Fibril Structure And Early Onset Mutants
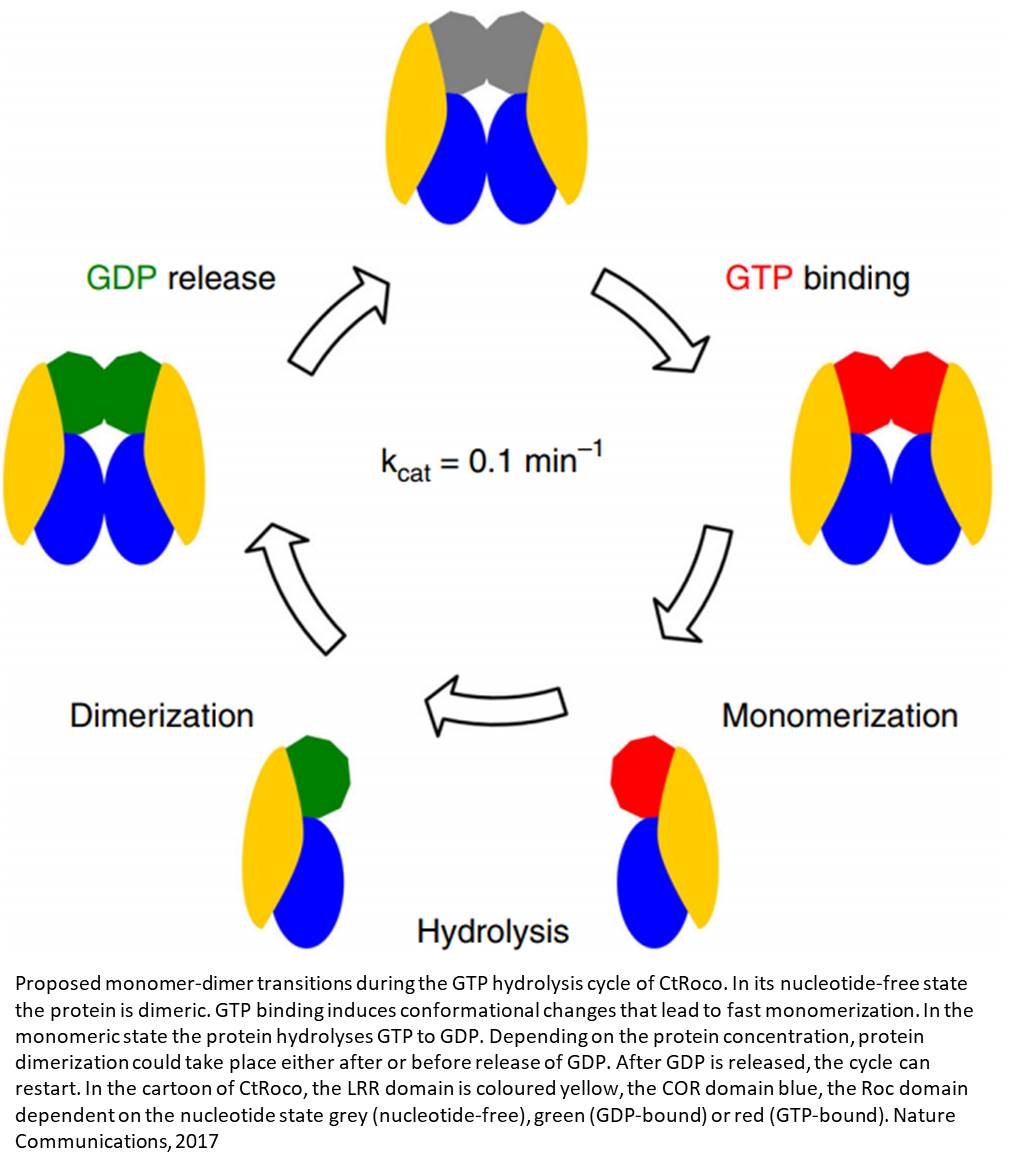
Recently, atomic resolution structures of the -sheet rich fibrilar forms of S have been elucidated. This was first reported by Tuttle et al using an ssNMR approach to achieve 4.8Å structural resolution , and more recently by Guerrero et al using cryoEM to obtain a 3.4Å resolution structure , closely followed by Li et al to 3.1Å resolution . The deduced Greek key conformation elucidated independently by all three groups is strikingly similar, showing that each S subunit in the fibril adopts a -sheet conformation, with hydrogen bonding between adjacent S subunits, spaced 4.84.9Å apart. The central -sheet rich core of the structures is located between residues 42102 and is comprised of an inner hydrophobic region of S that interlocks into right-angled spirals. N-terminal residues 141 and C-terminal residues 103121 display a flexible random coil arrangement that is consequently poorly resolved within the structure. The outer surface of the fibril is mostly hydrophilic, with the exception of two main regions; L38/V40 and F94/V95, with V82 providing further hydrophobicity . Moreover, the central hydrophobic region is comprised of Ala/Val residues, and one Ile . All structures highlight a potential salt bridge between E46 and K80, which likely serves to stabilize the conformation. An additional protofibril structure known as polymorph 1b shares the kernel structure that comprises the dimeric protofilament, but differs in the interface packing .
Fig. 2
Role Of Modifying Enzymes In Asyn Aggregation
Co-translational and post-translational modifications are crucial points of regulation of protein function. During biogenesis, aSyn is phosphorylated, acetylated, SUMOylated and ubiquitinated. These modifications can occur co-translationally when nascent chains are exiting the ribosomes, as well as post-translationally on mature proteins.
Acetylation is the addition of an acetyl group to a protein either co-translationally or post-translationally. aSyn is acetylated on the N-terminus at sites M1, K6, and K10, though the enzyme responsible is still not known . Acetylated aSyn has a more stable helix and increased lipid affinity, with a decrease in B-sheet propensity in regions with known familial mutations . Deacetylation of aSyn via deacylase SIRT2 increases aggregation and cytotoxicity in vivo through reduced clearance by the lysosome.
Ubiquitination is site-specific and differs between soluble and filamentous forms of aSyn. Soluble aSyn is mainly ubiquitinated at lysines in positions 21 and 23, as well as 32 and 34. Filamentous aSyn is ubiquitinated at lysines in positions 6, 10, and 12 by NEDD4 ligase . Ubiquitination of aSyn mediated by the E3 Ubiquitin ligase CHIP reduces aSyn oligomerization, while chaperone BAG5 mitigates ubiquitination by CHIP . Ubiquitination by SIAH1 promotes aggregation of aSyn . CHIP was also identified in the IPA pathway, along with ubiquitin.
Managing Pd Symptoms With Diet
Research supports these strategies for managing the following PD symptoms and medication side effects:
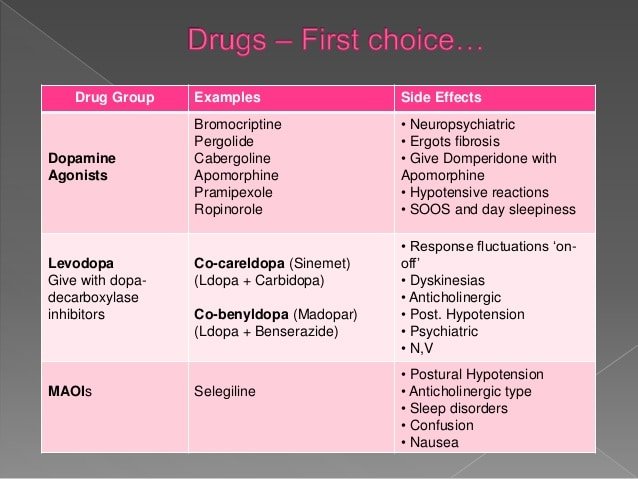
Fluctuations. Some people who take levodopa notice that their medication is less effective when taken with a high-protein meal . To address this difficulty, your doctor may recommend taking levodopa 30 minutes before, or 60 minutes after, you eat. Thats because levodopa is absorbed into the digestive system by the same route as protein when taken together, both compete to be absorbed into the body.
Even after adjusting medication timing, some people still have difficulty absorbing it. This can lead to fluctuations the levodopa wears off too soon or you experience changes throughout the day between the medicine working well and not having any benefit at all.
A protein-redistribution diet is a popular solution for fluctuations. That means eating most of your daily protein at dinnertime the last meal of the day to minimize Sinemet interference during most of the rest of the day. In research studies, fluctuations improved in about 80 percent of people who made this dietary change. People who benefitted most were those who started the regimen early in the course of their PD, before fluctuations became severe.
Iron also can prevent your body from taking up levodopa medications. Do not take iron supplements or multivitamins with iron within two hours of Sinemet.
Constipation. If you have less than one bowel movement per day, try to:
Read Also: Does Parkinson’s Make You Tired
A Protective Protein Gone Awry
Zasloffs team assessed biopsies from 42 children with upper GI issues, as well as 14 people who had norovirus a common cause of upper GI infections who had received intestinal transplants.
They found that S in enteric nerves of the upper GI tract in the children was linked to the degree of acute and chronic inflammation in the intestinal wall.
Some transplant patients showed S while they had norovirus. Researchers say that human S may attract human immune cells and activate dendritic cells to alert the immune system about the protein, driving the immune response that can cause damage.
We observed that in these kids the more inflammation, the more intense the presence of S in the nerves. We also could show that when a person contracted norovirus, S accumulated in the nervous tissues of their duodenum, not having been present before the infection, Zasloff told Healthline.
In a nutshell, his report shows that GI infections produce S as part of a normal immune response.
Zasloff noted that the protein is also present in the brains of people who have Alzheimers, and in the spinal cords of people who develop ALS, prompting the question of whether Alzheimers and ALS could be provoked by an infection.
In the meantime, Zasloff is starting a clinical trial of the drug ENT-01, which is a synthetic version of squalamine, a natural steroid found in the dogfish shark.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
You May Like: Dementia And Parkinsons Disease
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Don’t Miss: What Foods Should Parkinson’s Patients Avoid
Protein Shows Promise In Treating Parkinsons Disease
WEST LAFAYETTE, Ind. The true cause of Parkinsons disease is still a mystery to researchers, although they do know that in many patients, a protein called alpha-synuclein tends to aggregate in brain cells. But a different protein could help stop that aggregation, according to a new study in the Journal of Molecular Biology.
HYPE, the only Fic protein found in humans, is a key regulator of whether cells live or die under stress. In order to work properly, proteins need to fold in the correct shape. When cells are stressed, their proteins can become misfolded, at which point they can aggregate and become toxic. Cells sense stress by assessing the amount of misfolded proteins within them.
Since HYPE plays such an important role in how cells deal with stress from misfolded proteins, we wondered whether diseases that result from protein misfolding were likely to need HYPE, said Seema Mattoo, an assistant professor of biological sciences at Purdue University. We know that in Parkinsons disease, often the misfolded protein is aSyn. So we asked if HYPE could modify aSyn, and if so, what are the consequences?
The study shows that HYPE does modify aSyn and that this new modification, called AMPylation, decreases aggregation.
Clumps of aSyn, known as Lewy bodies, are the pathological hallmark of Parkinsons disease. Aggregated aSyn can poke holes in the membranes of neurons, which causes a decline in nerve function and messes up how nerve cells communicate.
ABSTRACT
Single Protein Causes Parkinson’s Disease And Multiple System Atrophy
- Date:
- KU Leuven
- Summary:
- Several neurodegenerative disorders are caused by aggregates of a single protein known as alpha-synuclein. Neurobiologists have discovered that the shape of these aggregates — ‘cylinders’ or ‘ribbons’ — determines whether a patient develops Parkinson’s disease or multiple system atrophy, respectively.
Several neurodegenerative disorders are caused by aggregates of a single protein known as alpha-synuclein. In collaboration with CNRS and the University of Antwerp, KU Leuven neurobiologists have discovered that the shape of these aggregates — ‘cylinders’ or ‘ribbons’ — determines whether a patient develops Parkinson’s disease or Multiple System Atrophy, respectively.
Typical of neurodegenerative disorders is the disrupted communication between brain cells together with a loss of cells in specific brain regions. For some brain diseases this phenomenon is linked to a protein known as alpha-synuclein. The exact function of this protein remains unclear, but it may play a role in the communication between brain cells. However, in the case of specific diseases, including Parkinson’s disease, Multiple System Atrophy , and dementia with Lewy bodies , this protein forms aggregates that cause neurodegeneration.
Story Source:
Don’t Miss: Does Flu Shot Cause Parkinson’s
Can Eating Well Alter The Course Of Pd
Scientists know a lot about the molecular changes that underlie Parkinsons. You may have heard of alpha-synuclein, the protein that forms clumps in brain cells, oxidative stress, mitochondrial dysfunction, and inflammation. The search is intense for therapies that can stop or reverse these processes. Can nutrition or dietary choices do anything to change them or alter the course of PD?
Some laboratory and animal research suggest that diet could have an effect, especially plant-based foods like fruits, vegetables, legumes, nuts and seeds. Every plant-based food contains hundreds of chemicals called phytochemicals. These are not nutrients, but substances that may, alone or in combination, affect many of the processes thought to be involved in PD including oxidation, chronic inflammation, protein aggregation and mitochondrial dysfunction.
Phytochemicals have not been proven to change disease progression in people with PD, but neither is there typically any harm in eating a diet that includes whole, unprocessed plants. This diet has proven benefits for preventing heart and vascular disease and can reduce PD symptoms, like constipation and risk of cognitive change.;
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Also Check: Does Parkinson’s Show Up In Blood Work
The Gi Infection Link
A study published in the Journal of Innate Immunity found that acute and chronic upper gastrointestinal tract infections seem to be linked to Parkinsons disease.
According to researchers at Georgetown University Medical Center, along with collaborators at the National Institutes of Health and other institutions, upper GI tract infections release S.
This causes a naturally occurring immune response. But when infections are regular or chronic, they may inhibit the body from clearing S, which may lead to developing the disease.
Dr. Michael Zasloff, professor of surgery and pediatrics at Georgetown University School of Medicine, and scientific director of the MedStar Georgetown Transplant Institute, said scientists already knew that S accumulation is tied to Parkinsons.
Prior to performing the research, Zasloff said researchers thought S was a bad player, but its actually good because it is produced when the nervous system detects a potential pathogen.
When the protein is secreted into tissues, it attracts white blood cells that can neutralize the pathogen.
By this means the nerve can protect both itself and the surrounding tissues, he told Healthline.
But too much S, which can occur with regular infections, can become toxic to the system.
What Causes Parkinsons Disease
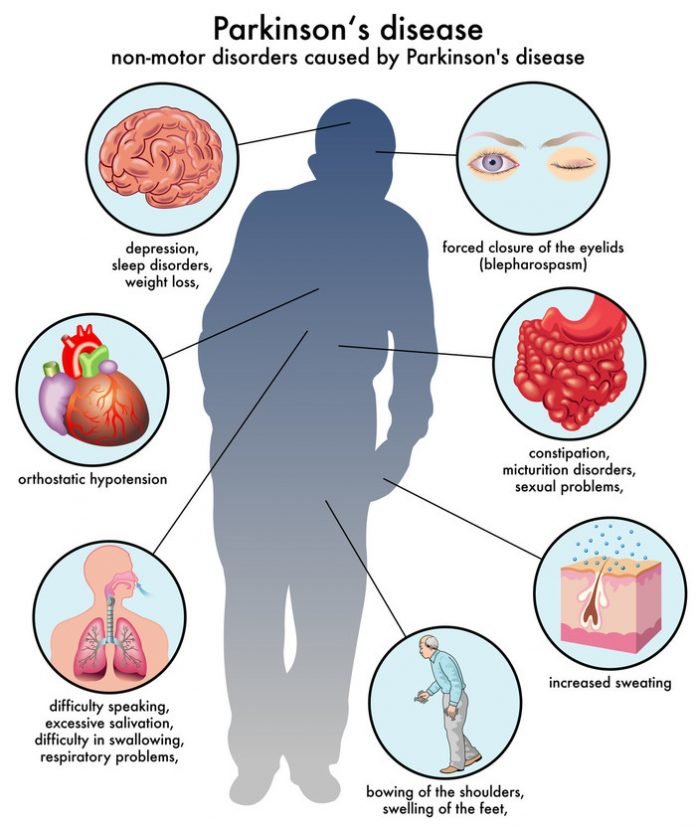
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
Recommended Reading: How Common Is Parkinson’s Disease
What Is Parkinsons Disease
Parkinsons disease is a nervous system disease that affects your ability to control movement. The disease usually starts out slowly and worsens over time. If you have Parkinsons disease, you may shake, have muscle stiffness, and have trouble walking and maintaining your balance and coordination. As the disease worsens, you may have trouble talking, sleeping, have mental and memory problems, experience behavioral changes and have other symptoms.
Protein And The Brain
Protein helps our bodies to carry out key functions to stay healthy, including looking after our brains.;
Our brains are made up of neurons cells which transmit information around the body. They use proteins to communicate with each other.
The amino acid tyrosine is found in many different foods. It is needed in the brain, along with nerve cells, to help produce a chemical called dopamine. People with Parkinsons dont have enough dopamine because some of these nerve cells have died. We dont yet know exactly why this happens but researchers think its a combination of genetic and environmental factors.
Read Also: What Percentage Of Parkinson’s Patients Develop Dementia
Dietary Protein And Parkinsons
This known interaction between levodopa and amino acids in the gut means that people with Parkinsons need to be careful about their protein consumption around the time of taking their medication.
When you have a large amount of protein, they get broken down in the stomach into amino acids. And once these amino acids enter the small intestine, they start competing with levodopa to use the transporter system out into the blood. This competition can cause a reduction in the amount of levodopa reaching the brain, in turn reducing the effectiveness of the dose.
An early study, from 1987, found that on a low protein diet, 11 people with Parkinsons were more sensitive to the effects of levodopa, and saw reduced fluctuations in their symptoms throughout the day compared with a high protein diet. However, we now know that a low-protein diet is not advisable for people with Parkinsons. So, whats the answer?
The Investigation In Mice
In their recent study paper, the scientists refer to research suggesting that neurotrophic factors molecules that help neurons survive and thrive could, in theory, restore the function of neurons that produce dopamine. However, the clinical benefit of these factors had yet to be proven.
The team focused on bone morphogenetic proteins 5 and 7 . They had previously shown that BMP5/7 has an important role in dopamine-producing neurons in mice.
In the latest study, the scientists wanted to see whether BMP5/7 could protect the neurons of mice against the damaging effects of misfolded alpha-synuclein proteins.
To do this, they injected one group of mice with a viral vector that caused misfolded alpha-synuclein proteins to form in their brains. They used other mice as a control group. The scientists then injected the mice with the BMP5/7 protein.
Recommended Reading: What Stage Is Freezing In Parkinson’s