoms of the disease, produce a greater impact on social and occupational functioning than Alzheimer’s.
Alzheimer’s, a fatal brain disease, causes declines in memory, thinking and reasoning skills. Physicians can diagnose Alzheimer’s. Visit the Alzheimer’s Association to learn the 10 signs Alzheimer’s disease.
Fortunately for people with PD, Parkinson’s disease dementia is less disabling than Alzheimer’s disease. People with Alzheimer’s have language difficulties earlier than people with Parkinson’s, and no new memories are formed. People with PD also have more ability to compensate and adjust based on cues.
What Is The Best Way To Communicate With A Person With Pdd
PD-related mood and motor changes can impact communication; cognitive changes and Parkinson’s disease dementia can further these difficulties.
- It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. Stay calm and be patient. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- You may find acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior: the person may be hungry, thirsty, tired, in pain, frustrated, lonely or bored.
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- It’s OK to use humor to diffuse stressful situations but avoid negative humor or sarcasm ? these can be misunderstood.
Page reviewed by Dr. Jori Fleisher, MSCE, Assistant Professor, Department of Neurological Sciences at Rush University Medical Center, a Parkinson’s Foundation Center of Excellence.
How Long Does It Take For Parkinsons Disease To Progress
It is quite common for any individual suffering from Parkinson’s disease to wonder about the unfolding of the condition. If you belong to the group that in search for the answers related to the progression of Parkinson’s disease, then you will try to learn about the symptoms that you can acquire with the condition, when they start, and the changes the disease brings in the body.
The questions are basic, but Parkinson’s disease is not. Like other illnesses, Parkinson’s disease does not have a specific path of progression. Due to this, it is difficult to state or pin down the exact time or the path of the progression.
Complications Related To Parkinson’s Can Affect Survival Claudia Chaves, MD
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Parkinson’s is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinson’s disease in the United States. During the six-year period, 64% of the participants with Parkinson’s disease passed away.
The risk of death of those with Parkinson’s was then compared to Medicare beneficiaries who did not have Parkinson’s or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinson’s was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinson’s disease was similar to those with hip fracture, Alzheimer’s dementia, or a recent heart attack—although it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
New Clues On Why Some People With Parkinson’s Die Sooner
- Date:
- American Academy of Neurology
- Summary:
- New research shows how old people are when they first develop Parkinson’s disease is one of many clues in how long they’ll survive with the disease.
New research shows how old people are when they first develop Parkinson’s disease is one of many clues in how long they’ll survive with the disease. The research is published in the October 5, 2010, print issue of Neurology®, the medical journal of the American Academy of Neurology.
The 12-year study included 230 people with Parkinson’s disease, of whom 211 died by the end of the research. “Remarkably, time to death for these people took anywhere from two to 37 years from diagnosis so it’s important we try to identify those risk factors that lead to an early death so we can find ways to increase a person’s life expectancy,” said Elin Bjelland Forsaa, MD, with Stavanger University Hospital in Norway and a member of the American Academy of Neurology.
The average time from the appearance of movement problems to death was 16 years. The average age at death was 81.
The study found that the risk of earlier death was increased about 1.4 times for every 10-year increase in age when symptoms began. People with psychotic symptoms, such as delusions and hallucinations, were also 1.5 times more likely to die sooner compared to those without these symptoms.
The study also found that taking antipsychotic drugs or drugs for Parkinson’s disease had no negative effect on survival.
Story Source:
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinson’s Disease – In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinson’s Disease – Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Whats The Life Expectancy For A Senior With Parkinsons
Parkinson’s is a progressive disorder that negatively affects mobility, dexterity, and cognitive health. There currently isn’t a cure for Parkinson’s, but doctors have come up with a wide variety of treatments that can minimize or delay some of the most prominent symptoms. Here’s a closer look at the average life expectancy of a person with Parkinson’s and a few steps that can be taken to increase longevity after being diagnosed with this disorder.
Stage One: Symptoms Affect Only One Side Of Your Body

The initial phase of Parkinson’s disease typically presents with mild symptoms. Some patients will not even detect their symptoms in the earliest phases of this stage. Typical motor symptoms experienced in Stage One include tremors and shaking limbs. Family members and friends may begin to notice other symptoms including tremor, poor posture, and mask face or loss of facial expression.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Can A Person With Parkinsons Have A Normal Life Span
When people first hear about a Parkinson’s diagnosis, their thoughts often go to the worst-case scenario. However, it’s important to keep a positive perspective about your senior loved one’s diagnosis. While you can expect your loved one to develop some symptoms such as tremors, there are many things that can be done to give him or her an excellent prognosis for a long and happy life.
Caregiving In The Late Stages Of Parkinsons Disease
In late-stage PD, patients have significant mobility challenges. Caregivers likely need to provide more hands-on assistance to help them get around the house. It’s important that caregivers learn safe and effective methods to provide help without injuring themselves. Physical therapists can be a great resource to assess an individual situation and teach effective ways of giving assistance.3
Freezing, a sudden but temporary inability to move, can become more common in late-stage PD. Freezing often happens when initiating movement or navigating around obstacles, and freezing episodes contribute to falls. Caregivers can help their loved one overcome freezing by providing a visual cue to step over, like a laser pointer, or using music or rhythm for the person with PD to walk to.3
Late stage PD can make daily activities, such as getting dressed, much more challenging. Caregivers can make getting dressed easier by ensuring adequate time to account for slow movement, choosing a time when medications are “on” and working well, and assembling all necessary items close to the person. Allowing the person with PD to do as much as they can gives them a sense of participation in the process.3
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
How Long Can A Person Live With Stage 5 Parkinson
When patients reach stage five – the final stage of Parkinson’s disease – they will have severe posture issues in their back, neck, and hips. In end–stage of Parkinson’s disease, patients will also often experience non-motor symptoms. These can include incontinence, insomnia, and dementia.
Additionally, what do Parkinson’s patients usually die from? But the most common cause of death in those with Parkinson’s is pneumonia, because the disease impairs patients‘ ability to swallow, putting them at risk for inhaling or aspirating food or liquids into their lungs, leading to aspiration pneumonia.
Also asked, what happens in stage 5 Parkinson’s?
Stage Five of Parkinson’s Disease –Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking.
How quickly can Parkinson’s progress?
While symptoms and disease progression are unique to each person, knowing the typical stages of Parkinson’s can help you cope with changes as they occur. Some people experience the changes over 20 years or more. Others find the disease progresses more quickly.
Caring For Your Health With Parkinson’s Disease
In addition to caring for your Parkinson’s health, it is also important to care for your overall health. This means visiting your primary care physician periodically for preventive care like the annual flu shot and cancer screenings—for example, a mammogram for breast cancer screening and a colonoscopy for colon cancer screening.
A primary care physician can also evaluate for risk factors related to heart attacks and strokes, and provide counseling on exercise, smoking, alcohol use, depression, or other mental health concerns. Regular visits to your primary care physician or neurologist will also allow them to catch bacterial infections like urinary tract infections before they get serious.
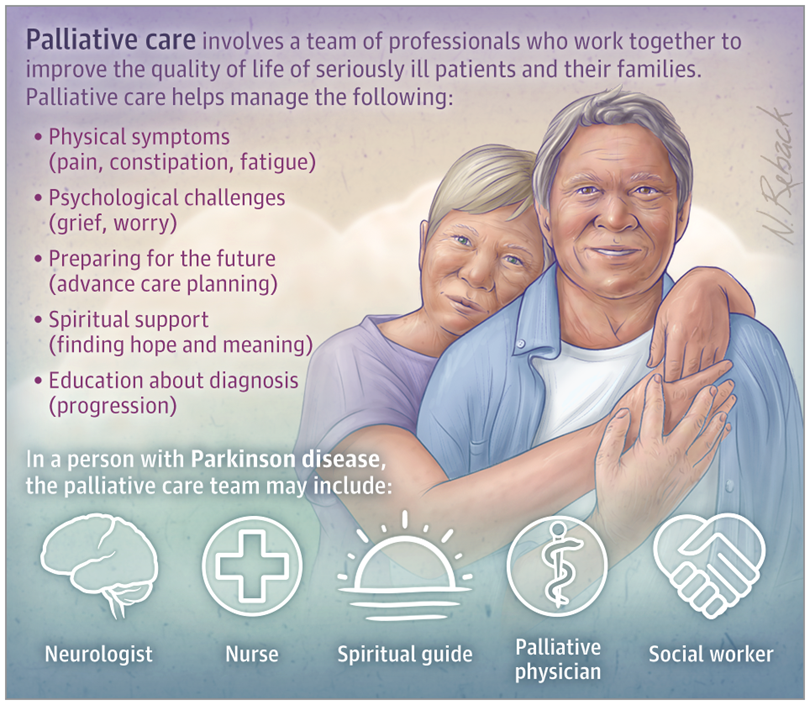
Complex Parkinson’s Disease And Palliative Care
Complex Parkinson’s disease is defined as the stage when treatment is unable to consistently control symptoms, or the person has developed uncontrollable jerky movements .
These problems can still be helped by adjustment or addition of some of the medications used to treat Parkinson’s disease, under the supervision of a doctor with a specialist interest in Parkinson’s disease.
As Parkinson’s disease progresses, you’ll be invited to discuss the care you want with your healthcare team as you near the end of your life. This is known as palliative care.
When there’s no cure for an illness, palliative care tries to alleviate symptoms, and is also aimed at making the end of a person’s life as comfortable as possible.
This is done by attempting to relieve pain and other distressing symptoms, while providing psychological, social and spiritual support for you and your family.
Palliative care can be provided at home or in a hospice, residential home or hospital.
You may want to consider talking to your family and care team in advance about where you’d like to be treated and what care you wish to receive.
Want to know more?
How Can We Support The Sleep/wake Cycle Of Pdd

For people with PDD who are confused about the day-night cycle, some daily strategies can be helpful. At night, starting a “lights out” routine that happens at the same hour every day, where all curtains are closed and lights are turned off, can help the person understand that it is sleep time. During the day, opening the curtains, allowing the person with PDD to spend as much time in the daylight as possible, avoiding naps, and organizing stimulating activities, can be helpful. Having lots of calendars and clocks in every room might also help a person with PDD be less confused about the time of day.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
Parkinson’s Disease Symptoms: Life Expectancy

Even though Parkinson’s disease is a serious, progressive condition, it is not considered a fatal illness. People who have Parkinson’s disease usually have the same average life expectancy as people without the disease.
But when the disease is in its advanced stages, Parkinson’s symptoms can lead to life-threatening complications, including:
- Falls that lead to fractured bones
- Pneumonia
- Choking
Thinking about the progression of Parkinson’s disease can be frightening. But proper treatments can help you live a full, productive life for years to come. And researchers hope to one day find ways to halt the progression of Parkinson’s and restore lost functioning.
Parkinsons Disease Is A Progressive Disorder
Parkinson’s Disease is a slowly progressive neurodegenerative disorder that primarily affects movement and, in some cases, cognition. Individuals with PD may have a slightly shorter life span compared to healthy individuals of the same age group. According to the Michael J. Fox Foundation for Parkinson’s Research, patients usually begin developing Parkinson’s symptoms around age 60. Many people with PD live between 10 and 20 years after being diagnosed. However, a patient’s age and general health status factor into the accuracy of this estimate.
While there is no cure for Parkinson’s disease, many patients are only mildly affected and need no treatment for several years after their initial diagnosis. However, PD is both chronic, meaning it persists over a long period of time, and progressive, meaning its symptoms grow worse over time. This progression occurs more quickly in some people than in others.
Pharmaceutical and surgical interventions can help manage some of the symptoms, like bradykinesia , rigidity or tremor , but not much can be done to slow the overall progression of the disease. Over time, shaking, which affects most PD patients, may begin to interfere with daily activities and one’s quality of life.
Risks Associated With A Parkinsons Diagnosis
Parkinson’s disease isn’t fatal itself, but it does lead to conditions that can be fatal. For instance, a senior who has significant tremors or freezing may have a serious fall that leads to a traumatic brain injury. Seniors with Parkinson’s disease also have a greater risk of choking on their food or developing pneumonia due to the ways their symptoms affect their muscles and organs. Understanding the risks associated with your loved one’s symptoms helps you add strategies to the care plan that increase his or her chances of enjoying a longer life.
Difficulty swallowing and other safety issues in the advanced stages of Parkinson’s disease can make caring for seniors increasingly challenging. Aging in place can present a few unique challenges for older adults. Some only require part-time assistance with exercise or meal preparation, while others are living with serious illnesses and benefit more significantly from receiving 24-hour care. Toronto, ON, Home Care Assistance are leaders in the elderly in-home care industry for good reason. We tailor our care plans based on each senior’s individual needs, our caregivers continue to receive updated training in senior care as new developments arise, and we also offer comprehensive care for seniors with Alzheimer’s, dementia, and Parkinson’s.
