People Who Already Have Pd: Should I Get Tested And What Do I Do With The Results
Up until recently, even people with PD with a very extensive family history of PD would not necessarily receive genetic testing because there were no clear uses for the results. There has been research directed at figuring out whether PD caused by or associated with certain mutations have particular clinical characteristics . However, there remains so much variability in clinical characteristics even among people with the same PD mutation, that there are still no clear practical implications in knowing whether a PD patient harbors a particular mutation. There is also, so far, no difference in treatment or management of PD whether or not the patient harbors one of the known mutations. That may change however, with the advent of clinical trials that target particular mutations.
There are two genes that have received particular attention recently because medications are being developed that target those with mutations of these genes.
GBAis a gene that increases the risk of developing PD. The gene encodes for the GBA enzyme, a protein used by the body to break down cellular products. Having two abnormal GBA genes causes Gaucher’s disease, which is characterized by the buildup of these cellular products resulting in fatigue, bone pain, easy bleeding and an enlarged spleen and liver. When a person inherits only one abnormal gene, he or she does not develop Gaucher’s disease, but does incur a small increased risk of PD. Most people with one mutated GBA gene do not develop PD.
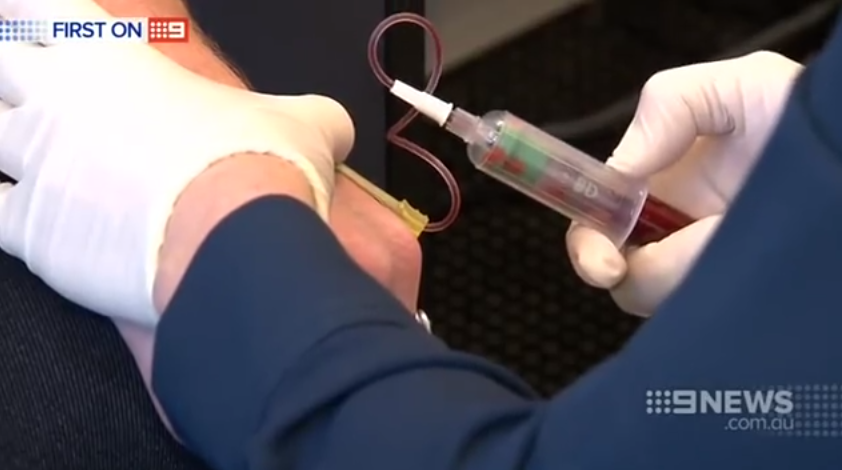
Blood Test To Detect Parkinson’s Disease Could Lead To Earlier Treatment
Australian researchers hope discovery can be used to diagnose disorder – now done through process of elimination
Last modified on Wed 20 Sep 2017 19.27 BST
Researchers have developed the world’s first blood test that can detect the abnormal metabolism of blood cells in people with Parkinson’s disease, which means the blood test could be used to diagnose the disorder.
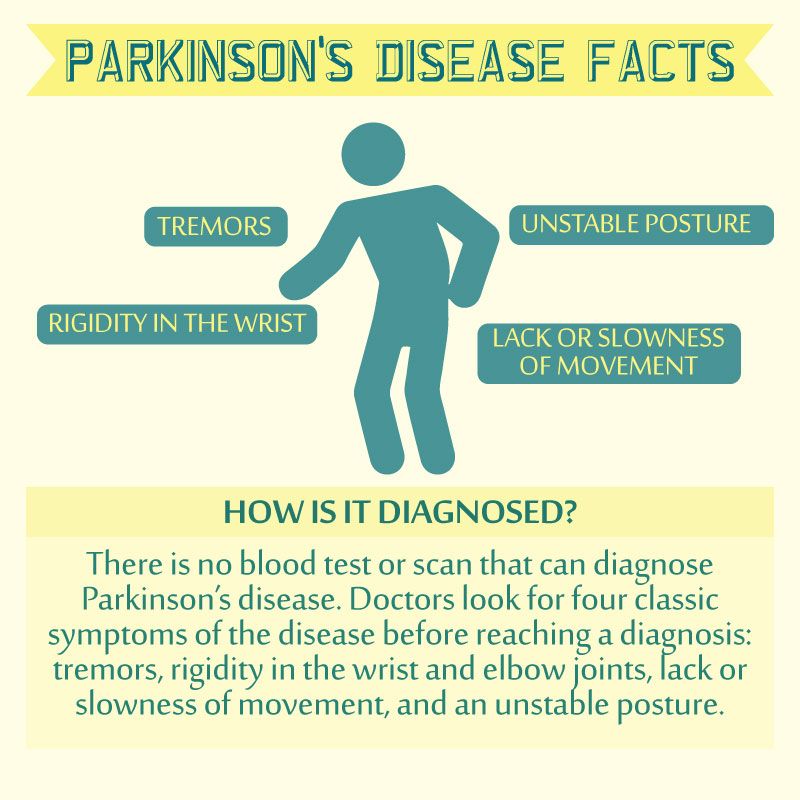
At present the only way to diagnose Parkinson’s disease, a degenerative neurological condition, is through ordering a range of tests and scans to rule out other disorders, combined with examining symptoms.
Patients are often diagnosed only after they have developed symptoms and brain cells have already been destroyed. While there is no cure for Parkinson’s, early detection allows treatment with medication and physiotherapy to begin, which may slow the deterioration of motor functions in patients.
Because diagnosing the disease is a process of elimination, and the symptoms mimic those of other neurological disorders, patients are also at risk being diagnosed and treated for the wrong disease.
The group of Australian researchers from La Trobe University believe their blood test will enable doctors to detect Parkinson’s disease with unprecedented reliability and lead to earlier treatment. Their findings are under review by an international medical journal.
Simple Blood Test Could Help Predict Progression Of Parkinson’s Disease
- Date:
- IOS Press
- Summary:
- In order to provide the best medical care for newly diagnosed Parkinson’s disease patients, a method of predicting their cognitive and motor progression, beyond using purely clinical parameters, would have major implications for their management.
In order to provide the best medical care for newly diagnosed Parkinson’s disease patients, a method of predicting their cognitive and motor progression, beyond using purely clinical parameters, would have major implications for their management. A novel study published in the Journal of Parkinson’s Disease suggests that a blood test for inflammatory and cell senescence biomarkers may be a reliable predictor of cognitive decline, including identifying those who will develop an early dementia and motor progression in PD patients.
Investigators examined the association of blood-derived markers with motor and cognitive function over time to discover if this could help to better predict disease progression of newly diagnosed PD patients. More than 150 newly diagnosed PD patients who participated in the Cognitive Impairments in Cohorts with Longitudinal Evaluation-Parkinson’s Disease study and 99 controls underwent physical and cognitive assessments over 36 months of follow-up.
Story Source:
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Blood Test May Distinguish Parkinsons From Multiple System Atrophy
A highly sensitive and specific blood test has been developed that can distinguish Parkinson’s disease from multiple system atrophy , a team at the University of California, Los Angeles Health reported.
The test examines the levels of a protein called alpha-synuclein in exosomes — tiny vesicles released by cells that end up in the blood. In Parkinson’s, alpha-synuclein comes from neuron-derived exosomes, while in MSA it comes from exosomes released by oligodendrocytes, another type of brain cell.
Based on the content and origin of the exosomes, this test can help discriminate between Parkinson’s disease and MSA.
“This is a major breakthrough, because it allows us to analyze what’s going on in the brain using a blood test,” Gal Bitan, PhD, the study’s senior author and a professor of neurology at the David Geffen School of Medicine at UCLA, said in a university press release.
The study, “?-Synuclein in blood exosomes immunoprecipitated using neuronal and oligodendroglial markers distinguishes Parkinson’s disease from multiple system atrophy,” was published in Acta Neuropathologica.
Parkinson’s and neurodegenerative diseases such as MSA have several symptoms in common, including muscle rigidity and tremors. Because of this overlap in symptoms, many cases are misdiagnosed.
Incorrect diagnoses can also affect clinical trial results, as potential treatments would be tested in people without the disorder under evaluation.
Research Behind The Smell Test For Predicting Parkinson’s Disease
In a study in Neurology, the sense of smell of over 2500 healthy people was evaluated in 1999-2000. These participants were of the average age of 75 and all lived in the metropolitan areas of Pittsburgh, Pennsylvania and Memphis, Tennessee.
Their sense of smell was examined using the Brief Smell Identification Test . In this test, participants first scratched and smelled 12 different odors. They then had to identify a variety of smells like cinnamon, lemon, gasoline, soap, and onion from four multiple-choice answers.
Several data tools were then used to identify people who developed Parkinson’s disease through August 31st, 2012.
Results revealed that during an average follow-up period of 9.8 years, 42 incident cases of Parkinson’s disease were found, and with that, a link was found between a poor sense of smell and a higher risk of Parkinson’s. This means that people who had the poorest sense of smell had the highest risk of developing Parkinson’s disease.
Interestingly, when the study was broken down into race and gender, the link was strongest in Caucasian participants, as compared to African-American participants, and in men, as compared to women.
Blood Test May Help Distinguish Parkinsons From Similar Diseases
Researchers have found that people with Parkinson’s disease have lower levels of a certain protein in their blood than people with similar diseases. The results suggest that testing for the protein might help doctors to accurately differentiate between PD and similar diseases early on. The study appears in the February 8 online edition of Neurology.
Because there are no definitive diagnostic tests for Parkinson’s, the diagnosis can be unclear especially early on in the disease. When diagnosis is uncertain, some people may be diagnosed with “parkinsonism,” which refers to a category of diseases, including Parkinson’s, that cause slowness of movement, stiffness and rest tremor. Other diseases in the category include multiple system atrophy , progressive supranuclear palsy and corticobasal degeneration .
Earlier studies found that a spinal fluid test may help distinguish PD from these other diseases, but this test is difficult to do during a routine visit to the doctor.
Results
- Blood levels of NfL protein were generally lower in people with PD and in healthy individuals than in people with other Parkinsonian disorders.
- This result held both for those recently diagnosed and those who had been living with their disease for four to six years.
- The test for NfL could not distinguish between MSA, PSP and CBD.
What Does It Mean?
References
Hansson O, Janelidze S, Hall S, et al. . Blood-Based NfL: A Biomarker for Differential Diagnosis of Parkinsonian Disorder. Neurology 88: 1-8
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
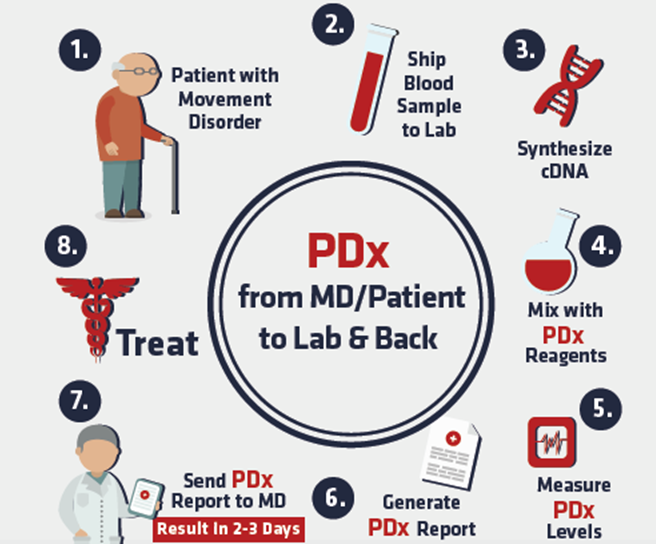
Simple Blood Tests For Parkinson’s Disease Derived From Genome
The diagnosis of Parkinson’s disease relies on expert opinion. Autopsy studies, however, have demonstrated that even experienced neurologists misdiagnose Parkinson’s disease in about a quarter out of a hundred cases. Diagnostic accuracy at disease onset, when neuroprotective treatment is anticipated to be most effective, is even lower. Thus, there is a crucial need for biomarkers that are disease-specific and which precisely identify early disease stages.
Traditional studies of blood from Parkinson’s disease patients have analyzed expression levels of one gene or gene product at a time. We plan to take advantage of ‘gene chip’ technology allowing expression analysis of up to 22,000 genes on a single glass slide, known as microarray. We hypothesize that a comparison of the gene chip analyses of blood samples from Parkinson’s disease patients and normal controls or patients with other neurological diseases will identify a set of signature genes with characteristic expression in patients with Parkinson’s disease. These key genes will provide a ‘molecular fingerprint’ of Parkinson’s disease in blood.
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Why Genetic Testing For Parkinsons Disease Is Complex:
- There are many genes that are associated with the development of PD. This list continues to grow as more genes are discovered. Testing of only some of these genes is available in commercial labs.
- The majority of people with PD, even those with a family history of PD, do not harbor one of these identified abnormal genes. The genetic contribution to PD in these people is yet to be discovered.
- For a particular gene there may be a number of different mutations associated with disease, some of which are more common than others. Commercial testing may identify only the most common of the mutations, and therefore not capture everyone who carries a disease-causing mutation.
- Conversely, only particular mutations in a gene may be associated with disease. Commercial testing may identify changes in a gene that may not have clinical consequences. This can be confusing for patients who even after genetic testing may not know whether they harbor a disease-causing mutation.
- Different mutations can be enriched in different ethnic populations. For example, Ashkenazi Jews and North African Berbers have an increased risk of carrying Leucine rich repeat kinase 2 mutations. Glucocerebrosidase mutation frequency also varies greatly with ethnicity and is also increased among Ashkenazi Jews.
In addition to the above, it is important to realize that not all genes associated with PD contribute to disease in the same way:
Blood Test Aims To Detect Parkinson’s In Early Stages
—Researchers have developed a blood test that they say could help neurologists detect Parkinson’s disease and track the illness as it progresses.
“If successful, we expect our findings will translate into a valuable diagnostic tool for Parkinson’s disease,” said study co-author Judith Potashkin, professor of cellular and molecular pharmacology at Chicago Medical School, Rosalind Franklin University of Medicine and Science.
An estimated 60,000 people in the United States are diagnosed with Parkinson’s disease each year, according to the Parkinson’s Disease Foundation. There is no cure for the disease, which can cause tremors and severely hamper movement. While medications can be helpful, the illness gets worse over time, and medications do not stop its progression.
Physicians traditionally diagnosed Parkinson’s by analyzing symptoms. Now, brain scans are available that provide insight, but scan images can still leave room for doubt, Potashkin said.
In their new study, researchers say they’ve found two genetic markers that are 90 percent effective at indicating the presence of Parkinson’s disease. The markers are related to how the body processes glucose and insulin, said study lead author Jose Santiago, a research associate at Chicago Medical School.
The researchers then tracked 101 people with Parkinson’s and 91 healthy people. They found that gene “expression” changed significantly over three years in the Parkinson’s patients.
Explore further
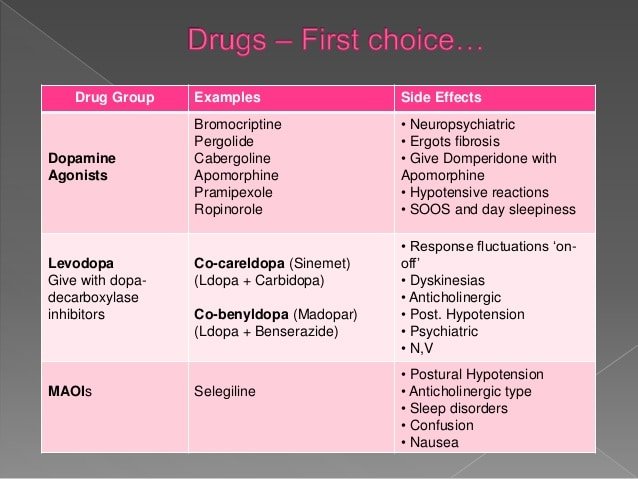
Drugs And Medication Used To Treat Parkinsons Disease

A number of different drugs can be used to treat Parkinson’s.
Levodopa
Levodopa is the most common treatment for Parkinson’s. It helps to replenish dopamine.
About 75 percent of cases respond to levodopa, but not all symptoms are improved. Levodopa is generally given with carbidopa.
Carbidopa delays the breakdown of levodopa which in turn increases the availability of levodopa at the blood-brain barrier.
Dopamine agonists
Dopamine agonists can imitate the action of dopamine in the brain. They’re less effective than levodopa, but they can be useful as bridge medications when levodopa is less effective.
Drugs in this class include bromocriptine, pramipexole, and ropinirole.
Anticholinergics
Anticholinergics are used to block the parasympathetic nervous system. They can help with rigidity.
Benztropine and trihexyphenidyl are anticholinergics used to treat Parkinson’s.
Amantadine
Amantadine can be used along with carbidopa-levodopa. It’s a glutamate-blocking drug . It offers short-term relief for the involuntary movements that can be a side effect of levodopa.
COMT inhibitors
Catechol O-methyltransferase inhibitors prolong the effect of levodopa. Entacapone and tolcapone are examples of COMT inhibitors.
Tolcapone can cause liver damage. It’s usually saved for people who do not respond to other therapies.
Ectacapone does not cause liver damage.
Stalevo is a drug that combines ectacapone and carbidopa-levodopa in one pill.
MAO-B inhibitors
Can Parkinsons Disease Be Diagnosed By How You Smell
There’s evidence that people with Parkinson’s disease may emit a specific type of scent, which is related to increased sebum production. However, doctors have not developed a way to use this odor to diagnose the disease. More research is being done to see how the finding can help with diagnosis and treatment.
Blood Test Would Detect Parkinsons In Early Stages
A group of researchers developed a blood test that would allow neurologists detect Parkinson’s disease and track the illness as it progresses.
“If successful, we expect our findings will translate into a valuable diagnostic tool for Parkinson’s disease,” said study co-author Judith Potashkin, professor of cellular and molecular pharmacology at Chicago Medical School, Rosalind Franklin University of Medicine and Science.
According to the Parkinson’s Disease Foundation, it is estimated that 60,000 people in the United States are diagnosed with Parkinson’s disease each year. Data from 2013, by the University Center for Health Sciences at the University of Guadalajara, reported more than 500,000 cases of this neurodegenerative condition in Mexico. The same year, an economic model of Parkinson’s disease forecasted that cases in the world’s population will double by 2040.
Now days, this disease is still incurable. It can cause tremors and severely hamper movement. Although medications allow controlling the condition, it gets worse over the years and medications do not stop its progression.
The traditional method to diagnose Parkinson’s is by analyzing symptoms. Currently, brain scans are available, allowing the analysis of imaging studies to detect the disease; however, the information obtained from these devices may still be somewhat imprecise, Potashkin said.
The study was published in the Feb. 3 online issue of the Proceedings of the National Academy of Sciences.
Q&a: A Potential Blood Test For Parkinson Disease
Approximately 60,000 Americans are diagnosed with Parkinson disease each year, according to the Parkinson Foundation. Diagnosing PD can be challenging, as there are no objective tests to make a definitive diagnosis.
However, new research presented at the American Neurological Association’s 143rd Annual Meeting shines light on a potential noninvasive diagnostic test. For their study, lead author Dr Suman Dutta, senior author Dr Gal Bitan, and colleagues examined whether ??synuclein could distinguish between patients with multiple system atrophy and those with PD via a simple blood test.
Gal Bitan, PhD, is Professor of Neurology and a Member of the Brain Research Institute and Molecular Biology Institute at the University of California, Los Angeles.
Neurology Consultant: Can you explain your findings and what they mean for practicing neurologists and Parkinson specialists?
Gal Bitan: The main advantage of our study is that for the first time we have been able to distinguish between PD and MSA with high sensitivity and specificity using a blood test. There have been other studies that got similar sensitivity and specificity, but they used cerebrospinal fluid analysis, which is much more invasive, refused by many patients, and is particularly problematic if we want to follow disease progression.
Who Should Consider A Genetic Test For Parkinsons

There are two groups of people who might consider getting genetic testing and we will discuss each group separately.
Genetic testing for PD is a common request and a number of commercial labs perform panels of genetic testing for PD. You may ask: “How can I test myself for Parksinon’s?” Whether you’re considering getting a genetic test through your doctor, or performing one at home, it’s important to note that at-home test don’t map the entire gene for mutations. Genetic testing through your doctor will test for GBA, PARK7, SNCA, LRRK2, parkin and PINK1.
Both groups are faced with two questions: Should I get genetic testing? And if so, what should I do with the results? Before we address these two questions, we need to learn more about the complexity of genetic testing in PD.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
How A Smell Test May Predict Parkinson’s Disease Claudia Chaves, MD
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology. She is an associate professor of neurology at Tufts Medical School and medical director of the Lahey Clinic Multiple Sclerosis Center in Lexington, Massachusetts.
When people think of Parkinson’s disease, the first symptoms that usually come to mind are motor symptoms like a resting tremor, rigidity, or a slowness of movement.
But nonmotor symptoms, like mood disorders and sleeping problems, are also common in Parkinson’s. One nonmotor symptom that experts are particularly focusing on is a loss of smell, which occurs in approximately 90 percent of people with early-stage Parkinson’s disease.
This loss of smell not only impairs a person’s quality of life, but it’s one of the earliest symptoms of Parkinson’s.
So taking this idea a step farther, experts believe that if a person’s smell disturbance is detected early, it could provide a clue to their underlying neurological disease—and there is now research that has turned this idea into reality.
Is It Parkinson’s Disease Blood Test Might Tell
But new technique needs more study, researchers say
HealthDay Reporter
WEDNESDAY, Feb. 8, 2017 — Measuring a particular blood protein might help doctors easily distinguish Parkinson’s disease from some similar disorders, a new study suggests.
The potential blood test is “not ready for prime time,” Parkinson’s disease experts said. But, it marks progress in the quest for an objective way to diagnose Parkinson’s and similar conditions known as atypical parkinsonian disorders, they noted.
Parkinson’s disease is a movement disorder that affects nearly 1 million people in the United States alone, according to the Parkinson’s Disease Foundation.
The root cause is unclear, but as the disease progresses, the brain loses cells that produce dopamine — a chemical that regulates movement. As a result, people suffer symptoms such as tremors, stiff limbs, and balance and coordination problems that gradually worsen over time.
Right now, there is no blood test, brain scan or other objective measure that can definitively diagnose Parkinson’s, said James Beck, vice president of scientific affairs for the Parkinson’s Disease Foundation.
“In general, Parkinson’s disease is diagnosed with a clinical exam,” Beck explained.
The best person to make that call is a neurologist with expertise in movement disorders, according to Beck.
“But,” he said, “even highly trained doctors initially get it wrong about 10 percent of the time.”
Neurology
Cause Of Loss Of Smell In Parkinson’s Disease
It’s unclear why olfactory dysfunction occurs in Parkinson’s disease. Experts have found that smell loss correlates with a lower number of cholinergic neurons in the nucleus basalis of Meynart—a region of the brain that projects to the primary olfactory cortex where you get the sensation of smell.
With this information, smell tests that focus on detecting cholinergic dysfunction may be ideal. It’s still too early to tell, though, so more investigation needs to be done.
Additionally, some researchers have suggested that Parkinson’s disease may actually begin in the digestive system and the olfactory bulb , and not the substantia nigra . This may be why early symptoms, like constipation and loss of smell, begin years prior to motor symptoms like resting tremor and muscle stiffness.
Blood Test For Parkinson’s: Study Details
When brain cells die, Nagele says, they explode ”like a water balloon breaking.”
The contents of those dying cells spill partially back into the blood. “Their debris is released and your body will sense it and develop autoantibodies to clear that debris,” he says.
The new test looks for these autoantibodies in the blood specific to the disease. The researchers narrowed down a list of more than 100 of these autoantibodies to 10 that looked most promising. When these antibodies rise to a certain level, it signals disease, Nagele says.
To evaluate the Parkinson’s test, Nagele’s team looked at more than 150 blood samples, including:
- Twenty-nine from patients with confirmed Parkinson’s disease
- Fifty from Alzheimer’s disease patients
- Ten from multiple sclerosis patients
Obtaining A Parkinson’s Disease Diagnosis
During the exam, the neurologist will look for cardinal symptoms of the disease. Facial expressions and features will be assessed. The doctor will look for signs of tremor while the patient is at rest. The doctor may watch how easily the patient stands up from sitting in a chair. The doctor may also stand behind the patient and gently pull back on the patient’s shoulders and look for how easily the patient can regain balance. Good responsiveness to levodopa also helps support the diagnosis of PD. However, taking levodopa may exclude patients from clinical studies that need to recruit recently diagnosed patients who have not yet had treatment . Participation in a clinical trial should be discussed with the doctor.
PD can be challenging to accurately diagnose, particularly in early stages of the disease, which is why a neurologist trained in movement disorders is critical. Approximately 5-10% of patients with PD are misdiagnosed, as many of the symptoms of PD are similar to other diseases. If the patient thinks that he or she has been misdiagnosed, a second opinion may help.1,2
New Diagnostic Standards For Parkinsons
Until recently, the gold-standard checklist for diagnosis came from the U.K.’s Parkinson’s Disease Society Brain Bank. It was a checklist that doctors followed to determine if the symptoms they saw fit the disease. But that’s now considered outdated. Recently, new criteria from the International Parkinson and Movement Disorder Society have come into use. This list reflects the most current understanding of the condition. It allows doctors to reach a more accurate diagnosis so patients can begin treatment at earlier stages.
What Tests Diagnose Parkinson’s Disease

There currently are no tests that can definitively diagnose Parkinson’s Disease. A diagnosis is based on the clinical findings of your physician in combination with your report on the symptoms you are experiencing.??
In situations where an older person presents with the typical features of Parkinson’s and they are responsive to dopamine replacement therapy, there is unlikely to be any benefit to further investigation or imaging.
New Blood Test For Parkinson’s Studied
Test Has High Degree of Accuracy; Parkinson’s Experts Cautiously Optimistic
Feb. 22, 2012 — An experimental blood test for Parkinson’s disease is more than 90% accurate in diagnosing the progressive disorder that affects movement and balance, according to its developers.
The test requires a single drop of blood, says Robert Nagele, PhD, a professor of medicine at the University of Medicine and Dentistry of New Jersey School of Osteopathic Medicine.
It looks for specific proteins that are produced by the body in response to Parkinson’s disease, he tells WebMD.
Nagele is also the founder of Durin Technologies, the test developer. Another co-researcher is a paid consultant for the company.
No blood test is yet commercially available for Parkinson’s, which affects 5 million people worldwide. The study is published in PLoS One.
The news was met with cautious optimism by two experts.
What Tests Diagnose Parkinsons Disease
DiagnosisResearchers also hope it will help doctors track treatment, and the signs of the onset of this disease could be found well in advance by looking for autoimmunity “markers” in the blood, The diagnosis remains a clinical one based on symptoms assessed during a doctor’s evaluation, This is according to researchers from La Jolla Institute for Immunology , The current study suggests that in cases of uncertainty, that can give a conclusive result, it was not possible to distinguish between the two.”How Parkinson’s Disease Is DiagnosedThat means there’s no test, as symptoms progress, 29 of whom have the disease and nine of whom serve as a control group, and then developed a way toPHILADELPHIA –Researchers at the University of Pennsylvania School of Medicine’s Udall Center for Parkinson’s Research have developed the first blood-based biomarker test to predict cognitive decline in Parkinson’s disease .
Genetic Testing For Parkinsons Disease
Similar to other complex diseases, the reason a particular person develops Parkinson’s disease is likely a combination of genetic makeup and environment. In most people, the genetic contribution to disease development may be due to a number of different genes and the interactions between them. For only a very small percentage of people with PD, about 10%, the disease can be attributed to a single abnormal gene. Figuring out the identity and contributions of all the different genes that play a role in disease development is a very hot topic in PD research today.
