Effectiveness Of Ropinirole And Gabapentin For The Treatment Of Rls In Patients On Maintenance Hd
| The safety and scientific validity of this study is the responsibility of the study sponsor and investigators. Listing a study does not mean it has been evaluated by the U.S. Federal Government. Read our disclaimer for details. |
| Recruitment Status : Suspended First Posted : October 17, 2018Last Update Posted : March 25, 2020 |
Study DescriptionArms and InterventionsOutcome MeasuresEligibility CriteriaContacts and LocationsMore Information
Restless legs syndrome is a neurologic disorder characterized by 1) an urge to move the legs, 2) uncomfortable sensations in the legs, 3) symptoms that are often worse the evening or when at rest , and 4) may be temporarily relieved by physical activity.
The overall prevalence of RLS in the general population is estimated to be around 10%, however, it is significantly in the end stage kidney disease population is significantly higher . Studies have shown that RLS has a substantial negative impact on both the physical and the mental health dimensions of quality of life , such as depression, anxiety, pain, fatigue and sleep disorder.
This study aims to evaluate effectiveness of ropinirole and gabapentin for the treatment of restless legs syndrome in patients on maintenance hemodialysis.
Purpose
This study aims to evaluate effectiveness of the off-label use of ropinirole and gabapentin for the treatment of restless legs syndrome in patients on maintenance hemodialysis.
Hypothesis
Justification
Primary Objectives
Quarterwatch Focus On Three Psychoactive Drugs: Gabapentin Pregabalin And Pimavanserin
The latest issue of ISMP’s QuarterWatch™ focuses on two older but widely used analogs of the inhibitory gamma-aminobutyric acid neurotransmitter and a new type of antipsychotic medication approved for Parkinson’s disease psychosis. Key findings include:
-
Extensive patterns of potentially unsafe use of the GABA analogs, gabapentin and pregabalin
-
New questions about both the safety and benefits of pimavanserin
The following is a summary of the full QuarterWatch™ report, which can be found, with additional references by .
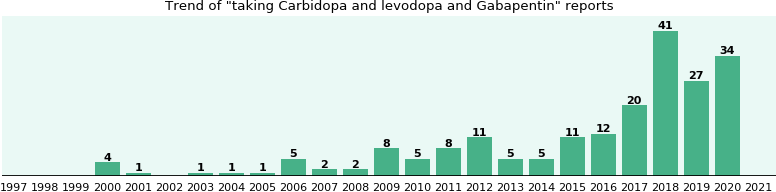
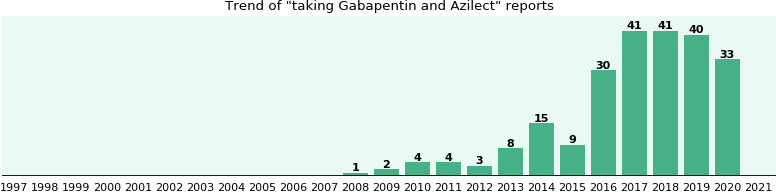
Can Gabapentin Be Taken With Parkinsons Meds Iecarbidopa/levadopa Azilect Mirapex
- Asked
- 31 Mar 2011 by rosadelgado1
Marvell
I realize this answer is very late but may be helpful in future.
Yes, gabapentin can be taken with the medicines listed above but with caution and the doctor must weigh the risks verses benefits. There is potential for interaction and the patient must be monitored.
Please see link below for interaction in detail.
What Is The Effectiveness Of Gabapentin In The Treatment Of Essential Tremor
A double-blind, crossover trial comparing gabapentin with propranolol found that both drugs demonstrated significant and comparable reductions in tremor compared with baseline. However, a double-blind, placebo-controlled, crossover study identified no difference between gabapentin and placebo.
What Are The Different Types Of Pain Experienced By People With Parkinsons
Five main types of pain are common for people with Parkinson’s. Multiple types may be present simultaneously or occur at different points throughout a person’s path with Parkinson’s. Recognizing which kind of pain is present can help you optimize treatment, as can paying attention to what activities or times of day make your pain better or worse.
Musculoskeletal pain
Musculoskeletal pain that affects muscles, bones, tendons, ligaments, and/or nerves. The pain can be localized or generalized and can fade or intensify at different times. Existing musculoskeletal pain can be exacerbated by Parkinson’s.
Neuropathic pain
Rather than being caused by a physical injury, this type of pain is caused by damage to the somatosensory nervous system or a disease affecting the somatosensory nervous system, which responds to external stimuli like touch, temperature, and vibration. It tends to be fairly consistent throughout the day and is present no matter what activity you’re doing. Unlike the aching you may feel when you’re doing a strenuous physical activity, neuropathic pain feels more like a tingly, crawly, uncomfortable sensation.
Dystonic pain
Dystonia, the movement disorder in which involuntary muscle contractions cause repetitive or twisting motions, is often very painful. Many people with Parkinson’s experience dystonia as a motor symptom, whether it’s localized , in multiple nearby body parts , or all over .
Akathisia
Central pain
Therapies For Pain In Parkinson Disease: Concerns Related To A Meta
Department of Oral and Maxillofacial Pathology, Radiology, and Medicine,
New York University College of Dentistry
380 Second Avenue, Suite 301, New York, NY 10010
E-Mail kgr234@nyu.edu
Dear Editor,
As an academic clinical research scientist studying pain conditions for several decades and as a person who has lived with Parkinson Disease for more than 8 years, I was initially delighted to see the review and meta-analysis by Qureshi et al. concerning treatment of pain in PD. Good quality meta-analytic reviews can help to reconcile inconsistent findings and small-sample studies within a field. Evaluating best treatments for pain in PD is particularly important, as pain is the most troublesome nonmotor symptom in early-stage PD . It may often precede the onset of motor symptoms .
Unfortunately, I fear that this meta-analysis does little to advance treatment of pain in PD. Why? Inherently, to justify combining across different studies, an assumption must have been made that “Parkinson’s Pain” is a uniform entity.
The fact that all of these distinct types of pain can be measured on a visual analogue severity scale or other severity scale does not justify collapsing across different types of pain when conducting a meta-analysis. Surveys suggest that the most prevalent type of pain in people with PD is musculoskeletal . Relative high representation of musculoskeletal pain may obscure the efficacy of treatments for less common types of pain in patients with PD.
Parkinsons & Restless Leg Syndrome: Using Dopaminergic Medication
Because RLS is well-treated by medications that also treat PD, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in PD, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that DaTscan results are not abnormal in RLS.
Using dopaminergic medications to treat RLS however can be tricky. In some people they can lead to a phenomenon known as augmentation, in which long term use of dopaminergic medications can worsen the symptoms – making them appear earlier in the day or migrating to the upper body in addition to the legs.
Innovative Treatment Modalities For Managing Pain In Parkinson’s
Botulinum toxin
Non-dopaminergic pharmacotherapy may benefit patients with PD-related pain. Botulinum toxin , both A and B derivatives, should be considered in patients who do not respond to dopaminergic treatment optimization.1,8 Botulinum toxin injection provides localized treatment by blocking the release of acetylcholine at the neuromuscular junction.4 Local injections of BTX type A or B can be effective for persistent dystonia-related pain and central pain, based on its neuromuscular action in movement disorders plus analgesic mechanism.
A randomized, double-blind, crossover, placebo-controlled trial concluded that BTX-A in patients with PD is safe and potentially useful in treating limb pain.29 The study was conducted in patients with PD over the age of 30 years with painful limbs not responding to the optimization of anti-Parkinsonian medications. Patients were randomized to receive BTX-A injection or placebo, followed by the other treatment per the crossover design. Depending on the location of pain, patients received up to 200 units in upper limbs or up to 300 units in lower limbs. Patients experienced a significant reduction in their self-reported numerical pain score 4 weeks after the BTX-A injection , but not with placebo . There was no difference between the change with BTX-A compared to placebo . This study demonstrated that targeted BTX-A injections are safe in patients with PD.
Cannabinoids
A Critical Reappraisal Of The Worst Drugs In Parkinsons Disease

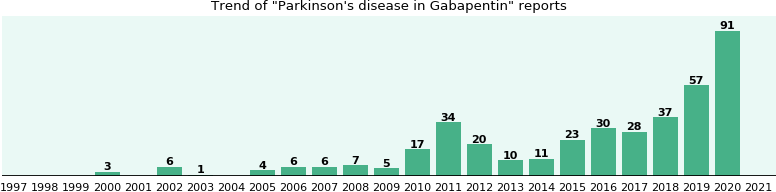
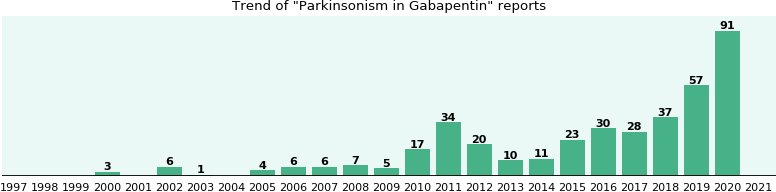
What are the worst drugs for Parkinson’s disease patients? Couldn’t a simple list be assembled and disseminated to the Parkinson community? Recently Ed Steinmetz, an experienced neurologist in Ft. Meyers, FL pointed out to me, a list approach published in the Public Citizen Newsletter . The approach was to list every drug associated with a single confirmed or unconfirmed symptom of Parkinson’s disease or parkinsonism. Parkinson’s disease is defined as a neurodegenerative syndrome , whereas parkinsonism encompasses a wider net of drug induced and other potential causes. In parkinsonism symptoms are similar to Parkinson’s disease, but patients do not have Parkinson’s disease. Patients and family members confronted with a simple “drug list” approach may falsely conclude that most medicines are bad for Parkinson’s disease, and that any medicine may cause parkinsonism. This concept is in general, incorrect. Although the approach is well-meaning, it is in need of a major revision, as Parkinson’s disease and parkinsonism are too complex to summarize by simple lists. In this month’s column I will try to summarize the key information that patients and family members need to know about the “worst pills,” for Parkinson’s disease and parkinsonism.
A Florida Parkinson’s Treatment Blog by Michael S. Okun, M.D.
UF Center for Movement Disorders & Neurorestoration, Gainesville FL
Discuss The Latest Research In The Parkinsons News Today Forums
Cora’s father is a PD patient and has taken Mirapex for two years. During this time, he developed serious gambling problems, delusions, and hallucinations.
Meanwhile, Jim had been taking Mirapex for restless leg syndrome , often a complication of PD. He read up on some undesirable side effects that included compulsive gambling, excessive spending, and compulsive, excessive sexual behavior.
What disturbed Jim most was that patients taking Mirapex often are unaware that a change is occurring. Jim began engaging in several of these atypical behaviors. He was unaware that they were actually becoming addictive behaviors. Fortunately for Jim, his doctor recognized that Mirapex was causing the addictions. Jim thought he was the only one with these side effects until his doctor put him in touch with Carl.
Carl first noticed his bowel movements had changed and constipation was regular. He gained 40 pounds in the first five months and couldn’t sleep. He understood it was the medication but had another issue: He was embarrassed by the things he couldn’t seem to quit doing. He never read the informational insert inside the drug box. He was just following the doctor’s orders.
Carl began to lose control sexually, and his internet use became an outlet for improper behavior. He was ashamed and felt isolated in his problem. He went to see a new neurologist and discovered he wasn’t alone. Several other PD patients who were prescribed Mirapex were dealing with similar issues.
***
Pain Is An Unfortunately Common Problem In Parkinsons Disease
Of course, pain is common in the general population, especially among older people. A recent American study found that pain affected about twice as many people with Parkinson’s Disease than those of the same age and gender without PD. About 50% of Parkinson’s Disease patients in that study suffered from painful disorders. Men and women seem to be about equally affected. A very well described scenario is the patient who is followed for a painful frozen shoulder for a year or so before a tremor develops leading to a diagnosis of PD. Pain clearly plays a major role in quality of life. Everyone with chronic pain enjoys life less, leading to a vicious cycle in which pain causes depression or isolation which in turn leads to more pain.
Parkinson patients suffer from the same pain problems that other people have, often amplified by the motor dysfunction, but they also have additional pain problems which are unique to PD.
One recent review classified the types of pain Parkinson’s Disease patients have into: musculoskeletal, in which the pain results from problems with the muscles , bones or joints; dystonic, which is due to abnormal muscle contractions caused by the Parkinson’s Disease or the medications used to treat it; radicular pain, which is feels like the pain caused by pinched nerves; central pain, which is presumed due to abnormalities in the brain, and is a continuously present pain that cannot be explained otherwise; and discomfort related to an unpleasant urge to move.
Essential Tremor: A Common Disorder With Limited Treatments
Edward M. DeSimone II, RPh, PhD, FAPhAProfessor of Pharmacy Sciences
Jacob M. Crimmins, PharmD CandidateCreighton UniversitySchool of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2011;36:HS-23-HS-27.
Essential tremor is an involuntary movement disorder of unknown cause that lacks a specific set of diagnostic criteria. In addition, pharmacologic treatment is modest, with only one FDA-approved drug and one off-label agent. This condition was believed to be benign, nothing more than a disruption of daily activities and a source of embarrassment. However, recent studies have demonstrated the evolution of ET in many areas. This review discusses the causes, prevalence, diagnosis, and current pharmacologic treatment of ET. In addition, some lifestyle modifications for ET are discussed.
Lower Back Pain And Back Of The Neck Pain Are Most Common
Pain occurs for a number of reasons and it’s not always clear what the cause is, making it difficult to figure out how best to treat it. I believe that most common pain problems in Parkinson’s Disease are the same as in the general population, but amplified. Low back pain and back of the neck pain are probably the most common pain conditions in PD. The reason Parkinson’s Disease patients have so many problems with their low back and their neck is their posture. Parkinson’s Disease causes a stooped posture. Some of this happens with age anyway, particularly in women after menopause when their bones soften, but is always worse from the PD. All Parkinson’s Disease patients have some degree of stooped posture and many also tilt to one side. Because of the stooped posture, the muscles in the lower back have to pull much harder to keep the spine upright.
Rewiring The Brain: Taking A Fresh Look At Chronic Pain
For 15 years, I have been a failure at managing my chronic pain. I was prescribed oxycodone with gabapentin, and after my Parkinson’s diagnosis, I was put on levodopa. This decreased my pain to the point where oxycodone was no longer needed.
I also tried alcohol and marijuana in a rigorous attempt to make the pain vanish, replacing it with “feel-goods.” I know that chasing after “feel-goods” is not the right approach for me, so I stopped all the pain medications except levodopa.
At this juncture, I wish to be clear that I am not recommending anyone stop their medications. This is my personal journey, and I made decisions in consultation with my healthcare providers. For me, the risk of opioid treatment far outweighed the benefits.
Gabapentin in my system dulled my brain to the point that my cognitive abilities adversely affected my quality of life. Only in the last few months have all the pieces finally fallen into place to reveal a fresh approach to chronic pain management.
Chronic pain management is not just about popping a pill and hoping to be pain-free. No matter what I do, I will always have chronic pain from Parkinson’s every day. The goal is to live better. Medications that seek to disguise this reality within the gaudy attire of society’s “feel-good” addictions always send up big, red warning flags for me.
The Parkinson’s chronic pain management program I use incorporates many of these small changes to help me live better. Here is my list:
***
Atypical Parkinsonism Or ‘parkinson’s Plus Syndromes’
“Parkinson’s Plus Syndromes” are less common than Parkinson’s disease.
Some atypical parkinsonism syndromes include:
Multiple system atrophy This is a category of several disorders in which one or more body systems deteriorate.
Your doctor may classify you as having MSA-P, in which parkinsonian symptoms are dominant; or MSA-C, in which dysfunction of the cerebellum is dominant.
The names of some of these syndromes include olivopontocerebellar atrophy , Shy-Drager syndrome , and striatonigral degeneration .
Progressive supranuclear palsy Symptoms of this condition usually begin after age 50 and proceed more rapidly than Parkinson’s disease.
In people with PSP, problems with eye movement can lead to blurry vision. Falls tend to occur early in the course of the disease, and dementia may occur later in the disease.
Corticobasal degeneration This condition may cause jerking and loss of control in a limb, often without weakness in that limb.
If you have this disorder, you may be given Botox to help your limb relax.
Lewy body dementia LBD is the second leading cause of dementia in the elderly, after Alzheimer’s disease.
In this condition, the same Lewy bodies occur in the brain as in Parkinson’s disease, but in multiple areas of the brain.
If you have LBD, you may experience speech problems, hallucinations, and gradual cognitive decline.
Strengthening Exercises Or Stretching May Be Helpful
Imagine that the spine is like a telephone pole or the mast of a sailboat. If the pole is not exactly upright, even a slight tilt requires a great force to keep it from tilting further and falling. In the human body, this means that the lower back muscles are under great stress. It also means that the tension on the back bones is much increased as well. This worsens whatever problems, like arthritis, that are already present. The same process applies to the neck, although the forces are less great. Strengthening exercises or stretching may be helpful. Almost everyone over the age of 60 has arthritis in their spine. Luckily most don’t have pain from it, but those who do will have it worsened by the spine curvature caused by the PD.
PD patients also frequently have an aching discomfort in their muscles, particularly in the thighs and shoulders. I think this is due to the rigidity, or stiffness, that is part of the Parkinson’s Disease syndrome, but I’ve seen many patients with this pain and no apparent stiffness on examination, hence not explained. It is common and it often, but not always, responds to alterations of the usual Parkinson’s Disease medications for movement. Exercise and stretching may be helpful as well and should always be tried first before increasing medications.
Pain is a challenge in PD. We can’t measure it and often cannot find its cause. It is, however, often treatable, and reducing pain improves quality of life.
What Can I Do On A Regular Basis To Manage My Pain
Remember, you’re your best advocate as you understands how your pain feels. Understanding and communicating the kind of pain you’re experiencing can greatly inform your treatment plan and will allow your doctors to address the type and severity of your specific pain. Keep your care team informed about activities that cause pain or the times of day your pain is worst so they can help fine-tune your care plan. Do you notice the pain starting to creep in at a certain point after you take your medication? Do you feel fine when you bike but experience pain when you jog? Did you start experiencing this pain before or after your Parkinson’s diagnosis? Taking stock of these sorts of questions can be helpful as you work with your care team to effectively treat your pain.
Incorporating approved medications and following the pain ladder can also help you find the right pain management solution, as can taking steps in your everyday life to be an active participant in your own pain management. Regular stretching, heat and cold treatments, exercise, yoga, and dance can all help reduce your pain, and they are all steps that you can take on your own. Making adjustments to your home and workspace, such as minimizing places where fall risks are likely, using an ergonomically designed desk, sleeping in a comfortable bed, and wearing clothes and shoes that don’t exacerbate pain, can help you establish a more pain-free daily routine.
Does Having Rls Increase The Risk Of Developing Pd
Since RLS affects as much as 4-10% of the US adult population, it is clear that the vast majority of those with RLS do not ever develop PD.
Despite this, it still might be the case that RLS increases the risk of subsequently developing PD. There have been many studies trying to figure this out – with conflicting results. Some studies show that there is no increased risk and others show that having RLS confers about a two-fold increased risk of developing PD over the general population.
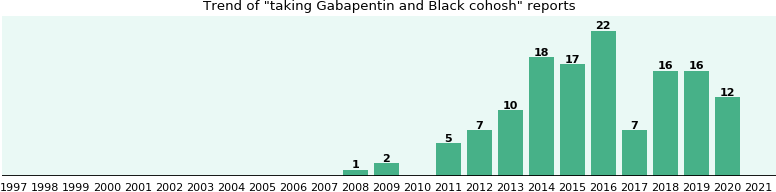
Interactions With Other Medications And Substances
Gabapentin can interact with other prescription or over-the-counter medications, vitamins, and herbal supplements.
Be sure to give the doctor a full list of current medications and supplements before taking gabapentin.
of a 2017 review suggest that the following are the main substances that interact with the drug:
- caffeine, which is present in tea, coffee, and cola
- ethacrynic acid, a diuretic
- seizures
Pain Management Principles In Parkinson’s Disease
Non-pharmacologic methods with a multidisciplinary pain team should be utilized to provide optimal multimodal treatment in patients with PD.4 Muscle relaxation exercises and walking regularly can improve flexibility and dampen experiences of pain associated with motor symptoms.6 Rehabilitation with a physical therapist can improve gait and balance, targeting pain caused by motor symptoms. Surgical interventions, such as deep brain stimulation or an implanted spinal cord stimulator, may be appropriate for those patients experiencing pain with PD who do not respond to pharmacologic or rehabilitation interventions.1,6,9
Optimization of treatment with levodopa and other antiparkinsonian medications should be the first pharmacological step in managing PD-related pain.6,8 Beyond this recommendation, no evidence encourages the use of specific analgesic agents in any stepwise order, making patient input and assessment of pain type critical to appropriate treatment.
Patients should be prescribed analgesics if optimization of dopaminergic agents is not effective on its own .4
Optimization of Dopaminergic Agents
Safinamide is a selective, reversible MAO-B inhibitor that reduces degradation and reuptake of dopamine to increase levels in the striatum.19 Safinamide also has non-dopaminergic properties that modulate glutamate release via inhibition of voltage-gated sodium channels. This dual mechanism may mitigate pain, especially during “off” periods.
Parkinsonism Due To Other Neurological Disorders
The following neurological disorders are known to cause parkinsonian symptoms:
Vascular parkinsonism Also known as arteriosclerotic parkinsonism, this condition is caused by multiple small strokes.
The onset of symptoms can be sudden or gradual, and often includes mobility problems in your legs. Symptoms may level off for a period of time.
Vascular parkinsonism has the slowest rate of progression of all atypical parkinsonisms. It doesn’t usually cause tremors, either.
Post-traumatic parkinsonism Also known as post-traumatic encephalopathy or “punch-drunk syndrome,” this condition may be caused by a severe head injury or by frequent head trauma, such as from boxing or football.
Post-traumatic parkinsonism can lead to a type of dementia called chronic traumatic encephalopathy . In March 2016, the National Football League admitted that there might be a link between CTE and head trauma.
Essential tremor This is a tremor that tends to run in families and become worse over time. It’s usually seen most severely in the hands, especially when the hands are moving.
Normal pressure hydrocephalus This condition is caused by an abnormal increase in fluid in the cavities of the brain.
NPH can sometimes be treated by draining the extra fluid into your abdomen using a shunt.
Environmentally Caused Parkinsonism
The following disorders are caused by outside factors like drugs and infection:
The following substances can cause drug-induced parkinsonism:
How Is Pain Treated For People With Parkinsons
No matter the cause, pain is often complex. When a person with Parkinson’s experiences intense pain, especially in combination with other symptoms of Parkinson’s, managing it can be challenging. There are, however, several ways you can adjust your medication regimen, exercise schedule, and lifestyle to reduce your pain and improve your quality of life.
Medications
There are various kinds of medications used to treat pain, especially for people with Parkinson’s. In a recent webinar, Dr. Janis Miyasaki described how physicians approach pharmacological treatment of pain for people with Parkinson’s:
The principle is to start with what is called the pain ladder. You always start with the least intensive, least side effect-giving treatment.Janis Miyasaki, MD
Step one
The first step of the pain ladder is hot and cold treatments along with stretching and flexibility exercises. People who experience rigidity and stiffness can sometimes alleviate pain using heating pads to loosen their muscles, then improve mobility by stretching, then address any residual pain with ice packs.
Step two
Step three
Step four
Step five
Other medical interventions
Who Should I See To Discuss My Parkinsons Pain
Your first point of contact should be your primary doctor. Whether that means your family doctor, neurologist, or Movement Disorder Specialist , start by asking them how to manage your pain. They may prescribe you one of the medications listed above, offer suggestions about altering your lifestyle, or refer you to a pain specialist.
Pain management specialists are physicians with specialized training in the field of evaluating, diagnosing, and treating pain; so, speaking to one of these specialists might be helpful for you. Be sure to get a referral from your primary care doctor, though, to ensure you are visiting a physician who understands the complexity of treating Parkinson’s-specific pain.
Health and wellness providers like physical therapists, acupuncturists, and massage therapists can also be valuable members of your care team. Be willing to try new things and approach alternative therapies with an open mind, as no one’s path with Parkinson’s pain is the same. What works for someone else may not work for you and vice versa. Consider visiting different specialists to find a treatment plan that works best for you.
Risks During Pregnancy And When Breastfeeding
People who are pregnant, or intend to become pregnant, should tell their doctor before taking gabapentin.
Pregnant women should only take the drug if it is absolutely necessary. However, it is also essential to control seizures while pregnant.
Do not start or stop taking gabapentin for seizure control before talking to the doctor, who will assess the potential risks and benefits.
Gabapentin passes into breast milk, but its effects on babies are unknown. It is best to discuss this issue with a doctor before breastfeeding.
Fda Reassurance Of Pimavanserin Not Warranted
Pimavanserin is approved for treating hallucinations and delusions associated with Parkinson’s disease psychosis. Unlike conventional antipsychotics, its primary effects are on serotonin rather than dopamine receptors. The November 2017 issue of QuarterWatch™ raised concerns about both the safety and benefits of this drug, which were also questioned in FDA’s initial medical review, resulting in an unheeded recommendation to reject the drug.9 Since then, other news media have reported additional safety concerns, notably hundreds of reported deaths in the FAERS data. After these safety concerns were raised in a Congressional hearing, FDA conducted a new safety review of pimavanserin. In September 2018, FDA announced the results of this review in a Drug Safety Communication advising that, “FDA analysis finds no new or unexpected safety risks associated with Nuplazid .”
We obtained the complete FDA safety reviews, new studies, and the most recent 12 months of FAERS data through September 2018 to conduct a reassessment of pimavanserin. Our results? Rather than being reassured about the safety of the drug, we found weak and incomplete data on patient deaths, new questions about efficacy, and a misleading Boxed Warning in prescribing information that did not adequately inform about the possibility of increased risks and death. Here are the highlights of what we found:
Usual Adult Dose For Restless Legs Syndrome
Gabapentin enacarbil available under the trade name Horizant :600 mg orally once daily with food at about 5 PM
Gabapentin can be used to treat the symptoms of restless legs syndrome .1 It may be especially helpful if the symptoms are perceived as less intense yet painful. In individuals with a history of peripheral neuropathy or chronic pain, it may be of added benefit. Furthermore, gabapentin may be helpful to treat RLS in the context of other neurological disorders such as Parkinson’s disease or dementia.
Potentially Unsafe Use Of Gaba Analog Drugs
Gabapentin is approved to treat postherpetic neuralgia in adults and as adjunctive therapy for some forms of epileptic seizures. It is an analog or synthetic form of GABA, a major inhibitory neurotransmitter. A different formulation is approved for postherpetic neuralgia and restless legs syndrome under the brand HORIZANT. Gabapentin is so widely used for other purposes that it is reported to be taken by more adults than any other psychoactive medication except HYDROcodone with acetaminophen.
The other GABA analog, pregabalin, is approved for the same indications as gabapentin as well as for fibromyalgia and neuralgia associated with diabetic neuropathy or spinal cord injury. Pregabalin is less widely used and, unlike gabapentin, it is designated as a controlled substance . Pregabalin is only available as a brand product, Lyrica, which costs 40 times more than gabapentin .
Using data from a large 2016 survey of medical care in the US,1 we evaluated gabapentin and pregabalin patterns of use. We also analyzed the safety profiles of these two drugs using the most recent 12 months of FAERS data and the literature. Through this analysis, we have identified a pattern of potentially inappropriate and unsafe use so pervasive that addressing it should rank as a major public priority.
Characteristics Of Restless Leg Syndrome
There are certain features of RLS that make it a unique and specific disorder.

