So What Can You Do To Manage Freezing
- If you find yourself getting stuck in particular places, try changing the layout of your living space. Freezing can occur because you have to pivot around furniture.
- Exploring rhythm helps you to maintain momentum where you previously got stuck. Some Parkinsons patients explore strategies like dancing, counting, marching, and shifting their weight from side to side.
Thinking outside of the box can assist you in unfreezing yourself. Dad finds that his posture can affect whether or not hes able to unfreeze himself: When I freeze, I stand up straight. If I move away from gravity, I can unfreeze. But if Im hunching over, gravity pulls me toward the floor and it takes longer to get out of the freeze. And once I move my left foot forward, I can unfreeze. Freezings scary. Thats why a lot of Parkinsons patients fall.
Analysis Of Slopes In Preferred Condition For Pd + Fog Group And Its Relation To Freezing Of Gait Episodes
To address the hypothesis that the negativity of the sequence effect could predict freezing episodes, the preferred and SL25 conditions were compared for the presence of FOG, as most of the freezing episodes occurred in the SL25 condition. The SL100, SL75 and SL50 conditions were not included in the subsequent analysis as the majority of PD + FOG participants did not exhibit FOG in these conditions. There was a significant negative relationship between the number of freezing episodes and the preferred average slope , indicating the number of episodes increased as the -value of the slope in the preferred walking trials decreased .
Further correlation analyses were conducted comparing the total number of FOG episodes with clinical measures . It was found that freezing in SL25 correlated strongly with duration of disease . The remainder of the results demonstrated that the number of freezing episodes did not correlate significantly with H&Y, UPDRS III motor scores, FOG-Q, MMSE or GDS scores.
What Is Parkinsons Disease
Parkinsons disease is a progressive brain disorder that affects mobility and mental ability. If you or a loved one has been diagnosed with Parkinsons, you may be wondering about life expectancy.
According to some research, on average, people with Parkinsons can expect to live almost as long as those who dont have the condition.
Confinement To Bed Or Wheelchair Unless Aided
The patient may exhibit: inability to arise from a chair or get out of bed without help; a tendency to fall when standing or turning; freezing, stumbling or pulsion when walking. Without someone immediately present to provide assistance, the patient is in danger of falling.A typical example of diagnosis using this method of staging would be: a 64 year old with Stage III PD, more marked on the left than the right, of seven years duration. Another would be: A 55 year old with severe fluctuations in response to Sinemet, with PD of Stages II/IV, of ten years duration. The second example indicates that the patient is at Stage II when at his best or on and at stage 3 IV when at his worst or off. This gives the reader a succinct description of the progression of the disease and the current status of the patient.This method of grading severity is rather a potpourri, combining the symptoms of the patient, the physical signs as observed by the physician and the patients functional ability. In some instances, it is not applicable. For example, while general experience has been that is the onset of disturbances of balance that heralds future disability, some patients may have such severe tremor that they are incapacitated even though balance in intact. Others may have mild disturbance of balance for many years without losing independence. There are occasional patients who are more incapacitated by severe unilateral disease than are others by milder bilateral disease.
If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229
Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
Differences In Eeg Between Pdfog+ And Pdfog
Table 1 summarizes the studies that focused on differentiating PDFoG+ vs. PDFoG for developing potential biomarkers. For PDFoG+ the LRP in EEG was shown to have an earlier onset and a larger magnitude during cognitive decision-making of target detection compared to PDFoG. These findings support the second mechanistic hypothesis, which states that dual-task-triggered FoG events are caused by the loss of automatic updating of motor programs by the dysfunctional BG . In terms of EEG frequency band analysis, the beta band was shown to increase in the frontal region during lower limb pedaling in PDFoG+, indicating preparatory adjustments and motor plan execution through top-down signaling . Also, for PDFoG+ theta band power was attenuated in the mid-frontal location, indicating an impairment in cognitive control . In the study that used the dual-task oddball paradigm, although the stimulus was detected by an increased P300, beta ERD was unchanged for PDFoG+. The inability of PDFoG+ to react to stimuli might have been caused by impairments at the BG. The BG impairments were suggested to be caused either by reduced input to the sensory-motor cortex or by the hypersynchronized thalamocortical activity. Additionally, the duration of beta ERS was found to be longer after the cue signal in the PDFoG+ compared with PDFoG .
Table 1. What differentiates PD with and without FoG?
Validation Study: Progression Of Thalamic Local Volumes In Ppmi Cohort
Twenty-four FOG converters and a hundred and one non-converters across a five-year follow-up were included from the PPMI cohort in this analysis. Linear mixed models evaluated the effect of group on local volume progression within the three thalamus clusters. No significant results were found between converters and non-converters in the two study-entry clusters on the left and right thalamus. However, for the longitudinal cluster on the left thalamus, a significant main effect of group was found, as well as significant interactions between years of follow-up and group , and between its quadratic term and group . Importantly, although converters showed local deflation compared to non-converters in this cluster within the observed follow-up , the sign for the interaction between group and years of follow-up quadratic effect was positive, signaling that local volume increased to a greater extent in converters over time . Further, local volume in this cluster was significantly associated with lower dopamine transporter uptake in the right putamen and tended to be associated with lower dopamine transporter uptake in the left putamen , but higher dopamine transporter uptake in the left caudate .
Does Anxiety Cause Freezing Of Gait
Although baseline levels of anxiety were not different between groups, anxiety induced during the walking paradigm was significantly amplified in Freezers beyond the level of Non-freezers. This would suggest that in Freezers, goal-oriented movement has the potential to induce greater anxiety, leading to a cautious and potentially maladaptive movement response such as freezing of gait. Thus, in other circumstances such as walking in darkness, or approaching doorways and narrow spaces, the anxiety-driven need for cautious movement might explain the occurrence of freezing in these situations. One might question whether freezing precedes anxiety or if anxiety does in fact lead to a freeze episode. Panic attacks and heart rate increases have been identified prior to and during a freezing episode. However, inferring a causal relationship would be difficult since there was no manipulation of anxiety-inducing conditions. Rather, associations make it ambiguous as to whether panic attacks and autonomic responses provoke freezing of gait or are a reactive response. The current findings support and extend this research, demonstrating that anxiety is in fact a cause of freezing of gait rather than simply a response, since manipulations of anxiety directly influenced the amount of freezing of gait participants experienced. Spatiotemporal gait changes , which have been previously linked with freezing behaviour, were also increased when anxiety was heightened.
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinsons disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
Literature And Research Methods
Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement , the eligibility criteria for articles included those published before March 2020, written in English, and currently published journal or full-length conference articles. PubMed was used as the primary information source with the search query EEG OR LFP AND Parkinson’s Disease AND Freezing of Gait. The search query was conducted by two independent authors who then combined the findings. This search yielded a total of 34 articles, 10 of which were removed. Six were removed because the terms Freezing of Gait,EEG, or Parkinson’s Disease were used in the introduction but not as part of the research objective . The other four were removed because the articles did not focus on electrophysiology for its methods , because the article was either a poster abstract and not yet a full publication , or because the article did not deal with human subjects . To complement the neurophysiology review aspect of this paper, in addition to the articles found through the PubMed search, sources such as Scopus or Google Scholar were used when clarification was needed.
Caregiving In The Late Stages Of Parkinsons Disease
In late-stage PD, patients have significant mobility challenges. Caregivers likely need to provide more hands-on assistance to help them get around the house. Its important that caregivers learn safe and effective methods to provide help without injuring themselves. Physical therapists can be a great resource to assess an individual situation and teach effective ways of giving assistance.3
Freezing, a sudden but temporary inability to move, can become more common in late-stage PD. Freezing often happens when initiating movement or navigating around obstacles, and freezing episodes contribute to falls. Caregivers can help their loved one overcome freezing by providing a visual cue to step over, like a laser pointer, or using music or rhythm for the person with PD to walk to.3
Late stage PD can make daily activities, such as getting dressed, much more challenging. Caregivers can make getting dressed easier by ensuring adequate time to account for slow movement, choosing a time when medications are “on” and working well, and assembling all necessary items close to the person. Allowing the person with PD to do as much as they can gives them a sense of participation in the process.3
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinsons disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
Techniques To Overcome Freezing
Physical therapy and occupational therapy can be helpful to reduce or overcome freezing episodes. Physical therapy focuses on the physical rehabilitation of people recovering from injuries or disease with the goal of restoring mobility, as well as educating patients on managing their condition to maintain long-term benefits. Occupational therapy also deals with rehabilitation and motion but is focused more on enabling the person to engage in daily activities as seamlessly as possible. Occupational therapists also suggest adaptations and modifications to the persons environment.3
There are several techniques that can help people with PD overcome freezing, including:
As with any symptom, patients who experience freezing episodes should mention this to their neurologist who is managing their care. The neurologist may make changes to medication or provide a referral to a physical or occupational therapist.
What Can I Do As A Caregiver
Freezing is completely involuntary. Rushing the person, getting impatient or saying things like lets go or hurry up can prolong freezing periods.
Instead, wait a few seconds for the person to find and implement a strategy to overcome the episode. If they do not succeed on their own, help them. For example, you can put your foot in front of them so they can step over it, or you can sound out a beat or rhythm .
Do not try to pull the person forward as they can fall, but you can help them with weight transfer movements from one leg to the other.
What Freezing Is Like For My Dad
Like many Parkinsons patients, my dad notices that he usually only freezes when hes not on his medication. It usually happens while hes moving through doors: When you pivot youre worried about losing your balance. Thats why we shuffle our feet and take baby steps initially. Once Im moving Im fine, he says.
Since hes worried about maintaining balance while navigating, its possible that theres a connection between fear and freezing. Continuous motion seems to bypass the risk of freezing, while shifting motion types can present challenges.
Walking With Parkinsons: Freezing Balance And Falls
Parkinsons disease can change the way a person walks. Movement Symptoms like stiff muscles, rigidity and slow movement make it harder to take normal steps. In fact, short, shuffling steps are a common sign of PD, as is freezing, the feeling that your feet are stuck to the floor, for people with mid-stage to advanced PD.
On their own, these changes are distressing enough. But add the fact that Parkinsons affects balance and they also become dangerous, putting people with PD at risk of falling. The good news is that with exercise and physical therapy, people with PD can improve their balance. What can you do to minimize freezing and avoid falls? Read on to find out.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about Parkinsons-related freezing, balance and falls hosted by Fay B. Horak, PhD, PT, Professor of Neurology at the Oregon Health & Science University, a Parkinsons Foundation Center of Excellence.
Coping With Freezing In Parkinson’s Disease
editorial processClaudia Chaves, MD
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Around half of people who have Parkinson’s disease experience freezinga temporary inability to move that occurs suddenly and without warning. Such episodes are short-lived, lasting from a few seconds to up to several minutes.
Parkinson’s freezing can affect nearly any part of the body and disrupt nearly any activitychewing for example, or writing. However, it most often occurs when someone is walking, causing them to feel as if their feet are glued to the ground even though the upper part of their body is still mobile. This sometimes is referred to as freezing of gait and can have repercussions ranging from a brief disruption in stride to an increased risk of falling that can lead to broken bones and other injuries.
The exact physiological cause of freezing in Parkinson’s has yet to be determined. What is known is that it’s often associated with lulls in the effectiveness of medication, particularly among people who have mid-to-late stage disease. There also are a number of common triggers of freezing while walking, such as changing direction, approaching a doorway, or navigating a crowded area. Although Parkinson’s freezing can have a negative impact on a person’s quality of life, there are simple and effective ways to manage it.
What Causes Freezing
Not everyone with Parkinsons experiences freezing, and the exact cause of freezing is unknown. But our relationship to balance gives insight into potential causes. Parkinsons patients experience changes in the brain that affect the way they walk.
Dr. Howard Weiss, in his blog for the Parkinson Foundation of the National Capital Area, writes, Freezing of gait is often triggered by specific activities or circumstances that demand switching between motor actions. While learning to walk, we strengthen the neural pathways that allow us to balance. But Parkinsons patients see a degradation of these pathways, leading to difficulty in stabilization.
What You Can Do
As of 2021, there is no definite cure for Parkinsons disease. There is also no definite known cause. Its likely due to a combination of an individuals susceptibility and environmental factors. Most cases of Parkinsons disease happen without a genetic link.
According to research published in 2012, only report having a family member with the disease. Many toxins are suspected and have been studied, but no single substance can be reliably linked to Parkinsons.
However, research is ongoing. Its estimated that
Bilateral Or Midline Involvement Without Impairment Of Balance
Months or years later similar symptoms and signs are noticed on the opposite side of the body, or other signs appear in midline what physicians call Axial signs. These may include: bilateral loss of facial expression ; decreased blinking; speech abnormalities; soft voice, monotony, fading volume after starting to speak loudly, slurring, stiffness of truncal muscles making the patient appear awkward and stiff or resulting in neck and back pain; postural abnormalities causing stooping, generalized slowness in, but still capable of, carrying out all activities of daily living, sometimes an aggravation to those waiting for the patient to complete tasks.
Usually the diagnosis is easy at this Stage if it has been preceded by a clear cut tremor or other symptom on one side. But not all Parkinson’s patients have tremor or other definite signs of Stage I unilateral Parkinsonism. If Stage I was missed and the predominant symptoms at Stage II are only slowness and a lack of spontaneous movement, the diagnosis may still be in doubt. For example, even in Stage II, Parkinsonism may be interpreted as only advancing age.
Does Anxiety Cause Freezing Of Gait In Parkinson’s Disease
-
Affiliations Sun Life Financial Movement Disorders Research and Rehabilitation Centre, Wilfrid Laurier University, Waterloo, Ontario, Canada, Cognitive Neuroscience, Department of Psychology, University of Waterloo, Waterloo, Ontario, Canada
-
Affiliation Cognitive Neuroscience, Department of Psychology, University of Waterloo, Waterloo, Ontario, Canada
-
Affiliation Sun Life Financial Movement Disorders Research and Rehabilitation Centre, Wilfrid Laurier University, Waterloo, Ontario, Canada
Negative Consequences Of Freezing
Freezing episodes limit the mobility of a person with PD and may contribute to reduced socialization and a lower quality of life. In addition, freezing can be dangerous and is associated with falls in people with PD. Approximately 38% of people with PD fall each year, and freezing increases the risk of falls as freezing occurs without warning. Falls can cause additional health problems, including broken bones or head injury.1,2
About Dr Sarah King Pt Dpt
Sarah is a passionate Parkinsons advocate who founded Invigorate Physical Therapy & Wellness, an online wellness practice 100% specialized in Parkinsons disease, to help her clients get out of overwhelm and into action by connecting them with the tools and support they need to thrive over the course of their Parkinsons journey. She lives in Austin, Texas with her husband , Matt.
Sarah will also be joining us for the Victory Summit® event in Austin, TX on Saturday, April 13, 2019. If youd like to join us and meet Sarah in person, you can register for this free event here.
Analysis Based On Average Slopes In Each Condition Across All Groups
The sequence effect, as measured by the regression slopes, of all three groups was included in this section of the analysis. One participant in the PD + FOG group, who experienced severe blocking, was excluded in this analysis because individual footsteps could not be identified in all four trials. Regression slope for one trial in the preferred condition could not be calculated for another participant in the PD + FOG group.
Table 4 demonstrates that the slopes for the PD + FOG group were substantially greater than those in the PD FOG and control groups across conditions, particularly at the reduced step length. Using scores for UPDRS , H&Y, GDS and disease duration as covariates in the analysis, there were no significant differences between groups reported in the preferred and SL100 conditions . However in the SL75, SL50 and SL25 conditions the PD + FOG group demonstrated a significantly higher -value compared to the PD FOG and control group. Tukey’s HSD test confirmed the difference in was located in the PD + FOG group, when compared with the PD FOG and control group. The PD FOG and control group did not differ in the -values across conditions.
Figure 2 displays the regression slopes for walking trials 1 and 3 in the SL25 condition, for a single age-matched participant in the PD + FOG group , PD FOG group and control group .
Mri Processing Shape Analysis
Vertex-based analysis of fifteen subcortical structures was performed using FMRIB Software Librarys FMRIB Integrated Registration and Segmentation Tool . This automated method has been validated in healthy and patient populations with high retest reliability over repeated measurements, particularly for segmenting the striatum. Deformable mesh models were fitted to the surface of each structure and local and global volumes were calculated. Local volume quantifies subregional shape variations on the surface of a nucleus calculated as the scalar distance of an individuals vertices to the mean sample vertices. Global volume quantifies the total volume of the nucleus calculated as the volume within the surface mesh. A change score for each participant was calculated as Scan2 Scan1, so positive values imply inflation in local volume or an increase in global volume over the two years.
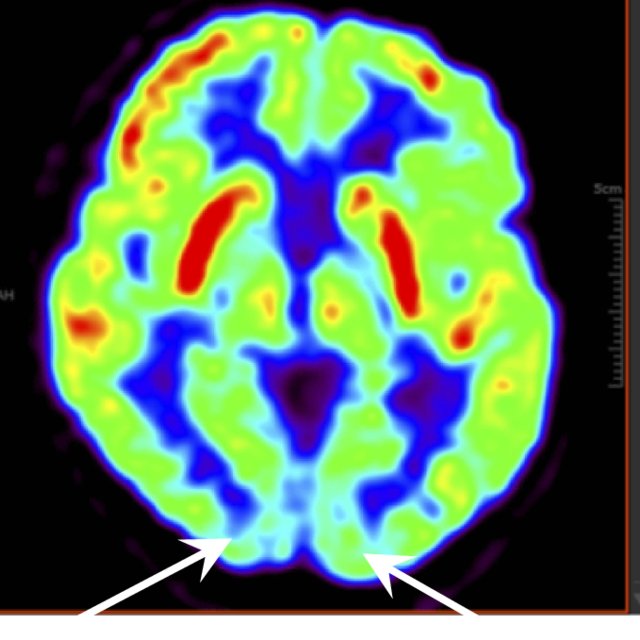
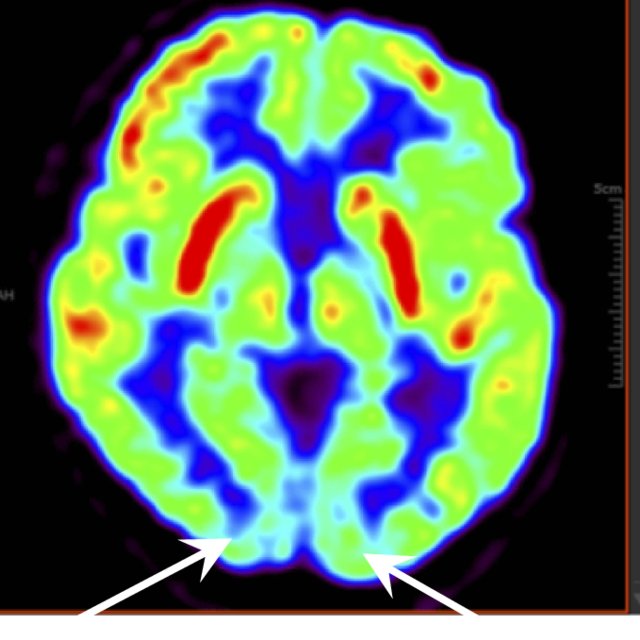
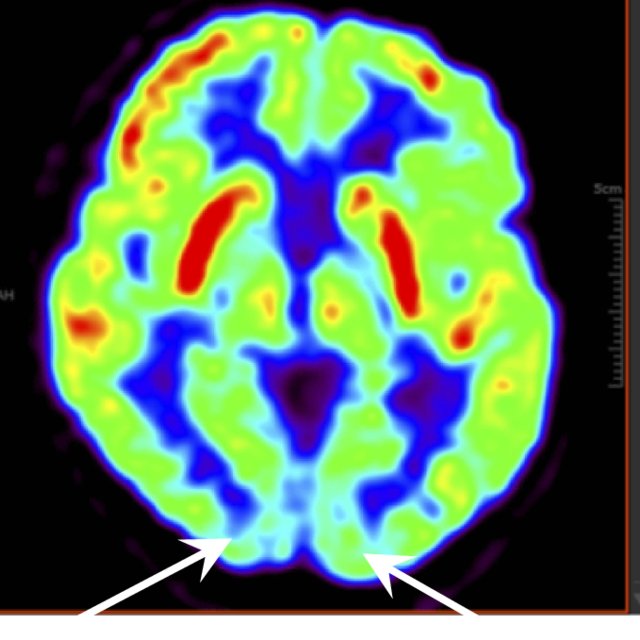
Pathophysiology Mechanisms Underlying Fog
Locomotion is a complex process that involves automatic, emotional, and volitional control . In non-automatic gait, the initiation command is generated at the cerebral cortex and is executed by the thalamocortical, corticobulbar, and spinal projections networks . Automatic rhythmicity, posture preparations, and adjustments during locomotion are regulated by the brainstem and spinal cord after gait is volitionally initiated. Meanwhile, the cerebellum simultaneously takes in the sensory feedback from the spinal cord and feed-forward information from the cortex to regulate predictive control . In PD, multilevel network failure may ultimately lead to FoG events. However, the neural complexity leads to uncertainty in identifying and isolating specific neural impairments that result in FoG. To explain the pathophysiology, five non-exclusive mechanisms have been suggested regarding the physiological alterations leading to FoG .
The fifth hypothesis states that FoG is a consequence of frontal executive dysfunction, where there is a disconnect between the BG and the frontal lobe, resulting in poor performance when trying to achieve multiple tasks . This is further supported by low scores in frontal assessment battery scores and verbal fluency in PDFoG+ compared to PDFoG . Extra-nigral pathology impairs compensatory attentional gait strategies and contributes to L-dopa-resistant FoG, especially with PD progression .
