Can I Take Other Medicines While I Take Parkinsonss Medication And How Can A Pharmacist Help
Many people with Parkinson’s take other medications to treat various unrelated conditions. Because some medications can interact with others, it is very important to tell your doctor or healthcare professional about any other medicines, remedies or supplements you are taking, including over the counter medications that have been bought without a prescription.
Some medications may have harmful interactions with other medications known as contraindications, and may worsen your symptoms or bring on Parkinson’s-like symptoms that will disappear if you stop taking that medication. Telling your doctor about other medicines, remedies or supplements you take can help to reduce the risk of contraindications.
Getting the balance of Parkinson’s medications right for each individual is complicated and very important so if you have any concerns about the medication you are taking, you will need to discuss this directly with your doctor who will continue to monitor your medication on a regular basis.
You can also talk to your pharmacist as he or she is qualified to prepare and dispense medicine, and to offer advice on your prescribed medications. Pharmacists are always willing to listen to concerns you may have and to help if they can. for instance, they should be able to advise about any possible side effects from the medication that you may experience. If your pharmacist cannot help then he or she will refer you to your doctor.
See also Managing medication.
What Could Help Me To Manage My Medication Better Eg Pill Dispensers Dosing Alarms Etc
If you have a number of different medications to take throughout the day, you may find it helpful to use a timer, rather like an alarm clock, which will remind you take another dose.
You can also buy various types of tablet organisers that have a compartment for each day which can be very useful to keep with you if you are going out. For advice on this speak to your pharmacist or look online, for example the Disabled Living Foundation website or commercial companies such as Tabtime.
See also Managing medication.
How Do I Get An Ongoing Supply And Can I Obtain Medication If I Go To Other Countries
You will need to discuss with the doctor or specialist who prescribes your medication how you can get an ongoing supply. This will vary according to where you live and the local services available, but usually arrangements are made for repeat prescriptions to be available at a pharmacy which is convenient for you.
Your doctor will also be able to tell you how many weeks’ supply you can have in advance. Again this varies from country to country so you will need to ask about this.
Not all medications are licensed in every country, and some are known by different names so it is a good idea to check the local names of medications you use before you travel if you are going abroad.
For information on availability at other international destinations it is best to check with your pharmacist, or local Parkinson’s association. This website contains contact details for Our members, Other Parkinson’s organisations.
As some medications are difficult to obtain in certain countries, and also in some cases, the quality may not always be of the highest standards, it is best to ensure that you take with you all the medications that you will need.
Carrying a few spare with you is always a good idea in case of any delays in your return. It is also advisable to carry a spare prescription with you just in case you do run out of medication while you are away.
For more information and useful suggestions on medication and travel, see Travel and relocating.
Full List Of Medications Approved For The Treatment Of Parkinsons Disease In The Usa
Below is a full list of Parkinson’s medications that have been approved to treat Parkinson’s in the United States. This material is intended to provide you with information. It should not be used for treatment purposes, but rather as a source for discussion with the patient’s own physician. Work with your physician to determine which medications are best for you, and know the risks and benefits of each.
What’s Hot In Pd When Should You Start Medication Therapy For Parkinsons Disease
One of the most common questions that we receive on both on the Parkinson’s Foundation Ask the Doctor forum, and on the1-800-4PD-INFO Helpline is “when should I start medications for my Parkinson’s disease.” This months What’s Hot in PD column will focus on this simple, but critically important question.
The most important factor in initiating medications for an individual patient is whether Parkinson’s symptoms are affecting quality of life, or alternatively whether symptoms are affecting work performance. Bothersome Parkinson’s symptoms commonly include motor issues , and/or non-motor issues . Most experts agree that there is no benefit to delaying medication therapy if bothersome symptoms appear, and there may be risks in delaying treatment, especially if a treatment delay results in unsteadiness, falls, and fractures.
Over the last 10-20 years the thinking has evolved on when and how to initiate medication therapy for early Parkinson’s disease. Most experts agree that the medication dosage and the timing of the medication dosage should be carefully monitored in order to maximize the control of potentially responsive Parkinson related symptoms. The recommendation that patients should be started on dopamine agonist instead of levodopa has faded over the last decade, especially with the emergence of impulse control disorders and other dopamine agonist associated side effects.
How Soon Will My Treatment Start How Long Will It Last And Will I Have To Pay
Treatment will usually start when a diagnosis has been confirmed. Initially, a single medication or a combination of different medications can be used. Medical treatment is started in low doses and increased gradually.
Once started, medication is generally taken for the rest of your life, with adjustments to the types and dosage as your symptoms alter over time.
Over the past few decades, there have been great advances in the effectiveness of Parkinson’s medications and they can provide good symptom control for a number of years. You will need to work closely with your doctor in finding the right balance and combination of medications to suit you, monitoring your response and their effectiveness on an ongoing basis in order to maintain good control of your symptoms.
Each country has its own guidelines and policy on the provision of medications so you will need to check with your healthcare professional, social worker or government office responsible for healthcare.
If you have private medical insurance, always check with them what cover they provide for medication at any stage of your treatment as this will be dependent on the terms of your individual policy cover.
If I Cannot Take A Particular Medicine Are There Others That Are Equally Good
Some medications interact with others so you should always discuss any change in medication with your doctor so that together you can find a substitute that works for you.
Most medications have two names. One is a generic name that always uses a small letter and describes the active ingredient in the medication, for example co-careldopa. This is likely to be the same name no matter what country you live in. The other is a brand or trade name by which the medication is marketed. This can vary from country to country and always uses a capital letter, for example Sinemet.
See also Types of medication.
What Are The Different Types Of Pain Experienced By People With Parkinsons
Five main types of pain are common for people with Parkinson’s. Multiple types may be present simultaneously or occur at different points throughout a person’s path with Parkinson’s. Recognizing which kind of pain is present can help you optimize treatment, as can paying attention to what activities or times of day make your pain better or worse.
Musculoskeletal pain
Musculoskeletal pain that affects muscles, bones, tendons, ligaments, and/or nerves. The pain can be localized or generalized and can fade or intensify at different times. Existing musculoskeletal pain can be exacerbated by Parkinson’s.
Neuropathic pain
Rather than being caused by a physical injury, this type of pain is caused by damage to the somatosensory nervous system or a disease affecting the somatosensory nervous system, which responds to external stimuli like touch, temperature, and vibration. It tends to be fairly consistent throughout the day and is present no matter what activity you’re doing. Unlike the aching you may feel when you’re doing a strenuous physical activity, neuropathic pain feels more like a tingly, crawly, uncomfortable sensation.
Dystonic pain
Dystonia, the movement disorder in which involuntary muscle contractions cause repetitive or twisting motions, is often very painful. Many people with Parkinson’s experience dystonia as a motor symptom, whether it’s localized , in multiple nearby body parts , or all over .
Akathisia
Central pain
What Side Effects Should I Be Aware Of And What Can I Do To Reduce Them
As with any medication, there can be side effects and these may differ from one medication to another. Each person’s reaction to a medication is individual and many experience little or no side effects.
Each prescribed medication has an information leaflet that outlines possible side effects and it is very important that this leaflet is read prior to taking the medication. If you have any concerns, please ensure that you discuss these with your doctor, health professional or pharmacist as soon as possible so that they can advise or change the medication if necessary.
It is important to follow the instructions you are given for taking each individual medication, as some should be taken in a different way or at a different time of day to another. By following this advice you can minimise side effects. Taking the correct dose, on time, is also very important.
See also Managing medication.
What Would Happen If I Try To Manage Without Medication For Some Time
Any change to your medication regime must be discussed with your doctor so that you understand how this might affect you.
Parkinson’s medication should never be stopped abruptly as this can be dangerous. If both you and your doctor agree to stop any medication, it will be necessary to do so by very gradually reducing the medication dose.
If you agree to do so, it would be useful if you kept a diary to monitor how this was affecting your symptoms. This can help to highlight any changes in symptom pattern, or in your emotions or behaviour that may be related to medication.
Writing down your own individual experiences on a day-to-day basis can also help you to talk about any changes in your symptoms and your feelings with your doctor. This can be very useful, particularly as appointments are often too short for doctors to ask lots of questions, and your visit may be on a day when your symptoms do not follow their general pattern.
See also Keeping a diary.
Apart From Taking Medication What Else Can I Do To Help Myself
Parkinson’s is a very individual condition and so each person will find their own way of coping and managing their symptoms.
Often a combination of approaches is helpful, but before making any changes it is very important that you discuss with your doctor any proposed changes. You may need to adopt a trial and error approach to find what works best for you.
Conventional and complementary treatments:
- Conventional Therapies, such as physiotherapy, occupational therapy, speech and language therapy
- Complementary therapies, such as aromatherapy, reflexology, yoga and Tai Chi
- Surgical treatments such as Deep brain stimulation are also available but are not suitable for everyone and should only be undertaken after very careful consideration and discussion with your doctor.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Parkinsons Disease Therapy When To Start And What To Choose
http://doi.org/10.17925/ENR.2008.03.02.34Article Information
Article:
Timing of Treatment
Treatment Choices
Levodopa
Dopamine Agonists
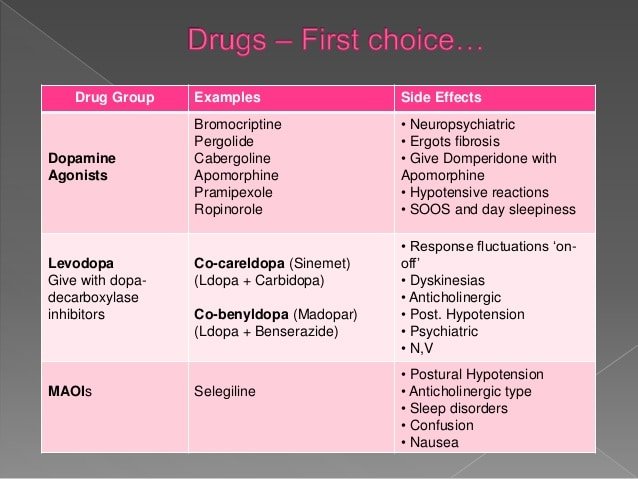
Non-ergot-derived dopamine agonists such as pramipexole, ropinirole, rotigotine patch and apomorphine injections are used widely as monotherapy and adjuvants to levodopa in PD. The older drug bromocriptine and other ergot-derived agonists such as pergolide and cabergoline are now rarely used due to an increased risk of fibrotic valvular heart and lung disease.18–20 A recent study by Moller et al. suggests a possible antidepressant action of pramipexole and beneficial effect on tremor when used as an adjuvant therapy to levodopa compared with placebo in advanced PD.21
Monoamine Oxidase-B Inhibitors
Anticholinergics/Catechol O-Methyltransferase Inhibitors/Amantadine
Levodopa versus Dopamine Agonists
Summary
Article Information:
What Should I Know About Parkinsons Disease And Medications
There have been rapid and remarkable changes over the past decade in treating Parkinson’s disease . The development of new medicines and the understanding of how best to use them and the older drugs have significantly improved the quality of life for people with the disease.
There is currently no treatment that has been proven to affect the disease progression or development of medication that can slow the disease process. There are two general approaches to the treatment of PD— improve the symptoms with medications and engage in physical therapy. Most patients with PD can be adequately treated with medicines that alleviate their symptoms. For the approximately 15% of patients for whom medicines are not sufficiently effective, new, highly effective, and safe surgical treatments are available.
Choices about medicines made early in the course of the disease have a strong impact on the long-term course of the illness. Therefore, you should seek the advice of doctors specially trained in treating PD even when the illness is only suspected. Movement disorders specialists are neurologists who have completed their training in neurology and have received special advanced training in treating PD and other related diseases.
Do I Need To Take Medication How And When Should I Take It
In the beginning, a single medication or a combination of different medications can be used with medical treatment being started in low doses and increased gradually. Medication is always individual and can vary greatly between people. Therefore, medical treatment requires follow-up by a physician with a good knowledge of the condition.
Your doctor will be on hand to advise when to take your medication so that it works best for you, for example before, with or after eating, whether you should take with or without protein etc. By working closely with your doctor, you will be able to find the right balance and combination of medications to suit you. It is important that you monitor your response to the medication regularly so that medicine remains as effective as possible in managing your symptoms. Again, if you are unsure or do not understand everything the doctor has told you, please ask him or her to explain again as it is important for you to follow the advice you are given accurately.
Some people find that combining medication with conventional therapies such as physiotherapy, occupational therapy and speech and language therapy, as well as surgical treatments or complementary therapies such as aromatherapy, reflexology, yoga, tai chi is helpful. But if you are considering these therapies it is always advisable to discuss with your doctor first.
See also:
See also Treatments and Therapies.
Levodopa: The Most Effective Drug For Treating Parkinsons
Levodopa, also known as L-DOPA, has long been, and continues to be, the most effective drug in treating Parkinson’s disease symptoms. Most people with Parkinson’s disease will take this drug at some point. There are side effects that can occur with Levodopa including nausea, fatigue and orthostatic hypotension. Often these side effects can be successfully treated so that Levodopa can be tolerated better. In addition, as the disease progresses and the brain has less ability to produce and process dopamine, dyskinesias, or involuntary movements can develop from Levodopa.
Read about dyskinesia, the main levodopa side effect
What Are The Surgical Treatments For Parkinsons Disease

Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
If I Go Into Hospital What Happens About My Medication
It is vital to get the right medication at the right time every time, not just at the set times scheduled for hospital medication rounds, in order for your symptoms to continue to be well managed and to speed up recovery. If admission is as an emergency, this can be more difficult as staff may not have a clear picture of your needs and may be very busy, so it is a good idea to discuss this scenario with those close to you so that they can liaise with staff on your behalf.
For any admission it is essential that staff have clear notes regarding your medication. A medication diary can be very helpful with this, specifying:
- dosage and timing of each medication you have to take, including complementary, trial, non-Parkinson’s medications and over the counter medications
- clear instructions on how each medication should be taken, e.g. with food, with water, avoiding protein etc.
Some hospitals will allow you to self-medicate but this is not always the case.
Make sure that you take plenty of each medication with you into hospital as they might not have ready supplies, and ensure that the dosage on the label is what you have indicated on any medications list you provide. If not, staff can sometimes only be authorised to dispense what is written on the label, which could be incorrect.
The Bottom Line On On/off Periods With Parkinsons Meds
Managing the cycling between on and off periods with Parkinson’s medications can be incredibly frustrating, but luckily, there are a number of effective ways to help reduce the peaks and valleys of motor symptoms.
Scientists are still exploring new and improved ways to help combat off periods with Parkinson’s drugs, according to the Michael J. Fox Foundation for Parkinson’s Research. You may even consider participating in one of these clinical trials, which you can learn more about with the Michael J. Fox Foundation’s clinical trial matching tool.
Even more exciting is the fact that researchers are also working diligently to try to improve Parkinson’s treatments in general—really looking into the crux of the disease to try to slow its progression overall, which would in turn help with this on-off period struggle, says Dr. Hui.
“There are a number of clinical trials going on, so I think we should also stay tuned for development of to slow progression of disease,” she says.
When Is It Best To Start The Parkinsons Drug Levodopa

Earlier treatment with levodopa provides symptomatic relief to those with symptoms but does not appear to slow Parkinson’s disease from progressing. Therefore, timing is best determined by symptoms.
The treatment of Parkinson’s disease is complex. Levodopa is the main drug used to reduce tremors and muscle stiffness. Whether it modifies the course of the disease or becomes less effective over time is debated, and it can have side effects, so patients and clinicians sometimes prefer to delay starting treatment.
This Dutch trial involved 445 participants with a recent diagnosis of Parkinson’s disease, enrolled over five years. About half took levodopa for 80 weeks, and half placebo for the first 40 weeks and levodopa for the last 40 weeks. There was no difference in symptoms between the groups at the end of the study.
This evidence supports current guidance to start levodopa when symptoms begin to affect the quality of life and confirm that it has insufficient impact on disease progression to justify earlier treatment.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
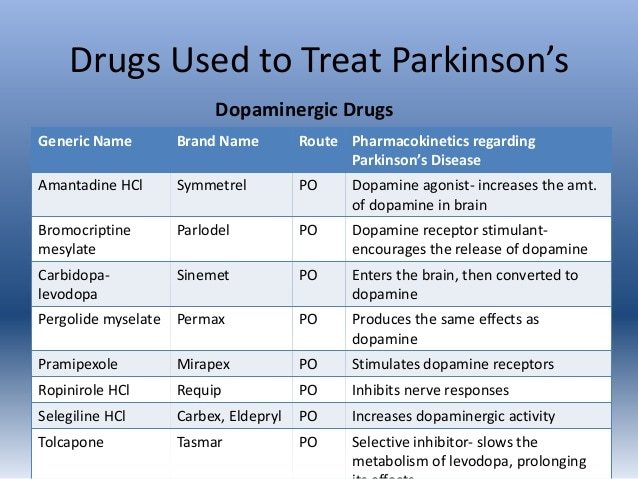
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
What Are The Most Common Medicines Used To Treat Pd
Sinemet®
Levodopa is the most commonly prescribed and most effective medicine for controlling the symptoms of PD, particularly bradykinesia and rigidity.
Levodopa is a chemical found naturally in our brains. When given as a medicine, it is transported to the nerve cells in the brain that produce dopamine. It is then converted into dopamine for the nerve cells to use as a neurotransmitter.
Sinemet is made up of levodopa and another drug called carbidopa. Levodopa enters the brain and is converted to dopamine while carbidopa prevents or lessens many of the side effects of levodopa, such as nausea, vomiting, and occasional heart rhythm disturbances. It is generally recommended that patients take Sinemet on an empty stomach, at least ½ hour before or one hour after meals.
There are two forms of Sinemet: controlled-release or immediate-release Sinemet. Controlled-release Sinemet and immediate-release Sinemet are equally effective in treating the symptoms of PD, but some people prefer the controlled release version. Ask your doctor which approach is best for you.
Dopamine agonists
Dopamine agonists are medicines that activate the dopamine receptor. They mimic or copy the function of dopamine in the brain.
Parlodel®, Requip®, and Mirapex® are all dopamine agonists. These medicines might be taken alone or in combination with Sinemet. Generally, dopamine agonists are prescribed first and levodopa is added if the patient’s symptoms cannot be controlled sufficiently.
Symmetrel®
What Can I Do On A Regular Basis To Manage My Pain
Remember, you’re your best advocate as you understands how your pain feels. Understanding and communicating the kind of pain you’re experiencing can greatly inform your treatment plan and will allow your doctors to address the type and severity of your specific pain. Keep your care team informed about activities that cause pain or the times of day your pain is worst so they can help fine-tune your care plan. Do you notice the pain starting to creep in at a certain point after you take your medication? Do you feel fine when you bike but experience pain when you jog? Did you start experiencing this pain before or after your Parkinson’s diagnosis? Taking stock of these sorts of questions can be helpful as you work with your care team to effectively treat your pain.
Incorporating approved medications and following the pain ladder can also help you find the right pain management solution, as can taking steps in your everyday life to be an active participant in your own pain management. Regular stretching, heat and cold treatments, exercise, yoga, and dance can all help reduce your pain, and they are all steps that you can take on your own. Making adjustments to your home and workspace, such as minimizing places where fall risks are likely, using an ergonomically designed desk, sleeping in a comfortable bed, and wearing clothes and shoes that don’t exacerbate pain, can help you establish a more pain-free daily routine.
What Will Happen If I Forget To Take My Medication
It is important to discuss with your doctor what would happen if you do forget to take your medication so that you are prepared, and understand what action you should take.
If you forget to take your medication you may notice that your symptoms become worse, often known as ‘wearing-off’, as the effects of the medication literally wear off. Symptoms may then either re-emerge or worsen before the next dose of medication is due. This tends to begin to happen over a period of time as Parkinson’s progresses and when it occurs, the control of both motor and non-motor symptoms fluctuates. This phenomenon is very individual and there is no standard time frame for when this may occur or what symptoms you might experience.
The range of ‘wearing-off’ symptoms is very broad so any changes in your usual pattern should be discussed with your doctor as he or she may be able to adjust your medication regime to help control these symptoms better.
See also Wearing-off and motor fluctuations and Managing medication.
Managing Medication Interactions And Side Effects
All prescribed medications can have potential side effects, including those used to treat Parkinson’s. Some things you think are symptoms of Parkinson’s may actually be side effects of medication. Some people’s side effects will have a big impact on their lives and have to be kept under control along with the symptoms.
Side Effects And Problems With Dopamine Agonists
Common side effects of dopamine agonists include:
- Nausea and vomiting
- Hallucinations or delusions and confusion
- Existing dyskinesias becoming more troublesome initially
If you are taking Cabergoline , Pergolide or Bromocriptine your neurologist or GP will have to arrange a chest CT scan or ultrasound of your heart yearly as over time these medications may effect heart or lung tissue.
This precaution does not apply to the other dopamine agonists available in Australia.

