Evaluating And Treating Urinary Issues In Parkinson’s Disease Multiple System Atrophy And The Other Atypical Parkinsonism Disorders
In this hour-long webinar, neuro-urologist Ekene Enemchukwu, MD focuses on urinary incontinence, overactive bladder, urinary retention, and other urinary issues in PD, MSA, and the atypical parkinsonism disorders. Following the presentation, moderator Candy Welch, Brain Support Network’s MSA caregiver support group leader, asks Dr. Enemchukwu many questions submitted by webinar participants.
Gastrointestinal Dysfunctions In Parkinsons Disease: Symptoms And Treatments Denis Soulet
1Axe Neurosciences, Centre de Recherche du CHU de Québec , Quebec City, QC, Canada
2Faculty of Pharmacy, Laval University, Quebec City, QC, Canada
3Department of Psychiatry and Neuroscience, Faculty of Medicine, Laval University, Quebec City, QC, Canada
4Faculty of Medicine, Laval University, Quebec City, QC, Canada
Abstract
1. The Importance of Nonmotor Symptoms in Parkinson’s Disease
In the early 19th century , with the publication of An Essay on the Shaking Palsy , Dr. James Parkinson was the first to provide a clear clinical description of the disease that now bears his name . There are currently four motor features characterizing this neurological disorder, namely, muscle rigidity, tremor at rest, bradykinesia, and postural instability . However, a definitive diagnosis of Parkinson’s disease is difficult to establish and can be obtained only postmortem by the demonstration of the presence of Lewy bodies . Therefore, clinicians currently rely not only on motor symptoms manifestations but also on a positive response to levodopa treatment .
2. GI Manifestations in Autonomic Disorders
2.1. Constipation
2.2. Drooling
2.3. Dysphagia
2.4. Nausea, Vomiting, and Gastroparesis
2.5. Pathophysiology
Recently, several clinical and postmortem studies exploring Lewy bodies expression and/or the presence of neurodegeneration in the enteric nervous system of parkinsonian patients have been conducted in order to better understand the etiopathogenesis of PD .
| Studies |
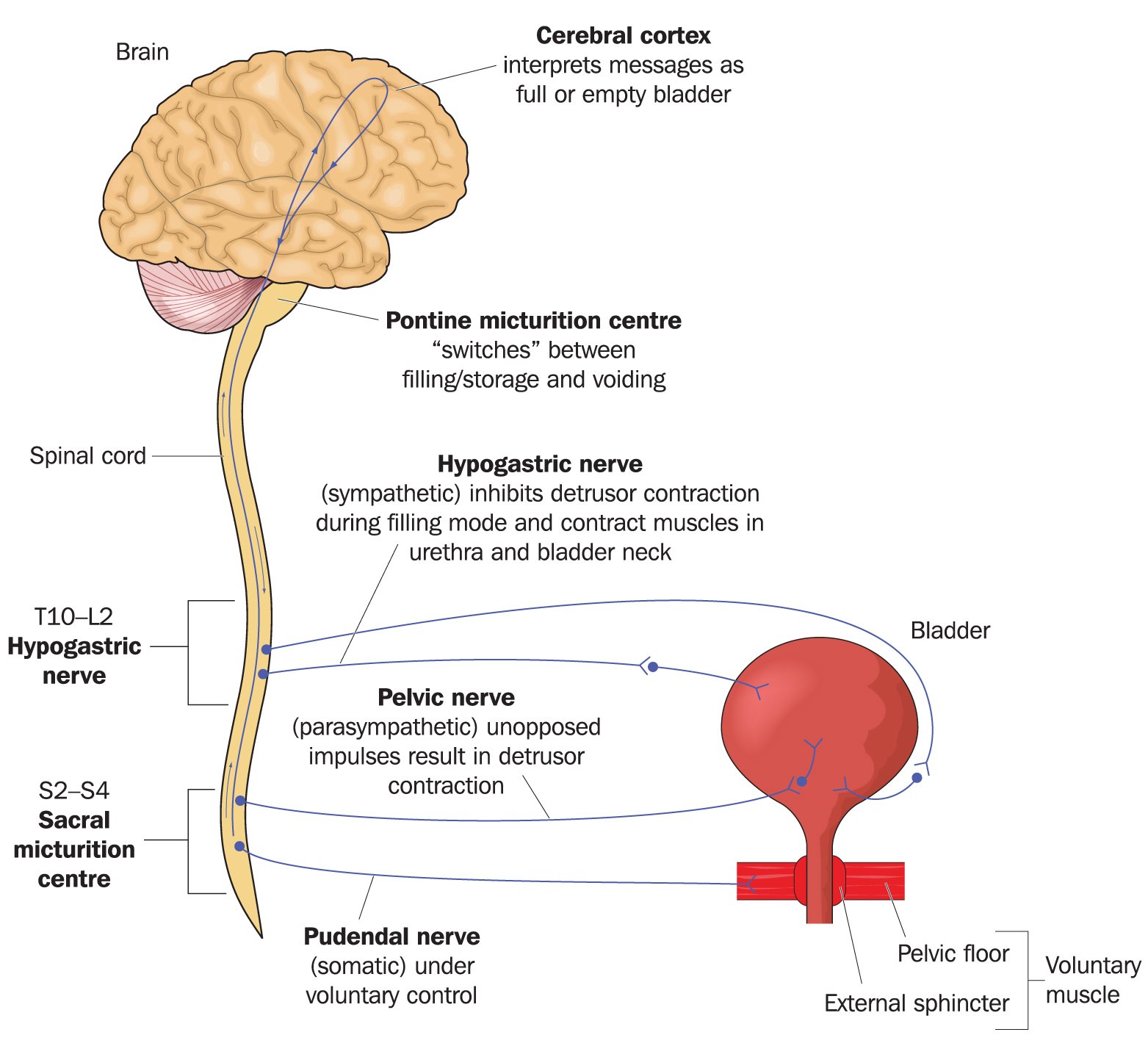
Neural Control Of Micturition: Normal Micturition And Detrusor Overactivity
The lower urinary tract consists of two major components, the bladder and urethra. The bladder has abundant muscarinic M2, 3 receptors and adrenergic beta 3 receptors, and is innervated by cholinergic and noradrenergic fibers for contraction and relaxation, respectively . The urethra has abundant adrenergic alpha 1A/D receptors and nicotinic receptors, and is innervated by noradrenergic and cholinergic fibers . The LUT performs two opposite functions, storage and emptying of urine, both of which require an intact neuraxis that involves almost all parts of the nervous system . This is in contrast to postural hypotension, which arises due to lesions below the medullary circulation center in humans .
Neural circuitry relevant to micturition. PAG, periaqueductal gray; LC, locus ceruleus; NBM, nucleus basalis Meynert; PVN, paraventricular nucleus; MPOA, medial preoptic area; A, adrenergic/noradrenergic; ZI, zona incerta; VTA, ventral tegmental area; SNC, substantia nigra pars compacta; DLTN, dorsolateral tegmental nucleus; PBN, parabrachial nucleus; IML, intermediolateral cell column; GABA, ?-aminobutyric acid; T, thoracic; L, lumbar; S, sacral. See text.
Neural Control Of Defecation: Enteric Nervous System And Dopamine
The enteric nervous system plays the most important role in regulating the peristaltic reflex of the lower gastrointestinal tract . Slow phasic pressure waves are the most common manometric phenomenon , and are measured in the colon and rectum in humans . The origin of the slow wave rhythmicity in LGIT has been identified in the myenteric and submucous plexuses, where interstitial cells of Cajal exist . The peristaltic reflex consists of two components: ascending contraction oral to, and descending relaxation caudal to, the site of stimulus . The reflex can be evoked by surface stroking or by circumferential stretch , in which 5-HT stimulates the sensory nerve terminals . The oral excitatory component is mediated by cholinergic fibers whereas the aboral inhibitory component is mediated by nonadrenergic, noncholinergic fibers. Thus, local neuronal circuits and ICCs, together with appropriate external stimuli, might bring about the peristaltic reflex. Other types of pressure changes in the colon include giant motor complexes , which is perhaps analogous to the migrating motor complex of small intestine . After a meal, the motility index increases for 20 to 30min and remains elevated for up to 3 hours. A combination of slow waves and giant motor complexes is thought to promote bowel transport, which is measured by colonic transit time in humans .
Articles On Digestive Problems With Dementia And Alzheimer’s
Bowel incontinence is when someone leaks stool or has an entire bowel movement by accident. This might be because they couldn’t get to the bathroom in time or didn’t realize what’s happening. It’s common in people who have Alzheimer’s disease.
Bowel incontinence isn’t usually an urgent problem, but get medical help right away if your loved one has:
- Black, tarry, or cranberry color in the stool
- Severe belly pain, especially with nausea and vomiting
- Bowel incontinence that’s new or gets worse, along with diarrhea and fever. Be especially alert if they were recently in the hospital or used antibiotics.
If your loved one has a bloody bowel movement, stay calm. These aren’t usually serious. Help them clean up, and as you do, try to estimate the amount of blood. If it’s just a little, it may be caused by something simple, such as the frequent use of toilet paper, hemorrhoids, or irritation to the anus or rectum.
In some cases, if there’s only a small amount of blood, it may be OK to watch and see if it comes back. But if your loved one is on blood thinners, get medical help right away.
You should also call their doctor if you notice . These can include:
- Urinating very little, or not urinating for 8 or more hours
- A dry tongue, especially if it’s so dry it has grooves or furrows in it
- A heart rate faster than 100 beats per minute
- Being less alert or more confused than usual
- Extreme weakness
- Trouble speaking
What Causes Constipation In People With Parkinson’s Disease
In some people with Parkinson’s disease, constipation may occur due to the improper functioning of the autonomic nervous system. The autonomic nervous system is responsible for regulating smooth muscle activity. If this system is not working properly, the intestinal tract may operate slowly, causing constipation.
Also, medications used to treat Parkinson’s disease can cause constipation.
Bowel Incontinence: Another Embarrassing Casualty Of Pd
Fecal Incontinence is where you lose control of your bowels. This blog post explains the primary cause of this in Parkinson’s disease. Problems reaching the toilet in time because of mobility, abdominal bloating or cramping compound the problem. Dr. De León has included a check list of things to help minimize occurrences and embarrassment, even to the point of surgery, if necessary.
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
Dietary Fibre For Constipation In Parkinsons Disease

Be guided by your doctor, but general suggestions include:
- Choose easy-to-eat fibrous foods such as soft fruits. Consider mashing or pureeing fruits to make them easier to eat. Make sure to include the skin, where most of the fibre is found.
- Eat at least two pieces of fruit and five serves of vegetables every day.
- Eat homemade vegetable soups.
- Sprinkle a tablespoon of bran, psyllium husks or chia seeds on your breakfast cereal or add the bran to baked products such as cakes. However, avoid bran if you have swallowing problems.
- Fibre supplements may be helpful, but you must drink enough fluids for these to work properly. Avoid fibre supplements if you have problems swallowing.
- Don’t increase dietary fibre too quickly or you’ll risk bloating and abdominal cramps. If discomfort occurs, cut back your fibre intake, increase your fluid intake, apply a hot water bottle to your abdomen and see your doctor.
Toilet Habits And Constipation In Parkinsons Disease
Suggestions for good toilet habits include:
- Go to the toilet as soon as you feel the urge to pass a bowel motion. Hanging on can contribute to constipation.
- Use the correct posture on the toilet to help you pass a bowel motion – place your elbows on your knees, bulge out your stomach, straighten your spine and put your feet on a footstool.
- Avoid holding your breath and don’t strain when you are on the toilet. Allow yourself plenty of time.
- Use a warm washcloth pressed against your back passage or gently massage with one or two fingers to help to relax the muscles.
- Talk to your doctor or pharmacist about medicines to help soften your bowel motions.
What Can You Do About Weight Loss Associated With Pd
If you do find yourself unable to maintain a healthy weight, discuss this with your doctor. The good news is that after a medical workup, he or she may suggest one or more of the following steps that can help you:
Tips and takeaways
- Despite a diagnosis of PD, weight loss should prompt a full medical workup.
- Weight loss that is attributed to PD can be caused by a variety of reasons including decreased appetite, increased energy expenditure, swallowing difficulties, and poor gut motility.
- Weight loss has been linked to a poorer quality of life in PD and may contribute to increasing frailty.
- There are steps you can take that may help. Depending on the causes contributing to weight loss, efforts to counteract weight loss could include consultation with a dietician, swallow evaluation and PD medication adjustment.
- As with all symptoms, discuss your concerns about weight loss with your doctor.
Do you have a question or issue that you would like Dr. Gilbert to explore?
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
Addressing Practical Aspects Of Eating And Drinking
Some people with Parkinson’s have problems chewing and swallowing. This can make it difficult to eat a diet with plenty of fibre. A speech and language therapist can give advice about this. Ask your GP, specialist or Parkinson’s nurse for a referral. If it takes a long time to eat and your meal goes cold, eat smaller portions and go back for seconds that have been kept warm. You can also get special plates that keep your meals hot – the Disabled Living Foundation has more information.
An occupational therapist will also be able to give you some tips and practical advice.
The Gastrointestinal Effects Of Parkinson’s Disease
Surveys show that between 20% and 40% of people with Parkinson’s disease suffer from serious constipation . Larger numbers of people with PD have related gastrointestinal issues such as bloating, a feeling of fullness and nausea.?? As the disease progresses, all of these GI problems become more common. In rare cases, serious complications—such as megacolon and perforation or tearing of the colon—may arise from these GI problems.
The connection between the two may seem odd on the surface, but research shines some light on these unpleasant consequences of the disease.
A large survey of healthy people who were followed over several years revealed that men who reported having less than one bowel movement daily had a 2 to 7 times higher risk of developing PD than that of men who had daily bowel movements; their risk was four times higher than that of men who had two or more bowel movements a day.??
What Can Be Done About These Unpleasant Gi Problems
Unfortunately, research studies on GI problems related to PD have been few and far between, so doctors do not have any tried and true methods to deal with them. Some of the drugs to treat GI problems in people without PD cannot be used for those with PD because these drugs negatively impact dopamine systems in the brain.
If you have PD and experience constipation, it makes sense to try to use safe and simple methods to address this issue before you add new drugs to your daily regimen. Increasing dietary fiber and drinking lots of water and other fluids is a reasonable first step in treatment. If your doctor approves it, you might also consider taking fiber supplements, such as psyllium or methylcellulose. If these simple methods don’t work, your doctor might consider giving you a stool softener or a laxative.
Neural Control Of Erection: Normal Erection In Men
Sexual dysfunction is not uncommon in PD . Studies have shown that sexual dysfunction has great significance in relation to quality-of-life measures. However, the detailed mechanism of sexual dysfunction in PD has not been well known.
The genital organ primarily shares lumbosacral innervation with the lower urinary tract. Erection is a vascular event ; occurring secondarily after dilatation of the cavernous helical artery and compression of the cavernous vein to the tunica albuginea . Helical artery dilatation is brought about by activation of cholinergic and nitrergic nerves; this activation facilitates nitric oxide secretion from the vascular endothelium. Ejaculation is brought about by contraction of the vas deferens and the bladder neck, in order to prevent retrograde ejaculation, by activation of adrenergic nerves . Sexual intercourse in healthy men can be divided into 3 phases : desire , excitement and erection, and orgasm, seminal emission from the vas deferens, and ejaculation from the penis. Erection can be further classified into 3 types by the relevant stimulation: psychogenic erection , reflexive erection , and nocturnal penile tumescence sleep). “Morning erection” is considered the last NPT in the nighttime.
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
Fecal incontinence can also be related to nerve dysfunction of the anal sphincter, or the ring of muscle that controls when feces is released. Cognitive dysfunction and mobility issues may further interfere with getting to the bathroom in time. Some treatment options are similar to urinary incontinence including the use of bedside equipment to minimize mobility issues and introduction of pelvic floor exercises to strengthen the musculature that keeps feces in place.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dr. Rebecca Gilbert
Background: The Stomach Parkinson’s And Levodopa

Levodopa is not absorbed from the stomach, but the stomach plays an important role in controlling how levodopa reaches the parts of the small intestine where it is absorbed. Some medicines, including dopamine agonists and anticholinergics, can also delay gastric emptying, as can severe stomach acidity, although over-treatment of this problem can also prevent the break-down of levodopa tablets, leading to incomplete absorption.
Unfortunately, gastric emptying can be delayed by Parkinson’s itself or by constipation caused by the colon-gastric reflex. Levodopa tablets may remain in the stomach for a long time, leading to delayed absorption in the small intestine and a delayed response to the treatment.
An enzyme called dopa-decarboxylase that is present in the stomach lining can convert levodopa trapped in the stomach into dopamine, making it unavailable to the central nervous system. Also, dopamine formed in the stomach may stimulate gastric dopamine receptors, leading to stomach relaxation and reduced gastric motility, and this can worsen the problem.
Liquid levodopa may improve motor fluctuations by ensuring better absorption than standard preparations, especially when taken after meals. Subcutaneous infusion of the dopamine agonist apomorphine is effective in controlling motor fluctuations by bypassing the gastrointestinal tract.
Treatment For Constipation In Parkinsons Disease
Your doctor may suggest various treatments to help combat constipation, including:
- dietary changes, including more fibre rather than refined or highly processed foods, and water
- moderate exercise
- good toilet habits
- avoidance of unnecessary medicines that contain substances known to cause constipation
- laxatives, particularly agents that bulk and lubricate the stools
- treatment for any other medical problem that may be contributing to your constipation, such as haemorrhoids .
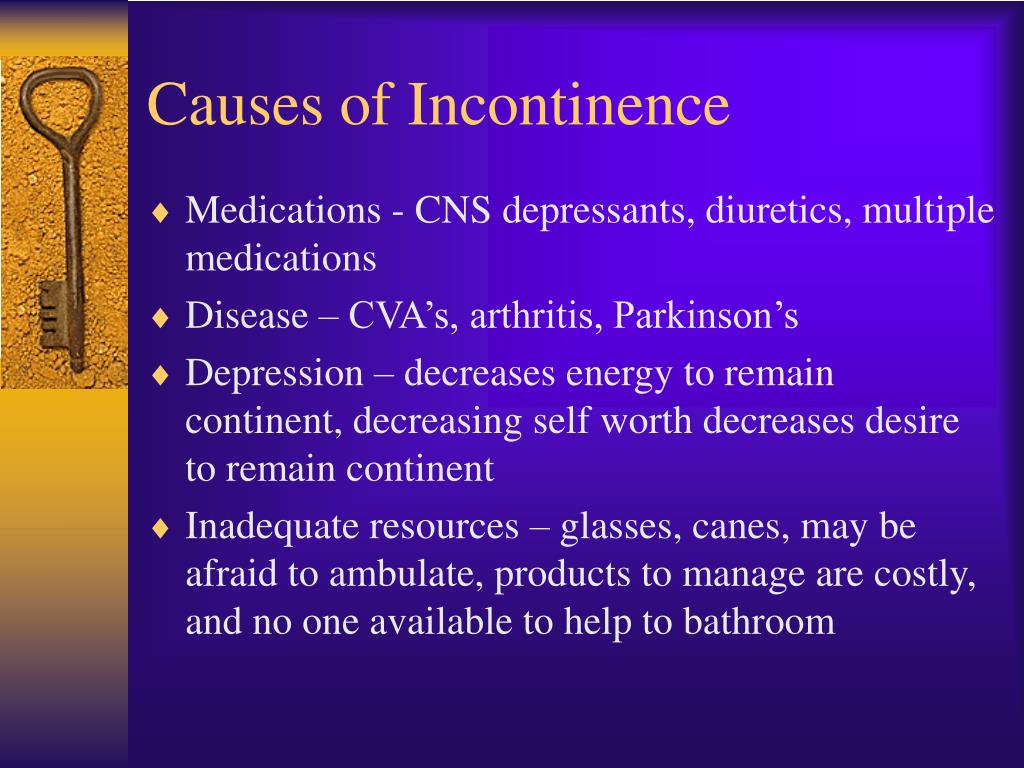
What Causes Incontinence In People With Dementia
In the later stages of dementia, a person’s ability to react quickly and remember things is reduced. They may no longer recognize when they experience the urge to urinate or have a bowel movement. Reasons for incontinence in someone with dementia include:
- not recognizing the bathroom
- mental status changes or abrupt worsening of confusion, including significant changes in behavior
UTIs can worsen without proper treatment.
Treatment For Over Active Bladder In Parkinsons
Overactive bladder affects up to 27% of men and 43% of women of the global population. Now, add a neurological condition and the problem becomes more challenging. First, there is a list of medications which make the problem worse, so should be avoided. Then, a thorough evaluation and physical exam. Treatment depends on the cause, but evaluating all medications and an adjustment of dopamine medication is often necessary. If you are still having problems, five further treatment options are included.
Diagnosis Of Constipation In Parkinsons Disease
Diagnosis of constipation may include:
- medical history
- detailed description of symptoms
- physical examination.
Medical problems other than Parkinson’s disease can also cause constipation. Your doctor may wish to do tests to rule out other possible causes. The tests depend on the medical condition under investigation.
Exercise For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Talk with your doctor, physiotherapist, exercise physiologist or healthcare professional when planning your exercise program.
- Aim for at least 30 minutes of exercise every day.
- Spend a few minutes warming up and cooling down. This could include marching in place or stretching.
- Start with the easiest exercises first. Slowly introduce the more difficult exercises as your fitness increases.
- Only exercise when other people are at home who can help if necessary.
- Remember: too little exercise and fluid intake with an increase in dietary fibre can worsen constipation for some people.
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Forgetfulness
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. It’s clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
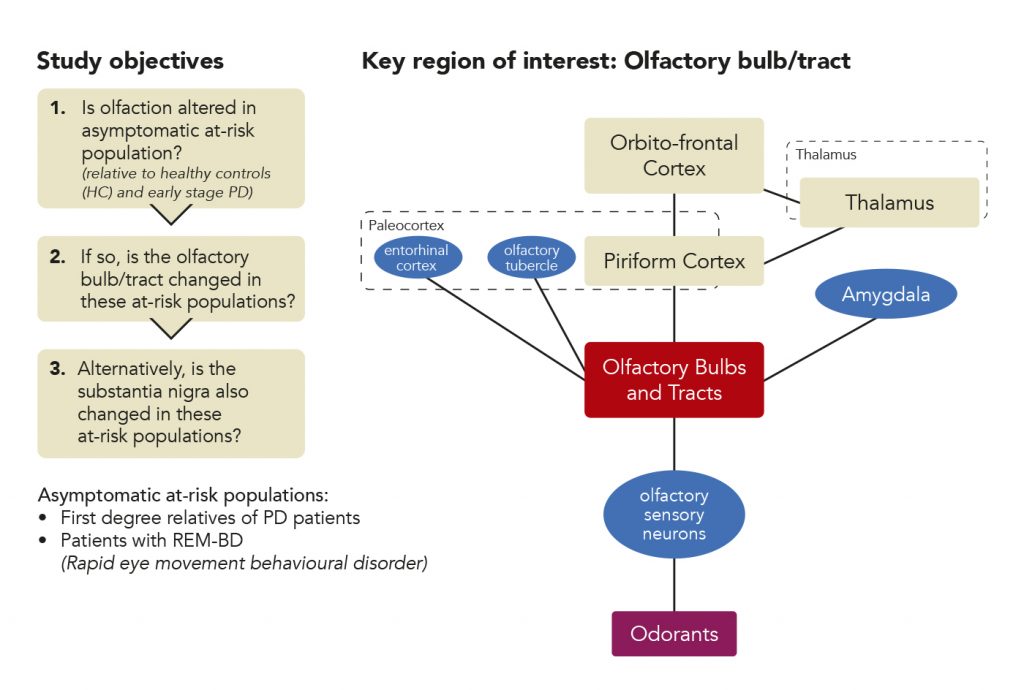
Why People With Parkinson’s Tend To Lose Weight
There are many theories about the origin of weight loss for people with Parkinson’s disease. Some believe a loss of smell, which can affect appetite, leads to weight loss as well as increased energy expenditure and fat burning due to tremors and dyskinesias.?? Other theories point to mood disorders related to Parkinson’s disease such as depression. Yet, none of these factors have been definitely confirmed as the sole cause of weight loss.
Why Worry About Weight Loss Associated With Pd

Weight loss has been linked to a poorer quality of life and more rapid progression of PD. The reasons for this are two-fold. On the one hand, as outlined in the list above, weight loss can be a hallmark of advancing disease – as it could be a consequence of more swallowing difficulties, worsened mobility, more impaired gut function etc.
On the other hand, having weight loss can further lead to poorer health. Inadequate food intake can contribute to malnutrition and vitamin deficiencies. Malnutrition can subsequently be the cause of increased susceptibility to infection, increased fatigue and increased frailty. The situation can spiral with more fatigue and frailty causing a further decrease in activity and function.
Osteoporosis, or porous and fragile bones, is more common in under-weight people since bone structure is dependent on weight-bearing. Since osteoporotic bones are more prone to fracture during a fall, this too can be a contributor to more disability and frailty. Bottom line is that it is important for your health to maintain a healthy weight.
Urinary Issues In Advanced Parkinsons Disease
Urinary dysfunction and symptoms in PD are most commonly caused by overactivity of the detrusor muscle, or the muscle of the bladder, which contracts excessively despite the fact that it is not filled with urine. This causes an increased urge to urinate and/or an increased frequency of urination, which can be especially prominent at night. In advanced PD, this could culminate in urinary incontinence, or involuntary release of urine. Mobility issues which make getting to the bathroom slower and more cumbersome, compound the problem.
Always remember that people with advanced PD may have other medical problems that affect their urination such as an enlarged prostate. Make sure to have a complete evaluation before assuming that the problem is only related to PD. It is also essential to keep in mind that if changes in urination occur suddenly, there could be a urinary tract infection present.
Once other medical issues and urinary tract infection are ruled out, there are a number of approaches to the issue of urinary incontinence in a person with advanced PD:
Unfortunately, for some, the above available options may not be sufficient to effectively treat urinary incontinence in advanced PD. If this is the reality, it becomes extremely important to keep the skin dry with frequent changes of incontinence products to prevent skin breakdown and the potential development of skin infection.
Fluids For Constipation In Parkinsons Disease
Be guided by your doctor, but general suggestions include:
- Try to drink six to eight glasses of fluid every day. Water is best, but you can also include fluid in the form of soup, juice, tea and coffee.
- Limit drinks that cause dehydration such as alcohol, tea and coffee.
- Spread your drinks throughout the day.
Causes Of Constipation In Parkinsons Disease
The ways in which Parkinson’s disease can increase the risk of constipation include:
- lack of dopamine in the brain – impairs control of muscle movement throughout the body. Bowel muscles can become slow and rigid
- uncoordinated bowel motions – the bowel muscles may be weak and unable to contract, or they may clench instead of relaxing when trying to pass a motion
- eating problems – dietary fibre containing insoluble fibre adds bulk to your bowel motions and can help prevent constipation. However, if a person with Parkinson’s disease finds it difficult to chew or swallow, they may avoid eating fibrous foods
- drinking problems – you need water to plump up the dietary fibre in your bowel motions. Swallowing difficulties may discourage a person with Parkinson’s disease from drinking enough fluids
- sedentary lifestyle – lack of exercise slows the passage of food through your intestines. Parkinson’s disease reduces muscle control, so lack of exercise is common
- medications – many different medications can cause constipation. Medications used in the treatment of Parkinson’s disease may slow bowel movements or cause a decrease in appetite.
Parkinson’s Disease And Voiding Dysfunction
In this 54-minute webinar, urologist Dr. Sidney Radomski explains how voiding function is affected by Parkinson’s disease in both men and women. He discusses how an enlarged prostate contributes to voiding problems and management options of voiding dysfunction for those with Parkinson’s disease and MSA.
What Are The Symptoms Of Fecal Incontinence
The symptoms of fecal incontinence depend on the type.
- If you have urge fecal incontinence, you will know when you need to pass stool but not be able to control passing stool before reaching a toilet.
- If you have passive fecal incontinence, you will pass stool or mucus from your anus without knowing it.
Some medical experts include streaks or stains of stool or mucus on your underwear—called soiling—as a symptom of fecal incontinence.
Separating Fact From Fiction About Sciatica
Your sciatic nerve starts in your lower back and travels down to your toes. This is true- your sciatic nerve is the largest single nerve in your entire body.
It starts in the front of the piriformis muscle, which is deep in your buttocks, and encompasses the lowest two nerves exiting the lower spine- your L4 and L5 vertebrae- and your first three sacral nerves- your S1, S2, & S3.
Each one of these nerves has two branches, one on each side of your spine. The root of each of these nerves exits your spine between two of the vertebrae in your lower back, travels down the back of each one of your legs, and then branches out of your leg into each one of your feet.
Pain that radiates along your sciatic nerve is excruciating- and can even be debilitating for many individuals.
Leg Pain caused by sciatica is due to a problem in your lower back. This is true- even though most people believe that when they experience leg pain, it means that there is something going wrong with their legs.
However, due to the fact that your sciatic nerve goes through your lower back, into your legs, and finally into your feet, problems resulting in nerve compression in your lower back can cause you to experience pain in your lower back, your legs, your feet, and even sometimes causes your toes to be in pain.
The condition of piriformis syndrome feels much like the condition of sciatica- but they are actually two completely different conditions.
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
What Causes Fecal Incontinence In Children

For children older than age 4, the most common cause of fecal incontinence is constipation with a large amount of stool in the rectum. When this happens, a child may not be able to sense when a new stool is coming into the rectum. The child may not know that he or she needs to have a bowel movement. A large amount of stool in the rectum can cause the internal anal sphincters to become chronically relaxed, which lets soft stool seep around hard stool in the rectum and leak out.
Birth defects of the anus, rectum, or colon, such as Hirschsprung disease, can cause fecal incontinence in children. These birth defects may weaken pelvic floor muscles or damage nerves in the anus or rectum. Injuries to the nerves in the anus and rectum can also cause fecal incontinence, as can spinal cord injuries and birth defects of the spinal cord.
Take Control Of Your Parkinsons Treatment
Our Every Victory Counts® manual gives people living with Parkinson’s, their care partners and their family members the tools they need to take control of their own Parkinson’s treatment through a proactive approach to self-care.
a powerful new print edition
It’s jam-packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
Living With Bowel Or Bladder Incontinence
There is no single, right way to cope with bladder or bowel incontinence. The challenge is to find what is best for your situation, so you can get the help you need and return to a normal daily life. Talk with your health care team if you notice a change in bowel or bladder habits, and about the best ways to manage incontinence, if it is a problem. You might find it helpful to talk with other people who are dealing with incontinence, too. Ask a member of your cancer care team about support groups in your area.
Here are some things you can do that may help make incontinence less of a problem:
- Empty your bladder every 3 to 4 hours while awake, to avoid accidents.
- Empty your bladder before bedtime or before strenuous activity.
- Limit drinks with caffeine, or and avoid alcohol and citrus juices, which can irritate the bladder and make you have to go more often.
- Avoid hygiene products that may irritate you Women should avoid feminine spray or over-the-counter vaginal suppositories.
- Because belly fat can push on the bladder, avoiding weight gain or losing needed weight sometimes helps improve bladder control.
- Avoid tobacco use which can cause coughing and bladder irritation due to harmful substances in tobacco products.
- Talk to your doctor about all medicines, vitamins, herbs, and supplements you’re taking. Some may affect urine control.
