Understanding How This Dementia Differs From Alzheimer’s Can Help Patients Know What To Expect And Feel Less Fearful
En español | Many symptoms of Parkinson’s disease — shuffling gait, quivering hands, stooped posture — are easy to spot. But this disease can also cause problems that are far less visible but no less distressing. Perhaps the most worrisome is cognitive decline, which affects about 50 percent of patients.
“This is a scary, confusing and concerning topic for a lot of people,” says neurologist Rachel Dolhun, M.D., senior vice president of medical communications at the Michael J. Fox Foundation. While these feelings are natural, common misconceptions can exacerbate patients’ fears.
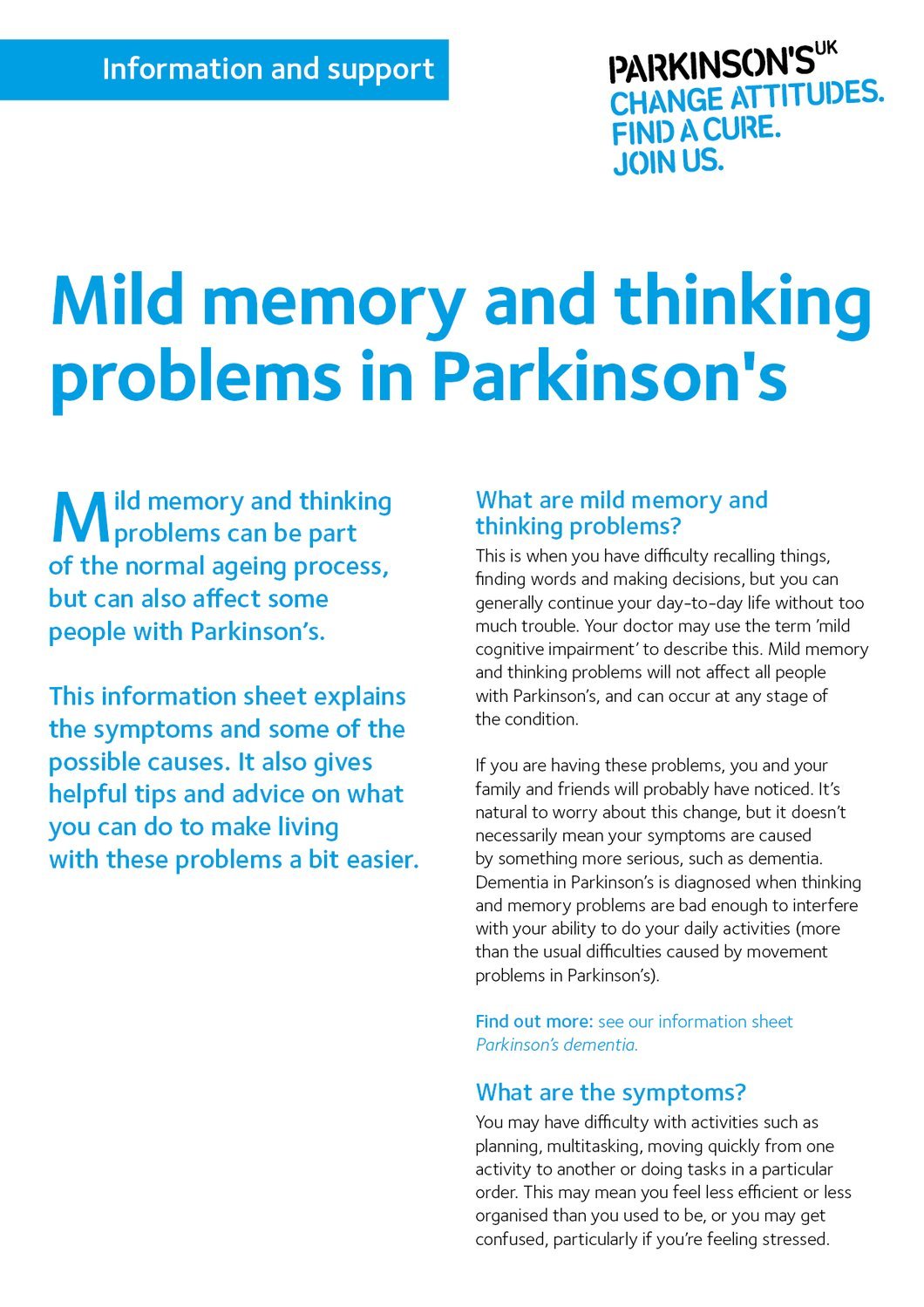
For starters, cognitive decline doesn’t necessarily equal full-blown dementia, and many people with Parkinson’s develop only mild impairment. Another misconception is that even slight memory slippage signals that rapid deterioration is imminent — but that’s far more common with Alzheimer’s disease than it is with Parkinson’s, says Tsao-Wei Liang, M.D., chief of the movement disorders division at Jefferson Health. “It’s not always relentlessly progressive, and more often than not, symptoms can be managed with medication, caregiver support and basic organizational strategies,” he says.
It’s also important to know that many Parkinson’s patients with some cognitive impairments are able to form new short-term memories, even if they struggle with attention and multitasking. “People with Parkinson’s will often remember if you give a clue or prompt them,” Dolhun says.
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Cognitive impairment can occur due to stress, particularly if the patient feels they are a burden to their caregiver, are experiencing a decline in daily functioning, have a worsening quality of life, are dealing with rising medical costs, or are concerned about their mortality.
According to the National Parkinson Foundation, some of the common cognitive issues people living with Parkinson’s disease face include:
- Slowness of thinking
- Struggling to find the right words in conversations
- Declining visual perception
- Lack of reasoning skills
- Declining general intelligence
Some Parkinson’s disease medications can help with areas such as motivation and concentration, but there are no medications that can improve memory function.
MORE:How does Parkinson’s disease affect the brain?
Parkinsons’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Difficulties With Memory And Thinking May Develop In Some People With Parkinson’s
January 7, 2011
Dear Mayo Clinic:
Does Parkinson’s disease affect memory and thinking? My 70-year-old husband has this condition and is showing signs of cognitive impairment.
Answer:Unfortunately, Parkinson’s disease is not simply a problem of tremor, walking and movement. With advancing age, and the longer a person has the disease, difficulties with memory and thinking may surface. Typically, these problems are subtle at first, but may become progressively worse in some people with Parkinson’s disease.
Parkinson’s disease is a disorder of the nervous system that develops gradually over time. The development of cognitive problems reflects the progressive nature of the disease process. Early in the course of the disease, most symptoms — such as tremor, muscle rigidity and difficulty with movement — are usually mild and can often be effectively managed with medications.
After many years of Parkinson’s disease, though, symptoms may become less responsive to medication, and new problems can develop. New symptoms can include additional movement problems and cognitive difficulties, as well as bladder and bowel issues and, in some people, low blood pressure.
Physicians should also review patients’ drug lists, as medications for other health problems may sometimes compromise mental clarity. Finally, adequate sleep is important to sound thinking, and occasionally treating sleep disorders, such as sleep apnea, can improve cognition.
What Are Parkinson’s Disease Dementia Medical Treatment And Medications
There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa; medications known as dopamine agonists that act on the dopamine receptor; and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with Alzheimer’s disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
How Is Parkinsons Disease Dementia Different From Alzheimers Disease
Parkinson’s disease Dementia must not be confused with Alzheimer’s disease. Dementia is a hallmark feature of Alzheimer’s whereas a patient may not necessarily contract Dementia if he happens to contract Parkinson’s. Having mentioned that, Dementia does have a greater social and occupational impact on the functioning of people when it affects someone with Parkinson’s as compared to Alzheimer’s.
This is due to the combination of motor and cognitive impairments. Parkinson’s directly affects problem-solving functions in a person, besides other aspects such as the speed of thinking, memory, and mood. Parkinson’s Dementia Aggression can also be related to Lewy bodies, where sticky clumps of protein are found in the nerve cells of people diagnosed with Parkinson’s.
Finally, it must be known to all those associated with Parkinson’s in any capacity, whether be it a patient or a caregiver, that majority of people with Parkinson’s may experience some of the other forms of cognitive impairment over time. Though cases vary from person to person, the development of Dementia in those diagnosed with Parkinson’s cannot be predicted. To put it in numbers, 30 percent of people with Parkinson’s never develop dementia as a part of their progression.
How Parkinsons And Alzheimers Affect The Body And Brain Differently
Alzheimer’s and Parkinson’s are both neurological illnesses. Both diseases are caused by damaged brain cells. Both conditions can involve dementia, as well as depression, anxiety, and sleep disturbances. Both conditions can lead to psychotic symptoms such as delusions and hallucinations.
While Alzheimer’s and Parkinson’s share certain causes and effects, the two diseases are different. They impact the brain and progress in different ways. Both disorders affect people differently, manifest themselves differently, and progress at different rates.
I had a father with Parkinson’s and a mother with dementia. My experience was that the Parkinson’s progressed at a slower rate and was more motor-related than mental.
My father experienced tremors, as well as changes in his walking and facial expressions. But his cognitive ability was relatively intact up to the very last stages of the disease. My mother’s dementia made her feeble and uncertain on her feet, but she remained active and mobile, even as her cognitive ability declined.
Treatment Modalities For Sexual Dysfunction In Parkinsons Disease
Given the high prevalence of SD in patients with PD, physicians and other healthcare providers should discuss and treat sexual health issues as an integral part of treating the disease. In all instances, drug regimens should be reviewed for possible effects on sexual function. Sexual education, counselling and specific suggestions about therapeutic methods are important, and should be provided by the treating physician.
In a newly diagnosed patient with PD the possible enhancing influence of dopaminergic treatment on sexuality should be discussed with both partners. The improved libido in the male PD patient may be unwelcome, as the elderly spouse has already settled in a situation of not being ‘bothered’. The emergence of hypersexuality in the treated PD patient is, as a rule, drug induced, and modification of treatment is helpful. Profound loss of libido in the well-treated PD patient may call for an endocrinological consultation if it causes distress.
In a newly diagnosed PD patient who present with SD, the dopaminergic drugs should be introduced first, and their effect followed up. Occasionally, the SD will also improve. Difficulties with the motor aspects of the sexual activity may be overcome by counselling and appropriate timing of dopaminergic treatment. Poor lubrication in the female patient with PD may be helped by lubricants; urge incontinence during coitus by previously emptying the bladder and treating the overactive bladder.
Thinking And Memory Problems Associated With Parkinsons Disease
April 29, 2020 —People living with Parkinson’s Disease may be affected by thinking and memory problems. These cognitive issues can have a significant impact on a person’s quality of life and interfere with their daily function.
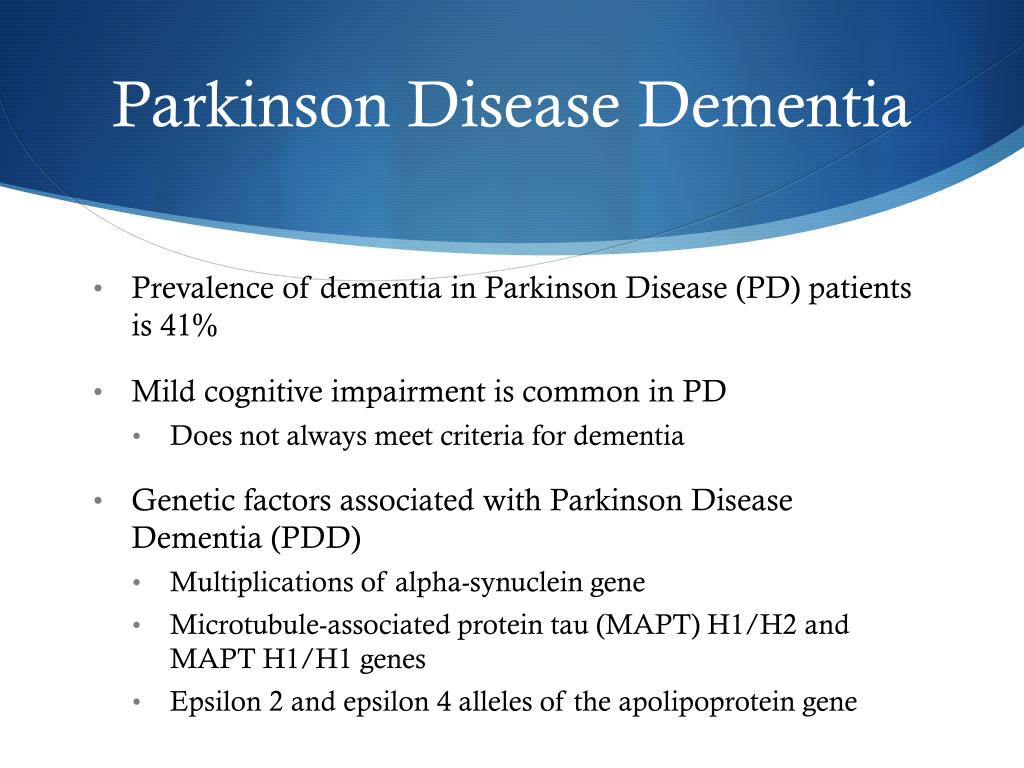
To some degree, cognitive impairment affects many people with PD. The same brain changes that lead to motor symptoms can also result in slowness in memory and thinking. Stress, medication and depression can also contribute to these changes. There are two levels of cognitive impairment.
Parkinsons Disease Linked To Sleep Disorders Sleep Disturbances
Parkinson’s disease has been linked to sleep disorders and sleep disturbances. Parkinson’s disease is characterized by the loss of brain cells that control movement. Symptoms of Parkinson’s disease can include tremors, stiffness, slowness of movements, as well as balance and coordination problems. Memory problems, depression, and sleep problems can all occur in Parkinson’s disease, too.
Sleep problems and sleep disorders may occur as an early sign of Parkinson’s disease, even before motor symptoms have started. Common sleep disorders experienced in Parkinson’s disease include insomnia, excessive daytime sleepiness, nightmares, sleep attacks, REM sleep behavior disorder , periodic leg movement disorder, restless leg syndrome, sleep apnea, and nocturia, which is frequent nighttime urination.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
There’s no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
What Is Needed For A Parkinson’s Disease Dementia Diagnosis
There is no definitive medical test that confirms cognitive decline or dementia in Parkinson’s disease. The most accurate way to measure cognitive decline is through neuropsychological testing.
- The testing involves answering questions and performing tasks that have been carefully designed for this purpose. It is carried out by a specialist in this kind of testing.
- Neuropsychological testing addresses the individual’s appearance, mood, anxiety level, and experience of delusions or hallucinations.
- It assesses cognitive abilities such as memory, attention, orientation to time and place, use of language, and abilities to carry out various tasks and follow instructions.
- Reasoning, abstract thinking, and problem solving are tested.
- Neuropsychological testing gives a more accurate diagnosis of the problems and thus can help in treatment planning.
- The tests are repeated periodically to see how well treatment is working and check for new problems.
Imaging studies: Generally, brain scans such as CT scan and MRI are of little use in diagnosing dementia in people with Parkinson’s disease. Positron emission tomographic scan may help distinguish dementia from depression and similar conditions in Parkinson’s disease.
Parkinsons Disease Brain Vs Normal Brain: Whats Different
It’s not yet possible to spot the difference between a brain with Parkinson’s and a normal, “healthy” brain on an MRI scan. However, since Lewy bodies were first found in the substantia nigra in 1927, doctors have known they are a feature of Parkinson’s disease. The presence of these Lewy bodies is thought to be what separates people with Parkinson’s disease from the general population. However, Lewy bodies can only be diagnosed with certainty during a brain autopsy after death.
The Preponderance Of Injury In The Past Of People With Pd
Complications Related To Parkinson’s Can Affect SurvivalClaudia Chaves, MD
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Parkinson’s is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinson’s disease in the United States. During the six-year period, 64% of the participants with Parkinson’s disease passed away.
The risk of death of those with Parkinson’s was then compared to Medicare beneficiaries who did not have Parkinson’s or any other common diseases, including:
What Are The Surgical Treatments For Parkinsons Disease
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Is The Dementia Caused By Parkinsons Or Something Else
Indications that dementia may be caused by something other than Parkinson’s disease include agitation, delusions , and language difficulties. If the onset of cognitive symptoms is sudden, they’re more likely due to something other than Parkinson’s disease—even reversible causes such as infection, a vitamin B12 deficiency, or an underactive thyroid gland.
Depression can mimic dementia by causing similar symptoms such as apathy, memory problems, and concentration difficulties. Since depression is very common in Parkinson’s patients, it’s important to recognize the signs and symptoms of depression in older adults.
Parkinson’s disease dementia vs. other dementias
Other types of dementia that can be commonly mistaken for Parkinson’s disease dementia include:
Lewy Body Dementia is characterized by fluctuations in alertness and attention, recurrent visual hallucinations, and Parkinsonian motor symptoms like rigidity and the loss of spontaneous movement. In this disorder, cognitive problems such as hallucinations tend to occur much earlier in the course of the disease and often precede difficulties with walking and motor control.
Alzheimer’s disease and Parkinson’s disease are both common in the elderly, especially in those over 85. Patients with Parkinson’s who develop dementia may even develop Alzheimer’s dementia as well. Therefore, it’s important to be aware of the and how it’s treated.
Gastrointestinal Issues In Advanced Parkinsons Disease
Problems with motility of the gut can be a major source of difficulty throughout the disease course and can be particularly problematic in advanced PD as well. . Constipation, which can be one of the earliest symptoms of PD is a very common problem throughout the disease course. Two gut issues that tend to be particularly problematic in people with advanced PD are abdominal pain and fecal incontinence.
Ways To Decrease The Risk Of Parkinsons And Alzheimers
There is currently no “cure” for either disease. Parkinson’s is considered a more treatable condition, however, especially in the early stages of the disease. Treatments include medication, physical therapy, and lifestyle modifications such as dietary changes. Research continues to suggest that a brain-healthy lifestyle can help prevent both Alzheimer’s and Parkinson’s. Here are some basic guidelines:
Drugs And Medication Used To Treat Parkinsons Disease
A number of different drugs can be used to treat Parkinson’s.
Levodopa
Levodopa is the most common treatment for Parkinson’s. It helps to replenish dopamine.
About 75 percent of cases respond to levodopa, but not all symptoms are improved. Levodopa is generally given with carbidopa.
Carbidopa delays the breakdown of levodopa which in turn increases the availability of levodopa at the blood-brain barrier.
Dopamine agonists
Dopamine agonists can imitate the action of dopamine in the brain. They’re less effective than levodopa, but they can be useful as bridge medications when levodopa is less effective.
Drugs in this class include bromocriptine, pramipexole, and ropinirole.
Anticholinergics
Anticholinergics are used to block the parasympathetic nervous system. They can help with rigidity.
Benztropine and trihexyphenidyl are anticholinergics used to treat Parkinson’s.
Amantadine
Amantadine can be used along with carbidopa-levodopa. It’s a glutamate-blocking drug . It offers short-term relief for the involuntary movements that can be a side effect of levodopa.
COMT inhibitors
Catechol O-methyltransferase inhibitors prolong the effect of levodopa. Entacapone and tolcapone are examples of COMT inhibitors.
Tolcapone can cause liver damage. It’s usually saved for people who do not respond to other therapies.
Ectacapone does not cause liver damage.
Stalevo is a drug that combines ectacapone and carbidopa-levodopa in one pill.
MAO-B inhibitors
Early stage
Mid stage
Mid-late stage
What Are The Symptoms Of Parkinson’s Disease Dementia
Cognitive impairment in Parkinson’s disease may range from a single isolated symptom to severe dementia.
- The appearance of a single cognitive symptom does not mean that dementia will develop.
- Cognitive symptoms in Parkinson’s disease usually appear years after physical symptoms are noted.
- Cognitive symptoms early in the disease suggest dementia with Parkinsonian features, a somewhat different condition.
Cognitive symptoms in Parkinson’s disease include the following:
- Loss of decision-making ability
- Loss of short- and long-term memory
- Difficulty putting a sequence of events in correct order
- Problems using complex language and comprehending others’ complex language
Persons with Parkinson’s disease, with or without dementia, may often respond slowly to questions and requests. They may become dependent, fearful, indecisive, and passive. As the disease progresses, many people with Parkinson’s disease may become increasingly dependent on spouses or caregivers.
Major mental disorders are common in Parkinson’s disease. Two or more of these may appear together in the same person.
The combination of depression, dementia, and Parkinson’s disease usually means a faster cognitive decline and more severe disability. Hallucinations, delusions, agitation, and manic states can occur as adverse effects of drug treatment of Parkinson’s disease, this might complicate the diagnosis of Parkinson’s dementia.
ADHD Symptoms in Children?
Parkinson’s Disease Dementia Surgery And Gene Therapy

- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy; there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Slowing Down The Progression Of Parkinsons Disease
We have all heard that keeping active is good for you and has immediate benefits for your health both short-term and long-term. Regular activity reduces the risk of developing some cancers, cardiovascular disease, as well as obesity and the health issues associated with this. What you may not have heard is regular exercise has also shown to slow the progression of Parkinson’s disease.
Parkinson’s disease is a neurodegenerative disease which targets and progressively damages nerve cells in a particular area of the brain over a long period of time. These nerve cells are very important for their role in producing a chemical called Dopamine. Without this chemical, the brain is not able to control normal bodily movement and the typical presentation of Parkinson’s beings to show in the individual. This can range from balance issues, difficulty with memory and smell, as well as the well-known involuntary shaking. The cause of Parkinson’s is still unclear, however, there is thought to be a combination of both genetic and environmental factors.
The link between exercise and reducing Parkinson’s progression is believed to be focused on a particular protein known as the DJ-1 gene. As we all become more and more sedentary in our day-to-day lives, scientists have noticed an increase of a normal neural protein alpha-synuclein, which is important for relaying messages and normal brain function. However, in excessive “clumps” this could potentially be an issue.
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinson’s disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinson’s disease.
The overlap in symptoms between Lewy body dementia and Parkinson’s disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinson’s disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinson’s disease itself isn’t fatal, but complications can be.
Research has shown a median survival rate of about
Fecal Incontinence In Advanced Parkinsons Disease
Fecal incontinence is a very debilitating symptom that can occur in advanced PD and refers to the involuntary release of fecal matter.
Once again, fecal incontinence, especially if it is a new symptom, should be fully evaluated to determine if there is a cause unrelated to PD. Diseases of the gut such as inflammatory bowel disease or compression of the lower spine cord can be the reason.
If related to PD, there are typically two situations to consider. One possibility is that severe constipation with impacted bowel movement allows loose stool from higher up in the gastrointestinal tract to escape around the edges of the obstruction. In this situation, fecal incontinence could be a harbinger of bowel obstruction. Aggressive and continuous treatment of constipation can help avoid this potential scenario.
Fecal incontinence can also be related to nerve dysfunction of the anal sphincter, or the ring of muscle that controls when feces is released. Cognitive dysfunction and mobility issues may further interfere with getting to the bathroom in time. Some treatment options are similar to urinary incontinence including the use of bedside equipment to minimize mobility issues and introduction of pelvic floor exercises to strengthen the musculature that keeps feces in place.
As with urinary incontinence, frequent and rapid exchange of dirtied incontinence products can keep skin intact and prevent infection.
Tips and Takeaways
Dr. Rebecca Gilbert

