Parkinson’s Disease Early Stages Detected With ‘simple’ Mri; Up To 85% Accurate
Detecting a life-threatening disease could give researchers the power of earlier diagnosis, treatment approaches, and innovative therapies — a power that could one day possibly lead to cure a disease like Parkinson’s. Researchers from Oxford University published their findings in the journal of Neurology, which reveal a promising new diagnostic approach for the early stages of Parkinson’s disease.
“At the moment we have no way to predict who is at risk of Parkinson’s disease in the vast majority of cases,” said Dr. Clare Mackay, the study’s co-author and professor of the Department of Psychiatry at Oxford University. Oxford researchers are turning the tables on that bleak risk evaluation now that they have developed an expediently simple technique to diagnose early Parkinson’s stages with a magnetic resonance imaging machine with 85 percent accuracy. A normal MRI scan cannot detect the early signs, which is why researchers used restating state functional MRI to look at how strong the brain connections were in the basal ganglia, where important dopamine nerves are located.
“We think that our MRI test will be relevant for diagnosis of Parkinson’s,” said Dr. Michele Hu, the study’s co-author and professor of the Nuffield Department of Clinical Neurosciences at Oxford University and the Oxford University Hospitals NHS Trust.
Differential Diagnosis Of Parkinsonian Syndromes Using Quantitative Biomarkers
Several studies have suggested that the combination of R2* and FA markers may better differentiate people with PD from healthy aged subjects with greater than 95% global accuracy .
In MSA-P, increased diffusivity and reduced anisotropy was found in the putamen, pons and middle cerebellar peduncle and greater iron deposition in the putamen, using phase-contrast susceptibility imaging or relaxometry .
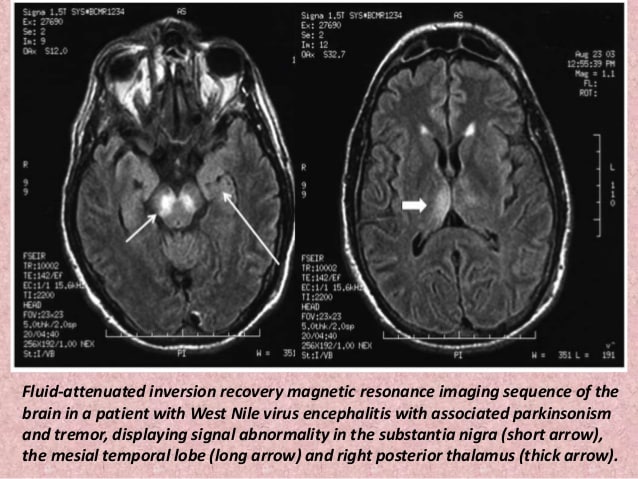
Imaging Studies Can Differentiate Parkinsons From Other Causes Of Parkinsonism
Catherine L. Gallagher, MD
Although Parkinson’s disease remains a clinical diagnosis, imaging studies are an important ancillary test for differential diagnosis of movement disorders. Imaging studies may be used to rule out structural and other causes of parkinsonian symptoms. Single-photon emission computed tomography scans using labeled tracers for dopamine transporters can also be used to confirm parkinsonism or differentiate PD from secondary causes of parkinsonian motor symptoms. Finally, imaging studies are being used in research to better understand the pathophysiology of PD and elucidate causative mechanisms that could be therapeutic targets in the future.
Diagnosis Of Parkinsons Via Datscan And Clinical Exam Are Similarly Accurate
Despite the DaTscan being available to help diagnose Parkinson’s, in most clinical situations, a DaTscan will not add information to what can be gleaned from the clinical exam. One study actually demonstrated that the accuracy of diagnosis in early PD was the same whether the diagnosis was reached using clinical exam or using DaTscan.
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Differences Between Parkinsons Disease And Atypical Parkinsonism
The symptoms of Parkinson’s disease and atypical parkinsonism overlap, and in a clinical setting, it can be hard to tell if a patient has one or the other. Atypical parkinsonism is diseases that present some of the signs and symptoms of Parkinson’s Disease but do not respond well to drug treatment. With an MRI, your doctor can help to make the diagnosis more accurate, which is essential for quality treatment. Additionally, an MRI can also help your medical team to determine if you have a certain type of atypical parkinsonism. This can help to create a prognosis and guide your treatment options.
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Morphometric And Signal Changes In Other Parkinsonian Syndromes
Volumetric MRI was efficient for differentiating Parkinsonian disorders such as progressive supranuclear palsy and the Parkinson variant of multiple system atrophy from PD. There changes were reviewed extensively . In contrast to PD, where structural changes are subtle or absent, PSP patients present with extensive atrophy in the brainstem, basal ganglia and cortex. Midbrain atrophy in PSP has a characteristic shape described as the ‘penguin’ or ‘hummingbird’ sign and can be quantified using various indexes . Using VBM, grey and white matter reductions have been constantly reported in PSP in the midbrain and more variably in the basal ganglia, the frontal cortex, the insula and the thalamus . In MSA-P, atrophy and signal changes were observed in the putamen , the pons , the middle cerebellar peduncle and the cerebellum . PSP patients had greater midbrain and superior cerebellar atrophy whereas MSA-P patients had greater pontine and middle cerebellar atrophy . In MSA-P patients atrophy was also evidenced in the cortex using VBM . Quantitative volumetric measures of pontine and midbrain areas were able to discriminate accurately PSP and MSA-P from PD patients or healthy controls.
Techniques For Visualization And Segmentation Of Brain Regions
MRI sequences for visualization of the basal ganglia and the cortex
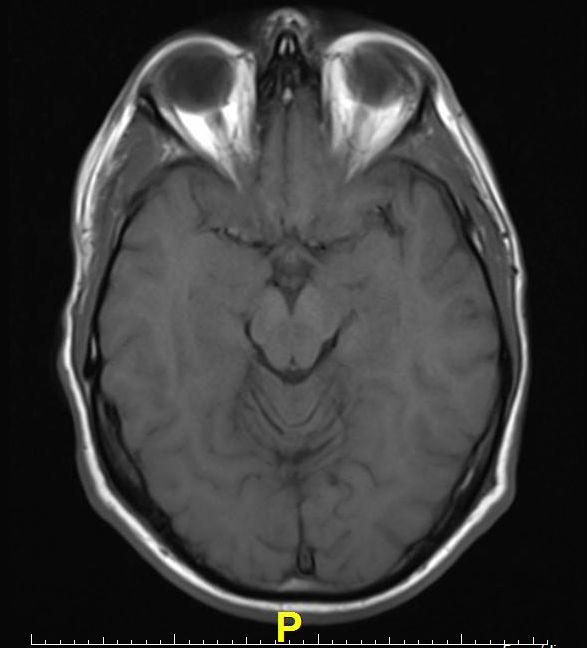
The anatomy of the cortex is usually better depicted using conventional three-dimensional T1-weighted sequences which present high grey/white matter contrast.
Segmentation and volume calculation
Small structures such as the SN are usually outlined and segmented manually. Some cortical regions can be segmented manually, but automated techniques are preferred as exploratory tools to detect grey and white matters changes in the cortex . These techniques are designed for group studies, are automated, whole brain and rater independent. They include voxel-based, deformation-based and tensor-based morphometry, cortical thickness and sulci measurements. Voxel-based morphometry is now a standard technique, sensitive to differences in grey and white matter . VBM provides metrics such as the concentration, density and volume of grey matter. A major limitation of VBM is the nonspecificity with respect to the underlying tissue changes. Deformation-based and tensor-based morphometry provide information about global or local differences in shape, respectively . Other software allows measurements of topographic differences in thickness, surface area and curvature of the cortex .
Is The Imaging Metric Appropriate For The Question Being Asked Fig. 1.Neuroanatomy Relevant to Parkinson’s Disease
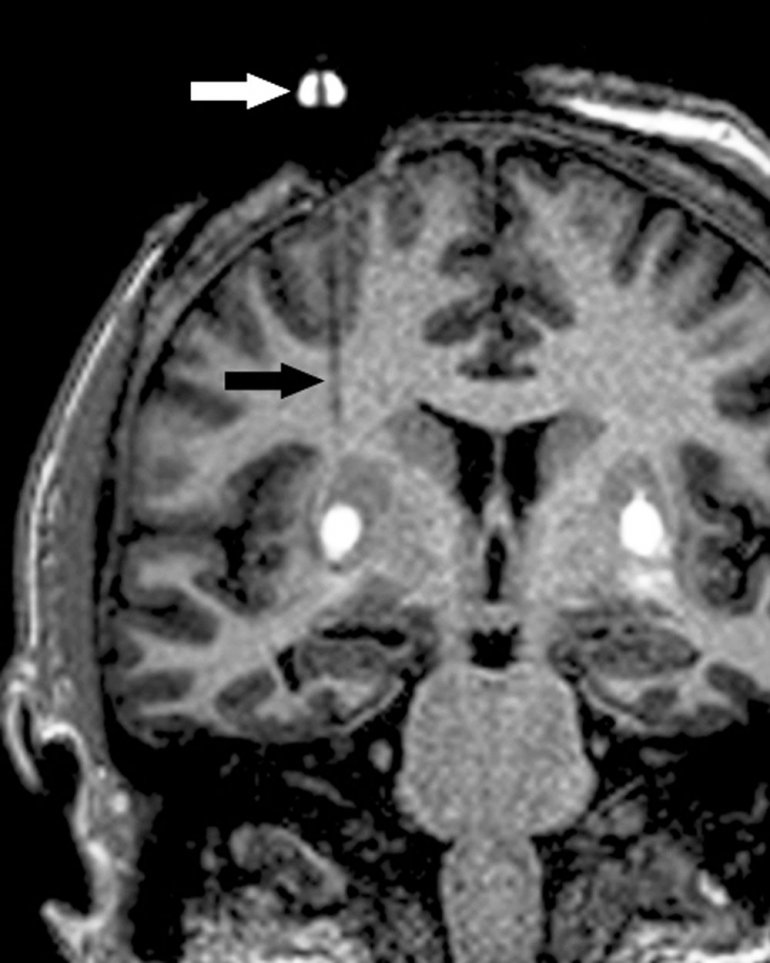
A. Braak staging of ?-synuclein pathology. At death, PD patients exhibit the following stages of ?-Syn pathology: stage I olfactory bulb only , Stage IIa brainstem predominant , stage IIb – limbic predominant , stage III brainstem and limbic and stage IV neocortical . While not all patients with pathology will exhibit clinical symptoms , the progression of neuropathology generally corresponds to the progression of both motor and non-motor symptoms . B. The SN is subdivided into the ventral pars reticulata and the dorsal pars compacta , the latter is composed of dopaminergic neurons. The SNc is further divided into the dorsal and ventral tier, with the loss of dopaminergic neurons occurring first in the caudal and ventrolateral tier . Within A9, there are five nigrosomes , with N1 exhibiting the earliest loss of dopaminergic neurons . Dopaminergic neuronal loss typically spreads to neighboring groups from the N1 in PD . C. Fronto-subcortical loops comprise the motor, associative, and limbic domains, which respectively transit through the posterior, anterior, and ventral striatum, thus segregated functionally and anatomically. GPe = globus pallidus externa. GPi = globus pallidus interna. STN = subthalamic nucleus. SNc = substantia nigra pars compacta. SNr = substantia nigra pars reticulata. Adapted with permission from: .
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
When Brain Mri Is Recommended To Help Diagnose Parkinsonism
Differentiating atypical parkinsonism from Parkinson’s disease can be a challenge in patients presenting with symptoms in early disease stages. A diagnosis cannot be made from a brain magnetic resonance imaging scan, but brain MRI can be of added value when there is uncertainty about the clinical diagnosis.
The appropriateness of and the added diagnostic value of a brain MRI scan in the work-up of parkinsonism is described in a newly published article in the Journal of Parkinson’s Disease. Lead author Frederick J.A. Meijer, MD, PhD, a neuroradiologist in the department of radiology and nuclear medicine at Radboud University Medical Center in Nijmegen, The Netherlands, offers advice on the scanning protocol to use, and also discusses its diagnostic value with respect to specific abnormalities that can be seen.
The authors of the article, who also include neurologists from the Radboud University Medical Center and Donders Institute for Brain, Cognition and Behavior, conducted a 3-year long prospective study on the contribution of routine brain MRI to the differential diagnosis of parkinsonism.1 Based on this research, the authors refuted clinical guidelines recommending standard use of cerebral MRI for all patients presenting with parkinsonism.
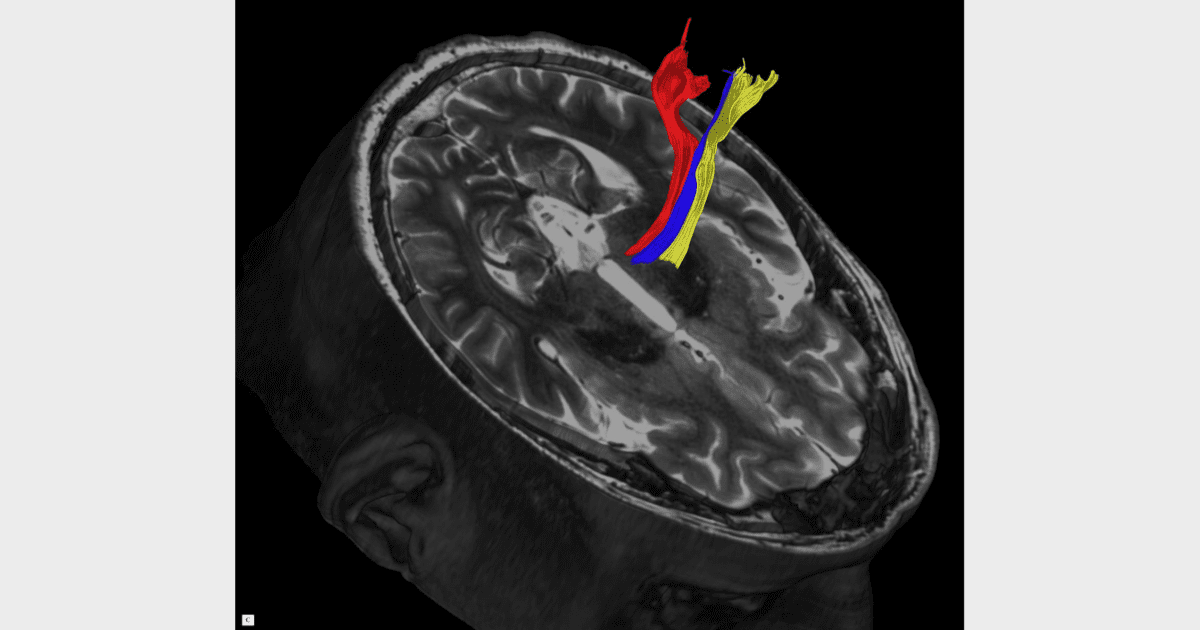
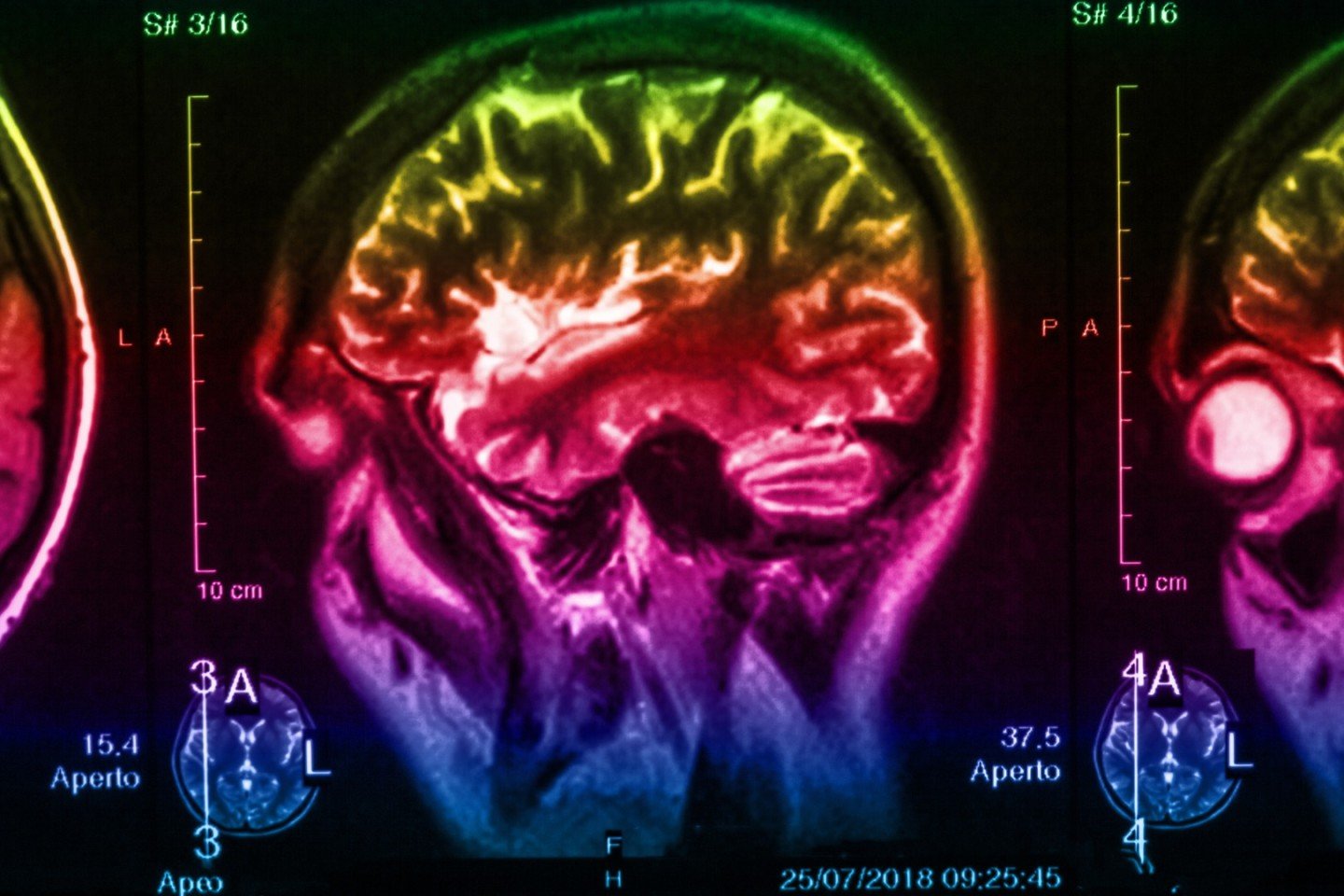
3T brain MRI including DTI tractography in a patient presenting with parkinsonism.
Clinical Application Of Brain Mri In The Diagnostic Work
aDepartment of Radiology and Nuclear Medicine, Radboud University Medical Center, Nijmegen, The NetherlandsbDepartment of Diagnostic Imaging, Medical Center of Postgraduate Education, Warsaw, PolandcDepartment of Neurology, Donders Institute for Brain, Cognition and Behaviour, Radboud University Medical Center, Nijmegen, The Netherlands
Keywords: Atypical parkinsonism, brain, magnetic resonance imaging, Parkinson’s disease
ABSTRACT
Background: Differentiating Parkinson’s disease and atypical parkinsonism on clinical parameters is challenging, especially in early disease courses. This is due to large overlap in symptoms and because the so called red flags, i.e. symptoms indicating atypical parkinsonism, have not developed. Brain MRI can aid to improve the accuracy and confidence about the diagnosis.Objective and Methods: In the current paper, we discuss when brain MRI should be performed in the diagnostic work-up of parkinsonism, our preferred brain MRI scanning protocol, and the diagnostic value of specific abnormalities.Results and Conclusions: The main purpose of brain MRI is to assess cerebrovascular damage, and to exclude other possible – and sometimes treatable – causes of parkinsonism, such as normal pressure hydrocephalus. Furthermore, brain MRI can support the possible or probable diagnosis of a specific form of atypical parkinsonism.
INTRODUCTION OF THE CLINICAL DILEMMA
DESCRIPTION OF THE TEST
DISCUSSION
ACKNOWLEDGMENTS
CONFLICT OF INTEREST
Brain Scan Can Spot Early Signs Of Parkinson’s Disease
Scientists at Oxford University have discovered that an MRI scan can pick up the very earliest signs of Parkinson’s disease, giving hope that it could be treated before the symptoms start
A brain-scanning technique that detects early signs of Parkinson’s holds out the hope of tackling the disease before it starts to cause symptoms.
Researchers identified patients with early-stage Parkinson’s disease with 85% accuracy using a special type of magnetic resonance imaging scan.
Conventional MRI scans cannot detect early Parkinson’s. The new approach, known as resting state fMRI, involves measuring the connectivity of neurons in the basal ganglia region of the brain.
Lead scientist Dr Clare Mackay, from the department of psychiatry at Oxford University, said: ”At the moment we have no way to predict who is at risk of Parkinson’s disease in the vast majority of cases.
”We are excited that this MRI technique might prove to be a good marker for the earliest signs of Parkinson’s. The results are very promising.”
Around 127,000 people in the UK are believed to have Parkinson’s, an incurable neurodegenerative disease that causes tremors, slow movements and muscle rigidity.
The progressive nerve cell damage produced by the condition is thought to begin long before symptoms appear.
Treatments that slow or halt the disease prior to it taking hold require better ways of identifying those affected.
Datscan: A Test To Help In The Diagnosis Of Parkinsons
In 2011, the Food and Drug Administration approved an imaging test to help diagnose PD. In this test, a radioactive tracer, Ioflupane 123I, also known as DaTscan, is injected into the blood, where it circulates around the body and makes its way into the brain. It attaches itself to the dopamine transporter, a molecule found on dopamine neurons. Several hours after the tracer has been injected, special imaging equipment scans the head to detect the presence of DaTscan.
People with PD will typically have a smaller signal in a part of the brain called the striatum, where the ends of the dopamine neurons are meant to be. Here is a normal scan on the left, which would indicate a healthy dopamine system, next to an abnormal scan on the right, which would indicate an unhealthy dopamine system.
It is important to note that conventional MRI imaging will appear normal in PD and is therefore not helpful in confirming the diagnosis. Other atypical parkinsonian conditions, such as vascular parkinsonism however, can have abnormalities on MRI, so the test may be done to rule out other diagnoses.
Gray Matter Density And Disease Duration Associations
To confirm that group level differences in regional GMD were related to disease duration, a set of regression analyses that examined the relationship between GMD and disease duration controlling for chronological age and sex was performed. The individual regression analyses were conducted using the data of both early and advanced PD patients to increase the range of disease duration present in the sample. For subcortical regions, Ch4 GMD declined with disease duration and Ch123 GMD declined with disease duration . The centromedial amygdala GMD declined with disease duration , superficial amygdala GMD declined with disease duration , laterobasal amygdala GMD declined with disease duration , amygdala-striatal transition area GMD declined with disease duration , and HATA GMD declined with disease duration . Entorhinal cortex GMD declined with disease duration . For cortical regions, only the GMD of the secondary auditory association area TE3 declined with disease duration .
Mri Brain Scans Detect People With Early Parkinson’s
Oxford University researchers have developed a simple and quick MRI technique that offers promise for early diagnosis of Parkinson’s disease.
The new MRI approach can detect people who have early-stage Parkinson’s disease with 85% accuracy, according to research published in Neurology, the medical journal of the American Academy of Neurology.
‘At the moment we have no way to predict who is at risk of Parkinson’s disease in the vast majority of cases,’ says Dr Clare Mackay of the Department of Psychiatry at Oxford University, one of the joint lead researchers. ‘We are excited that this MRI technique might prove to be a good marker for the earliest signs of Parkinson’s. The results are very promising.’
Claire Bale, research communications manager at Parkinson’s UK, which funded the work, explains: ‘This new research takes us one step closer to diagnosing Parkinson’s at a much earlier stage – one of the biggest challenges facing research into the condition. By using a new, simple scanning technique the team at Oxford University have been able to study levels of activity in the brain which may suggest that Parkinson’s is present. One person every hour is diagnosed with Parkinson’s in the UK, and we hope that the researchers are able to continue to refine their test so that it can one day be part of clinical practice.’
We think that our MRI test will be relevant for diagnosis of Parkinson’s
Dr Michele Hu
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Regional Differences In Gmd Slope Directionality
To further test differences in disease progression between early and PD groups, a comparison of the directionality of the early and PD slope parameters for the age and sex adjusted relationships between duration of disease and GMD was performed. For subcortical regions in early PD, one region had a positive slope, compared to 12 regions which had a negative slope. For subcortical regions in advanced PD patients, all 13 regions had a negative slope. For cortical regions in early PD, 13 regions had a positive slope, compared to one region which had a negative slope. For cortical regions in advanced PD patients, all 14 regions had a negative slope. The difference in the distribution of positive and negative slopes for subcortical and cortical regions in early PD is significant . Additionally, the difference in the distribution of positive and negative slopes for cortical regions between early PD and advanced PD is significant .
Other Tests Used To Diagnose Parkinsons Disease
Diagnosis of PD is generally made using a medical history and a physical exam. In addition to these tests, the patient presenting with Parkinsonian symptoms is usually given treatment with the medication levodopa. The relief of symptoms with levodopa is a sign that symptoms are caused by PD.6
An active area of research is discovering “biomarkers”, which are molecules in the blood, urine, or cerebrospinal fluid that can reliably diagnose Parkinson’s disease.
What Diseases Can Be Mistaken For Parkinson’s
This is the list of different diseases that may be mistaken with Parkinson’s disease:
- Progressive supranuclear palsy.
Alzheimer’s disease and primary lateral sclerosis can also be mistaken for Parkinson’s disease. Other similar conditions include essential tremor, dystonic tremor, vascular Parkinsonism, and drug-induced Parkinsonism.
One may also ask, what are the four cardinal signs of Parkinson’s disease? Cardinal symptoms. Four symptoms are considered cardinal in PD: bradykinesia, tremor, rigidity, and postural instability also referred to as parkinsonism. Tremor is the most apparent and well-known symptom.
Moreover, what is similar to Parkinsons?
Progressive Supranuclear Palsy: An Atypical Parkinsonian Syndrome. Progressive supranuclear palsy is not Parkinson’s disease , but is a Parkinsonian-like syndrome. PSP is a rare brain disorder that causes serious and progressive problems with gait and balance, as well as eye movement and thinking problems.
Does stress cause Parkinson’s disease?
Research suggests that stressful life events may increase the risk of Parkinson’s disease. In addition, animal studies indicate that stress damages dopamine cells, resulting in more severe parkinsonian symptoms. In humans, acute stress can worsen motor symptoms, including bradykinesia, freezing, and tremor.
Volume And Shape Changes In Parkinson Disease
Substantia nigra
The volume of the SN is usually measured using manual segmentation. Results in PD are discordant with normal , reduced and even increased volumes . The origin of this variability is probably due to differences in methodology between studies. First, the variability of volume measurements is large, given the small size of the structure. Second, different contrasts were used resulting in changes in SN contours. Third, some methods relied on tractography and anatomical connectivity changes which are completely different in nature as compared with other structural methods. Lastly, increased SN volume was obtained using 7T imaging and may be explained by the increased volume of regions with iron load. Inversion recovery methods were able to detect a predominant involvement of the lateral segments of the SN in line with the preferential degeneration of dopaminergic neurons in the caudal and lateral SN in histological studies . Overall, although volume changes were detected in the SN of PD patients, changes varied between studies and the reproducibility was low. Ultra-high-field MRI may provide improved results due to increased spatial resolution.
Other basal ganglia and brainstem nuclei
Cortex
Nondemented cognitively intact PD
Mild cognitive impairment and dementia
Cortical correlates of other nonmotor dysfunctions
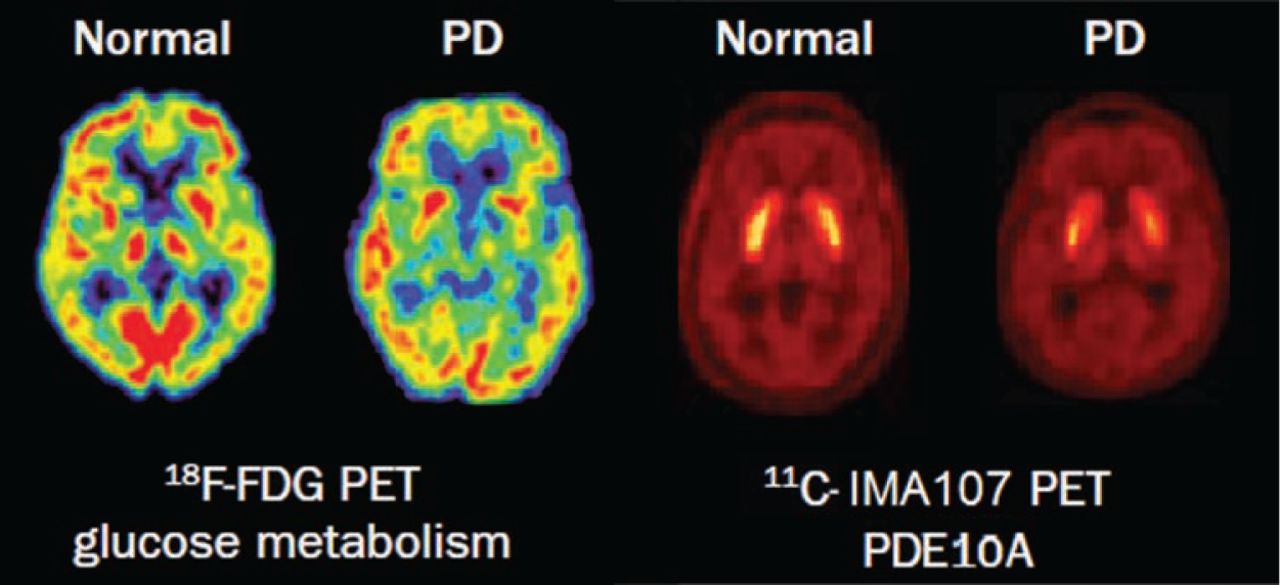
Mri And Pet Reveal Parkinsons Is Two Diseases Whitney J. Palmer
Advanced imaging shows Parkinson’s can begin as brain-first or body-first.
It’s been a long-standing question in neuroscience: is Parkinson’s more than one disease? Now, thanks to MRI and PET scans, clinicians have an answer – yes. And, having this knowledge could pave the way for personalized medicine for these patients.
Based on the analysis of advanced imaging scans, researchers have determined that Parkinson’s in, in fact, two distinct conditions – one that begins in the intestines and moves to the brain, and one that starts in the brain and migrates to the intestines and other organs.
“Until now, many people have viewed the disease as relatively homogeneous and defined it based on the classical movement disorders. But, at the same time, we’ve been puzzled about why there was such a big difference between patient symptoms,” said Per Borghammer, Ph.D., professor of nuclear medicine and neuroscience at Aarhus University in Denmark. “With this new knowledge, the different symptoms make more sense, and this is also the perspective in which future research should be viewed.”
In addition to the showing the differences between the brain-first and body-first types of Parkinson’s, the team also hypothesized that isolated REM sleep behavior disorder – a known risk factor for developing Parkinson’s – could be specifically associated with body-first disease.
The team of Aarhus University researchers published their findings recently in the journal Brain.
Why Doctors Consider Mri To Detect Dementia
Medical experts will advise on the use of MRI when they suspect that a person has dementia.
MRI uses focused radio waves and magnetic fields to detect the presence of hydrogen atoms in tissues in the human body.
MRI scans also reveal the brain’s anatomic structure with 3D imaging allowing doctors to get a clear view of the current state of the organ.
This way, the doctor is able to rule out other health problems like hydrocephalus, hemorrhage, stroke, and tumors that can mimic dementia.
With these scans, physicians can also detect loss of brain mass that relates to different types of dementia.
fMRI records blood flow changes that are linked to the activities of the brain. This may help physicians differentiate dementia types.
Verywellhealth.com also suggests that MRI scans can at times identify reversible cognitive decline.
In such a case, a doctor will recommend appropriate treatment that will reverse this decline and restore cognitive functioning.
Diagnosing And Treating Parkinsons Disease
The diagnosis of Parkinson’s disease is largely based upon the type of symptoms that the patient experiences. When someone has symptoms such as tremors or shaking of arms or legs while at rest, muscle stiffness or slow movements, Parkinson’s disease must be a consideration, particularly if the individual is at a typical age for the onset of the disorder. Not all patients have every symptom, and often the symptoms start on one side of the body and then progress over time to include the other side. A good response to a trial of Parkinson’s disease medication also helps to add confidence to the diagnosis.
The symptoms of Parkinson’s disease can be similar to the symptoms of other conditions, and it is frequently misdiagnosed. Skilled doctors who specialize in the treatment of Parkinson’s disease are the best practitioners to see for an accurate diagnosis.
The diagnostic process begins with a full medical history and neurological exam, testing movement, strength, coordination, balance, and reflexes. A doctor will often order additional tests to make sure that there are no other conditions present that could explain the patient’s symptoms. These tests may include an MRI of the brain and/or spine, or diagnostic tests of the electrical responses of muscles and nerves. In Parkinson’s disease, these are usually normal and are performed to make sure that there are not problems other than Parkinson’s disease that could explain symptoms.
Treatment Options
Brain Mri Advances For Parkinsons Disease
In Parkinson’s disease, the damage to brain cells begins long before any symptoms develop. Therefore, at-risk patients can benefit from early diagnosis, and efforts to slow the progression of the disease can start early.
Researchers are working on newer MRI approaches to precisely detect Parkinson’s disease-related structural and metabolic activity in the brain and correlate it to the function of the organ. For example, scientists from Oxford University used a technique called the resting-state functional MRI to assess the strength of nerve cells in the a region of the brain called the basal ganglia to send and receive information. Because the physical signs of brain cell damage in Parkinson’s disease are not recognizable by conventional MRI, this approach may help visualize the impact of the damage on the activity of brain cells and aid in early diagnosis.
Similarly, MRI is used to identify Parkinson’s disease-specific biomarkers. Tracking the biomarkers using high-field and ultra-high field MRI can identify Parkinson’s disease patients and help follow the progression of the condition.
Although many of these advancements are yet to be implemented in the clinical setting, such adaptations may help better understand the disease and develop new treatments.
***
What Can You Detect With A Parkinsons Mri
Generally, you can receive a Parkinson’s diagnosis in a clinical setting, but an MRI can help to assess various aspects of the disease and its progress. In particular, a Parkinson’s MRI can do the following for patients who have or are suspected to have Parkinson’s disease:
- Evaluate tissue loss and how the brain is atrophying
- Check for changes to the basal ganglia region of the brain
- Find out if there are abnormal iron deposits in the basal ganglia or brainstem
- Look at changes to white matter
- Examine the diffusion of restricted tissues in acute infarction and neurodegenerative diseases
- Help to diagnose atypical parkinsonism
- Exclude treatable causes of parkinsonism such as normal pressure hydrocephalus
What Is Parkinson’s And How Can Mri Help
More than ten million people are living with Parkinson’s disease worldwide, with about one million cases expected to be in the United States by 2020.1 This is more than the number of people with multiple sclerosis, muscular dystrophy and Lou Gehrig’s disease combined.1 With the rising prevalence of Parkinson’s disease, its important to understand the signs and symptoms of the disease. Likewise, physicians and radiology departments may need to know what role magnetic resonance imaging may play.
Tractography And Anatomical Connectivity
Tractography is a technique based on the anisotropy of water diffusion that allows reconstructing fibre tracts in the brain. Tracks are reconstructed by assuming that the main direction of diffusion in a voxel indicates the local orientation of white matter fibres . Using tractography, diffusion measures and connectivity measures can be calculated within the specific fibre tracks. Tractography has also been successfully used to parcel out the SN and the basal ganglia into specific territories .
In PD, reduced connectivity was observed between the SN and ipsilateral putamen and thalamus as well as in the sensorimotor circuit of the basal ganglia . Automated diffusion-based parcellation of SN subregions showed that the SNr and SNc in PD patients showed a general atrophy . Tractography is therefore used to investigate changes in anatomical connectivity in PD patients .
