Tom Thought That Because Some Pink Tablets Relieved His Symptoms This Meant He Was Ok He Didn’t
I first suspected there was something wrong when I was travelling and I was writing a postcard to a friend of mine in, in Australia whose name is Anthony Diecopolis. And, and I got to the Anthony Diec and I couldn’t finish the opolis. And it’s very strange my hand had sort of gone into a sort of spasm and it just wouldn’t, wouldn’t finish writing the, the, the word. And so that’s a bit strange.
And so I went when, when I got I, I went to the doctor and said, “What on earth’s going on?” And I had since then I’d also developed this slight tremor in my right hand. He said, “Well it’s probably, Essential Tremor or trapped nerve or something like that”. And anyway, then it got a bit worse and then I was, I was recommended to go to a neurologist. And the neurologist had a look at me and gave me some pills. And he said, “Come back and tell me if these work”.
This is about, about sort of, nine months after my, my not being able to finish the, the postcard. And, and he said, “Take these pills”. And the pills worked. Magically the tremors stopped and I thought this is wonderful. And so I went back to the neurologist and I said, “Yes everything’s fine now. The pills have, the pills have worked.” And far from looking happy about this he looked rather, rather grave and he said, “I think you’d better go to another neurologist.”
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
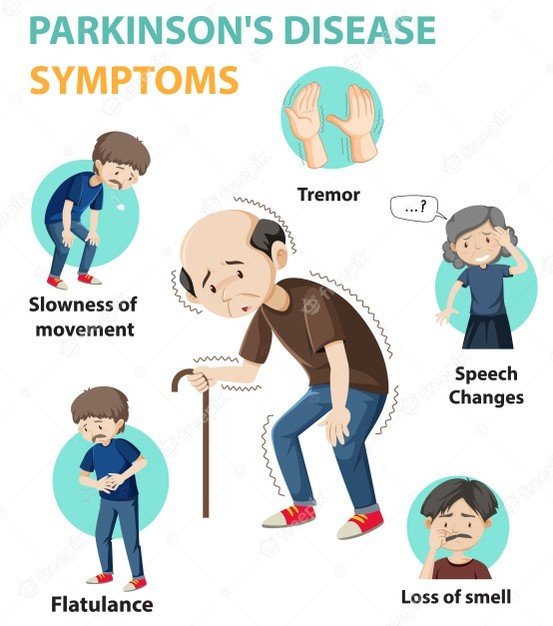
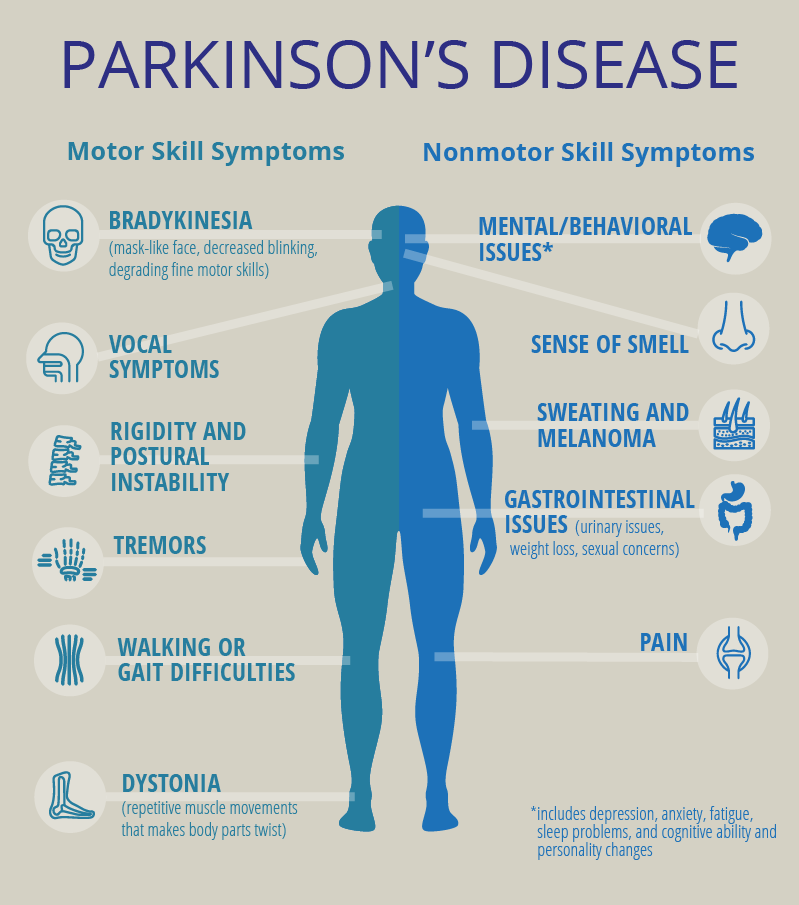
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Understanding Parkinsons Disease: Getting A Parkinsons Diagnosis
Once you start noticing some changes in your body that impact your daily life or are just simply bothersome, you should begin the process of figuring out if you have Parkinson’s disease. It may seem like a daunting undertaking, but don’t let fear stop you. Once you are diagnosed, you can start treating your symptoms and learning strategies that will help you feel better.
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Parkinsons Disease Signs And Symptoms: Before The Diagnosis
Mindy Bixby
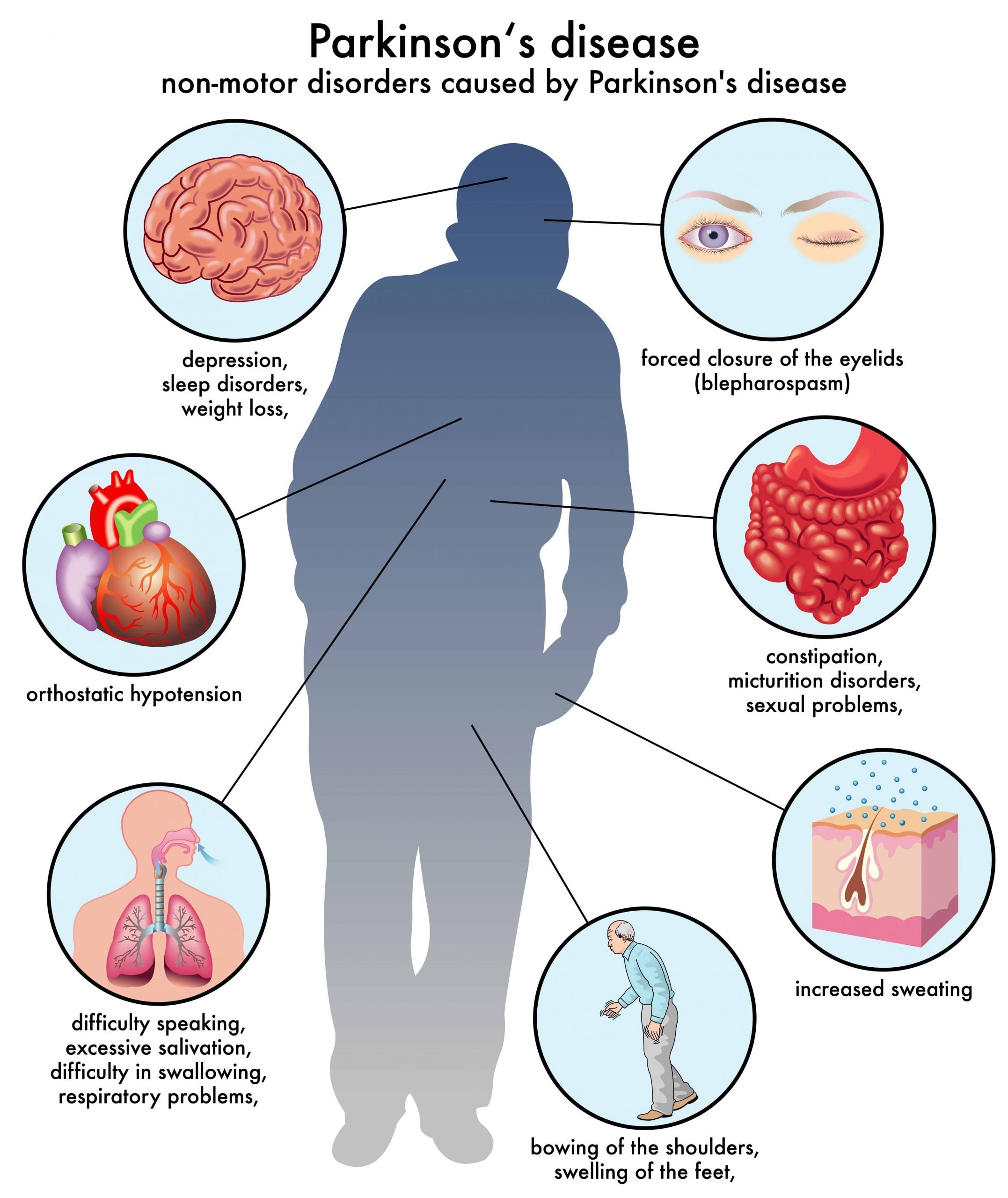
Neurologist, Mindy Bixby, DO, discusses the early signs and symptoms of Parkinson’s Disease, commonly referred to as non-motor symptoms.
Dr. Bixby explains how to identify and differentiate these symptoms from other disorders and when it’s time to visit your doctor for an accurate diagnosis.
She also covers therapy and treatment options if diagnosed with Parkinson’s Disease or other movement disorders.
Tags
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Conditions That May Be Mistaken For Parkinsons Disease
There are a few conditions that may be confused with Parkinson’s disease. These conditions can cause similar symptoms, and because there is no definitive test that proves you have Parkinson’s disease or any of these “similar” conditions. As you might imagine, this can make it challenging at times for doctors to figure out which condition you have. A few of the most common conditions that might look like Parkinson’s are:
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Methodological Limitations Of The Diagnostic Studies
When interpreting the literature about PD diagnosis, the following methodological issues should be considered:
- lack of long-term prospective clinical and pathological as a reference standard
- lack of operational definitions such as defining specialists or clinical diagnostic criteria
- unclear whether investigators were blinded to initial diagnosis
- sample sizes necessarily limited by the number of cases available with neuropathological outcomes
- PD trial age groups are often young as studies were performed by neurologists who see a younger population of people with PD
- most studies included people with established disease lasting some years
- varying geographical locations
- some studies are in specialised units and may not reflect the diagnostic accuracy of other units in the UK
- exclusion of some studies using magnetic resonance volumetry and magnetic resonance spectroscopy as they lacked appropriate population, intervention and outcome criteria
- lack of statistical details of diagnostic accuracy such as sensitivity, specificity and positive predictive values
- lack of economic evaluations of SPECT.
Treatment Options For Early Onset Parkinsons Disease
Parkinson’s treatment aims to slow the disease’s progression. Medication treatment options may include the following:
- Levodopa is a chemical that’s converted to dopamine in the brain. People with early onset Parkinson’s may experience more negative side effects, such as involuntary movements.
- MAO-B inhibitors can help reduce the breakdown of dopamine in the brain.
- Catechol-O-methyltransferase inhibitors can help extend Levodopa’s effects on the brain.
- Anticholinergics can help reduce tremors.
- Amantadine may be used to improve muscle control and relieve stiffness.
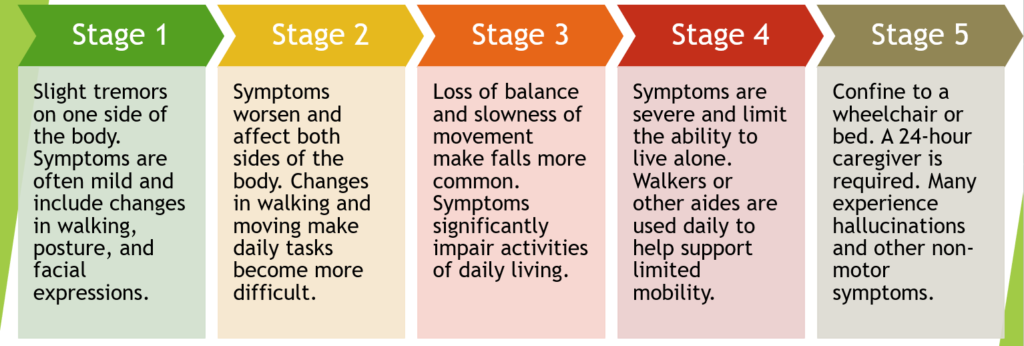
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Defining Populations At Risk For Parkinsons Disease
One of the areas of research that aims to aid in the early detection and treatment of PD is seeking to identify “biomarkers”—protein or chemicals in the blood, urine, or cerebrospinal fluid that reliably help diagnose PD, particularly at the early stage. For example, a recent study detected aggregates of alpha-synuclein in the cerebrospinal fluid. These aggregates were found in PD patients but not patients with other neurologic disorders. Many research studies are attempting to identify new biomarkers, particularly those that may even predict whether someone will develop PD over time.5
Tips For Caring For Someone With Parkinsons Disease
Caring for a loved one with early onset Parkinson’s can be difficult. If you’re a caregiver for someone with this condition, it’s important that you remember your own emotional and physical health.
Not only are you dealing with a difficult diagnosis, you’re also managing an increased number of responsibilities. Burnout is common in caregivers, so make sure you’re checking in with your own needs.
The Michael J. Fox Foundation Center for Parkinson’s Research recommends these tips for caregivers:
Braaks Hypothesis On How Parkinsons Disease Begins
Braak’s hypothesis, named for professor Heiko Braak, MD, who outlined the theory in 2003, suggests that rather than beginning in the brain, Parkinson’s disease begins in the periphery of the body. Braak’s hypothesis proposes that the earliest signs of PD are found in the gut and the olfactory bulb, an area of the brain involved in the sense of smell.2-4
The accumulation of the protein alpha-synuclein is believed to begin in the gastrointestinal tract or the olfactory bulb before progressing to other areas of the brain. After the aggregates of alpha-synuclein have formed, they appear to be capable of growing and spreading from nerve cell to nerve cell across the brain.2-4
The appearance of alpha-synuclein aggregates coincides with the appearance of symptoms: alpha-synuclein aggregates in the brainstem correlates with the onset of motor symptoms. Appearance of alpha-synuclein aggregates in the cortex correlates with dementia and cognitive dysfunction.2-4
What Parkinsons Diagnosis Criteria Do Doctors Use
Until the 1980s, there was no formal diagnostic criteria for Parkinson’s disease. Beginning with James Parkinson’s 1817 article, “An Essay on the Shaking Palsy,” and Margaret Hoehn and Melvin Yahr’s description of the five stages of motor progression in 1967, scientists focused on the unique ways Parkinson’s disease affects movement. A few scientists also noted non-motor symptoms like issues with automatic body functions, such as heart rate and blood pressure.
With the discovery in the 1950s of levodopa, a drug that gets turned into dopamine in your brain and thus replaces some of the dopamine that is lost due to PD, and the discovery of how dramatically levodopa improves motor symptoms, the medical community continued to focus more of their efforts on defining and treating Parkinson’s as a motor condition.7
Other Challenges Of Diagnosing Parkinsons Disease
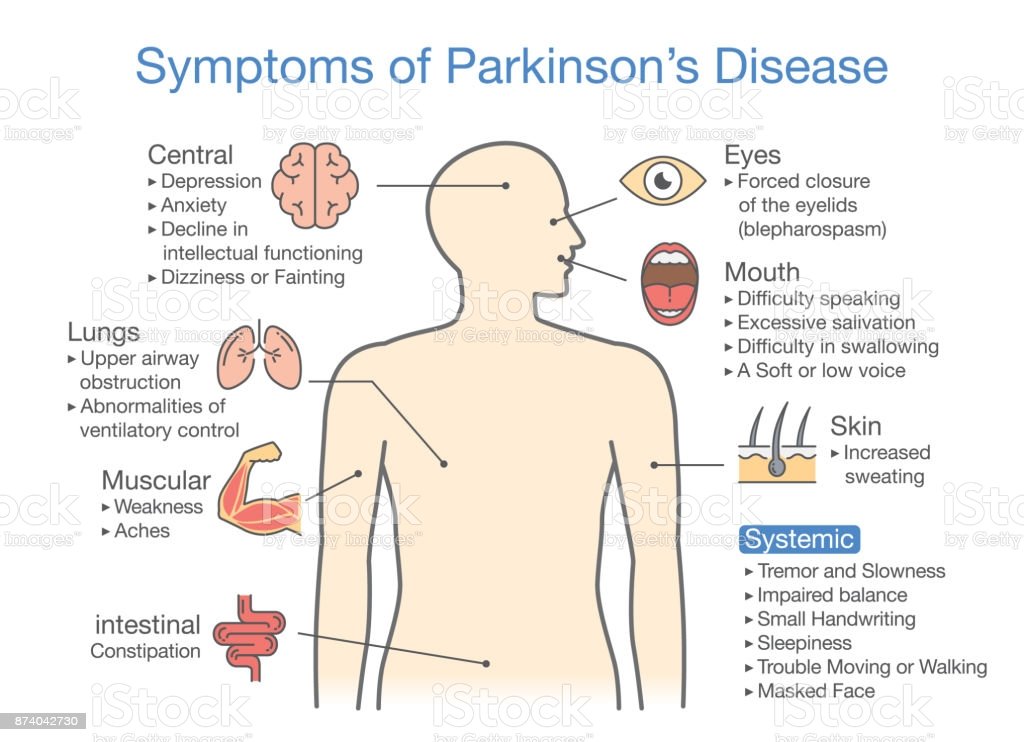
Parkinson’s disease progresses slowly, often with non-motor symptoms appearing months or years before motor symptoms. This can make it challenging for doctors to diagnose you in the early stages, especially since the diagnostic criteria is based mostly on motor symptoms. You may have to wait until your symptoms progress for you and your doctor to confirm your diagnosis.14
Age and gender can be another issue. Since Parkinson’s is associated more with older men, doctors may not think their younger or female patients have Parkinson’s.5 On the other hand, since the disease is associated with aging, your symptoms may be blamed on “getting older.”
Remember that movement disorder specialists are extremely knowledgeable about Parkinson’s disease and can help put the pieces together where other more generalized doctors may not. Never hesitate to fight for the care you deserve.
Related: Here’s what’s important to remember if you were just diagnosed with Parkinson’s disease.
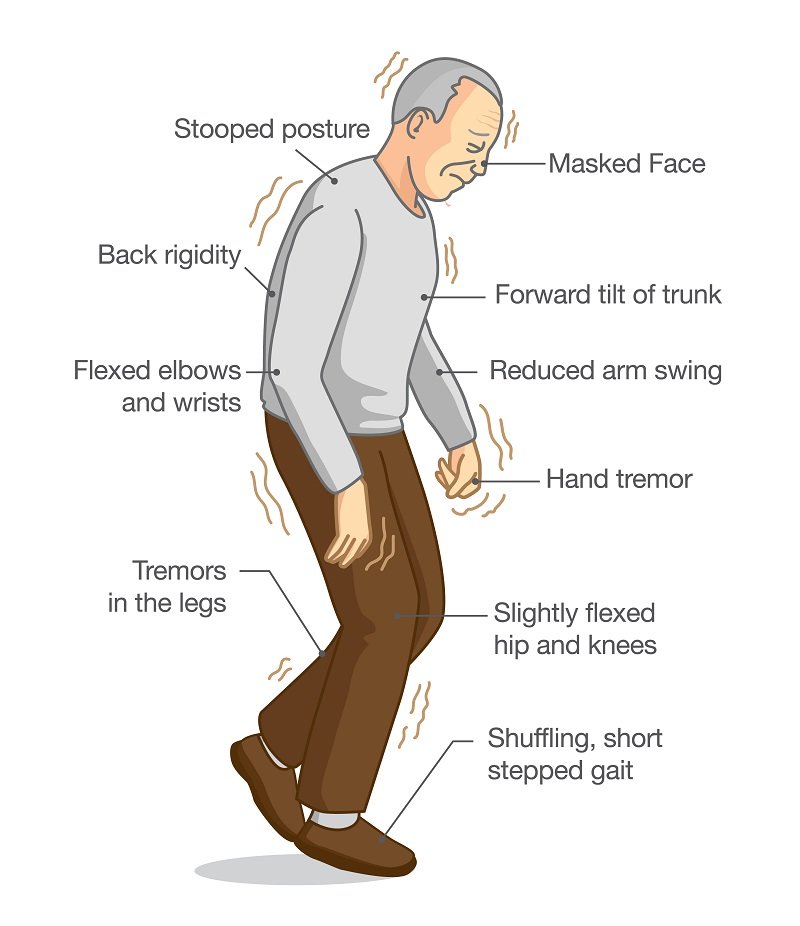
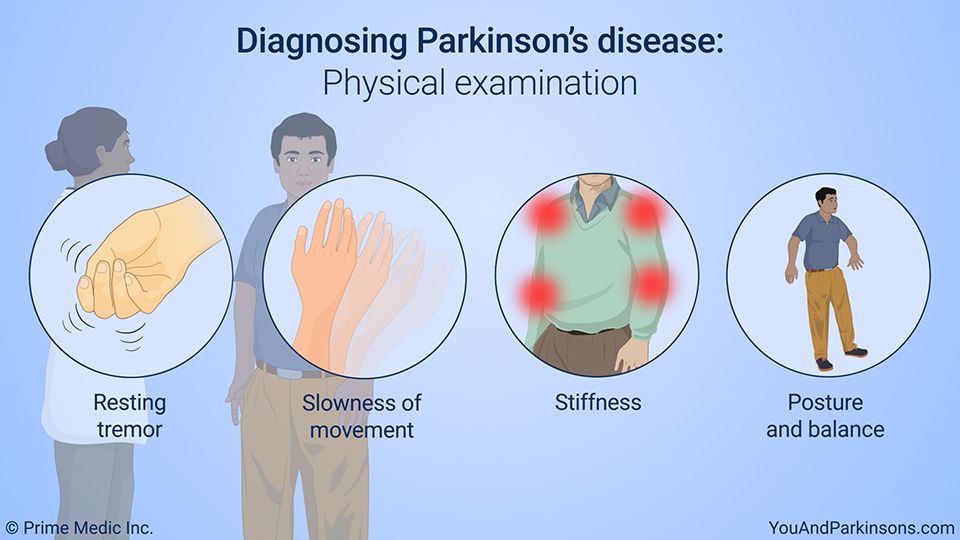
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Depression May Be An Early Symptom Of Parkinsons
Depression is one of the most common, and most disabling, non-motor symptoms of Parkinson’s disease. As many as 50 per cent of people with Parkinson’s experience the symptoms of clinical depression at some stage of the disease. Some people experience depression up to a decade or more before experiencing any motor symptoms of Parkinson’s.
Clinical depression and anxiety are underdiagnosed symptoms of Parkinson’s. Researchers believe that depression and anxiety in Parkinson’s disease may be due to chemical and physical changes in the area of the brain that affect mood as well as movement. These changes are caused by the disease itself.
Here are some suggestions to help identify depression in Parkinson’s:
- Mention changes in mood to your physician if they do not ask you about these conditions.
- Complete our Geriatric Depression Scale-15 to record your feelings so you can discuss symptoms with your doctor. Download the answer key and compare your responses.
- delusions and impulse control disorders
If Its Not Parkinsons Disease What Could It Be
Here are some possibilities:
Side effects of medication: Certain drugs used for mental illnesses like psychosis or major depression can bring on symptoms like the ones caused by Parkinson’s disease. Anti-nausea drugs can, too, but they typically happen on both sides of your body at the same time. They usually go away a few weeks after you stop taking the medication.
Essential tremor: This is a common movement disorder that causes shaking, most often in your hands or arms. It’s more noticeable when you’re using them, like when you eat or write. Tremors caused by Parkinson’s disease usually happen when you’re not moving.
Progressive supranuclear palsy: People with this rare disease can have problems with balance, which may cause them to fall a lot. They don’t tend to have tremors, but they do have blurry vision and issues with eye movement. These symptoms usually get worse faster than with Parkinson’s disease.
Normal pressure hydrocephalus : This happens when a certain kind of fluid builds up in your brain and causes pressure. People with NPH usually have trouble walking, a loss of bladder control, and dementia.
How Is Parkinsons Disease Tested And Diagnosed
At Banner Health, our neurologists have years of experience in testing and diagnosing Parkinson’s disease. Our team of compassionate experts knows that each patient is different, so we work with you to quickly find the right diagnosis to begin building your treatment plan.
Parkinson’s is not simple to diagnose. No test exists to diagnose Parkinson’s disease. Doctors test and diagnose Parkinson’s based on your medical history, symptoms and neurological and physical exams.
Many times a primary care provider is the first to suspect a Parkinson’s diagnosis. If you’re experiencing symptoms such as tremors, shaking, slow movement, stiffness and/or trouble with balance, talk to your doctor or seek the opinion of a neurologist. Banner Health neurologists are movement disorder specialists, who have experience and specific training to assess and treat Parkinson’s.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
Learn More About Parkinsons Disease: Overview
Tests For The Diagnosis Of Parkinsons Disease
There’s no specific single test that allows a direct diagnosis of Parkinson’s disease. This means that it can’t be detected by a blood, urine, or cerebrospinal fluid test, as well as an imaging test.
We hope that, in the future, researchers will be able to detect a biomarker that will facilitate direct diagnosis. However, for the time being, we have to use what’s available.
The Michael J. Fox Foundation explains to us that the diagnosis is made from the patient’s symptoms, their history, the answers to certain questions, and the findings found in the check-up. The experience and knowledge of the specialist play a key role in this. For this reason, they recommend consulting a specialist in movement disorders or a neurologist with specialized training in Parkinson’s.
On the other hand, the MSD Manual points out that when Parkinson’s disease isn’t certain, the doctor may prescribe a drug called levodopa. If the person shows a clear improvement after taking it, then the diagnosis is that they have Parkinson’s.
How Will Parkinson’s Disease Affect Your Life
Finding out that you have a long-term, progressive disease can lead to a wide range of feelings. You may feel angry, afraid, sad, or worried about what lies ahead. It may help to keep a few things in mind:
- Usually this disease progresses slowly. Some people live for many years with only minor symptoms.
- Many people are able to keep working for years. As the disease gets worse, you may need to change how you work.
- It is important to take an active role in your health care. Find a doctor you trust and can work with.
- Depression is common in people who have Parkinson’s. If you feel very sad or hopeless, talk to your doctor or see a counsellor.
- It can make a big difference to know that you’re not alone. Ask your doctor about Parkinson’s support groups, or look for online groups or message boards.
- Parkinson’s affects more than just the person who has it. It also affects your loved ones. Be sure to include them in your decisions.
What Are The Symptoms Of Parkinson’s Disease
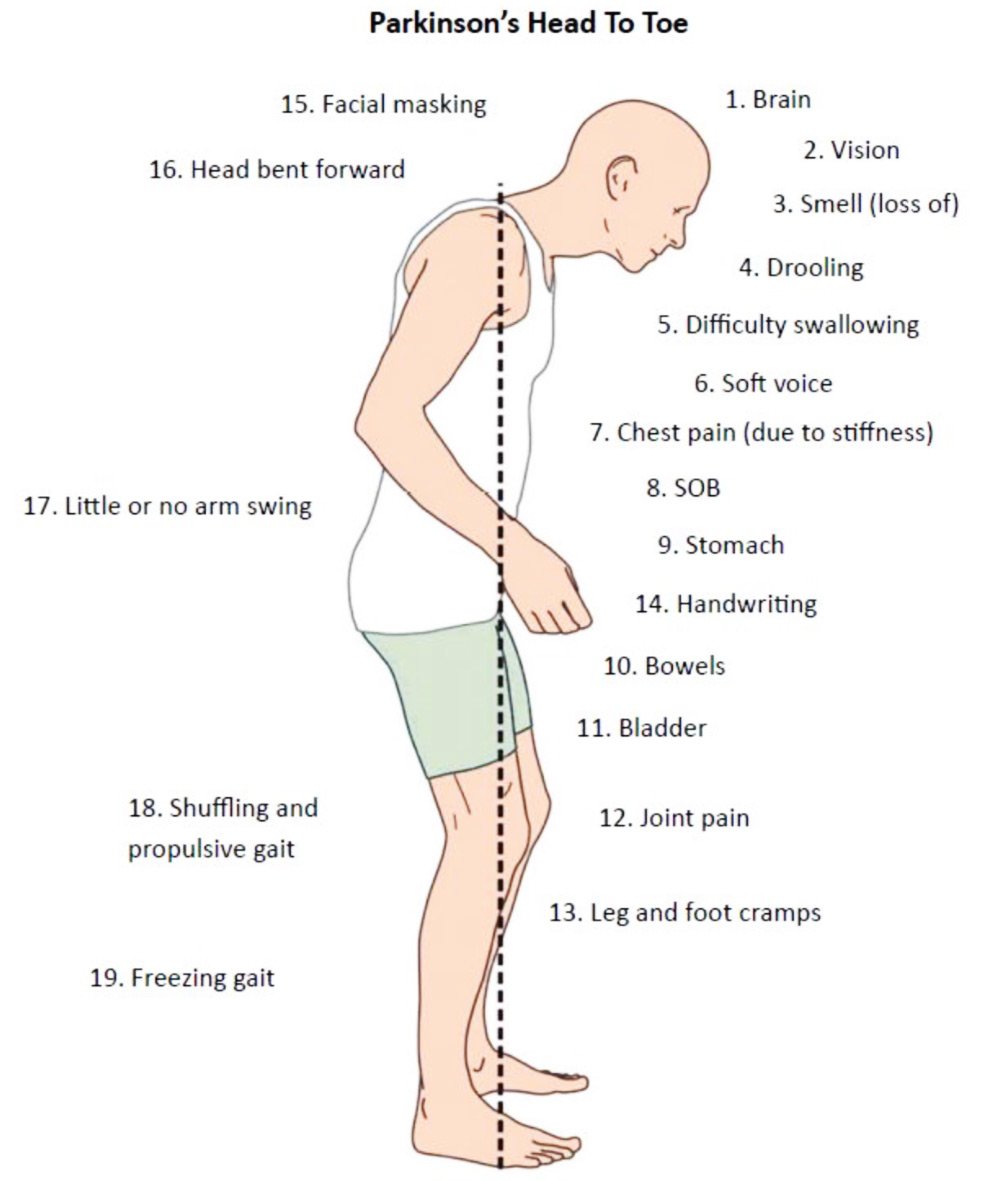
The main symptoms of Parkinson’s disease are:
- tremor or shaking, often when resting or tired. It usually begins in one arm or hand
- muscle rigidity or stiffness, which can limit movement and may be painful
- slowing of movement, which may lead to periods of freezing and small shuffling steps
- stooped posture and balance problems
The symptoms of Parkinson’s disease vary from person to person as well as over time. Some people also experience:
- loss of unconscious movements, such as blinking and smiling
- difficulties with handwriting
- drop in blood pressure leading to dizziness
- difficulty swallowing
- sweating
Many of the symptoms of Parkinson’s disease could be caused by other conditions. For example, stooped posture could be caused by osteoporosis. But if you are worried by your symptoms, it is a good idea to see your doctor.
What Is The Prognosis For Parkinsons Disease
The rate at which Parkinson’s progresses varies from patient to patient. Some patients experience its changes over 20 years or more. While others find the disease advances quicker.
Parkinson’s is not a fatal disease. However, secondary complications from symptoms may increase falls, blood clots or pneumonia, which can be life-threatening. These are more common in later stages of Parkinson’s.
In general, the average life expectancy of Parkinson’s patients is similar to people without the disease.
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinson’s disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Decreased facial expressions: You may not smile or blink as often as the disease worsens; your face lacks expression.
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
How Do I Prevent Falls From Common Hazards
- Floors: Remove all loose wires, cords, and throw rugs. Minimize clutter. Make sure rugs are anchored and smooth. Keep furniture in its usual place.
- Bathroom: Install grab bars and non-skid tape in the tub or shower. Use non-skid bath mats on the floor or install wall-to-wall carpeting.
- Lighting: Make sure halls, stairways, and entrances are well-lit. Install a night light in your bathroom or hallway and staircase. Turn lights on if you get up in the middle of the night. Make sure lamps or light switches are within reach of the bed if you have to get up during the night.
- Kitchen: Install non-skid rubber mats near the sink and stove. Clean spills immediately.
- Stairs: Make sure treads, rails, and rugs are secure. Install a rail on both sides of the stairs. If stairs are a threat, it might be helpful to arrange most of your activities on the lower level to reduce the number of times you must climb the stairs.
- Entrances and doorways: Install metal handles on the walls adjacent to the doorknobs of all doors to make it more secure as you travel through the doorway.
Single Photon Emission Computed Tomography
In single photon emission computed tomography , a gamma ray-emitting radioactive isotope is tagged to a molecule of interest , which is given to the person with PD by intravenous injection. The labelled cocaine derivatives 123I-?-CIT and 123I-FP-CIT tropane) have most commonly been used, although only the latter is licensed in the UK. These label the presynaptic dopamine re-uptake site and thus the presynaptic neurone, which can be visualised in two-dimensional images. These demonstrate normal uptake in the caudate and putamen in controls and in people with essential tremor, neuroleptic-induced parkinsonism or psychogenic parkinsonism, but reduced uptake in those with PD, PD with dementia, MSA or PSP.
How useful is SPECT in discriminating PD from alternative conditions?
