If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229
Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
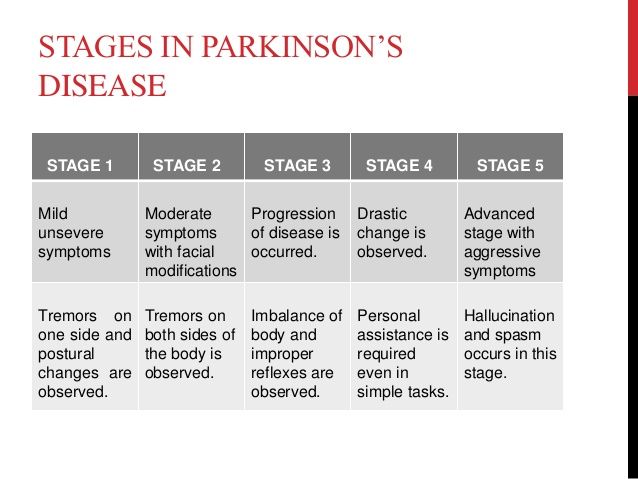
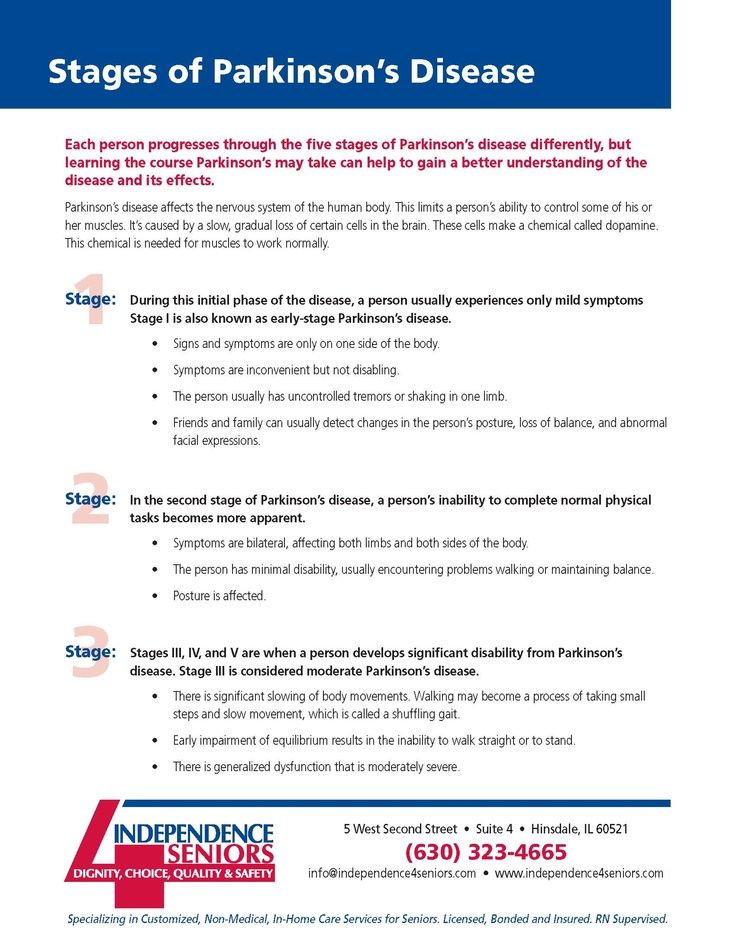
Stage 3As motor symptoms become worse, patients may begin to experience loss of balance leading to falls and movement can become very slow. Although many patients can still live independently they may have difficulty in everyday activities such as eating or dressing.
MORE: How does Parkinson’s disease affect the brain?
Stage 4In this later stage, symptoms are now extremely limiting. Many patients can still stand without assistance but movement is greatly impaired. Most will need help with everyday activities and will not be able to look after themselves.
Stage 5This is the most advanced stage of the disease and most patients will experience difficulty in walking and standing, often requiring a wheelchair. Assistance will be needed in all areas of daily life as motor skills are seriously impaired. In addition, people with advanced Parkinson’s disease may also begin to suffer hallucinations.
MORE: How Parkinson’s disease affects your body.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half “of the patients were described as unable to make any decisions in the last month of life.” 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Parkinson’s Patients Saw Continued Improvement In Motor Symptoms Quality Of Life
Deep brain stimulation remained effective in Parkinson’s disease patients more than 15 years after the device was implanted, and patients continued to demonstrate significant improvement in motor symptoms, a retrospective study showed.
Parkinson’s patients who had bilateral subthalamic nucleus deep brain stimulation for 15 years or longer spent 75% less time with dyskinesia and 58.7% less time in the off state than pre-surgery baseline , reported Elena Moro, MD, PhD, of Grenoble Alpes University in France, and co-authors.
These patients also reduced their dopaminergic drugs by 50.6% , they wrote in Neurology. The Parkinson’s Disease Quality of Life questionnaire total score, emotional function domain score, and social function domain score improved by 13.8% , 13.6% and 29.9% , respectively.
“Deep brain stimulation benefits seem to last for several years but not enough data have been available to show that these effects are still present more than 15 years after surgery,” Moro said in a statement.
“Our study found that, despite the natural progression of Parkinson’s disease and the worsening of some symptoms that become resistant to medications over the years, participants still maintained an overall improvement in quality of life,” she added.
In the long-term, 19 patients were completely independent in their activities of daily living, 27 patients needed some help, and five were institutionalized. A total of 18 of 51 patients had dementia.
Disclosures
Mayo Clinic Q And A: Rate Of Progression Of Parkinsons Disease Hard To Predict
DEAR MAYO CLINIC: My father is 64 and was diagnosed with Parkinson’s last year. So far his symptoms are very mild, but I’m wondering what the typical progression of the disease is like. I have read that deep brain stimulation is sometimes recommended. When is this type of treatment usually considered? Is it safe?
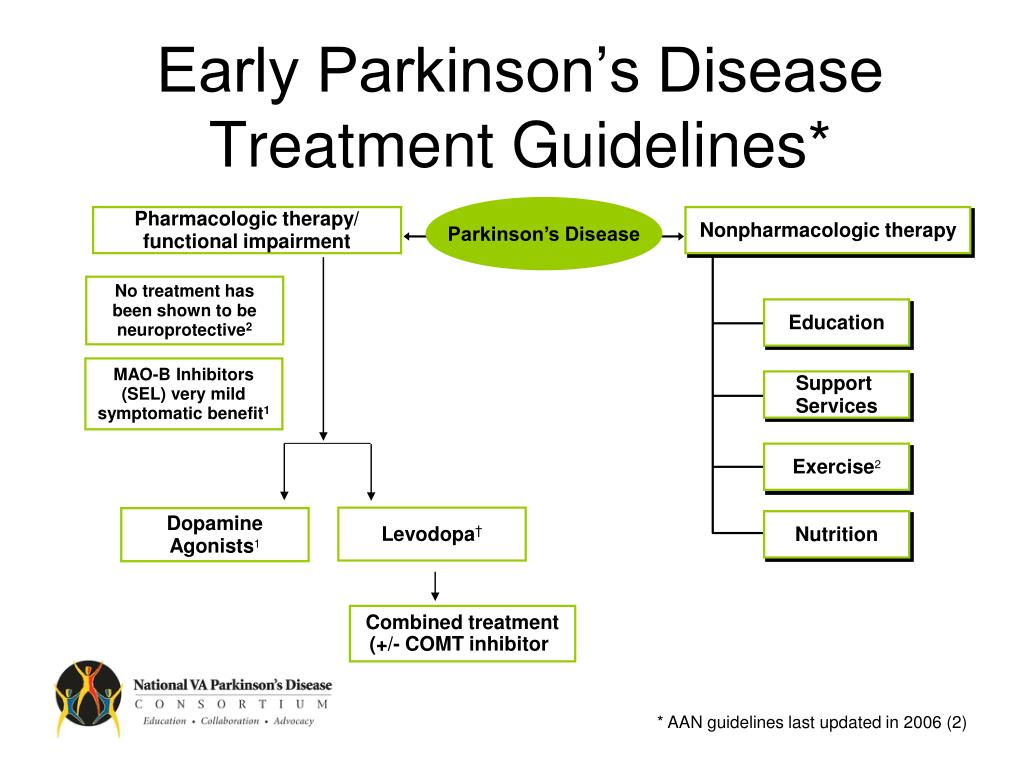
ANSWER: The symptoms of Parkinson’s disease, or PD, tend to begin very gradually and then become progressively more severe. The rate of progression is hard to predict and is different from one person to another. Treatment for PD includes a variety of options, such as exercise, medication and surgery. Deep brain stimulation is one surgical possibility for treating PD, but it’s usually only considered in advanced cases when other treatments don’t effectively control symptoms.
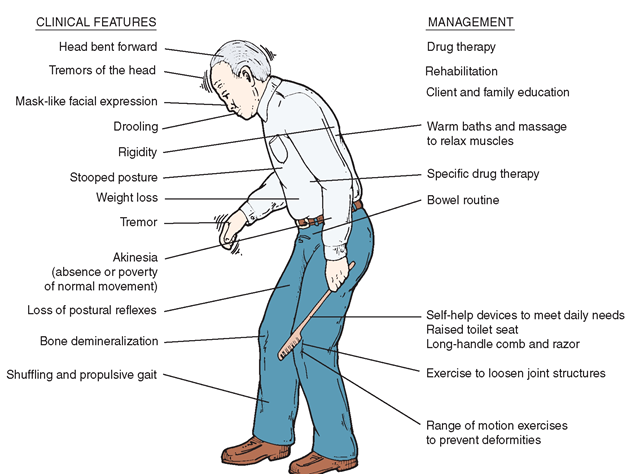
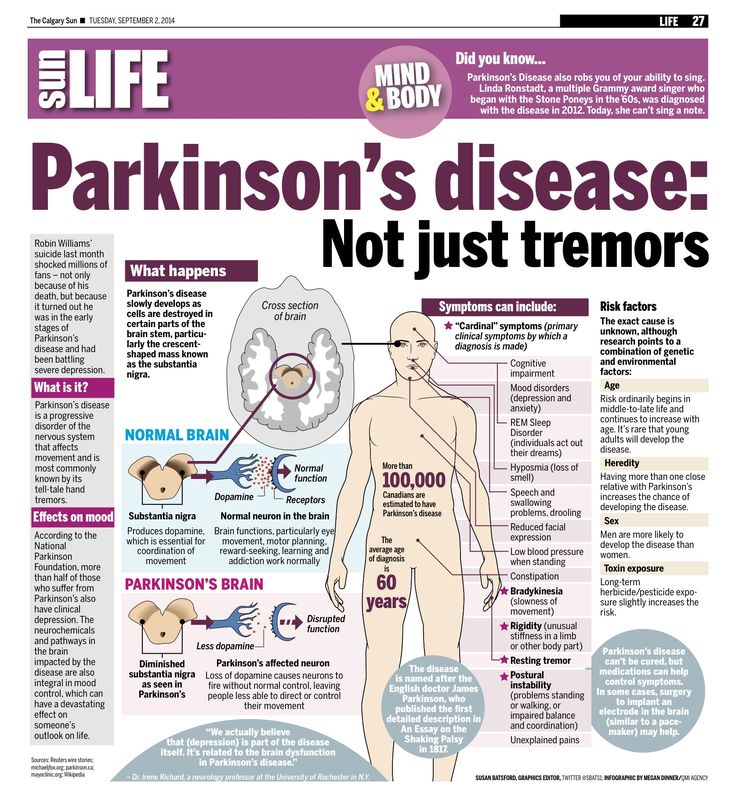
Parkinson’s disease is a syndrome which typically has no known cause. The diagnosis is based on symptoms. Neurologists who specialize in movement disorders typically have the most experience with PD diagnosis and treatment. There are many symptoms of parkinsonism. The most common include excessive slowness and lack of movement, as well as shaking or tremor.
As in your father’s situation, symptoms are often mild at the outset. How quickly they get worse varies substantially, perhaps because there may be multiple underlying causes of the disease. In most cases, symptoms change slowly, with substantive progression taking place over the space of many months or years.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinson’s disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day – even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
Mean Life Expectancy In Patients With Pd Compared With The General Population
The estimated changes in LE compared with the general population for a range of possible SMR values, stratified by age and sex, using the Gompertz function and the 2003 UK mortality rates, are presented in table 2?2.. Calculated LEs ) and AAD ) were compared between patients with PD and the UK general population. The graphical comparisons show that LE and AAD are considerably shorter or earlier in patients with age at onset before 50years compared with the general UK population. This difference decreases with increasing age in females and males. The mean LE of patients with PD with onset between 25 and 39years was 38 years, corresponding to an AAD of 71 years compared with an LE of 49 and AAD of 82 years in the general population. The mean LE of patients with PD with onset between 40 and 64years was 21 years, resulting in an AAD of 73 years compared with an LE of 31 and an AAD of 83 years in the general population. The mean LE for older individuals with PD was 5 years, resulting in an AAD of 88 years compared with an LE of 9 years and an AAD of 91 years in the general population. The SMR calculations were the same for both sexes, and therefore changes in LE were the same, but the actual LE and AAD estimates were higher in women because they live longer, on average, than males in the general population.
| Age |
|---|
Deep Brain Stimulation May Offer Lasting Benefits For Parkinsons Disease
Study: Patients Continue to See Improvement in Tremors 10 Years After Surgery
Aug. 8, 2011 — A new study shows that Parkinson’s disease patients treated with deep brain stimulation can expect the technology to control symptoms like tremors for a decade or longer, while other improvements, such as those in speech and balance, may lessen over time.
Deep brain stimulation uses a battery operated device similar to a pacemaker to deliver electrical impulses that stimulate areas of the brain that control movement.
The impulses are thought to block abnormal signals that cause many of the debilitating symptoms of Parkinson’s, like tremors, slowness, stiffness, and difficulty with speech.
The procedure, which has been used for over a decade, is typically offered to patients when medications no longer help.
The surgery costs between $30,000 and $50,000 but is usually covered by insurance.
“About 90,000 people now worldwide have received deep brain stimulation for Parkinson’s disease,� says study researcher Andres M. Lozano, MD, PhD, professor and chairman of neurosurgery at the University of Toronto. “The issue is, how long do the benefits last?�
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
Life Expectancy Of Parkinsonism Patients In The General Population license
Absolute life expectancy estimates of parkinsonism are easy to translate to patients.
- •
-
Patients with parkinsonism have a reduced life expectancy compared to matched controls.
- •
-
The most prominent decrease in life expectancy is observed if parkinsonism is diagnosed before the age of 70.
- •
-
The number of years lived with parkinsonism in the general population is relatively low.
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Why It Is Hard To Detect The Progression Of Parkinsons Disease
As we stated above that Parkinson’s disease is not basic, it becomes difficult to detect it in its early stage due to 2 symptoms – it affects motor issues such as the rigid muscles and tremors, and the other is the development of non-motor symptoms such as dementia, pain, and loss of smell.
Although one cannot see that a person suffering from Parkinson’s disease will show all the symptoms, you cannot even tell or predict which symptoms will be present and their severity. For instance, one patient may show severe dementia with slight tremors. Another patient displays a critical condition of tremors but does not have any problem related to memory or thinking. In another case, the patient can show a severe state of all the symptoms. Therefore, it is difficult to predict the progression of the condition.
In addition to this, the medicines that help in treating Parkinson’s disease also make it difficult to predict the results because a few patients show positive results while others do not show any improvement.
What Is The Main Cause Of Death In Parkinsons Disease Patients
Parkinson’s is often referred to as a “bespoke” disease because it affects each patient differently. Another factor worth considering is that Parkinson’s disease generally affects people in their 60s, most of whom die of unrelated conditions such as cancer, heart disease or stroke. However, the most common cause of death in those with Parkinson’s disease is pneumonia. This is because the disease can impair your ability to swallow in the later stages, putting you at risk for aspirating food or liquid into the lungs.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms

Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a “last in, first out approach.” 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patient’s medication history should be considered.29
Is Parkinsons Disease Fatal Life Expectancy For Parkinsons Emma-Marie Smith
Worried about your Parkinson’s disease life expectancy? A Parkinson’s disease diagnosis comes with many worries and anxieties. One worry concerns the progression of the disease and whether Parkinson’s disease can be fatal. The issue is rarely straightforward, but there is no reason to think your condition is a death sentence. Many people live for years or decades with their Parkinson’s disease symptoms under control, while the illness progresses more quickly for others. It’s important that you know what to expect when you’re diagnosed with Parkinson’s disease, so don’t be afraid to ask questions and air your concerns to your doctor. For now, let’s explore the issue of life expectancy of patients with Parkinson’s disease and address some common concerns.
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patient’s handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
Complications Related To Parkinson’s Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Parkinson’s is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinson’s disease in the United States. During the six-year period, 64% of the participants with Parkinson’s disease passed away.
The risk of death of those with Parkinson’s was then compared to Medicare beneficiaries who did not have Parkinson’s or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinson’s was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinson’s disease was similar to those with hip fracture, Alzheimer’s dementia, or a recent heart attack—although it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
How Long Does It Take For Parkinsons Disease To Progress
It is quite common for any individual suffering from Parkinson’s disease to wonder about the unfolding of the condition. If you belong to the group that in search for the answers related to the progression of Parkinson’s disease, then you will try to learn about the symptoms that you can acquire with the condition, when they start, and the changes the disease brings in the body.
The questions are basic, but Parkinson’s disease is not. Like other illnesses, Parkinson’s disease does not have a specific path of progression. Due to this, it is difficult to state or pin down the exact time or the path of the progression.
Reported Standardised Mortality Ratios From 1935 To 2001
The SMRs or mortality ratios comparing PD cases and controls from 39 studies from 1935 to 2006 are reported in table 1?1.. The SMRs ranged from 1, indicating no differences compared with the general population, to 3.4, indicating more than threefold higher mortality in PD. The time trend of estimates is inconsistent, although there appears to be a decrease in the 1970s, corresponding to the introduction of levodopa trials during that time period .). A geographical trend is not apparent, as the SMRs within each geographical region are as variable as between regions .
Table 1Summary of studies that have reported a standardised mortality ratio, comparing Parkinson’s disease patients with a general population
| Reference/date |
|---|
Figure 1Standardised mortality ratios for Parkinson’s disease from 39 studies by publication date.
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinson’s Disease – In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinson’s Disease – Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Stages Of Parkinsons Disease: Progression Of Parkinsons
The Parkinson’s disease stages are well-known among doctors. If you are diagnosed with Parkinson’s, it’s important to be aware of these stages so you can prepare yourself and your family for the future. As the disease progresses, you may develop further needs or require full-time care. Find out everything you need to know about the five stages of Parkinson’s disease and the progression of Parkinson’s symptoms.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
New Clues On Why Some People With Parkinsons Die Sooner
The American Academy of Neurology, an association of more than 22,000 neurologists and neuroscience professionals, is dedicated to promoting the highest quality patient-centered neurologic care. A neurologist is a doctor with specialized training in diagnosing, treating and managing disorders of the brain and nervous system such as epilepsy, dystonia, migraine, Huntington’s disease, and dementia.For more information about the American Academy of Neurology, visit http://www.aan.com.
Parkinsons Disease Late Stages: What Will Happen To Me
With advanced Parkinson’s disease, stage 5 life expectancy can be months or years depending on how your condition presents. You are likely to need round-the-clock care at this stage, and you may not be able to move around independently. Patients with late-stage Parkinson’s disease are more susceptible to pneumonia, sepsis, pyelonephritis and decubitus ulcers. Late-stage Parkinson’s also leads to Parkinson’s disease dementia in 50% of cases. For all of these reasons, many late-stage Parkinson’s patients are cared for by loved ones or in a hospice.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Caregiving In The Late Stages Of Parkinsons Disease
In late-stage PD, patients have significant mobility challenges. Caregivers likely need to provide more hands-on assistance to help them get around the house. It’s important that caregivers learn safe and effective methods to provide help without injuring themselves. Physical therapists can be a great resource to assess an individual situation and teach effective ways of giving assistance.3
Freezing, a sudden but temporary inability to move, can become more common in late-stage PD. Freezing often happens when initiating movement or navigating around obstacles, and freezing episodes contribute to falls. Caregivers can help their loved one overcome freezing by providing a visual cue to step over, like a laser pointer, or using music or rhythm for the person with PD to walk to.3
Late stage PD can make daily activities, such as getting dressed, much more challenging. Caregivers can make getting dressed easier by ensuring adequate time to account for slow movement, choosing a time when medications are “on” and working well, and assembling all necessary items close to the person. Allowing the person with PD to do as much as they can gives them a sense of participation in the process.3
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
