A General Rule Is That Dbs Will Likely Improve Parkinsons Symptoms That Respond To Medication
The Evaluation prior to DBS Surgery
A team of experts, including a movement disorder specialist and a neurosurgeon , conduct an extensive assessment when considering DBS for someone. The evaluation consists of medication and symptom review, examination both on and off Parkinson’s drugs, brain imaging, and oftentimes also detailed memory/thinking testing . If DBS is offered, it’s important to discuss the expected benefits as each person’s experience is unique. It’s also critical to discuss the potential surgical risks, including bleeding, stroke and infection.
The DBS Procedure and Device Programming
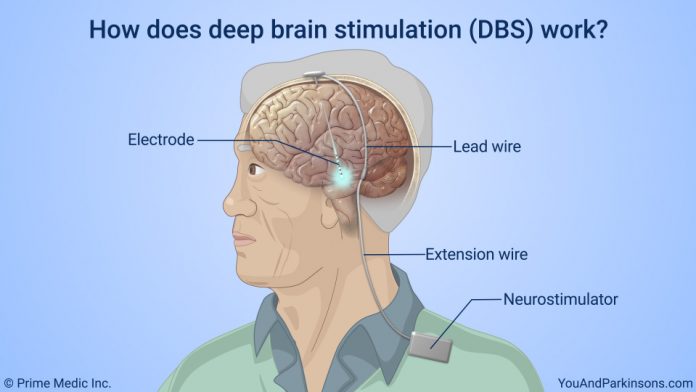
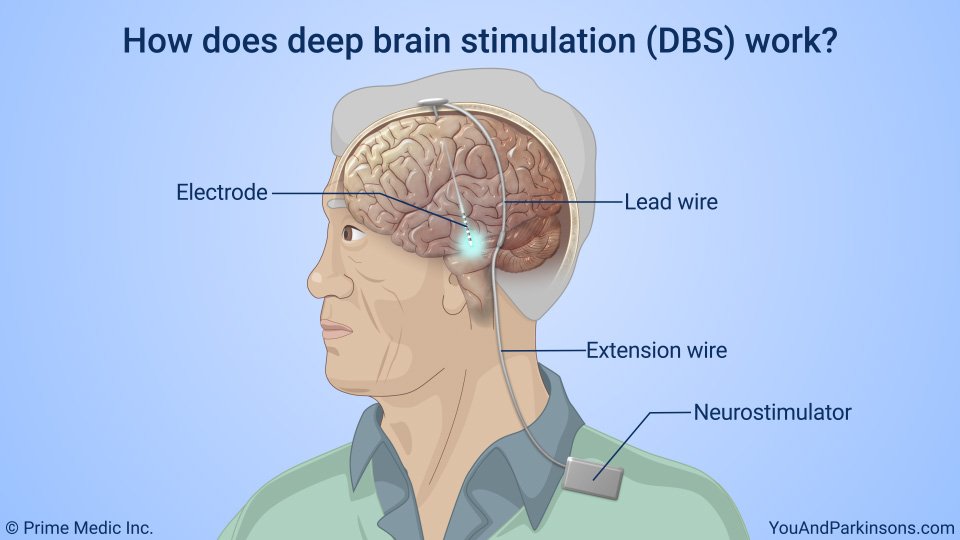
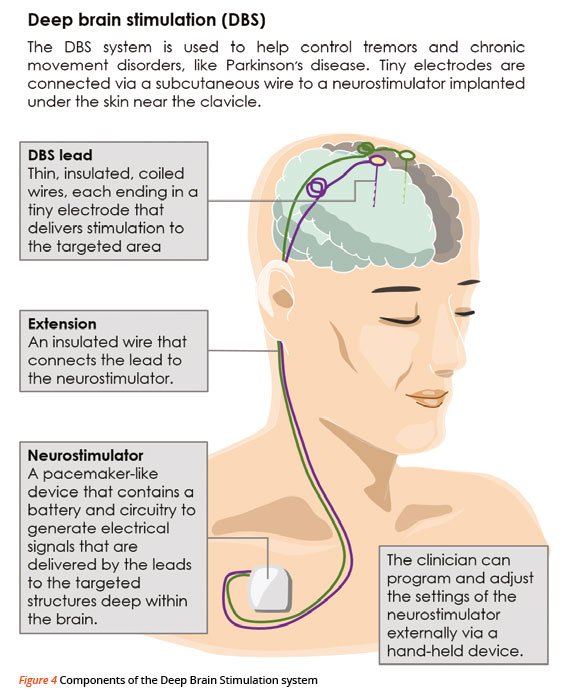
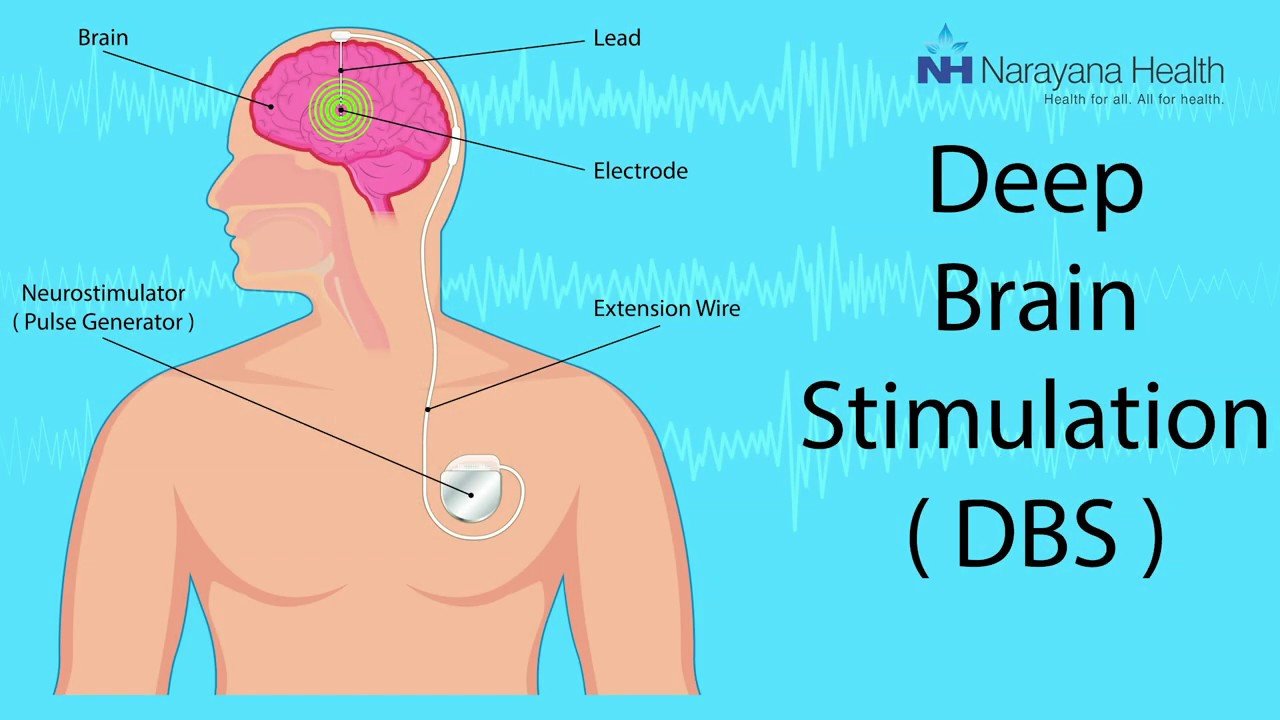
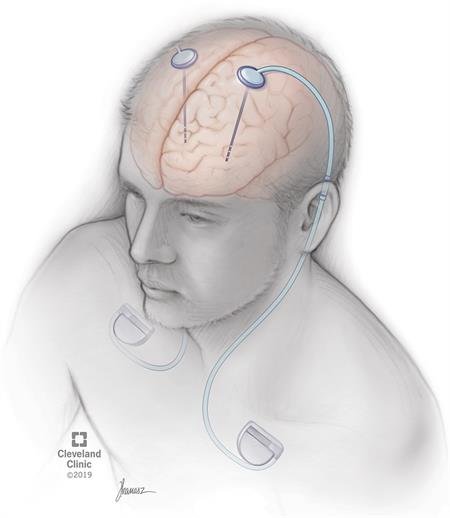
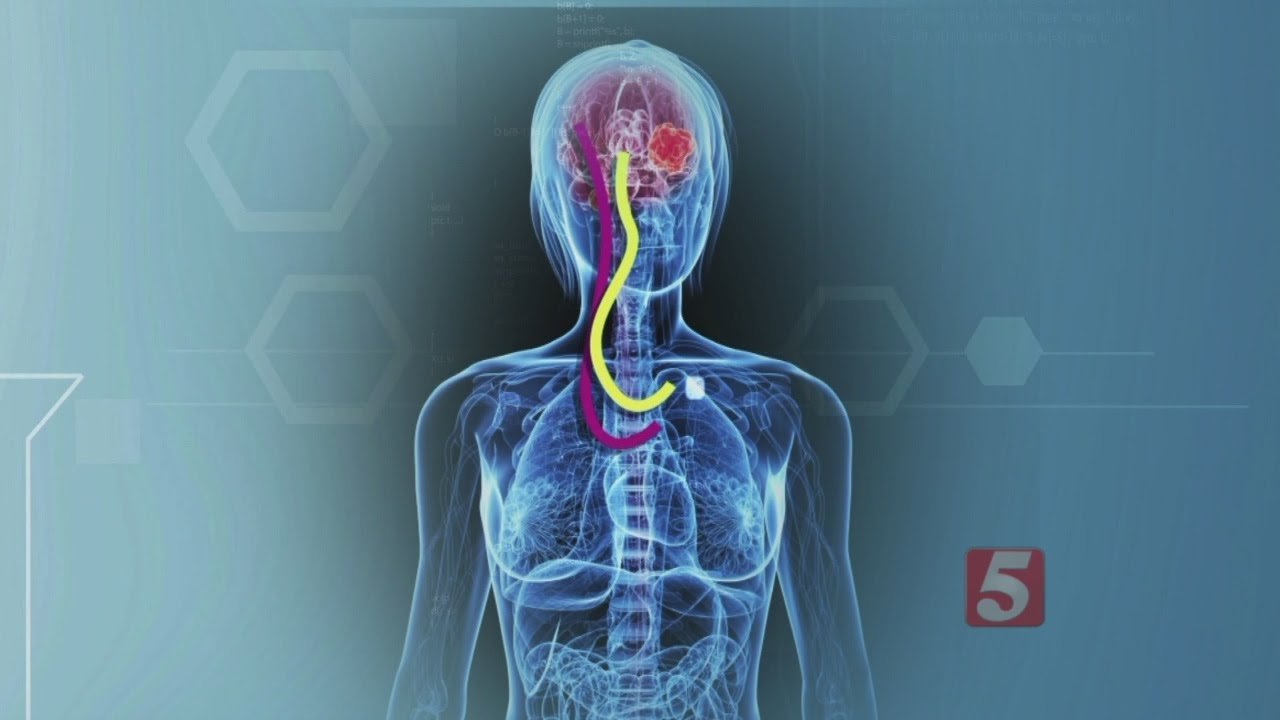
In DBS surgery, thin wires called electrodes are placed into one or both sides of the brain in specific areas that control movement. Usually a person remains awake during surgery so that he or she can answer questions and perform certain tasks to make sure that the electrodes are positioned correctly. However, some medical centers now are using brain imaging to guide the electrodes to the right spot while a person is asleep. Each method has its pros and cons and may not be suitable for everyone or available everywhere.
Once the electrodes are situated, they are connected to a battery-operated device that is typically placed under the skin below the collarbone. This device, called a neurostimulator, delivers continuous electrical pulses through the electrodes to decrease Parkinson’s symptoms.
How DBS Works
Research on DBS
Parkinson’s Patients Saw Continued Improvement In Motor Symptoms Quality Of Life
Deep brain stimulation remained effective in Parkinson’s disease patients more than 15 years after the device was implanted, and patients continued to demonstrate significant improvement in motor symptoms, a retrospective study showed.
Parkinson’s patients who had bilateral subthalamic nucleus deep brain stimulation for 15 years or longer spent 75% less time with dyskinesia and 58.7% less time in the off state than pre-surgery baseline , reported Elena Moro, MD, PhD, of Grenoble Alpes University in France, and co-authors.
These patients also reduced their dopaminergic drugs by 50.6% , they wrote in Neurology. The Parkinson’s Disease Quality of Life questionnaire total score, emotional function domain score, and social function domain score improved by 13.8% , 13.6% and 29.9% , respectively.
“Deep brain stimulation benefits seem to last for several years but not enough data have been available to show that these effects are still present more than 15 years after surgery,” Moro said in a statement.
“Our study found that, despite the natural progression of Parkinson’s disease and the worsening of some symptoms that become resistant to medications over the years, participants still maintained an overall improvement in quality of life,” she added.
In the long-term, 19 patients were completely independent in their activities of daily living, 27 patients needed some help, and five were institutionalized. A total of 18 of 51 patients had dementia.
Disclosures
Schedule An Appointment With Qualified Deep Brain Stimulator Surgeon In Nevada
As a leading brain, spine, and pain management service provider, Sierra Neurosurgery offers qualified and experienced spine specialists in Reno. Our expansive range of services includes minimally invasive spine surgery, neuro-oncology, brain tumor treatment, X-ray and MRI imaging services, pituitary tumor surgeries, and more.
How Has Deep Brain Stimulation Benefitted Patients With Parkinsons Disease Neurology,Healthy Tips & Resources
Dr. Sameer Sheth, neurosurgeon at Baylor St. Luke’s Medical Center, uses deep brain stimulation as an alternative to medication for treating disorders such as Parkinson’s disease and essential tremor. DBS involves placing a device called a neurostimulator that sends electrical impulses through implanted electrodes to specific targets in the brain.
Will I Have To Limit My Activity Following Deep Brain Stimulation Surgery
- You should not engage in light activities for 2 weeks after surgery. This includes housework and sexual activity.
- You should not engage in heavy activities for 4 to 6 weeks after surgery. This includes jogging, swimming, or any physical education classes. Anything strenuous should be avoided to allow your surgical wound to heal properly. If you have any questions about activities, call your doctor before performing them.
- You should not lift more than 5 lbs. for at least 2 weeks.
- You should not raise your arms above your shoulders or over bend or stretch your neck.
- Depending on the type of work you do, you may return to work within 4 to 6 weeks.
How Does Dbs Compare To Other Methods Of Treatment For Parkinsons Disease
As in Hardy’s case, every patient’s treatment begins with medication until it is determined that they can benefit from DBS. “Medications are always tried first. Unfortunately, we can only get so far with medications. Oftentimes, many patients try them, and they may work for a little while,” said Dr. Sheth.
“But at some point, oftentimes the medications stop working as much because the disorder tends to progress over the years. It could get worse, and the medicines may not be able to keep up. Many of the medicines themselves have their own side effects. So, you get to a point where perhaps the medicines are helping to a degree, but they’re causing their own side effects, and exactly when we get to that point is when we introduce the idea of a surgical therapy like DBS.”
How Does The Neurosurgeon Know Where To Place The Electrodes In My Brain
Positioning the electrodes in the brain is the most critical step. The electrodes have to be placed in an exact location in the brain to improve symptoms. Computed tomography or magnetic resonance imaging scans are taken before and/or during the procedure to pinpoint the exact areas to target and guide the lead and electrode placement. Many times an electrode may be used to record brain cell activity at the target site to improve lead placement.
Deep Brain Stimulation Can Preserve Working Status In Parkinsons Disease Norbert Kovács
1Department of Neurology, University of Pécs, Rét Utca 2, Pécs 7623, Hungary
2Department of Neurosurgery, University of Pécs, Rét Utca 2, Pécs 7623, Hungary
3MTA-PTE Clinical Neuroscience MR Research Group, Rét Utca 2, Pécs 7623, Hungary
4Department of Neurology, Kaposi Mór County Hospital, Tallián Gyula Utca 16, Kaposvár 7400, Hungary
Abstract
The present scientific contribution is also dedicated to the 650th anniversary of the foundation of the University of Pécs, Hungary
1. Introduction
The 27-year-old deep brain stimulation revolutionized the treatment of movement disorders including drug-resistant tremor, advanced Parkinson’s disease , and dystonia . Based on its high efficacy and relatively small side effect profile, more than 100,000 patients have undergone DBS implantation worldwide . Approximately 80% of indications for DBS are the pharmacologically not efficiently treatable PD and considerably less patients receive DBS for other movement disorders . The most frequently applied surgical target for PD is the bilateral subthalamic DBS capable of improving all cardinal symptoms. Besides the symptomatic improvement, STN DBS can also dramatically and permanently extend the ON time and the health-related quality of life .
2. Materials and Methods
2.1. Patients
2.2. Applied Tests
2.3. Statistics
3. Results
3.1. Study Population
| Active job group | No job group | Statistics |
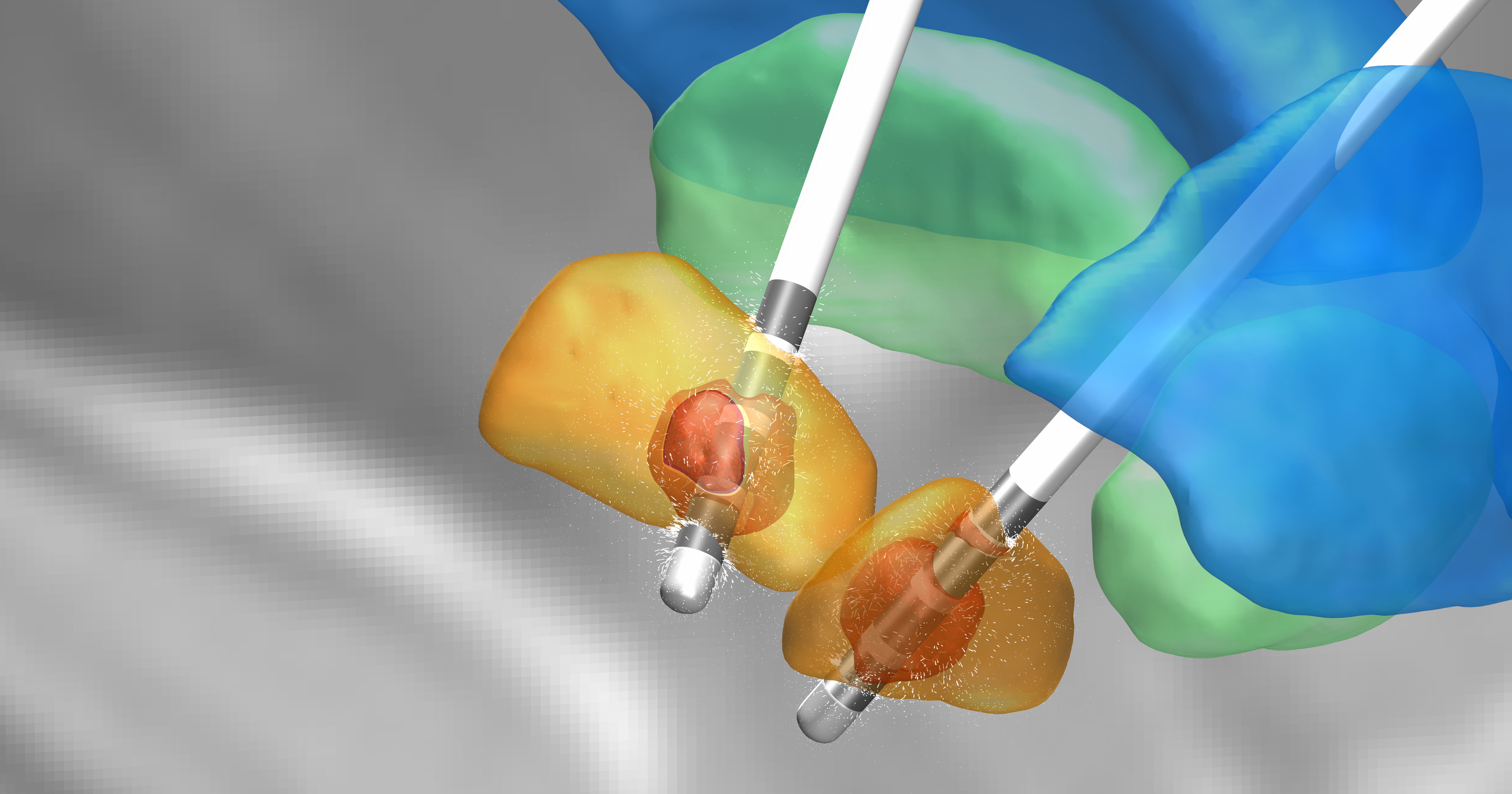
Postoperative Mri Based Evaluation Of Deep Brain Stimulating Electrodes
Correlations of preoperative and postoperative MRI can be used to delineate the deep brain stimulating electrodes with respect to the subthalamic nucleus, as depicted by T2 weighted spin echo imaging. This is best done with MRI of high resolution and devoid of artefacts, a situation achievable by the acquisition of the preoperative images under general anaesthesia. As demonstrated for a representative patient in fig 2, the subthalamic nucleus can be clearly delineated in preoperative axial spin echo images as well as in coronal and sagittal reconstructions derived therefrom. The planning tracks are indicated by red lines and blue lines . The implanted electrodes can be visualised relative to the subthalamic nucleus using different image fusion modes—that is, a detail of the postoperative image shows part of the electrode overlaying the preoperative image , or intermediate weighting of images reveals both the electrode and the subthalamic nucleus .
Figure 2
MRI may also be valuable for the analysis of electrodes implanted in patients who previously had ablative procedures within the basal ganglia. In one patient a thalamo-subthalamotomy had been placed within and towards the base of the Vop according to the Schaltenbrand and Wahren atlas, which had been correlated with the T1 weighted MRI . In this patient deep brain stimulation was done in the vicinity of, but in an area clearly distinct from, the site lesioned previously.
Figure 3
Will I Have To Limit Activity Following Deep Brain Stimulation Surgery
- You should not engage in light activities for two weeks after deep brain stimulation surgery. This includes housework and sexual activity.
- You should not engage in heavy activities for four to six weeks after surgery. This includes jogging, swimming, or any physical education classes. Anything strenuous should be avoided to allow your surgical wound to heal properly. If you have any questions about activities, call your doctor before performing them.
- You should not lift more than five pounds for at least two weeks.
- Depending on the type of work you do, you may return to work within four to six weeks.
Effects Of Deep Brain Stimulation On Parkinsons Disease Patients
Studies show that DBS has a positive impact on people suffering from PD. It helps in alleviating mobility issues and enhances the patient’s quality of life. Moreover, many patients are also able to reduce their medical interventions in the first few months after treatment.
One excellent and noteworthy benefit of DBS is that it increases the time period when PD patients are at their best state without any signs of troublesome dyskinesia, or impairment of voluntary movement.
How Is Deep Brain Stimulation Used To Treat Parkinsons Disease
Deep brain stimulation delivers electrical impulses to a targeted area of the brain that is responsible for the movement symptoms caused by Parkinson’s disease. The electrical impulses disrupt the abnormal activity that occurs in the brain’s circuitry, which is causing the symptoms.
There are three areas in the brain that can be targets for deep brain stimulation in patients with Parkinson’s disease. They are the subthalamic nucleus, the globus pallidus internus, and the ventral intermediate nucleus of the thalamus. Each of these areas plays a role in the brain’s circuitry that is responsible for the control of movement.
The specific area in the brain to target in an individual with Parkinson’s disease depends on symptoms that need to be treated. For example, deep brain stimulation of subthalamic nucleus is effective for all major movement symptoms of Parkinson’s disease, such as tremor, slowness of movement , stiffness , and problems with walking and balance. Deep brain stimulation of globus pallidus is another effective target for a wide range of Parkinson’s symptoms. The thalamic target is sometimes selected for patients with tremor symptoms. The recommended target for each patient is made collaboratively with the neurologist, neurosurgeon and other caregivers involved in the decision making process.
What Are The Risks And Complications Of Deep Brain Stimulation

As with any surgical procedure, there are risks and complications. Complications of DBS fall into three categories: surgery complications, hardware complications, and stimulation-related complications.
- Surgical complications include brain hemorrhage, brain infection, wrong location of the DBS leads, and less than the best location of the leads.
- Hardware complications include movement of the leads, lead failure, failure of any part of the DBS system, pain over the pulse generator device, battery failure, infection around the device and the device breaking through the skin as the thickness of skin and fat layer change as one ages.
- Stimulation-related complications occur in all patients during the device programming stage. Common side effects are unintended movements , freezing , worsening of balance and gait, speech disturbance, involuntary muscle contractions, numbness and tingling , and double vision . These side effects are reversible when the device is adjusted.
How Effective Is Deep Brain Stimulation For Parkinsons Disease
Deep brain stimulation provides excellent relief for most patients’ symptoms including tremor, stiffness , slowed movement , freezing of gait and dyskinesias. Long-term studies have shown continued improvement in tremor, bradykinesia, and dyskinesia. Many patients are able to reduce their medications and maintain their level of function including independent participation in activities of daily living required to care for oneself. One of the distinct advantages, is that after DBS, patients on average improve their daily ‘on time’—when they are at their best, without troublesome dyskinesia—by half a day.
How Long Does The Battery In The Impulse Generator Device Last
Batteries can last 3 to 5 years in non-rechargeable devices and up to 15 years or even longer in rechargeable battery devices. However, these times may vary significantly. A simple outpatient procedure is needed to replace the battery. Rechargeable battery devices can be charged daily or every 10 to 14 days . Your doctor will discuss how often you should recharge your battery based on your therapy settings.
If The Mechanism Of Dbs Is Not Known Why Should I Consider It
Because it works.
Because it is quite safe.
There are many things for which we don’t understand the exact reason. For example, we are still finding out more about the myriad benefits of exercise.
For example – How does exercise improve Mood? We don’t understand that too well. But it is easy to grasp that exercise is good for you.
This what-you-see-is-true evidence is called “Empiric Evidence”.
Correlation Of Active Electrode Contacts With Microrecordings

To account for individual variability within the basal ganglia and the subthalamic area, the position of single electrode contacts should preferentially be put in relation to the location of the structures of interest. For that purpose, we developed an algorithm for three dimensional plotting of the electrode contact within the same stereotactic coordinate system, showing the microrecording tracks explored intraoperatively . The intercommissural plane is indicated for orientation purposes, while the three dimensional plots can be rotated to be viewed from different angles of interest. The area where subthalamic nucleus activity was first recorded and which corresponds to its dorsal margin was defined by retrospective off-line analysis of intraoperative microrecordings . Despite continuous on-line analysis during the operation, recordings of longer duration used for off-line reassessments had been made at intervals of 0.5 mm. This results in some uncertainty over the exact location of the border. Taking the length of single electrode contacts into account as well , contacts located within ± 1.0 mm from the neurophysiologically mapped subthalamic nucleus margin were categorised as being located in the border area.
Figure 4
Active electrode contacts relative to the margin of the subthalamic nucleus
Will I Be Asleep During The Deep Brain Stimulation Procedure
You will remain awake during most of the deep brain stimulation procedure. This allows the surgical team to interact with you when testing the effects of the stimulation. Small amounts of local anesthetic are given in sensitive areas. The vast majority of people experience minimal discomfort during the procedure.
How Do I Know If Im A Candidate For Deep Brain Stimulation
Before being considered a candidate for deep brain stimulation , patients with Parkinson’s disease must undergo an extensive evaluation process. Ideally, a multidisciplinary team of specialists in the area of movement disorders will assess the patient. This clinical team typically includes a neurologist, neurosurgeon, neuropsychologist and psychiatrist.
If patients are well managed on medications, DBS is not considered. Candidates for DBS are patients who meet one or more of the following criteria:
- Symptoms are not well controlled despite receiving the appropriate dose of levodopa and other medications.
- Symptoms are significantly reducing patients’ quality of life.
- Abnormal or uncontrolled involuntary movements or motor fluctuations are not improving despite adjustments in medications.
- Four or more doses of levodopa are required a day.
- Tremors that have not been able to be controlled by medications.
Levodopa response test
Patient’s response to a single dose of levodopa is another test physicians use to identify which patients are likely to benefit from DBS. In this test, patients stop taking levodopa for 8 to 12 hours and then receive a single dose. Patients are likely to benefit from DBS if they have a clear positive response after receiving the single dose of levodopa.
Deep Brain Stimulation For Parkinson’s May Help Long Term HealthDay Reporter
THURSDAY, June 3, 2021 — Parkinson’s disease patients can get symptom relief with deep brain stimulation therapy that lasts over the long term, a new study shows.
Over 15 years, patients who received DBS, which requires surgical implantation, had significant improvement in motor symptoms and less need for medication, researchers found.
“Our study, for the first time, supports the efficacy of deep brain stimulation in the very long term — 15 years after surgery and 25 years since Parkinson’s diagnosis,” said senior researcher Dr. Elena Moro, director of the Movement Disorders Unit at Grenoble Alpes University in France.
“Indeed, after an average of 15 years after surgery, patients could experience improvement, compared to before surgery,” she said. “Moreover, we could still observe a marked reduction of anti-Parkinson’s medication and improvement of quality of life, compared with before the intervention.”
Patients with Parkinson’s disease no longer make dopamine, which affects their speech, walking and balance. Symptoms can be partially relieved by the drug levodopa, which temporarily restores dopamine.
But as levels of dopamine fluctuate during the day, patients can suffer from dyskinesia, a side effect of levodopa that can cause twisting, swaying or head bobbing.
For the study, Moro’s team collected data on 51 patients being treated with DBS. On average, they had the device for 17 years.
More information
Signs Indicating That Youre A Suitable Candidate For Dbs

Deep brain stimulation isn’t suitable for every patient who suffers from Parkinson’s disease. Here are the common signs and symptoms that may lead a physician to recommend DBS treatment.
- Parkinson’s disease symptoms lingering for five years or more
- You experienceintermittent memory loss issues
- Your symptoms worsen sometimes despite regular medical administration
- You’re suffering from dyskinesia
- Medications have adverse side effectson your health
- Parkinson’s disease symptoms are affecting your daily routine and activities.
How Should I Care For The Surgical Area Once I Am Home
- Your stitches or staples will be removed 10 to 14 days after surgery.
- Each of the four pin sites should be kept covered with band aids until they are dry. You will be able to wash your head with a damp cloth, avoiding the surgical area.
- You may only shampoo your hair the day after your stitches or staples are removed, but only very gently.
- You should not scratch or irritate the wound areas.
Is Deep Brain Stimulation Effective Against Parkinsons
Jul 12, 2021 | Guides
Although there’s no definitive treatment to cure Parkinson’s disease, doctors might recommend lifestyle modifications, supportive therapies, or medications based on your symptoms.
Stats show that more than 60,000 US citizens are diagnosed with Parkinson’s disease every year. Around 10 million people are currently living with initial or advanced stage PD worldwide. In addition, April is observed as “Parkinson’s Disease Awareness” month in which we strive to create awareness about this unforgiving medical condition.
Among many kinds of preventive or restorative treatments available for Parkinson’s, Deep Brain Stimulation is considered one of the most effective ones.
This technique was first approved in 1997 to treat Parkinson’s tremors and advancing symptoms. With technological advancements, in 2016, DBS was approved for treating early Parkinson’s stages. Our spinal and neurosurgeons prescribe and perform DBS on patients with five years or more history of motor and memory symptoms associated with Parkinson’s.
Let’s get to know more about deep brain stimulation and its impact on Parkinson’s disease patients.
What Is Deep Brain Stimulation For Parkinsons Disease
DBS is electrical stimulation of the brain by using a small machine. DBS can stimulate many brain areas.
DBS is actually approved for many diseases. It is not just a “Parkinson’s surgery”. It can be used for epilepsy and other movement disorders as well.
The basic setup is the same.
The DBS battery is inserted below the chest skin. Two small wires from the battery go up to the head. The wires go through the skull. They are inserted into the desired area of the brain.
For Parkinson’s disease: This target area of the brain is usually the “Subthalamic Nucleus .
In some patients, another area is chosen as the target. This other area is the Globus Pallidus interna .
How is the target chosen? Read this article
DBS can dramatically improve Parkinson’s symptoms. There are many before-after videos available on the internet.
For example, here is a video posted on youtube by the Neuromedical Center in USA.
Deep Brain Stimulation: How Awake Brain Surgery Works
August 21, 2019
Parkinson’s disease makes it hard to do many things that people without the condition take for granted. A disorder of the nervous system, Parkinson’s affects movement and often includes tremors—uncontrollable shaking of the hands or other body parts that can turn patients’ lives upside down, robbing them of the motion control they need to do their jobs, or simple tasks like brushing their teeth. Many patients can manage their tremors with medication, but for some, the treatment becomes less effective over time.
There is hope. Deep Brain Stimulation is a surgery that can—almost instantaneously in the operating room—stop the tremors. “It’s the use of stimulation within nuclei deep inside the brain to try to correct dysfunction within neurological circuits,” explains Jason Gerrard, MD, chief of functional neurosurgery at Yale.
The procedure involves implanting one or more electrodes into specific areas in the brain associated with the movement disorder. The electrodes, controlled by an external stimulator, send electrical impulses that regulate abnormal or overactive impulses.
“Early on, it was identified in Parkinson’s disease that neurons within the substantia nigra were being lost,” says Dr. Gerrard. “And these neurons were known to contain the neurotransmitter dopamine.”
What Kind Of Results Can You Expect After Having Dbs
A few weeks after the surgery, a specialist will program the DBS settings to your symptoms.
DBS won’t eliminate symptoms, but more than 70 percent of people with Parkinson’s experience a significant improvement.
You’ll likely be able to cut back on medication. DBS settings can be adjusted without surgery. It may take a few months to find the best combination of medications and DBS settings.
Surgery To Implant The Deep Brain Stimulation Device
Deep brain stimulation requires the surgical implantation of an electrical device into the brain. A neurosurgeon uses imaging scans to pinpoint the right spot in the brain for implanting the electrode.
When surgeons have determined the correct location, they create a small opening in the skull and insert a thin, insulated wire, through which they insert the electrode. Surgery to implant the electrode takes about four hours and requires general anesthesia. You may then stay overnight in the hospital for observation.
The next day, doctors perform the second part of the surgery, which involves connecting the insulated wire to a battery-operated pulse generator that is implanted under the skin near the collarbone. Most people can return home after this procedure.
Several days after the surgery, you meet with your neurologist, who programs the pulse generator. Pushing a button on an external remote control sends electrical impulses from the pulse generator to the electrode in the brain.
People who use deep brain stimulation work closely with their neurologist to find the combination of settings that best controls their symptoms. After several visits, they are able to control the strength of the electrical impulses on their own. Following this adjustment period, most people require only occasional maintenance visits.
What Is Deep Brain Stimulation And How Does It Work
“DBS is a therapy that we have for various neurological conditions,” said Dr. Sheth. “It’s a system that you can think of like a pacemaker. But rather than being a pacemaker for the heart, it’s for the brain.”
Dr. Sheth describes the brain as having many circuits that govern everything we do, including how we move.
“If the movement circuit is not working properly, we may have a movement disorder like Parkinson’s,” he said. “If we can identify the circuit within the brain that is not working properly, we can use this device to reset the rhythms in the brain and restore the balance so that our movements can be better controlled or without a tremor.”
Pallidal Stimulation Versus Subthalamic Stimulation
As mentioned, there are two main anatomic targets for using DBS to treat PD – the STN and the GPi. There have been several large randomized studies comparing STN and GPi DBS in PD. It is suggested that both STN DBS and GPi DBS overall equally and successfully improve motor symptom, and are similar in cost-effectiveness. However, although no differences were observed in the on phase between STN DBS and GPi DBS, significant differences were seen in the off phase; STN DBS was more effective in terms of motor function improvement in the off phase. There are different opinions in terms of effects of STN DBS and GPi DBS on quality of life. Some authors have found no significant difference between the STN and GPi targets. However, others agree with that greater improvements in quality-of-life measures are achieved in patients with GPi DBS.
GPi DBS can be used for patients with more axial symptoms, gait issues, dyskinesias, depression, and word fluency problems. STN DBS is often favored in reducing medication post surgery, and for patients with greater tremor. STN-DBS has also demonstrated an improvement in the quality of sleep for patients.
Findings On Medication Use And Motor Complications
The results showed that deep brain stimulation was effective at reducing motor complications from Parkinson’s disease for more than 15 years.
The researchers also found that the therapy reduced the amount of time a person experienced dyskinesia by a whopping 75%. Dyskinesia is a side effect of a common Parkinson’s medication called levodopa that results in rapid, involuntary body movements, like twisting, squirming, and head bobbing.
What’s more, participants spent about 59% less time in an “off state,” when medication stopped being as effective, and reduced their use of medications to manage dopamine levels by 51%.
Strength And Limitations Of Deep Brain Stimulation
Even though participants still experienced progression of Parkinson’s disease over the course of the study, their quality of life continued to climb by an average of 14% from the time of their surgery to their follow-up around 15 years later. That finding illustrates both the strengths and the limitations of deep brain stimulation for Parkinson’s disease, experts say.
Three Components Of Deep Brain Stimulation Therapy
During deep brain stimulation therapy, your doctor performs three main steps:
- A small incision is created in the skin throughwhich an electrode is inserted. This electrode is a thin, insulated wire that targets the affected brain area.
- The electrode is connected to a neurotransmitter.
- The battery packis connected with a neurotransmitter, planted under the skin, usually near the collarbone, lower abdomen, or chest.
What Are The Advantages Of Deep Brain Stimulation
Deep brain stimulation has many advantages:
- DBS does not cause permanent damage in any part of the brain, unlike thalamotomy and pallidotomy, which surgically destroy tiny areas of the brain and therefore is permanent and not reversible.
- The electrical stimulation is adjustable and reversible as the person’s disease changes or his or her response to medications change.
- Because DBS is reversible and causes no permanent brain damage, use of innovative not-yet-available treatment options may be possible. Thalamotomy and pallidotomy result in small, but permanent changes in brain tissue. A person’s potential to benefit from future therapies may be reduced if undergoing these procedures.
- The stimulator can also be turned off at any time if DBS is causing excessive side effects without any long-term consequences.
What Should I Expect After Deep Brain Stimulation
You may feel tired and sore but will be given medication and kept comfortable after your deep brain stimulation procedure. Also, you may have irritation or soreness around the stitches and pin sites.
As with any surgery, there are some guidelines and limitations that you should follow after DBS. Be sure to discuss these with your doctor and ask questions before surgery. Understanding what you will be experiencing and knowing what to expect afterward can help ease some of the natural anxiety that comes with any medical procedure.
What Is Deep Brain Stimulation How Does Dbs Work Dr. Siddharth Kharkar
DBS is the short form of “Deep Brain Stimulation”. DBS is one type of Parkinson’s Surgery.
DBS works by passing a small current into the brain. This current is passed into only to a small part of the brain.
The doctor selects one out of two brain parts .
DBS works by changing the electrical currents in these areas. At present, we cannot mathematically calculate these changes.
But, empirically – DBS improves Parkinson’s symptoms.
Let us learn more about these topics:
How Does The Deep Brain Stimulation Implant Work
The deep brain stimulation device has an electrode, which is shaped like a tip. It is implanted in the region of the brain involved with the disease symptoms.
Electrical pulses are transmitted through four metal pads on the surface of the electrode. Because they are tiny, the electrical pulses stimulate only brain tissue near the electrode. Thus, the electrical stimulation can specifically target only the brain region near where the electrode is planted.
The simulator, which is also called the pulse generator is a small device that is shaped like a box and generates the electrical signals sent to the electrode.
Usually implanted in a space under the skin, near the patient’s chest, the pulse generator includes a battery with a lifespan that can range from two to seven years.
Quick on-off electrical pulses are delivered at very high frequencies, typically exceeding 100 times per second.
The high frequencies are necessary to help reduce unwanted symptoms.
The extension, the final component of an implanted DBS device, is an insulated cable. It takes the electrical signals from the pulse generator and delivers them to the electrode implanted in the brain.
Because having any part of the DBS device going through the skin could pose a risk for infection, the surgeon generally tunnels a small path under the skin, going from the pulse generator to the electrode.