The Efficacy And Safety Of Antipsychotic Medications In The Treatment Of Psychosis In Patients With Parkinsons Disease
Nevena Divac
1Department of Pharmacology, Clinical Pharmacology and Toxicology, Faculty of Medicine, University of Belgrade, Dr. Suboti?a Starijeg 1, 11000 Belgrade, Serbia
2Clinic of Psychiatry, Clinical Center of Serbia, Faculty of Medicine, University of Belgrade, Pasterova 2, 11000 Belgrade, Serbia
Abstract
1. Introduction
Parkinson’s disease is a complex neurobehavioral disorder. Among behavioral problems, psychotic symptoms are highly relevant because they significantly affect the quality of life and complicate the treatment of motor symptoms by limiting the use of medications .
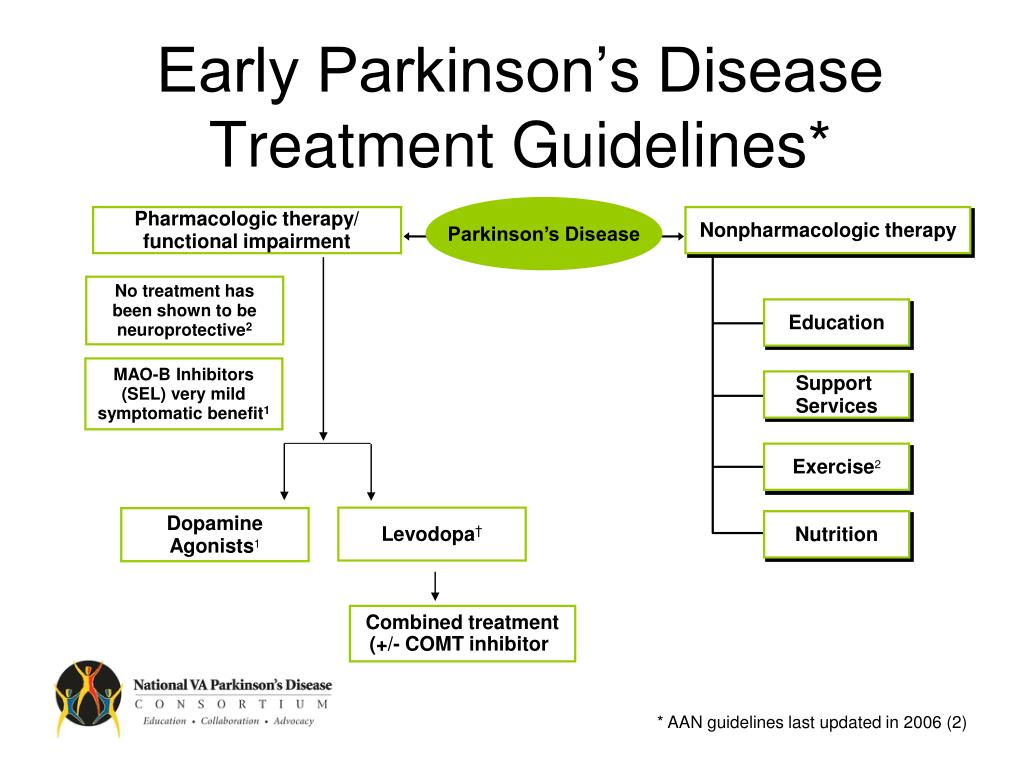
Psychotic symptoms are present in up to 50% of patients with PD, but estimates vary widely . They are usually associated with other correlates such as older age, more advanced age at the onset of the disease, duration of disease, disease staging, cognitive decline, presence of depression, and the use of antiparkinson medication . Psychotic symptoms in PD patients are also associated with increased caregivers’ stress, increased rates of nursing home placement, and poor clinical prognosis . Therefore, psychotic symptoms in patients with PD require treatment. The reduction of antiparkinson medication is usually the first step but is usually ineffective and accompanied with worsened motor symptoms . When reduction of antiparkinson drugs does not improve psychotic symptoms, antipsychotic agents should be considered .
3. Antipsychotic Medications in Patients with PD
5. Conclusion
Competing Interests
What’s Hot In Pd: As A New Drug Gains Fda Approval For Parkinsons Disease Psychosis Should We Fear Using It
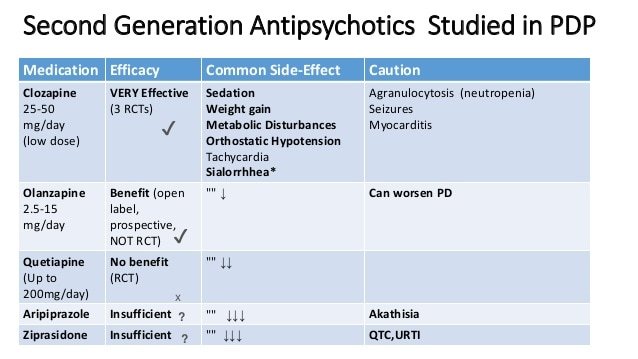
This week the FDA approved the drug Pimavanserin for the treatment of Parkinson’s disease psychosis. There has been a critical, unmet need for development of better drugs to address hallucinations and psychosis in the setting of Parkinson’s disease. We have learned over many years that typical high potency neuroleptic antipsychotic drugs may improve hallucinations but do so at the cost of worsening Parkinson’s disease motor symptoms and are associated with an increased mortality. We have changed our treatment strategy to address hallucinations in Parkinson’s disease by using agents that will not worsen the common motor symptoms . We routinely choose quetiapine or clozapine instead of the classical dopamine blocking drugs. There are, however, shortcomings with these two drugs. Quetiapine has not been shown effective across several randomized Parkinson’s disease clinical trials, but many Parkinson experts believe it is moderately helpful, particularly in the setting of mild hallucinations. Clozapine has been shown to be highly efficacious, but it requires weekly blood monitoring to check for a potentially life-threatening side effect called agranulocytosis; where the drug attacks the bone marrow. The inconvenience and discomfort of blood draws have limited the penetration of this therapy.
Selected References:
Okun, MS. 10 Breakthrough Therapies in Parkinson’s Disease. Books4Patients. 2015 .
Okun, MS. Should We Fear Antipsychotics in Parkinson’s Disease Patients? 2015.
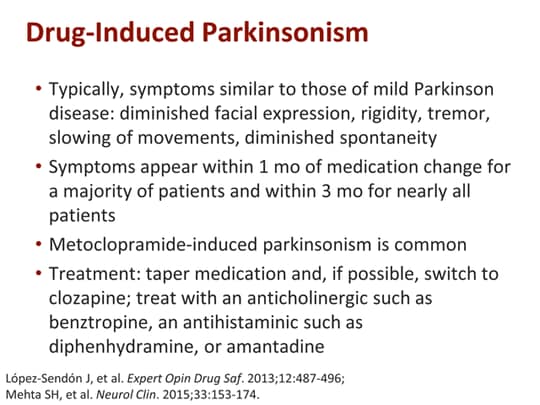
What Is The Difference Between Drug Induced Parkinsons Disease And Typically Occurring Parkinsons Disease
It has been seen that drug-induced Parkinsonism usually occur on both sides of your body while usual Parkinson’s starts from one side of the body. Apart from this, the medication-induced signs generally are seen to go away after the medicine is finished. However, it may take few months to stop, but is does stop eventually. On the contrary, the typically occurring Parkinson’s disease cannot be reversed. Another thing to be kept in mind is that medication-induced Parkinson’s disease is not progressive, unlike the typical Parkinson’s disease.
Interested In Parkinsons Disease Research Register For Our Forums And Join The Conversation
Besides Nuplazid, the team focused on Seroquel, a second-generation antipsychotic , which is often used to treat Parkinson’s psychosis. Results were mixed. Use of Seroquel and other SGAs led to concerns about increased morbidity and mortality in patients with dementia or those with Parkinson’s, prompting an .
Unlike Seroquel, Nuplazid does not affect dopamine receptors, so it does not interfere with the effectiveness of Parkinson’s treatments for motor symptoms.
The team conducted a retrospective analysis of 4,478 UC San Diego Health patients with Parkinson’s, of whom 676 were being prescribed Nuplazid, Seroquel, or both, between April 29, 2016 and April 29, 2018.
Results showed that patients treated with Nuplazid alone had a lower mortality percentage when compared to those treated with quetiapine only , or with both compounds . However, the differences were not statistically significant.
When compared to 784 Parkinson’s patients not on these medications , the results revealed a significantly greater risk of mortality in the Seroquel-only group and a trend toward increased risk in the combination treatment group.
“It’s reasonable to assume, however, that individuals requiring these medications have greater disease severity and are at a higher risk of complications and death,” Nahab noted.
“Our findings provide the largest comparative report of mortality risk in ,” researchers wrote.
This Antidepressant May Be No Better Than Cheaper Alternatives But Demand Could Soon Soar
Nuplazid, if given the FDA go-ahead, would undoubtedly cost far more than existing antipsychotics, which are mostly used to treat schizophrenia and are available as generics. In the pivotal trial behind Acadia’s marketing application, Nuplazid showed only modest improvements over placebo, and was tested in a way that makes it difficult to compare against other treatments.
Physicians involved in the trial stand by the drug, nonetheless.
Dr. Jeffrey Cummings, a neurologist at the Cleveland Clinic Lou Ruvo Center for Brain Health in Las Vegas, said he was struck by some of the patients’ “dramatic” responses.
“Of course, families will also respond to placebos, and that’s why we don’t approve drugs based on anecdotal reports,” said Cummings, who has taken consulting fees from Acadia. “But when families are saying this really made a difference for his life and our lives together, for me it was a pretty impressive study.”
Parkinson’s psychosis usually occurs in the latter stages of the disease, and generally involves nonthreatening visual hallucinations. Cynthia Hatfield, a 72-year-old former banker living in Westerly, R.I., several times a week sees a calico cat resembling one she’d actually owned many years ago, and which her children named “Mushroom.” For years, her hallucinations included a menagerie of small animals.
“Chipmunks and little squirrels and cats, and a little mouse would come out every once in a while,” she said. “I actually enjoy seeing them.”
What Are The Other Forms Of Medicines That Can Cause Parkinsons Disease
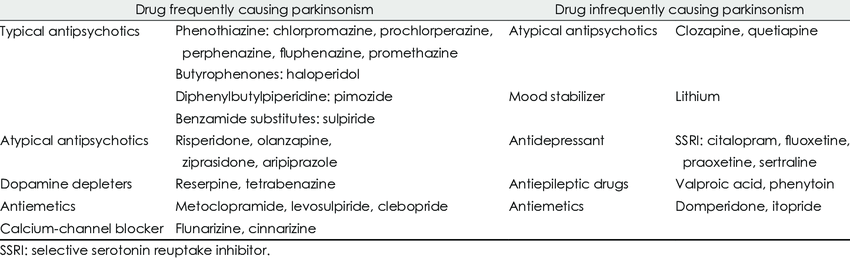
Some of the other common medicines which can cause Parkinson’s disease may include some forms of anti-depressants, anti-nausea drugs, drugs used for the treatment of vertigo, drugs used for epilepsy and anti-arrhythmics. It should be remembered that not all drugs in these classes may cause signs of Parkinsonism. The doctor generally makes the patient aware of the side-effects before prescribing a certain form of drugs. Nevertheless, it is important from the patient’s part to ask about the side-effects of the prescribed medicines.
Study Analyzed Medical Records Of Fifteen Thousand Parkinson’s Patients
- Date:
- University of Pennsylvania School of Medicine
- Summary:
- At least half of Parkinson’s disease patients experience psychosis at some point during the course of their illness, and physicians commonly prescribe antipsychotic drugs, such as quetiapine, to treat the condition. However, a new study suggests that these drugs may do significantly more harm in a subset of patients.
At least half of Parkinson’s disease patients experience psychosis at some point during the course of their illness, and physicians commonly prescribe antipsychotic drugs, such as quetiapine, to treat the condition. However, a new study by researchers at the Perelman School of Medicine at the University of Pennsylvania, the University of Michigan Medical School, and the Philadelphia and Ann Arbor Veterans Affairs Medical Centers and suggests that these drugs may do significantly more harm in a subset of patients. The findings will be published in the March 21, 2016 issue of JAMA Neurology.
The researchers’ analysis of about 15,000 patient records in a VA database found that Parkinson’s patients who began using antipsychotic drugs were more than twice as likely to die during the following six months, compared to a matched set of Parkinson’s patients who did not use such drugs.
“Antipsychotics should be used in these patients only when the psychosis is of clinical significance, and patients probably should not be left on these drugs long-term without re-evaluation,” Weintraub said.
Story Source:
Us Food And Drug Administrationapproved Agents For Pdp: Pimavanserin
Pimavanserin is a 5-HT2A inverse agonist indicated for the treatment of hallucinations and delusions associated with PDP.25 Pimavanserin binds preferentially to the 5-HT2A receptor and, to a lesser extent, to the 5-HT2C receptors, and has low binding affinity to alpha, dopamine D2, histamine, muscarinic, and other serotonin receptors.26 The pharmacologic rationale for the efficacy of pimavanserin in PDP is based on investigations demonstrating that overstimulation of postsynaptic 5-HT neurons contributes to psychotic symptoms in PD. Serotonin 5-HT2A receptors exhibit baseline activity.27,28 In other words, 5-HT2A receptors spontaneously signal to produce and regulate cellular postsynaptic activity. Pimavanserin binds to 5-HT2A receptors and blocks the receptor and reduces the spontaneous baseline activity.28 This property of binding to the receptor and reducing spontaneous baseline activity is referred to as inverse agonism.
The US Food and Drug Administration–approved labels for pimavanserin and all antipsychotics contain a boxed warning stating elderly patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death.31 However, it is important to note that if the psychotic symptoms are related to the underlying PD, pimavanserin can be used in patients with concurrent dementia.
A Critical Reappraisal Of The Worst Drugs In Parkinsons Disease
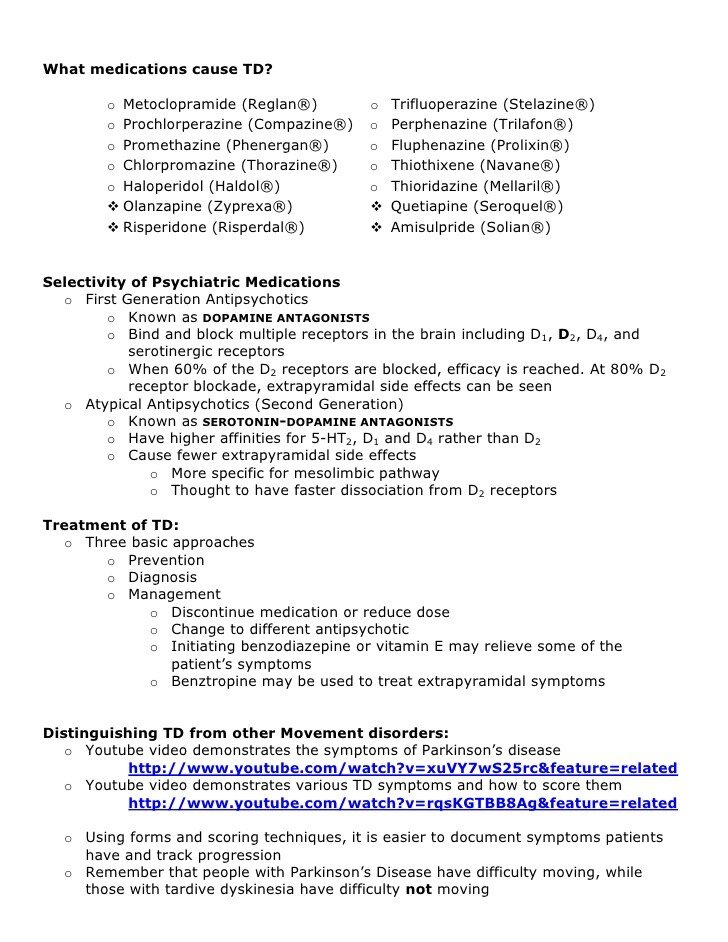
What are the worst drugs for Parkinson’s disease patients? Couldn’t a simple list be assembled and disseminated to the Parkinson community? Recently Ed Steinmetz, an experienced neurologist in Ft. Meyers, FL pointed out to me, a list approach published in the Public Citizen Newsletter . The approach was to list every drug associated with a single confirmed or unconfirmed symptom of Parkinson’s disease or parkinsonism. Parkinson’s disease is defined as a neurodegenerative syndrome , whereas parkinsonism encompasses a wider net of drug induced and other potential causes. In parkinsonism symptoms are similar to Parkinson’s disease, but patients do not have Parkinson’s disease. Patients and family members confronted with a simple “drug list” approach may falsely conclude that most medicines are bad for Parkinson’s disease, and that any medicine may cause parkinsonism. This concept is in general, incorrect. Although the approach is well-meaning, it is in need of a major revision, as Parkinson’s disease and parkinsonism are too complex to summarize by simple lists. In this month’s column I will try to summarize the key information that patients and family members need to know about the “worst pills,” for Parkinson’s disease and parkinsonism.
A Florida Parkinson’s Treatment Blog by Michael S. Okun, M.D.
UF Center for Movement Disorders & Neurorestoration, Gainesville FL
How Commonly Do Parkinsons Disease Patients Develop Psychosis
Psychosis in Parkinson’s disease generally comes in two forms: hallucinations or delusions . When hallucinations occur, they are mostly visual . Sometimes, they can be threatening, but this is less common. Auditory hallucinations are rare in Parkinson’s disease and if they do occur, they are usually accompanied by visual hallucinations.
Delusions are usually of a common theme, typically of spousal infidelity. Other themes are often paranoid in nature Because they are paranoid in nature, they can be more threatening and more immediate action is often necessary, compared to visual hallucinations . It is not uncommon that patients actually call 9-1-1 or the police to report a burglary or a plot to hurt them.
Unfortunately, psychosis occurs in up to 40% of Parkinson’s disease patients . In the early stage of Parkinson’s disease psychosis, the patient often still has a clear understanding and retains their insight, but this tends to worsen over time and insight may eventually be lost. At later stages, patients may be confused and have impaired reality testing; that is, they are unable to distinguish personal, subjective experiences from the reality of the external world. Psychosis in Parkinson’s disease patients frequently occurs initially in the evening, then later on spills into the rest of the day.
Fda Warning: Increased Risk Of Death In Adults With Dementia
This drug has a . This is the most serious warning from the Food and Drug Administration . A boxed warning alerts doctors and patients about drug effects that may be dangerous.
Older adults with psychosis related to dementia may have a higher risk for death when taking antipsychotic drugs such as Nuplazid. This drug should not be used in people with dementia-related psychosis that’s not related to Parkinson’s disease psychosis.
Antipsychotic Use In Patients With Dementia With Lewy Bodies
Am Fam Physician. 2017 Nov 15;96:629.
Original Article: Behavioral Disorders in Dementia: Appropriate Nondrug Interventions and Antipsychotic Use
Issue Date: August 15, 2016
See additional reader comments at: https://www.aafp.org/afp/2016/0815/p276.html
to the editor: We read with interest the review of interventions for behavioral disorders in dementia. It reviewed the evidence for behavioral interventions and recommended judicious use of antipsychotics in cases when the benefit would be great and safer tactics have already failed. However, dementia is a collective term for a set of behaviors that can arise from many different biological causes. Medications appropriate for treating Alzheimer disease, the most common and best-studied dementia, may be harmful in dementias with other etiologies. Antipsychotic use may be warranted after failure of behavioral interventions in many types of dementia, but it can cause significant problems in others.
Dementia with Lewy bodies is the second most common etiology of dementia,1 and it is becoming more common. Its three core symptoms are fluctuating level of consciousness, parkinsonian movement symptoms, and fully formed visual hallucinations. Dementia with Lewy bodies shares dopamine dysfunction with Parkinson disease. Symptoms of these two diseases commonly co-occur, with the primary diagnosis depending on which set of symptoms presented first.
Read the full article.
Who Are At Risk Of Developing Drug Included Parkinsonism
Some patients may be at a higher risk of developing medication-induced Parkinson
ism than others. Some of the risks include-
Women: Women are seen to be two times as much at risk of having drug inducing Parkinson’s disease than men.
AIDS Patients: People with AIDS are at a higher risk.
Family History: Patients having a family history Parkinson’s disease are at a higher risk of having drug induced Parkinsonism.
Elderly: Since elder people are usually on multiple medicines, they are at risk of having drug induced Parkinsonism.
How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue with someone who is experiencing a hallucination or delusion. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Chauncey Spears, Movement Disorders Fellow at the University of Florida, a Parkinson’s Foundation Center of Excellence.
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication you’re taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldn’t be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Medications To Help Treat Parkinsons Disease Psychosis
Your doctor might consider prescribing an antipsychotic drug if reducing your PD medication doesn’t help manage this side effect.
Antipsychotic drugs should be used with extreme caution in people with PD. They may cause serious side effects and can even make hallucinations and delusions worse.
Common antipsychotic drugs like olanzapine might improve hallucinations, but they often result in worsening PD motor symptoms.
Clozapine and quetiapine are two other antipsychotic drugs that doctors often prescribe at low doses to treat PD psychosis. However, there are concerns about their safety and effectiveness.
In 2016, the approved the first medication specifically for use in PD psychosis: pimavanserin .
In clinical studies , pimavanserin was shown to decrease the frequency and severity of hallucinations and delusions without worsening the primary motor symptoms of PD.
The medication shouldn’t be used in people with dementia-related psychosis due to an increased risk of death.
Psychosis symptoms caused by delirium may improve once the underlying condition is treated.
There are several reasons someone with PD might experience delusions or hallucinations.
Antipsychotics Used For Parkinson’s Despite Warnings
Doctors Still Prescribe Antipsychotics Despite Risks for Some Parkinson’s Patients
July 11, 2011 — Doctors continue to prescribe antipsychotic drugs to their patients with Parkinson’s disease and psychosis, despite “black box” warnings from the FDA linking them to increased risk of death among patients with dementia, a study shows.
A black box warning is the strongest drug warning issued by the FDA.
“My sense is that the black box warnings don’t factor into decision making,” says study researcher Daniel Weintraub, MD, an associate professor of psychiatry at the University of Pennsylvania.
The study is published in the Archives of Neurology.
The black box warning for antipsychotics says the drugs are associated with an increased risk of death for those with dementia, which is common among people diagnosed with Parkinson’s. Some commonly prescribed antipsychotics also worsen symptoms of Parkinson’s.
Risperdal and Zyprexa , for example, are two such drugs, and neither has been shown to be very effective. Yet according to the study, nearly 30% of patients with Parkinson’s and psychosis take them.
Clozaril , the only drug known to be both effective and well-tolerated for treating psychosis in Parkinson’s patients, is prescribed to less than 2% of those with the disease.
“Quetiapine is the No. 1 choice without clear evidence that it’s effective,” says Weintraub.
Quetiapine Improves Symptoms Of Parkinson’s Disease
March 02, 2001
New York Mar 2 — In patients with Parkinson’s disease and psychosis who failed treatment with other atypical antipsychotic agents, quetiapine improved both cognitive and psychotic symptoms. These results from a 6-month, open-label study were presented this week at the American Association for Geriatric Psychiatry meeting in San Francisco, California. Seroquel is indicated for the treatment of schizophrenia.
The single-center study examined the safety, tolerability, efficacy, and cognitive effects of quetiapine in 29 patients with psychosis associated with Parkinson’s disease who had failed treatment with clozapine, risperidone, or olanzapine due to lack of efficacy, intolerable adverse effects, or noncompliance with blood monitoring. Patients received up to 400 mg/day of quetiapine, which was dosed according to clinical response and tolerability for up to 6 months.
Psychiatric assessments included the Brief Psychiatric Rating Scale , the Clinical Global Impressions Severity of Illness item, the Neuropsychiatric Inventory sum of delusions and hallucinations , and the Unified Parkinson’s Disease Rating Scale mental subscale and a modified Hoehn and Yahr assessment. Assessments for Parkinson’s disease symptoms included the remaining UPDRS subscales.
Three patients withdrew from the study due to adverse events.
Identifying Psychosis Diagnosis And Antipsychotics
The purpose of this study was to identify the incidence of new cases of antipsychotic use to treat psychosis in the first year after PD diagnosis. To be considered an antipsychotic user, first, a patient was required to have a new Read Code of psychosis diagnosis that appeared in the data after the diagnosis of PD diagnosis. Additionally, the Read Code for antipsychotics must have appeared after the diagnosis of psychosis and within the first year after PD diagnosis. Appendix 2 lists drugs considered antipsychotics and their drug classes .
Will Nuplazid Cure My Parkinsons Disease Psychosis
No, Nuplazid won’t cure your Parkinson’s disease psychosis. There is currently no cure for this condition. However, it can help decrease hallucinations and delusions that may be caused by Parkinson’s disease psychosis.
Talk with your doctor if you have questions about how Nuplazid works to treat your condition.
Quetiapine For Psychosis In Parkinsons Disease
Quetiapine for Psychosis inParkinson’s Disease
Abstract & Commentary
Visual hallucinations and delusions are common in patients with moderate to advanced Parkinson’s disease . Typically fleeting images of people, children, or animals are easily ignored; however, hallucinations often become more intense and frequent, with loss of insight. Fixed delusions, in which patients may become fearful, paranoid or even frankly psychotic, are especially problematic. Levodopa and dopamine agonists fuel hallucinations and delusions, and the treating neurologist is often faced with the difficult choice of lowering dopaminergic medications in an attempt to control hallucinations at the expense of impaired motor performance.
Fortunately, atypical neuroleptics offer an attractive option to control hallucinations in PD patients without worsening rigidity or stiffness. Recent studies have evaluated risperidone and olanzapine in hallucinating PD patients, with disappointing results—both agents reliably worsen parkinsonian symptoms and should be avoided in PD patients. Clozapine, the gold-standard atypical neuroleptic, controls hallucinations without worsening motor performance; however, the inconvenience of weekly blood tests to monitor for agranulocytosis and side effects of sedation or hypersalivation often limit the drug’s use.
Dr. Frucht, Assistant Professor of Neurology, Movement Disorders Division, Columbia-Presbyterian Medical Center, is Assistant Editor of Neurology Alert.
What Triggers Psychosis In Parkinsons Disease
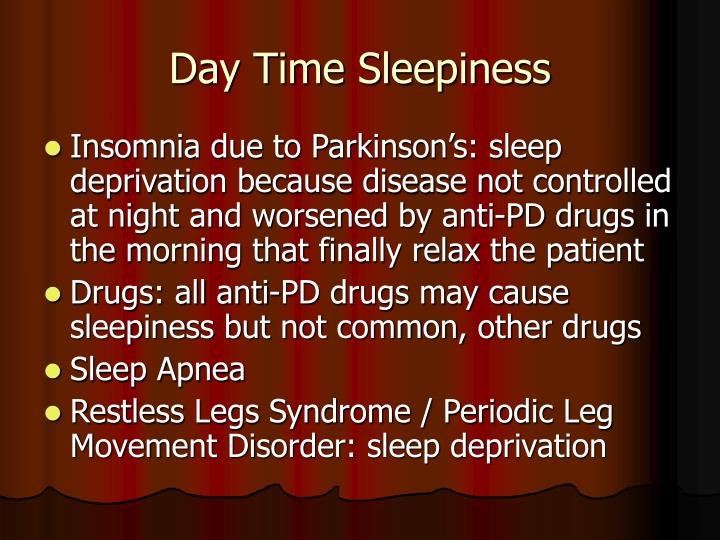
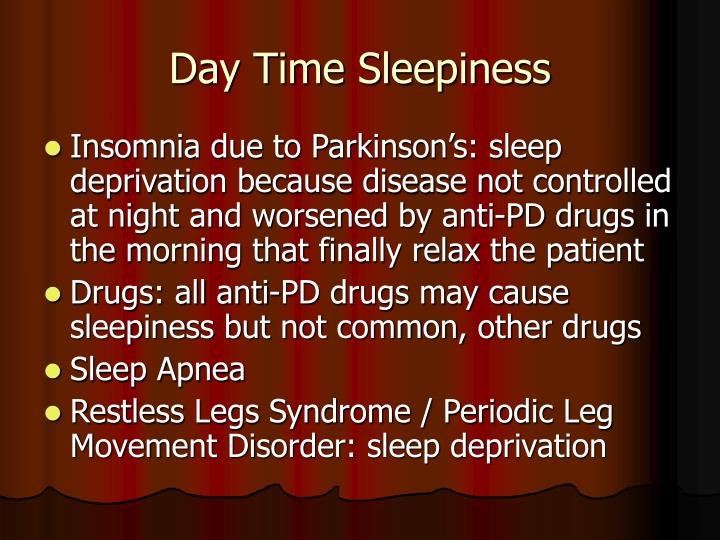
Psychosis in Parkinson’s disease is believed to be due to long term use of parkinsonian medications especially dopaminergic and anticholinergic drugs . However, significant medication exposure is no longer a pre-requisite in Parkinson’s disease psychosis . The “continuum hypothesis” states that medication-induced psychiatric symptoms in Parkinson’s disease starts with sleep disturbances accompanied by vivid dreams, and then develops into hallucinations and delusions, and ends in delirium. However this theory is now being challenged .
What To Do In Case You Take Too Much Nuplazid
If you think you’ve taken too much of this drug, call your doctor. You can also call the American Association of Poison Control Centers at 800-222-1222 or use their online tool. But if your symptoms are severe, call 911 or your local emergency number, or go to the nearest emergency room right away.
When you get Nuplazid from the pharmacy, the pharmacist will add an expiration date to the label on the bottle. This date is typically 1 year from the date they dispensed the medication.
The expiration date helps guarantee that the medication is effective during this time. The of the Food and Drug Administration is to avoid using expired medications. If you have unused medication that has gone past the expiration date, talk to your pharmacist about whether you might still be able to use it.
Diagnosis Of Dip And The Role Of Dat Imaging
The clinical diagnostic criteria for DIP are defined as 1) the presence of parkinsonism, 2) no history of parkinsonism before the use of the offending drug, and 3) onset of parkinsonian symptoms during use of the offending drug. Since asymmetrical rest tremors are common in many DIP patients and symptoms persist or progress after cessation of the offending drug, patients clinically diagnosed with DIP may include individuals in the preclinical stage of PD whose symptoms were unmasked by the drug.15,41,58,59
DATs are presynaptic proteins in the membrane on terminals of dopaminergic neurons. They take up dopamine from the synaptic cleft projections that extend from the substantia nigra to the striatum. These transporters control dopaminergic transmission by spatial and temporal buffering, rendering the molecule an imaging target in diseases affecting the dopaminergic nigrostriatal pathway. Single-photon-emission computed tomography and positron-emission tomography scans are available using several DAT ligands.6,60 SPECT radioligands include 123I-N-3-fluoropropyl-2?-carbomethoxy-3?-nortropane , 123I-ioflupane, DaTSCAN, and 123I-2?-carbomethoxy-3?-tropane .61 PET scans may be superior to SPECT for imaging DATs, in that the lower energy of positrons provides higher resolution, resulting in better image quality with widespread clinical applications.60 However, most DAT imaging studies, including those in patients with DIP, have utilized SPECT.53,62–64
Management Of Psychosis In Parkinson Disease
Sam Adler, MDPsychiatric Times
For some patients with Parkinson disease, the neuropsychiatric complications are a greater source of morbidity than the motor dysfunction. This article focuses on the management of psychosis in Parkinson disease.
The diagnosis of Parkinson disease is based on the observation of a constellation of motor abnormalities and the exclusion of other secondary causes of parkinsonism. The disease is classified as a “movement disorder,” but for many patients with PD the motor problems are only the tip of the iceberg. A host of neuropsychiatric disorders are intrinsic to PD or occur as a complication of the dopaminergic therapies or anticholinergic medications used to treat the motor symptoms . For some patients with PD, the neuropsychiatric complications are a greater source of morbidity than the motor dysfunction.1,2
The neuropsychiatric disorders associated with dopaminergic therapies are important to recognize, because they are at least partially iatrogenic and can often be successfully managed by adjustment of the patient’s PD medications. This article focuses on the management of psychosis in PD-a problem with significant morbidity. Psychosis in PD and Parkinson-related disorders is an independent predictor for the need for institutionalization and increased mortality.
Susceptibility to psychosis
Pros and cons of pharmacological treatment
Fluctuating motor symptom responses
CASE VIGNETTE
Neuroleptics
CASE VIGNETTE
Disclosures:
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinson’s report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include “delirium,” in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and “isolated minor symptoms” or “minor hallucinations,” including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinson’s. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinson’s not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinson’s is a complex disease and as it progresses the percentages and risk of symptoms will change.
Can Drug Induced Parkinsonism Be Prevented
Although there is no surety in the prevention of drug-induced parkinson’s disease, but efforts may be made to check the dosage of drugs so prescribed-
Be Cautious with Antipsychotics: The patient or in some cases the caregiver should make sure that antipsychotic drugs are given at their least effective dosage.
Inform the Doctor: The doctor should be informed well before in case the patient already has symptoms of Parkinson’s disease so that they do not appear to get worse with the starting of some prescribed drugs.
Abrupt Stoppage of Medicine: It is never a wise decision to stop taking a medicine by oneself. It is important to talk to the doctor in case of any concerns.
Will Nuplazid Make My Hallucinations Worse
It’s not likely that Nuplazid will worsen your hallucinations, but it can happen. In clinical trials:
- 5% of people taking Nuplazid experienced hallucinations
- 3% of people taking a placebo experienced hallucinations
It’s not known whether people’s hallucinations got worse during clinical trials, or if their treatment wasn’t effective at reducing hallucinations they were already experiencing.
If you notice that your hallucinations are getting worse while taking Nuplazid, talk with your doctor. They may be able to determine if the hallucinations are a side effect of Nuplazid.
Does Nuplazid Cause Any Heart Side Effects
Nuplazid may cause heart side effects, such as an irregular heart rhythm called QT prolongation. However, in most cases QT prolongation only occurs if you’re taking another drug that also affects your heart rhythm. Or this could also occur if you have a condition that causes an irregular heart rhythm.
For more information on which medications to avoid while you’re taking Nuplazid, see the “Nuplazid interactions” section below. To learn about prolonged QT interval, which could cause QT prolongation during your Nuplazid treatment, see the “Nuplazid precautions” section below.
Treatment Of Parkinsons Disease Psychosis
Andrew Schleisman, PharmD Candidate 2017
Mikayla Spangler, PharmD, BCPSAssociate Professor of Pharmacy Practice
Emily Knezevich, PharmD, BCPS, CDEAssociate Professor of Pharmacy PracticeCreighton University School of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2016;41:HS20-HS26.
ABSTRACT: Delusions and hallucinations in patients with Parkinson’s disease, a condition known as Parkinson’s disease psychosis , have historically been treated with clozapine and quetiapine because of their relatively low likelihood of worsening motor symptoms. Although clozapine is considered the drug of choice, it is underused in this population because of the need for frequent monitoring. Quetiapine, on the other hand, is generally first-line treatment despite its questionable efficacy. Consequently, in 2006, the American Academy of Neurology identified a need for the development of a novel antipsychotic with evidence of both safety and efficacy in patients with PDP. Pimavanserin, which has shown promise in clinical trials, recently became the first agent to receive FDA approval for the treatment of PDP.
Nuplazid For Parkinsons Disease Psychosis
Nuplazid is FDA-approved to treat hallucinations and delusions related to Parkinson’s disease psychosis. A hallucination is seeing or hearing something that isn’t really there. A delusion is believing something that isn’t true, and such beliefs may often be unrealistic.
Parkinson’s disease is a condition that affects your nervous system. It’s a progressive disease, which means that it gets worse over time. More common symptoms can include tremors , slow movements, and stiff muscles.
Some people with Parkinson’s disease may also experience psychosis . It’s the hallucinations or delusions caused by this psychosis that Nuplazid is used to treat.
Effectiveness for Parkinson’s disease psychosis
Nuplazid has been shown to be effective for treating hallucinations or delusions that are related to Parkinson’s disease psychosis.
In clinical trials, the effectiveness of Nuplazid was measured using a test called the Scale for the Assessment of Positive Symptoms of Parkinson’s Disease . This scale goes from 0 to 45, and a higher score means more severe symptoms.
In clinical trials:
- people taking Nuplazid had their SAPS-PD scores decrease by 5.79 points
- people taking a placebo had their SAPS-PD scores decrease by 2.73 points
