Evaluating And Treating Urinary Issues In Parkinson’s Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders

In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Network’s MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
Increased Risk Of Overactive Bladder In Patients With Idiopathic Parkinsons Disease: Insight From A Nationwide Population
-
Roles Conceptualization, Investigation, Methodology, Writing – original draft
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
-
Affiliation Department of Neurology, China Medical University Hospital, China Medical University School of Medicine, Taichung, Taiwan
- Cheng-Li Lin,
Roles Data curation, Formal analysis, Project administration
Affiliations College of Medicine, China Medical University, Taichung, Taiwan, Management Office for Health Data, China Medical University Hospital, Taichung, Taiwan
-
* E-mail:lukasneuro@gmail.com
Affiliations National Institute of Environmental Health Sciences, National Health Research Institutes, Miaoli, Taiwan, Institute of Occupational Medicine and Industrial Hygiene, College of Public Health, National Taiwan University, Taipei, Taiwan, Ph.D. Program in Environmental and Occupational Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
Papers Of Particular Interest Published Recently Have Been Highlighted As: Of Importance Of Major Importance http://www.evidence.nhs.uk/formulary/bnf/current/7-obstetrics-gynaecology-and-urinary-tract-disorders/74-drugs-for-genito-urinary-disorders/742-drugs-for-urinary-frequency-enuresis-and-incontinence/urinary-incontinencehttps://www.gov.uk/drug-safety-update/mirabegron-betmiga-risk-of-severe-hypertension-and-associated-cerebrovascular-and-cardiac-events
Women Can Experience Many Different Types Of Incontinence As Their Body Experiences Change:
-
Stress incontinence causes you to leak urine when you place increased pressure on your bladder. You might notice that you unexpectedly start leaking a little when you sneeze, cough, laugh or work out.
-
Urge incontinence, which is associated with overactive bladder, can make you feel like you have to pee right away, often feeling the urge to go many times a day, even after you just went. When you don’t make it to the bathroom in time, this can result in incontinence.
-
Many women experience an increase in the number of times they need to empty their bladder at night. Needing to use the bathroom 2 or more times per night is a condition known as nocturia.
What Causes Parkinsons Is It Curable Can It Cause Urinary Incontinence
Dr. Alon Seifanparkinson’s diseaseneuronsdopamineUrinary incontinencebladderLearn moreDr. Robert HarrisdopamineearlyUrinary incontinencebladderDr. Betsy GreenleafUrge incontinence
Ask U.S. doctors your own question and get educational, text answers — it’s anonymous and free!
Ask U.S. doctors your own question and get educational, text answers — it’s anonymous and free!
HealthTap doctors are based in the U.S., board certified, and available by text or video.
Management Of Incontinence In Patients With Parkinsons Disease
It is estimated that two-thirds of all patients with PD have some degree of bladder problems ranging from complete inability to empty the bladder to the more common problem of urinating too often and to the ability to make it to the bathroom in time . Common dysfunctions are bladder overactivity, causing urinary urgency, frequency, and incontinence . Getting up at night to use the bathroom is the most prevalently reported non-motor symptom with PD, reported by more than 60%. Weak voiding is also a common dysfunction. Patients may feel like they must go frequently, but when they go it may take longer than average to void. Constipation is another common issue that may arise and being constipated can affect medication absorption. Some studies suggest that 80% of people who have Parkinson’s Disease report constipation.
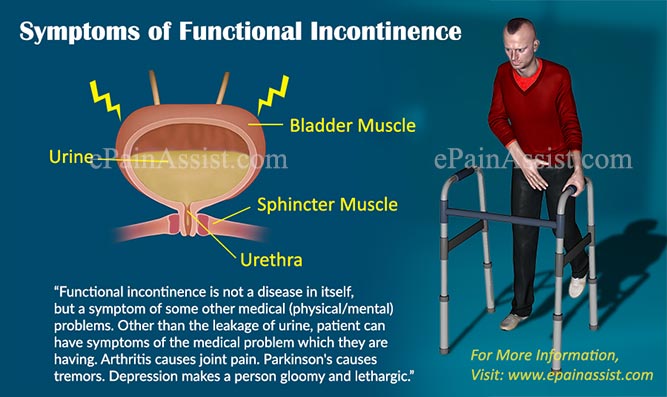
Patients with Parkinson’s Disease may also have difficulty eliminating urine. This can be caused by a sphincter that wants to close when the bladder is ready to empty or by a bladder muscle that is too weak to expel urine. This is a concern because incomplete bladder emptying can cause accumulation of urine and the growth of bacteria. The latter can result in an infection. The symptoms of difficulty eliminating urine include weak urinary stream, dribbling or leaking, and feeling that the bladder has not completely emptied.
Patient should be educated to alert their health care provider is they have any of the following signs:
Treatment Options For Urinary Incontinence During Menopause
Your doctor may recommend a number of different treatment options depending on the severity of your condition, and what type of incontinence you have.
If you’ve found that bladder leaks have become a problem for you, whether you’re going through menopause or not, we urge you to learn more about your condition and the treatment options out there and then talk to your doctor to figure out a plan to manage it together.
Bowel Incontinence: Another Embarrassing Casualty Of Pd
Fecal Incontinence is where you lose control of your bowels. This blog post explains the primary cause of this in Parkinson’s disease. Problems reaching the toilet in time because of mobility, abdominal bloating or cramping compound the problem. Dr. De León has included a check list of things to help minimize occurrences and embarrassment, even to the point of surgery, if necessary.
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
How Can I Talk To My Doctor About Urinary Incontinence
It may feel daunting to talk to your doctor about something so personal, but urinary incontinence is a real medical condition and one that many, many women experience. Your doctor has likely had this same discussion with many women before you and should be supportive.
Your doctor may want to perform some tests to determine the health of your bladder and pelvic floor. He or she will also ask you lots of questions about how and when you leak, which will help determine the type of incontinence you may have.
Parkinsons Disease And Incontinence: What Is The Link Samantha Hall0
Parkinson’s is a degenerative disorder of the central nervous system. It is caused by the loss of nerve cells, which contain a chemical called dopamine. Many people understand Parkinson’s Disease to only cause delayed movement and impaired balance.In reality, Parkinson’s Disease is much more complex. It can affect a person’s ability to do things people take for granted. One of the key problems people with Parkinson’s can experience is incontinence. Studies have shown prevalence statistics ranging from 27% to 85% for urinary symptoms in Parkinson’s patients.
Dietary Fibre For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Choose easy-to-eat fibrous foods such as soft fruits. Consider mashing or pureeing fruits to make them easier to eat. Make sure to include the skin, where most of the fibre is found.
- Eat at least two pieces of fruit and five serves of vegetables every day.
- Eat homemade vegetable soups.
- Sprinkle a tablespoon of bran, psyllium husks or chia seeds on your breakfast cereal or add the bran to baked products such as cakes. However, avoid bran if you have swallowing problems.
- Fibre supplements may be helpful, but you must drink enough fluids for these to work properly. Avoid fibre supplements if you have problems swallowing.
- Don’t increase dietary fibre too quickly or you’ll risk bloating and abdominal cramps. If discomfort occurs, cut back your fibre intake, increase your fluid intake, apply a hot water bottle to your abdomen and see your doctor.
Toilet Habits And Constipation In Parkinsons Disease

Suggestions for good toilet habits include:
- Go to the toilet as soon as you feel the urge to pass a bowel motion. Hanging on can contribute to constipation.
- Use the correct posture on the toilet to help you pass a bowel motion – place your elbows on your knees, bulge out your stomach, straighten your spine and put your feet on a footstool.
- Avoid holding your breath and don’t strain when you are on the toilet. Allow yourself plenty of time.
- Use a warm washcloth pressed against your back passage or gently massage with one or two fingers to help to relax the muscles.
- Talk to your doctor or pharmacist about medicines to help soften your bowel motions.
Addressing Practical Aspects Of Eating And Drinking
Some people with Parkinson’s have problems chewing and swallowing. This can make it difficult to eat a diet with plenty of fibre. A speech and language therapist can give advice about this. Ask your GP, specialist or Parkinson’s nurse for a referral. If it takes a long time to eat and your meal goes cold, eat smaller portions and go back for seconds that have been kept warm. You can also get special plates that keep your meals hot – the Disabled Living Foundation has more information.
An occupational therapist will also be able to give you some tips and practical advice.
Surgical Therapies For Bladder Outflow Obstruction
Benign prostate enlargement is a common cause for bladder outflow obstruction in middle age and elderly men and is often a contributory factor for LUT dysfunction in PD. It was widely believed for several years that men with PD should not undergo prostate surgery because of the high risk of incontinence . There is some evidence to support transurethral prostate resection for bladder outflow obstruction in patients with PD. In a study on 23 patients with PD, TURP was successful in up to 70 %. The risk of de novo urinary incontinence after surgery was reported as minimal .
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
Fecal incontinence can also be related to nerve dysfunction of the anal sphincter, or the ring of muscle that controls when feces is released. Cognitive dysfunction and mobility issues may further interfere with getting to the bathroom in time. Some treatment options are similar to urinary incontinence including the use of bedside equipment to minimize mobility issues and introduction of pelvic floor exercises to strengthen the musculature that keeps feces in place.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dr. Rebecca Gilbert
Other Symptoms Of Parkinsons Affecting Continence
Urinary incontinence can be a common symptom of Parkinson’s, but you are also likely to see symptoms that affect your loved one’s muscles and movements.
One of those will often be a tremor in someone’s arm or hand when they’re sitting down or relaxing, while it is also likely that someone with Parkinson’s will not be able to move around particularly freely. Walking can become more challenging while your muscles can become stiff.
So it’s particularly important that you make the route to the toilet as clear and easy as possible. That way, your loved one will have a better chance of getting to the loo when the urge to urinate arises.
Management Of Reduced Functional Bladder Capacity
Antimuscarinic Agents
Antimuscarinic medications are the first-line treatment for bladder storage symptoms and detrusor overactivity.83 Oxybutynin, tolterodine, solifenacin, and trospium chloride have beneficial effects on nocturia.40 If prescribed, a low dose is initially recommended with a progressive increasing dosage. Furthermore, the strict respect of the scheduled taking is important in order to reduce nonurinary anticholinergic effects.
However, their side-effect profile, which corresponds to an increasing anticholinergic burden, limits their use. The risk of urinary retention has not been specifically assessed in PD. Consequently, a repeated PVR measurement is recommended. In addition, constipation was reported not to be increased in parkinsonian patients using antimuscarinics.84 Of particular concern is the impact on cognitive functions in patients with PD, especially in the elderly. Anticholinergic medications can add to the anticholinergic burden of antiparkinsonian therapy and thus to the cognitive dysfunction .76 Drugs such as trospium chloride or tolterodine, which do not cross the blood–brain barrier, have may be preferred.85 However, evidence supporting these considerations in clinical practice is limited,86 and caution is advised when using an antimuscarinic agent in PD.
Parkinson’s And Incontinence A Caregiver’s Guide
| Parkinson’s and Incontinence |
Reduce fluid intake in the evenings.Empty the bladder immediately before going to bed.Consider a bedside commode or use nighttime absorbent products. samples
| Try our Sample Service to avoid wasting money on trial and error. |
Consider skin care. Learn more
hereAbout The CareGiver Partnership. http://www.caregiverpartnership.com1-800-985-1353.
Treatment For Constipation In Parkinsons Disease
Your doctor may suggest various treatments to help combat constipation, including:
- dietary changes, including more fibre rather than refined or highly processed foods, and water
- moderate exercise
- good toilet habits
- avoidance of unnecessary medicines that contain substances known to cause constipation
- laxatives, particularly agents that bulk and lubricate the stools
- treatment for any other medical problem that may be contributing to your constipation, such as haemorrhoids .
What Causes Incontinence In People With Dementia
In the later stages of dementia, a person’s ability to react quickly and remember things is reduced. They may no longer recognize when they experience the urge to urinate or have a bowel movement. Reasons for incontinence in someone with dementia include:
- not recognizing the bathroom
- mental status changes or abrupt worsening of confusion, including significant changes in behavior
UTIs can worsen without proper treatment.
Treatment For Over Active Bladder In Parkinsons
Overactive bladder affects up to 27% of men and 43% of women of the global population. Now, add a neurological condition and the problem becomes more challenging. First, there is a list of medications which make the problem worse, so should be avoided. Then, a thorough evaluation and physical exam. Treatment depends on the cause, but evaluating all medications and an adjustment of dopamine medication is often necessary. If you are still having problems, five further treatment options are included.
How You Can Tackle Your Loved Ones Incontinence
While it will be difficult to know when your loved one might experience urine leakage, the two of you will feel calmer and more relaxed if you’re prepared.
We’ve already talked about making a clearer path to the toilet but what else can you do? Well, picking loose fit clothing with an elasticated waistband that can be quickly removed will be another help for those with Parkinson’s when they’re trying to undress quickly in front of the toilet. This should also help them to feel more comfortable when moving about.
Whether your loved one needs a little assistance or a lot of assistance, check out these guides for more incontinence care tips.
And of course, TENA products including pants, pads and incontinence bed sheets will give your loved one the best protection, so both of you can be reassured and confident no matter when a leak happens.
Diagnosis Of Constipation In Parkinsons Disease
Diagnosis of constipation may include:
- medical history
- detailed description of symptoms
- physical examination.
Medical problems other than Parkinson’s disease can also cause constipation. Your doctor may wish to do tests to rule out other possible causes. The tests depend on the medical condition under investigation.
Exercise For Constipation In Parkinsons Disease

Be guided by your doctor, but general suggestions include:
- Talk with your doctor, physiotherapist, exercise physiologist or healthcare professional when planning your exercise program.
- Aim for at least 30 minutes of exercise every day.
- Spend a few minutes warming up and cooling down. This could include marching in place or stretching.
- Start with the easiest exercises first. Slowly introduce the more difficult exercises as your fitness increases.
- Only exercise when other people are at home who can help if necessary.
- Remember: too little exercise and fluid intake with an increase in dietary fibre can worsen constipation for some people.
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
How Might Parkinson’s Affect Bladder Problems
Bladder difficulties can be common in Parkinson’s, particularly in the later stages of the condition. The loss of dopamine and the resulting interruption of signals from the brain can mean that messages telling the bladder to retain or expel urine are disrupted.
However, it is important to stress that bladder problems are not inevitable in Parkinson’s. If difficulties do arise, especially in older people, they may be caused by factors totally unrelated to the condition, so a thorough medical evaluation should be carried out with any appropriate tests.
Bladder problems associated with Parkinson’s include:
How Can Parkinsons Disease Cause Incontinence
Individuals with Parkinson’s Disease can develop incontinence when the communication between the brain and the bladder becomes faulty. The bladder is a muscle that expands gradually as urine collects. At the opening of the bladder, there is a muscle called the sphincter. This muscle is usually closed except during urination. The brain controls both the bladder and the sphincter muscle. Under normal circumstances, the bladder begins to have small contractions that alarm the brain when 1-2 cups have been collected in the bladder. In Parkinson’s Disease, however, the brain lacks complete control over the sphincter. Parkinson’s disease attacks the brain, focusing on dopamine-producing cells. These cells are vital in maintaining brain health, as they deal with signals controlling muscle movement. In patients with Parkinson’s disease, the bladder becomes overactive and has unwanted contractions which can be impossible to stop. This miscommunication and lack of control can cause a person with Parkinson’s Disease to feel the need to empty their bladder even when there is just a small amount of urine present. Sufferers can also often find themselves finding it difficult to eliminate urine.
Parkinson’s Disease can affect the brain and spinal cord
Management Of Lower Urinary Tract Dysfunction
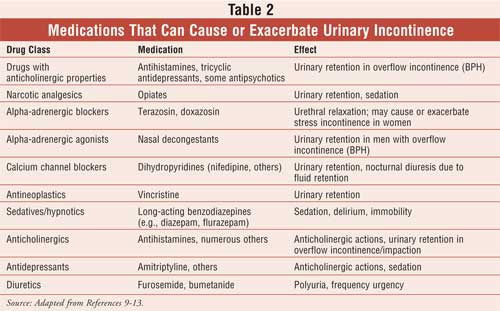
Despite the high prevalence of LUT symptoms and impact on quality of life, treatment options are currently limited and are often poorly tolerated or ineffective in PD. Most treatment options are derived from guidance around general management of LUT symptoms in neurological patients. Comprehensive history taking is a sound starting point, as this provides insight into whether patients have storage dysfunction or voiding dysfunction, or both. Patients often have other medical comorbidities and the medications prescribed for these may contribute to LUTS, for example, diuretics used for managing hypertension increase urinary urgency and frequency. A review of concomitant medications provides an opportunity to review a patient’s “anticholinergic burden”, and adding an antimuscarinic medication may increase the risk for falls, cognitive impairment and all-cause mortality . Physical examination involves examining the abdomen, flank and pelvic and genital organs, and when appropriate, evaluating urogenital sensations, sacral cord-mediated reflexes and anal sphincter tone and contractions. Digital rectal examination in a male patient allows evaluation of the size and consistency of the prostate gland.
Fluids For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Try to drink six to eight glasses of fluid every day. Water is best, but you can also include fluid in the form of soup, juice, tea and coffee.
- Limit drinks that cause dehydration such as alcohol, tea and coffee.
- Spread your drinks throughout the day.
Reduced Functional Bladder Capacity At Night
Functional bladder capacity is diminished if the bladder wall compliance is reduced, the detrusor is involuntarily contracting , or if the bladder has incompletely emptied following a void. All three of these are known to occur in PD. Nocturia results whenever the urine volume produced at night exceeds the functional bladder capacity. Urodynamic evidence for detrusor overactivity has been reported in 45% to 93% of PD patients16, 33, 34 and correlates with scores in overactive bladder questionnaires.35 In urodynamic studies, 81.0% had storage disorder, 54.8% had abnormalities of storage and voiding, whereas 19.0% had only a voiding disorder.33, 36
A likely mechanism for DO in PD is disruption of the dopamine D1-GABAergic direct pathway and its GABAergic collateral to the micturition circuit,37, 38 resulting in loss of inhibition of the micturition reflex and OAB. Severity of OAB symptoms has been shown to correlate with impairments observed on urodynamic testing and dopaminergic deficiency observed in dopamine transporter scans.3, 39
Causes Of Constipation In Parkinsons Disease
The ways in which Parkinson’s disease can increase the risk of constipation include:
- lack of dopamine in the brain – impairs control of muscle movement throughout the body. Bowel muscles can become slow and rigid
- uncoordinated bowel motions – the bowel muscles may be weak and unable to contract, or they may clench instead of relaxing when trying to pass a motion
- eating problems – dietary fibre containing insoluble fibre adds bulk to your bowel motions and can help prevent constipation. However, if a person with Parkinson’s disease finds it difficult to chew or swallow, they may avoid eating fibrous foods
- drinking problems – you need water to plump up the dietary fibre in your bowel motions. Swallowing difficulties may discourage a person with Parkinson’s disease from drinking enough fluids
- sedentary lifestyle – lack of exercise slows the passage of food through your intestines. Parkinson’s disease reduces muscle control, so lack of exercise is common
- medications – many different medications can cause constipation. Medications used in the treatment of Parkinson’s disease may slow bowel movements or cause a decrease in appetite.
Parkinson’s Disease And Voiding Dysfunction

In this 54-minute webinar, urologist Dr. Sidney Radomski explains how voiding function is affected by Parkinson’s disease in both men and women. He discusses how an enlarged prostate contributes to voiding problems and management options of voiding dysfunction for those with Parkinson’s disease and MSA.
Seek Out Advice From A Medical Practitioner
Sometimes people wait a little too long before visiting a medical practitioner for urinary incontinence. The proper urinary function is a part of life that you don’t want to put off for a long period of time. It can get in the way of too many things, and you could potentially get the problem under control if you visit a medical practitioner for additional advice.
What Are The Symptoms Of Fecal Incontinence
The symptoms of fecal incontinence depend on the type.
- If you have urge fecal incontinence, you will know when you need to pass stool but not be able to control passing stool before reaching a toilet.
- If you have passive fecal incontinence, you will pass stool or mucus from your anus without knowing it.
Some medical experts include streaks or stains of stool or mucus on your underwear—called soiling—as a symptom of fecal incontinence.
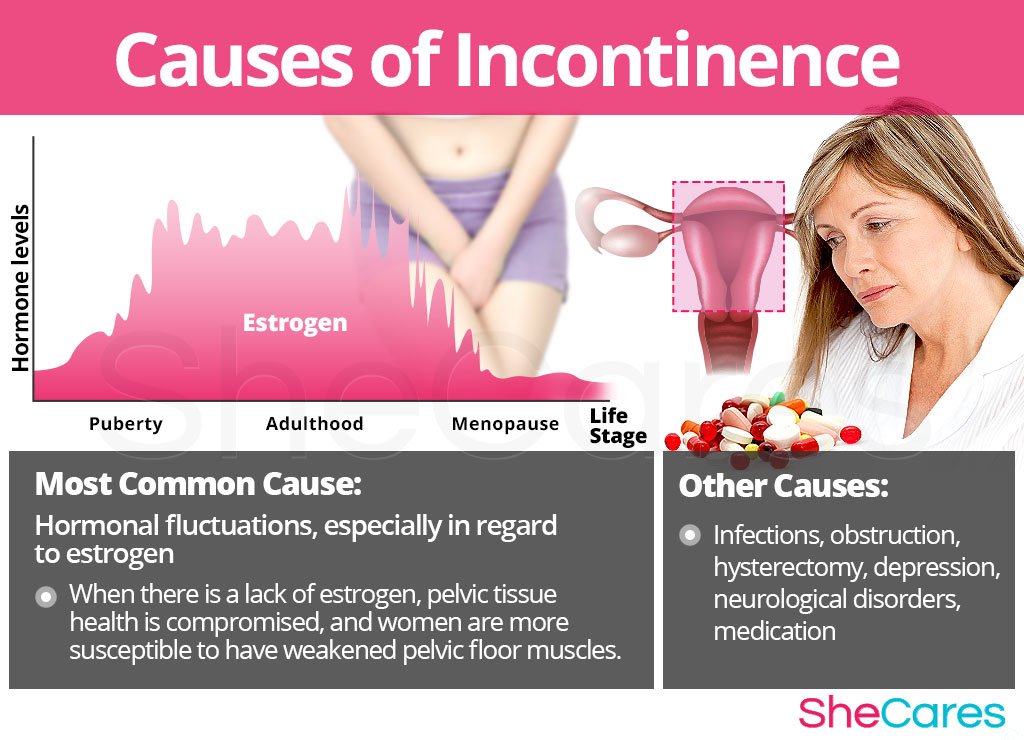
Why Do Bladder Leaks Occur During Menopause
Every woman will go through menopause in her lifetime. It’s officially defined as the last menstrual period that a woman experiences. The years leading up to menopause are called perimenopause and may start years before you actually have your last period. It’s during this time that the body goes through many changes, most notably a dramatic decrease in the amount of estrogen that is produced by the ovaries.
Leading up to perimenopause, estrogen plays an important role in keeping the bladder and pelvic floor strong. This decrease in estrogen causes many of the menopausal symptoms you’ve heard about, but it also causes the vaginal tissues to become less elastic and thin and can weaken your pelvic floor muscles. Without intervention, your muscles also naturally weaken with age.
Your weakened pelvic floor makes it harder to control your bladder, especially when stress is placed upon it .
Urinary Incontinence In Parkinsons Disease

The most common urinary difficulty experienced by people with PD is a frequent and urgent need to urinate. This may occur even when the bladder is not full. Recent research studies estimate approximately 27-39% of people with PD experience urinary difficulties, although urinary incontinence only develops in about 15% of those with PD. Bladder issues are more common in the later stages of PD.2
Urinary Difficulties In Parkinsons Disease
The most common urinary difficulty experienced by people with PD is a frequent and urgent need to urinate. Urinary incontinence, the involuntary loss of urine, is also a symptom of PD. This may occur even when the bladder is not full. Recent research studies estimate approximately 27-39% of people with PD experience urinary difficulties, although urinary incontinence only develops in about 15% of those with PD. Bladder issues usually develop in the later stages of PD.2
There are several medications that can help manage urinary difficulties, such as tolterodine, oxybutynin, darifenacin, and solifenacin. These medications work to block or reduce overactivity in the bladder. However, these medications may make the symptoms of PD worse. It is recommended to discuss these treatments with a movement disorders specialist who has been trained to understand the effects of various medications on the disease.2
What Causes Fecal Incontinence In Children
For children older than age 4, the most common cause of fecal incontinence is constipation with a large amount of stool in the rectum. When this happens, a child may not be able to sense when a new stool is coming into the rectum. The child may not know that he or she needs to have a bowel movement. A large amount of stool in the rectum can cause the internal anal sphincters to become chronically relaxed, which lets soft stool seep around hard stool in the rectum and leak out.
Birth defects of the anus, rectum, or colon, such as Hirschsprung disease, can cause fecal incontinence in children. These birth defects may weaken pelvic floor muscles or damage nerves in the anus or rectum. Injuries to the nerves in the anus and rectum can also cause fecal incontinence, as can spinal cord injuries and birth defects of the spinal cord.
Circadian Rhythm Disturbances And Nocturia
The suprachiasmatic nucleus of the hypothalamus controls the circadian rhythm by regulating melatonin release from the pineal gland in response to the environmental light/dark cycle.44 Neurodegeneration and cell death occurring in PD has been shown to affect structures involved in circadian rhythm control, such as the hypothalamus. It has been shown that mice overexpressing ?-synuclein exhibit a reduced SCN firing rate, potentially weakening their ability to communicate neural and hormonal signals from the central clock.45 Sleep disturbances are common in PD,46–48 and alterations in the circadian rhythm have been demonstrated in PD, even at the early stages.49, 50
In health, there exists a circadian rhythm for urine production, and, as a result, roughly less than 25% of 24-hour urine is produced during the night. This is thought to be mediated through release of AVP and melatonin and is known to be affected with aging.51 Production of urine is influenced by the circadian regulation of sodium and free water handling.52 Diurnal release of hormones are regulated through the pituitary and increased plasma levels of arginine vasopressin at night.51 A loss of this diurnal response has been observed in otherwise elderly healthy individuals reporting NP.42 A loss of circadian regulation of urine production results in limited reabsorption of free water and diuresis. Reduced AVP secretion is linked not only to nocturnal polyuria,39, 53 but also to nocturnal enuresis.53
