Dementia Is Notoriously Difficult To Accurately Diagnose Parkinsons Disease Dementia And Lewy Body Dementia Can Be Especially Hard To Tell Apart Even For Experts
Gordon Gastil was a field geologist, an amateur botanist, and scientist his whole life, constantly in awe of the world around him. “He was climbing mountains, running around being crazy, cracking terrible dad jokes,” His son John told Being Patientin a LiveTalk. “When Parkinson’s came to him, that freedom of movement was the first thing that you started to see go.”
In the United States, roughly60,000 people are diagnosed with Parkinson’s disease every year. The second most common form of neurodegeneration after Alzheimer’s, Parkinson’s not only leads to a decline in motor functions; it may also bring cognitive impairment and behavioral symptoms.
Some people with Parkinson’s disease would eventually develop dementia, a syndrome that describes the loss of memory, thinking and behavioral functions that interferes with people’s daily lives. When dementia occurs after people develop Parkinson’s, clinicians call this condition Parkinson’s disease dementia, though not all people with the disease would experience dementia.
Because symptoms of the disorders often overlap and that various health conditions can mimic their symptoms, getting an accurate diagnosis can be difficult. Accordingly, clinicians say that seeking a specialist is critical to receiving the appropriate diagnosis and care.
Robin Williams Would Have Been 70 This Year Here’s What We Know About Lewy Body Dementia Suicide And Parkinson’s
On July 21, actor and comedic genius Robin Williams would have turned 70. Williams not only amplified and brought awareness to the life-changing, prevalent disease known as Lewy Body Dementia, but his passing brought much needed attention to the importance of mental health and the non-movement symptoms of depression and anxiety that can accompany a neurodegenerative disease.
Nearly seven years after his passing, what do we know about Lewy Body Dementia? How can we help people with a neurological disease experiencing suicidal thoughts?
Whats The Difference Between Lewy Body Dementia Parkinsons Disease And Alzheimers Disease
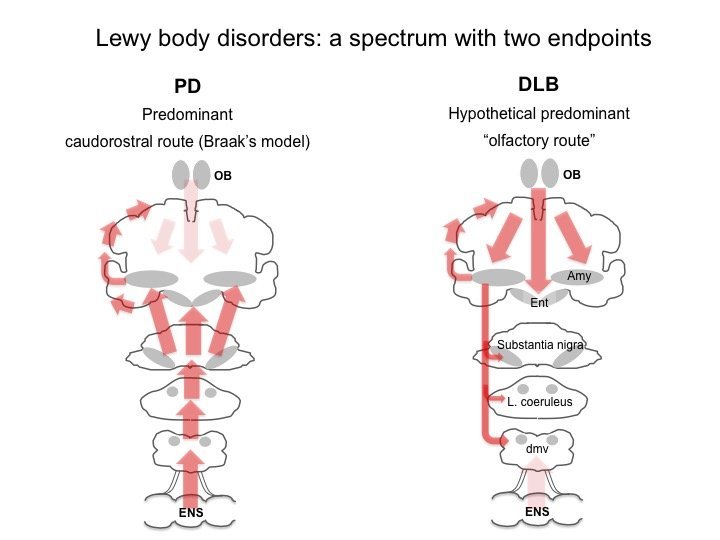
Lewy body dementia is an umbrella term for two related clinical diagnoses: “dementia with Lewy bodies” and “Parkinson’s disease dementia.” These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending on where the Lewy bodies first form.
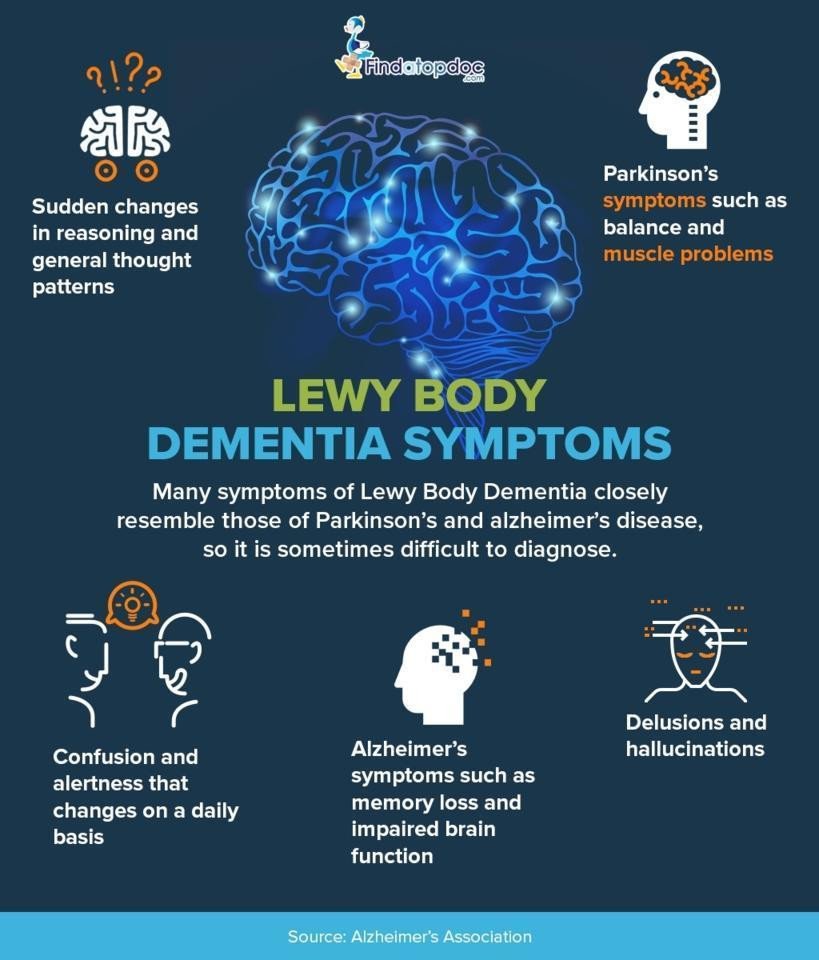
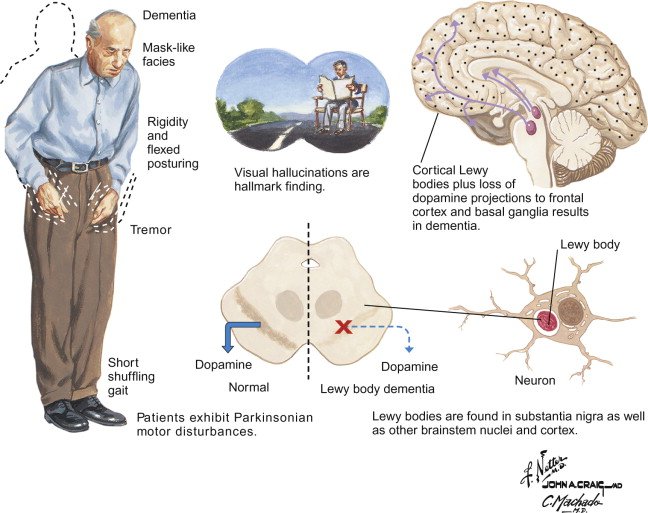
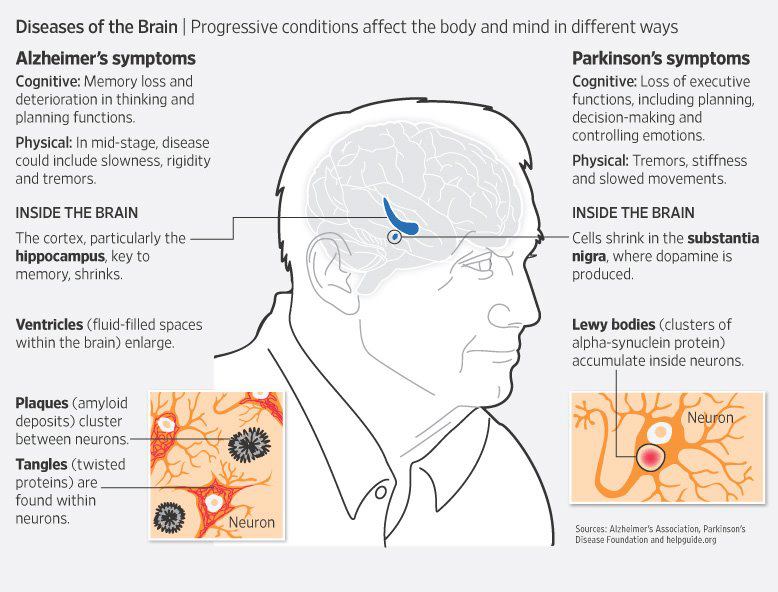
Dementia with Lewy bodies is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a person’s ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first in DLB. The motor symptoms of Parkinson’s such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
Finally, Alzheimer’s is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
Genetic Study Of Lewy Body Dementia Supports Ties To Alzheimers And Parkinsons Diseases
NIH-led study locates five genes that may play a critical role in Lewy body dementia.
In a study led by National Institutes of Health researchers, scientists found that five genes may play a critical role in determining whether a person will suffer from Lewy body dementia, a devastating disorder that riddles the brain with clumps of abnormal protein deposits called Lewy bodies. Lewy bodies are also a hallmark of Parkinson’s disease. The results, published in Nature Genetics, not only supported the disease’s ties to Parkinson’s disease but also suggested that people who have Lewy body dementia may share similar genetic profiles to those who have Alzheimer’s disease.
“Lewy body dementia is a devastating brain disorder for which we have no effective treatments. Patients often appear to suffer the worst of both Alzheimer’s and Parkinson’s diseases. Our results support the idea that this may be because Lewy body dementia is caused by a spectrum of problems that can be seen in both disorders,” said Sonja Scholz, M.D., Ph.D., investigator at the NIH’s National Institute of Neurological Disorders and Stroke and the senior author of the study. “We hope that these results will act as a blueprint for understanding the disease and developing new treatments.”
The study was led by Dr. Scholz’s team and researchers in the lab of Bryan J. Traynor, M.D., Ph.D., senior investigator at the NIH’s National Institute on Aging .
Article:
NIH…Turning Discovery Into Health®
How Exactly Is Lewy Body Dementia Related To Alzheimers Disease And Parkinsons Disease
Lewy body dementia is a broad, general term for dementia in which lewy bodies are present in the brain. Dementia with lewy bodies and Parkinson’s disease dementia are two related clinical disorders that make up the general broader category of Lewy body dementia. Sometimes LBD is first diagnosed as Parkinson’s disease or Alzheimer’s disease based on its symptoms.
- Parkinson’s disease dementia : You might be diagnosed with Parkinson’s disease if you start out with a movement disorder typical to Parkinson’s but then have your diagnosis changed to PDD when dementia symptoms develop.
- Alzheimer’s disease : You might start out with memory or cognitive disorder that leads to a diagnosis of AD. Over time, other distinctive symptoms begin to appear and your diagnosis is then changed to dementia with lewy bodies. Distinctive symptoms of LBD include the changes in attention, alertness and cognitive ability; changes in walking and movement; visual hallucinations; REM sleep behavior disorder and severe sensitivity to some antipsychotics used to treat hallucinations.
What Complications Are Associated With Medications Used To Treat Lewy Body Dementia
Up to 50% of people living with Lewy body dementia can have severe side effects when treated with certain antipsychotic medications. These are known as the typical or traditional antipsychotics and include such drugs as thoridazine, haloperidol, chlorpromazine and perphenazine. This class of older, first-generation antipsychotics can cause sedation and make cognitive symptoms and movement problems worse. A life-threatening reaction to an antipsychotic medication, called neuroleptic malignant syndrome, is possible. Symptoms include rigid muscles, changing blood pressure, high fever, confusion and fast heart rate. Contact your healthcare provider immediately if you or your loved are taking an antipsychotic and develop these symptoms.
Visual hallucinations and behavioral changes may be treated with the newer, atypical antipsychotic medications pimavanserin , quetiapine or clozapine . However, because all antipsychotic medications – both older, typical medications and newer atypical medications – can increase the risk of death in elderly patients with dementia, you and your healthcare provider should carefully discuss the risks and benefits and using these medications.
Other medications, like antidepressants or sedative antihistamines, may increase confusion in people with LBD.
What Is The Difference Between Lewy Body Dementia And Parkinsons Disease Dementia
Lewy Body Dementia is a term used for both Parkinson’s disease dementia and Lewy Body Dementia. They have some things in common, but their progression and treatment are different.
While many people with Parkinson’s can experience cognitive changes, it is important to know that not everyone with Parkinson’s will develop dementia. “When we see more severe cognitive changes, particularly when they affect someone’s function or ability to act independently for activities of daily living, their work or hobbies, we think of that as being a form of dementia,” said Dr. Goldman.
“With Parkinson’s dementia, the motor symptoms precede the dementia. In dementia with Lewy Body the initial core symptom is dementia — cognitive changes are early, and motor features, if present, occur either after the onset of dementia or concurrently,” said Dr. Goldman.
How Can A Person Diagnosed With Lewy Body Dementia Live The Best Life Possible
First, it’s important to interact with others as much as possible. Plus exercise and eat a healthy diet to keep mind and body as strong as possible.
Use music and aromatherapy to reduce anxiety and improve mood.
Other things you can do involve seeking the help and assistance of others. Therapists can improve the quality of life of someone living with Lewy body dementia. Therapists include:
- Physical therapists: These therapists can help improve physical strength, flexibility, balance and walking mechanics.
- Occupational therapists: These therapists can teach skills and methods to maintain your ability to perform activities of everyday life and remain independent.
- Speech therapists: These therapists can improve swallowing difficulties and ability to speak more clearly.
Persons with Lewy body dementia and their families can also benefit from counseling with a psychotherapist. This counselor teaches how to manage emotional and behavioral problems. Finally, joining a support group – there are support groups for persons with LBD and for the caregivers of persons with LBD. Support groups help solve day-to-day problems and frustrations through sharing similar experiences. See the resource section of this article for links to support groups.
What Can I Expect If I Or My Loved One Have A Diagnosis Of Lewy Body Dementia
Each person’s experience with Lewy body dementia is unique to them. How slowly or quickly the disease progresses is impossible to know, but may be influenced by your general health and any existing diseases you may have. Because LBD is a progressive disease, difficulties with mind and body functions get worse over time. Currently, there is no known way to stop the progression of the disease. After diagnosis, most people with LBD live between five and seven years. Some people with LBD live up to 20 years after their diagnosis.
However, there’s always hope. Research on LBD, dementia with lewy bodies, Alzheimer’s disease, Parkinson’s disease with dementia are ongoing. New medications are being developed and new approaches to treatment are being investigated.
Difference Between Parkinsons Disease Dementia And Dementia With Lewy Bodies
Technically, the difference between these two conditions lies in how quickly the cognitive difficulties and hallucinations develop in relation to the movement issues. In DLB, the cognitive difficulties and hallucinations develop much sooner in the disease course than in PDD, sometimes even prior to the movement difficulties. Because of the similarities between PD, PDD, and DLB, current thinking in the medical community is that they should be viewed as related diseases which fall along a continuum of Lewy body disorders.
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
How Is Dementia With Lewy Bodies Different Than Parkinson’s Disease
It is worthy of note that dementia is often present with Parkinson’s disease, but not everyone who has this brain disorder will have this symptom. When it is present, people will first experience a movement disorder, with symptoms such as slowed movement, muscle stiffness, tremor and a shuffling walk. Subsequently, they will experience the cognitive symptoms of dementia, which include changes in mood and behavior. Another important aspect to keep in mind is that dementia with Lewy bodies is the umbrella term for two similar diagnoses, namely dementia with Lewy bodies and Parkinson’s disease dementia.
The difference between the two conditions is that the former is a type of dementia that results in difficulties with memory and thinking that are serious enough to disrupt everyday activities, whereas the latter is used to describe dementia that occurs with Parkinson’s disease several years after the patient received their diagnosis. Therefore, dementia with Lewy bodies occurs suddenly, while dementia that may occur in people with Parkinson’s disease arises later in the condition. Consequently, it is essential for medical professionals to make the difference between dementia with Lewy bodies and dementia that is present in people with Parkinson’s disease in order to assign a correct diagnosis.
File A Paraquat Claim With The Help Of Our Resourceful Legal Team
Our law firm specializes in toxic exposure and has the necessary knowledge and resources to help your family member who struggles with Parkinson’s disease as a result of paraquat exposure recover the financial compensation they are eligible for. With over 25 years of experience in pursuing compensation for the victims of toxic exposure, we will thoroughly assess your situation and gather pertinent evidence to support your paraquat claim. Although the legal process is quite complex, it will require minimal involvement on your part, as you will only have to provide our legal experts with proof of paraquat exposure and evidence of the diagnosis of Parkinson’s disease. The involvement of a family member is crucial, as people with Parkinson’s disease often have a difficult time clearly explaining their situation.
Parkinsons Disease With Dementia Versus Dementia With Lewy Bodies
Some patients with Parkinson’s disease experience no or only subtle cognitive decline, and their primary limitation is their motor disorder. However, other patients with Parkinson’s disease develop dementia as a consequence of the disease. When dementia develops after an established motor disorder, we call the disease Parkinson’s disease with dementia . In contrast, when dementia develops prior to or at the same time as the motor disorder, we call the disease DLB. Although the initial sequence of symptoms differs in PDD and DLB, as the disorders progress, the symptoms and the underlying brain changes are much more similar than they are different. As such, many researchers and clinicians think of PDD and DLB as being on a continuum of a similar disease process rather than as two distinct entities.
The Difference Between Parkinson’s Disease And Lewy Body Dementia
One of the most confusing concepts to explain in the clinic is the difference between Parkinson’s Disease, Parkinson’s Disease Dementia and Lewy Body Dementia. Ultimately people with Parkinson’s can look very similar with motor and non-motor problems. This is particularly tricky when PwP first present but the easiest way to consider Lewy Body Dementia is like having a very aggressive progression of Parkinson’s where patients are dementing in the first year of their condition whereas this process is much slower when patients develop Parkinson’s Disease Dementia. Indeed, clinically Lewy Body Dementia patients look like they have a cross between Parkinson’s and Alzheimer’s, which is actually close to what is seen down the microscope when researchers study the brain. Understanding the differences between Parkinson’s Disease and Lewy Body Dementia is not only difficult for patients and their families but has led some professional groups to try and lump all of these patients together under one umbrella, which probably does little to help individual families appreciate what the future holds.
Hopefully this video will help you to gain a more complete understanding of the differences between Parkinson’s Disease, Parkinson’s Disease Dementia and Lewy Body Dementia.
_____________________________________________________________________________________
Treatment Of Behavior And Mood Problems In Lewy Body Dementia
Behavioral and mood problems in people with LBD can arise from hallucinations, delusions, pain, illness, stress, or anxiety. They may also be the result of frustration, fear, or feeling overwhelmed. The person may resist care or lash out verbally or physically.
Medications are appropriate if the behavior interferes with the person’s care or the safety of the person or others. If medication is used, then the lowest possible dose for the shortest period of time is recommended.
The first step is to visit a doctor to see if a medical condition unrelated to LBD is causing the problem. Injuries, fever, urinary tract or pulmonary infections, pressure ulcers , and constipation can worsen behavioral problems and increase confusion.
Certain medications, such as anticholinergics and antihistamines may also cause behavioral problems. For example, some medications for sleep problems, pain, bladder control, and LBD-related movement symptoms can cause confusion, agitation, hallucinations, and delusions. Similarly, some anti-anxiety medicines can actually increase anxiety in people with LBD. Review your medications with your doctor to determine if any changes are needed.
Antidepressants can be used to treat depression and anxiety, which are common in LBD. Many of them are often well tolerated by people with LBD.
Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
There’s no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
What Is Lewy Body Dementia Causes Symptoms And Treatments
On this page:
Lewy body dementia is a disease associated with abnormal deposits of a protein called alpha-synuclein in the brain. These deposits, called Lewy bodies, affect chemicals in the brain whose changes, in turn, can lead to problems with thinking, movement, behavior, and mood. Lewy body dementia is one of the most common causes of dementia.
LBD affects more than 1 million individuals in the United States. People typically show symptoms at age 50 or older, although sometimes younger people have LBD. LBD appears to affect slightly more men than women.
Diagnosing LBD can be challenging. Early LBD symptoms are often confused with similar symptoms found in other brain diseases or in psychiatric disorders. Lewy body dementia can occur alone or along with other brain disorders.
It is a progressive disease, meaning symptoms start slowly and worsen over time. The disease lasts an average of five to eight years from the time of diagnosis to death, but can range from two to 20 years for some people. How quickly symptoms develop and change varies greatly from person to person, depending on overall health, age, and severity of symptoms.
In the early stages of LBD, symptoms can be mild, and people can function fairly normally. As the disease advances, people with LBD require more help due to a decline in thinking and movement abilities. In the later stages of the disease, they often depend entirely on others for assistance and care.
Caregiver Corner: Lewy What Explaining Lewy Body Dementia
Dementia with Lewy bodies is a common progressive brain disease that affects thinking, movement, behavior and sleep. Approximately 1.3 million Americans have Lewy body dementia, but may not be correctly diagnosed because many doctors are unfamiliar with it. Most people see multiple doctors before receiving the final diagnosis of Lewy body dementia. Their first response is often, “Lewy what?”
Symptoms and Diagnosis
Lewy body dementia is a general term and includes both Parkinson’s disease dementia and dementia with Lewy bodies . LBD symptoms include dementia, visual hallucinations and frequent variations in cognitive ability, attention or alertness. There are also changes in walking or movement, as well as a sleep disorder called REM sleep behavior disorder, in which people physically act out their dreams. LBD patients may also have a severe sensitivity to medications prescribed for hallucinations.
Treatment
Many LBD symptoms are highly treatable and aggressive symptom detection and treatment can improve quality of life for both the person with LBD and their caregiver. Some Alzheimer’s and Parkinson’s medications can help cognition, behavior and movement symptoms. Family caregivers are an important link in the partnership with healthcare professionals and also require significant support throughout the illness. For more information and to find support visit www.lbda.org.
Elizabeth Patrick is the Marketing and Communications Manager for the Lewy Body Dementia Association.
Lewy Body Dementia: A Common Yet Underdiagnosed Dementia
While it’s not a household word yet, Lewy body dementia is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known disorders like Alzheimer’s disease and Parkinson’s, it is often underdiagnosed or misdiagnosed. In fact, many doctors or other medical professionals still are not familiar with LBD.
Dementia With Lewy Bodies And Parkinson Disease Dementia
, MD, PhD, Department of Neurology, University of Mississippi Medical Center
Dementia with Lewy bodiesParkinson disease dementia
Dementia is chronic, global, usually irreversible deterioration of cognition.
Dementia with Lewy bodies is the 3rd most common dementia. Age of onset is typically > 60.
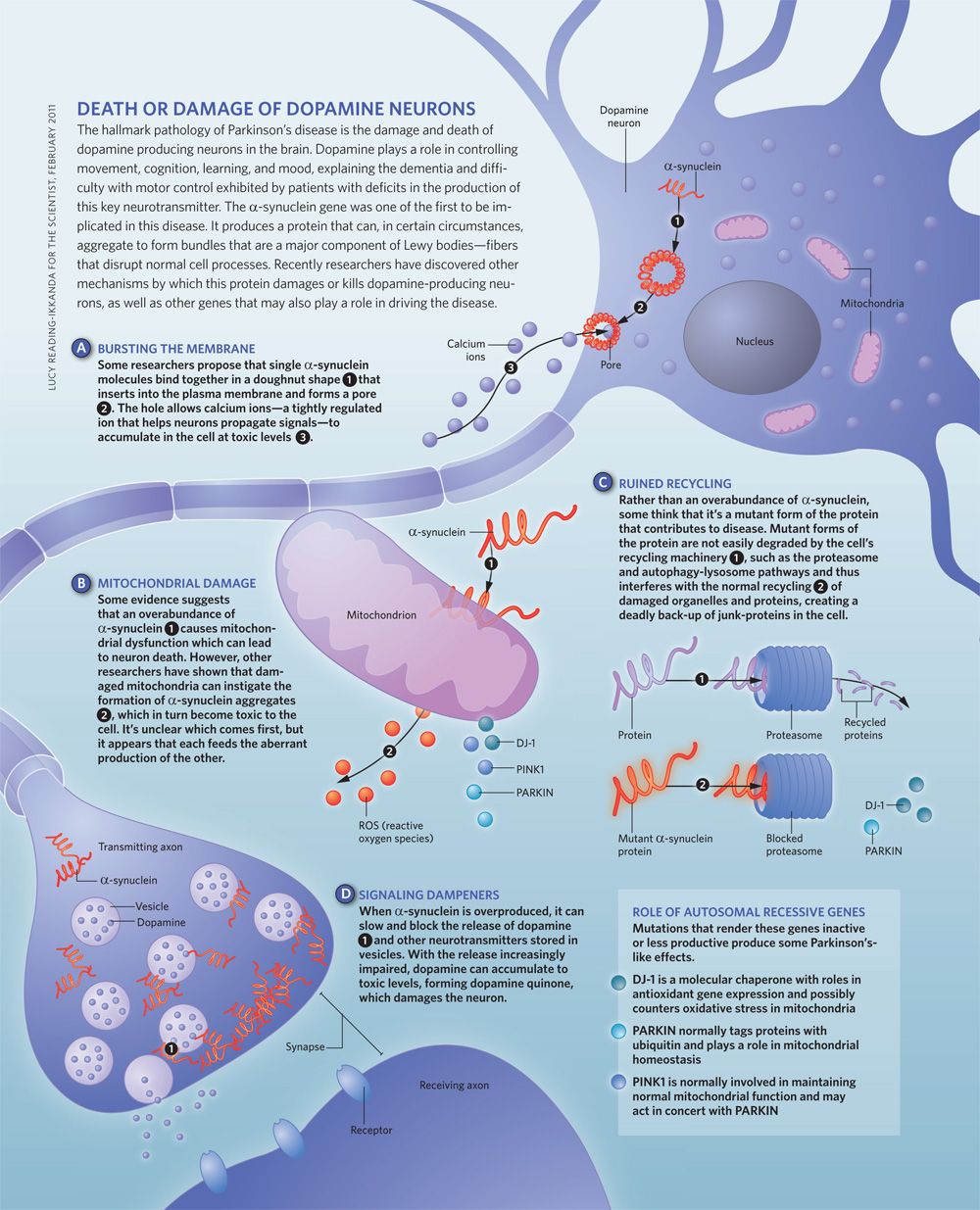
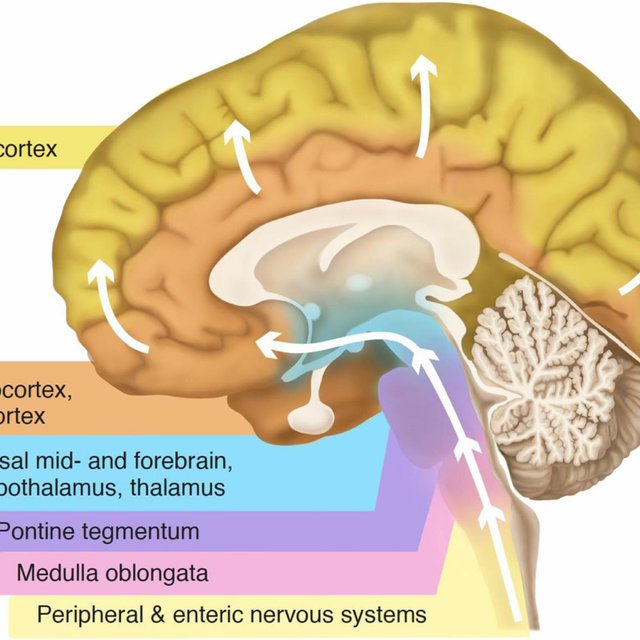
Lewy bodies are spherical, eosinophilic, neuronal cytoplasmic inclusions composed of aggregates of alpha-synuclein, a synaptic protein. They occur in the cortex of some patients who have dementia with Lewy bodies. Neurotransmitter levels and neuronal pathways between the striatum and the neocortex are abnormal.
Lewy bodies also occur in the substantia nigra of patients with Parkinson disease, and dementia may develop late in the disease. About 40% of patients with Parkinson disease develop Parkinson disease dementia, usually after age 70 and about 10 to 15 years after Parkinson disease has been diagnosed.
Because Lewy bodies occur in dementia with Lewy bodies and in Parkinson disease dementia, some experts think that the two disorders may be part of a more generalized synucleinopathy affecting the central and peripheral nervous systems. Lewy bodies sometimes occur in patients with Alzheimer disease, and patients with dementia with Lewy bodies may have neuritic plaques and neurofibrillary tangles. Dementia with Lewy bodies, Parkinson disease, and Alzheimer disease overlap considerably. Further research is needed to clarify the relationships among them.
Dlb Parkinsons Disease And Parkinsons Disease Dementia
DLB is closely related to Parkinson’s disease. Lewy bodies also cause the damage that leads to movement problems in Parkinson’s. People with Parkinson’s are more likely to go on to develop dementia, which is known as Parkinson’s disease dementia .
DLB and PDD can affect people in very similar ways. If dementia symptoms appear before or at the same time as people start to have movement problems, a diagnosis of DLB is likely to be given. If movement problems are present for a year or more before signs of dementia appear, a diagnosis of PDD is likely to be given.
Behavioral And Mood Symptoms Of Lewy Body Dementia
Changes in behavior and mood are possible in LBD and may worsen as the person’s thinking abilities decline. These changes may include:
- Depression
- Apathy, or a lack of interest in normal daily activities or events and less social interaction
- Anxiety and related behaviors, such as asking the same questions over and over or being angry or fearful when a loved one is not present
- Agitation, or restlessness, and related behaviors, such as pacing, hand wringing, an inability to get settled, constant repeating of words or phrases, or irritability
- Delusions, or strongly held false beliefs or opinions not based on evidence. For example, a person may think his or her spouse is having an affair or that relatives long dead are still living.
- Paranoia, or an extreme, irrational distrust of others, such as suspicion that people are taking or hiding things
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinson’s disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinson’s disease.
The overlap in symptoms between Lewy body dementia and Parkinson’s disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinson’s disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinson’s disease itself isn’t fatal, but complications can be.
Research has shown a median survival rate of about
How Is Lewy Body Dementia Treated Is There A Cure
There is no cure for Lewy body dementia . Medications and nonmedical therapies, like physical, occupational and speech therapies, manage symptoms as much as possible.
Medications called cholinesterase inhibitors help manage the cognitive symptoms of LBD. Memantine may also be helpful. Symptoms of Parkinsonism, like tremors, are usually treated with levodopa, a drug commonly used to treat Parkinson’s disease.
You or your loved one may also benefit from treatments like physical therapy or speech therapy. These treatments help retain physical function and improve muscle strength.
Managing The Effects Of Dementia With Lewy Bodies
A person with dementia with Lewy bodies might:
- have recurring visual hallucinations – see things that are not there
- experience disturbed sleep– known as Rapid Eye Movement sleep disorder, in which people are restless and can experience intense dreams/nightmares
- experience sudden changes and fluctuations in alertness – people may stare blankly into space for periods of time, seem drowsy and lethargic and spend a lot of time sleeping
- have slowed movement, difficulty walking, shuffling or appear rigid
- experience tremors – usually in the hands whilst at rest
- have problems with balance and be prone to falls
- bladder and bowel problems
- difficulties with swallowing
Memory is often less affected than with other types of dementia but people may be at more risk of mood and behaviour changes such as apathy, anxiety, depression, delusions and paranoia. One type of delusion, known as Capgras syndrome, in which the person believes that a friend or relation has been replaced by an imposter can be particularly difficult for families. Other symptoms may include changes in blood pressure, body temperature and impaired sense of smell.
Treating Movement Symptoms In Lewy Body Dementia
LBD-related movement symptoms may be treated with medications used for Parkinson’s disease, called carbidopa-levodopa. These drugs can help make it easier to walk, get out of bed, and move around. However, they cannot stop or reverse the disease itself. Side effects of this medication can include hallucinations and other psychiatric or behavioral problems. Because of this risk, physicians may recommend not treating mild movement symptoms with medication. Other Parkinson’s medications are less commonly used in people with LBD due to a higher frequency of side effects.
People with LBD may benefit from physical therapy and exercise. Talk with your doctor about what physical activities are best.
Clinical Features And Diagnostic Criteria Of Dlb Table 1 Clinical overlap and dissimilarities between dementia with Lewy bodies and Parkinson disease with dementia Full size table
Supporting clinical features for the diagnosis of probable or possible DLB are repeated falls, syncopes, hyposmia, severe autonomic dysfunction, hypersomnia, hallucinations in non-visual modalities, apathy, depression, and severe sensitivity to antipsychotic agents . However, since these changes also occur in advanced PD, they cannot differentiate DLB from PDD, e.g., the prevalence of neuroleptic sensitivity does not differ significantly between them .
A diagnosis of clinically probable DLB requires two or more core clinical features to be present, with or without indicative biomarkers, or the presence of only one core clinical feature but with one or more indicative biomarkers . Although the diagnostic specificity of these criteria is high , the sensitivity can be low , improving with additional supporting features such as biomarkers . A recent meta-analysis reported a pooled sensitivity, specificity, and accuracy of 60.2% , 93.8% , and 79.7% , respectively, for the diagnostic criteria of DLB . Thus, currently, approximately 20% of DLB diagnoses are incorrect .
What Is Dementia With Lewy Bodies And Parkinsons
Both conditions relate to decline in cognitive thinking and reasoning, loss of brain cells and abnormal alpha-synuclein protein clusters termed as Lewy bodies.
Both disorders have very similar symptoms, but the symptoms usually happen in a different order dependant on where the Lewy bodies first form.
Major similarities between Parkinson’s and Lewy Body Dementia include;
- Both disorders affect approximately one million people in the United States
- They both cause an impact to the brain nerve cells
- There is no cure for both of these conditions
- Symptoms that impact the body include stiffness, weakness and slowness in movements
- Symptoms that affect brain include: memory loss, attention span and impaired executive functioning
The protein – alpha-synuclein unusually builds up in the brain in aggregates, or clumps, called Lewy bodies. The location of those clumps makes a difference.
Also, people who have Lewy bodies dementia tend to exhibit greater variation in brain function ability than those with PD dementia.

