Join The Parkinsons Forums: An Online Community For People With Parkinsons Disease And Their Caregivers
Chronic pain between the two groups was assessed using the Brief Pain Inventory , which measures pain severity , pain interference and pain frequency. A qualitative description of pain was also conducted.
Patients described pain as “exhausting,”“tiring,”“penetrating,”“miserable” and “unbearable” significantly more often than controls.
Among patients, those with depressive symptoms — as evidenced by a score of eight or higher in the Hospital Anxiety and Depression Scale — reported pain as tender more frequently than those without depression. Controls with depressive symptoms were more likely to report pain as stabbing, tender and tiring compared to those without evidence of depression.
“These descriptions indicate a significant impact of pain on the psychological well-being of the patient,” the researchers wrote.
Subsequent analysis showed that patients overall scored higher than controls in “worst pain felt since last week” and in global pain severity. Among all participants with depressive symptoms, those with Parkinson’s had higher scores of worst pain felt and average pain felt since last week, as well as higher reported pain levels at the time of assessment and global pain severity than those in the control group.
Symptoms of depression led to similar differences – plus an additional higher impact on social relations – between patients and controls. Of note, depression was associated with greater difficulties in walking in the group without Parkinson’s.
What Is The Trend Over Time In The Prevalence And Incidence Of Parkinsonism In Canada
Between 2004?2005 and 2013?2014, the number of Canadians living with diagnosed parkinsonism increased from approximately 61,000 to 84,000, while the number of Canadians newly diagnosed increased from approximately 8,000 to 10,000. However, during the same period, there was no significant change in the age-standardized prevalence proportion, which remained at 0.4%, or the incidence rate, which went from 51.6 per 100,000 to 52.6 per 100,000. The sex differential also remained constant over time for both indicators .
Figure 3: Age-standardized prevalence and incidence of diagnosed parkinsonism, including Parkinson’s disease, among Canadians aged 40 years and older, by sex, 2004?2005 to 2013?2014
| Indicator | |
|---|---|
| 67.8 | 40.3 |
Notes: Age-standardized estimates to the 2011 Canadian population. The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. The 95% confidence intervals of the prevalence estimates are too small to be illustrated.Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
How Many Canadians Live With Parkinsonism And How Many Are Newly Diagnosed Each Year
Based on the latest estimates available , in 2013?2014, approximately 84,000 Canadians aged 40 years and older were living with diagnosed parkinsonism and 10,000 Canadians were newly diagnosed with this condition . The age-standardized prevalence was 1.5Footnote i times higher among males than among females , and similarly the age-standardized incidence was 1.7Footnote i times higher among males than females . The epidemiological burden of parkinsonism increases with age. In 2013?2014, when comparing estimates among Canadians aged 85 years and older vs. those aged 40-44 years, the prevalence of the condition was 169Footnote i times higher in the older age group , while the incidence was 48Footnote i times higher in the older age group .
Figure 1: Prevalence of diagnosed parkinsonism, including Parkinson’s disease, by sex and age group, Canada, 2013?2014
| Age group |
|---|
| 44.7 | 55.1 |
Note: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
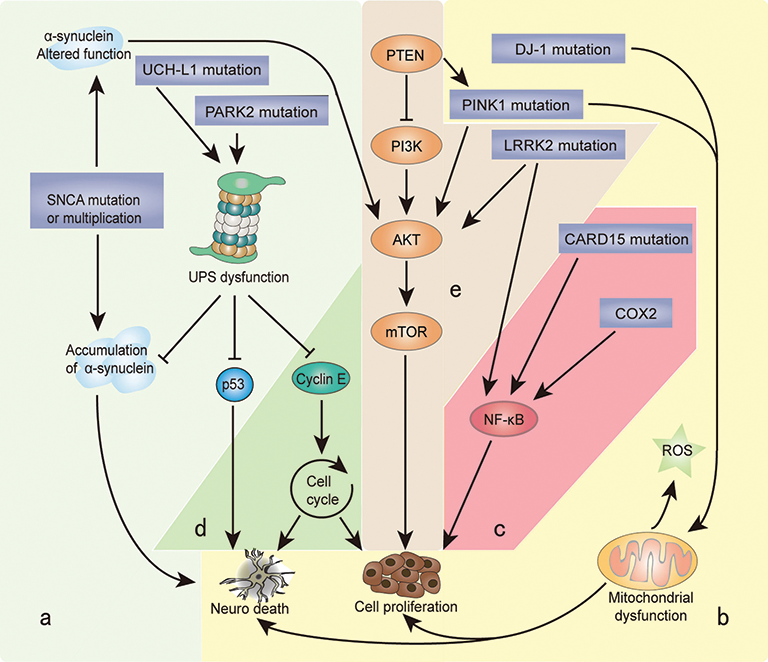
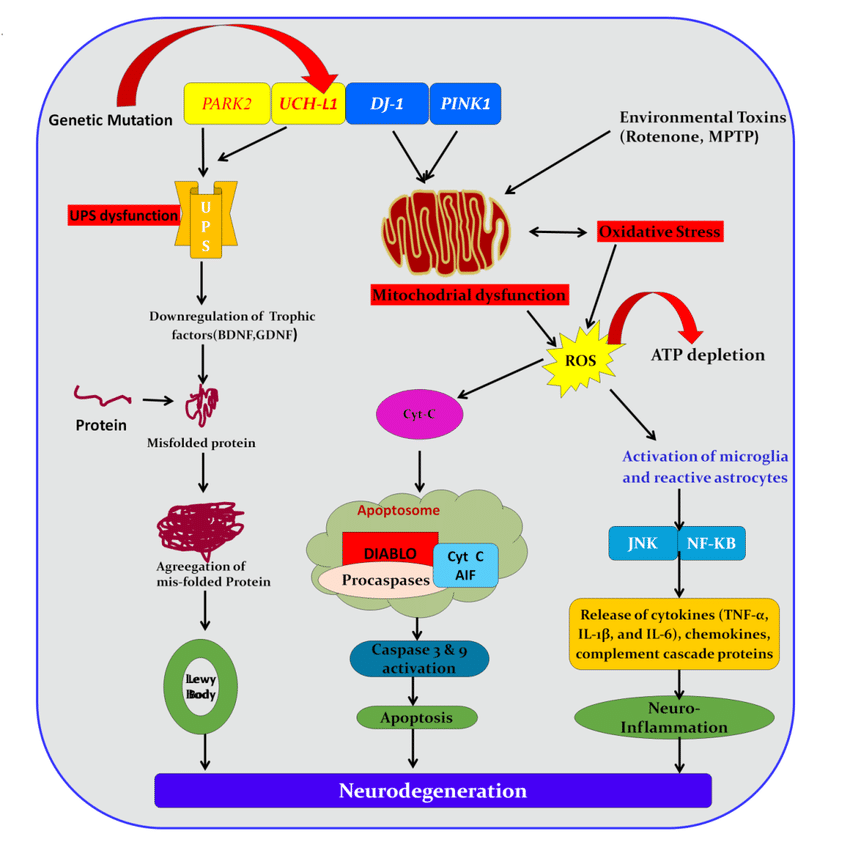
Sidebar: Morris K Udall Centers Of Excellence For Parkinson’s Disease Research
The Morris K. Udall Parkinson’s Disease Research Act of 1997 authorized the NIH to greatly accelerate and expand PD research efforts by launching the NINDS Udall Centers of Excellence, a network of research centers that provide a collaborative, interdisciplinary framework for PD research. Udall Center investigators, along with many other researchers funded by the NIH, have made substantial progress in understanding PD, including identifying disease-associated genes; investigating the neurobiological mechanisms that contribute to PD, developing and improving PD research models, and discovering and testing potential therapeutic targets for developing novel treatment strategies.
The Udall Centers continue to conduct critical basic, translational, and clinical research on PD including: 1) identifying and characterizing candidate and disease-associated genes, 2) examining neurobiological mechanisms underlying the disease, and 3) developing and testing potential therapies. As part of the program, Udall Center investigators work with local communities of patients and caregivers to identify the challenges of living with PD and to translate scientific discoveries into patient care. The Centers also train the next generation of physicians and scientists who will advance our knowledge of and treatments for PD. See the full list of Udall Centers.
What Are The Management Options For Canadians Living With Parkinsonism
There is currently no cure for Parkinson’s disease and most other parkinsonism cases. However, treatment options are available to help mitigate the symptoms and health impacts associated with these conditions. Most often the primary treatment is pharmacological, but it may also include other therapeutic options and, in the case of Parkinson’s disease, surgical interventions. Studies have shown that specially tailored exercise programs, supervised by physiotherapists or other trained professionals, may help affected individuals maintain or improve their physical functionality and general well-being.Footnote 2 Footnote 3 Footnote 4 Footnote 5
Box 1: What’s in the data?
The data used in this publication are from the Canadian Chronic Disease Surveillance System , a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries.
Definition of diagnosed parkinsonism, including Parkinson’s disease, in the CCDSS
Parkinsons & Restless Leg Syndrome: Using Dopaminergic Medication
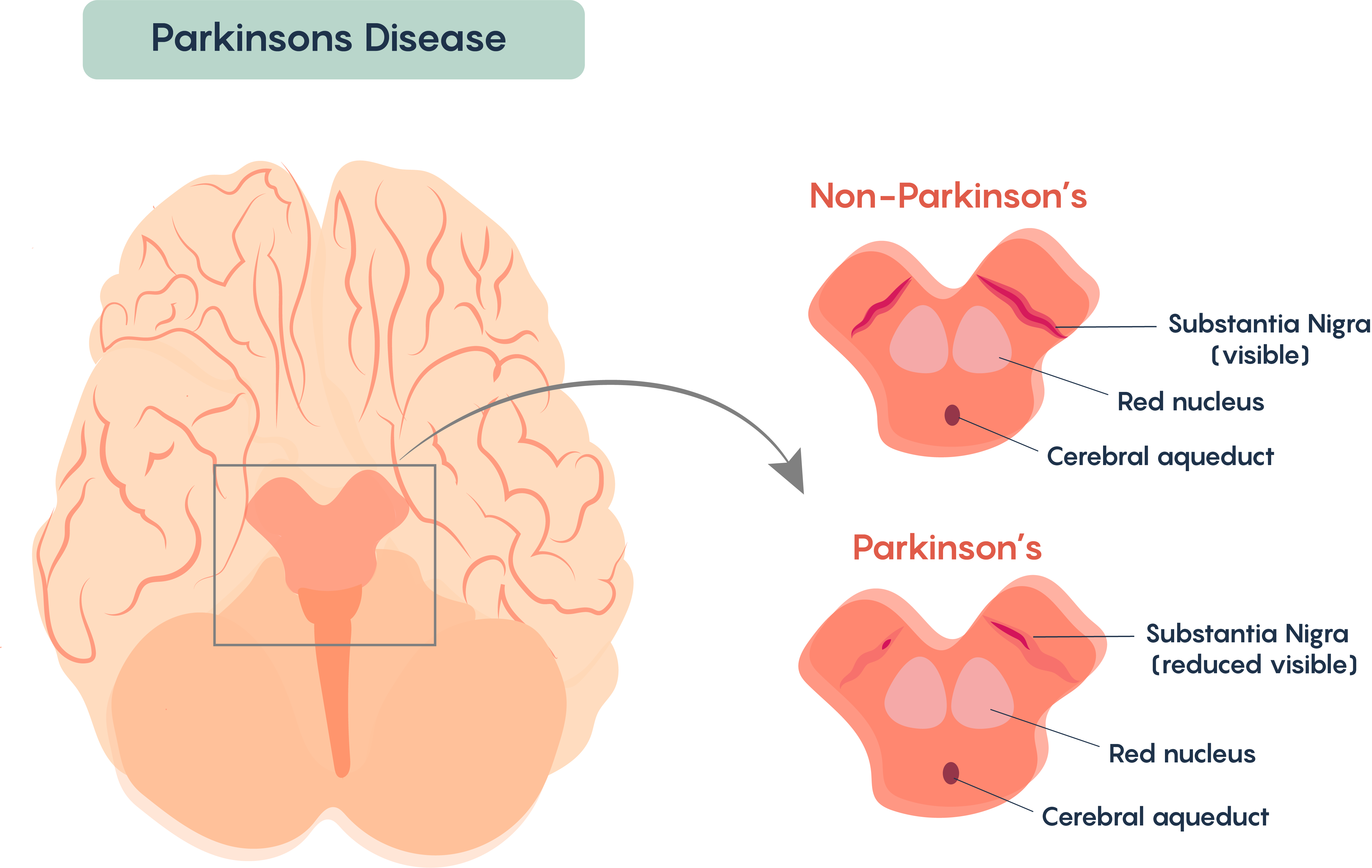
Because RLS is well-treated by medications that also treat PD, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in PD, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that DaTscan results are not abnormal in RLS.
Using dopaminergic medications to treat RLS however can be tricky. In some people they can lead to a phenomenon known as augmentation, in which long term use of dopaminergic medications can worsen the symptoms – making them appear earlier in the day or migrating to the upper body in addition to the legs.
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
Highlights From The Canadian Chronic Disease Surveillance System
Parkinsonism, including Parkinson’s disease, can have significant impacts for those affected, their caregivers, and society. With a growing and aging population, it is estimated that the number of Canadians living with parkinsonism will double between 2011 and 2031 and that the incidence will increase by 50%.Footnote 1
The Public Health Agency of Canada , in collaboration with all Canadian provinces and territories, conducts national surveillance of parkinsonism to support the planning and evaluation of related policies, programs, and services. This fact sheet presents an overview of the data on diagnosed parkinsonism, including Parkinson’s disease, from the Canadian Chronic Disease Surveillance System .
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
What Is It And How Does It Affect Those Whove Been Diagnosed
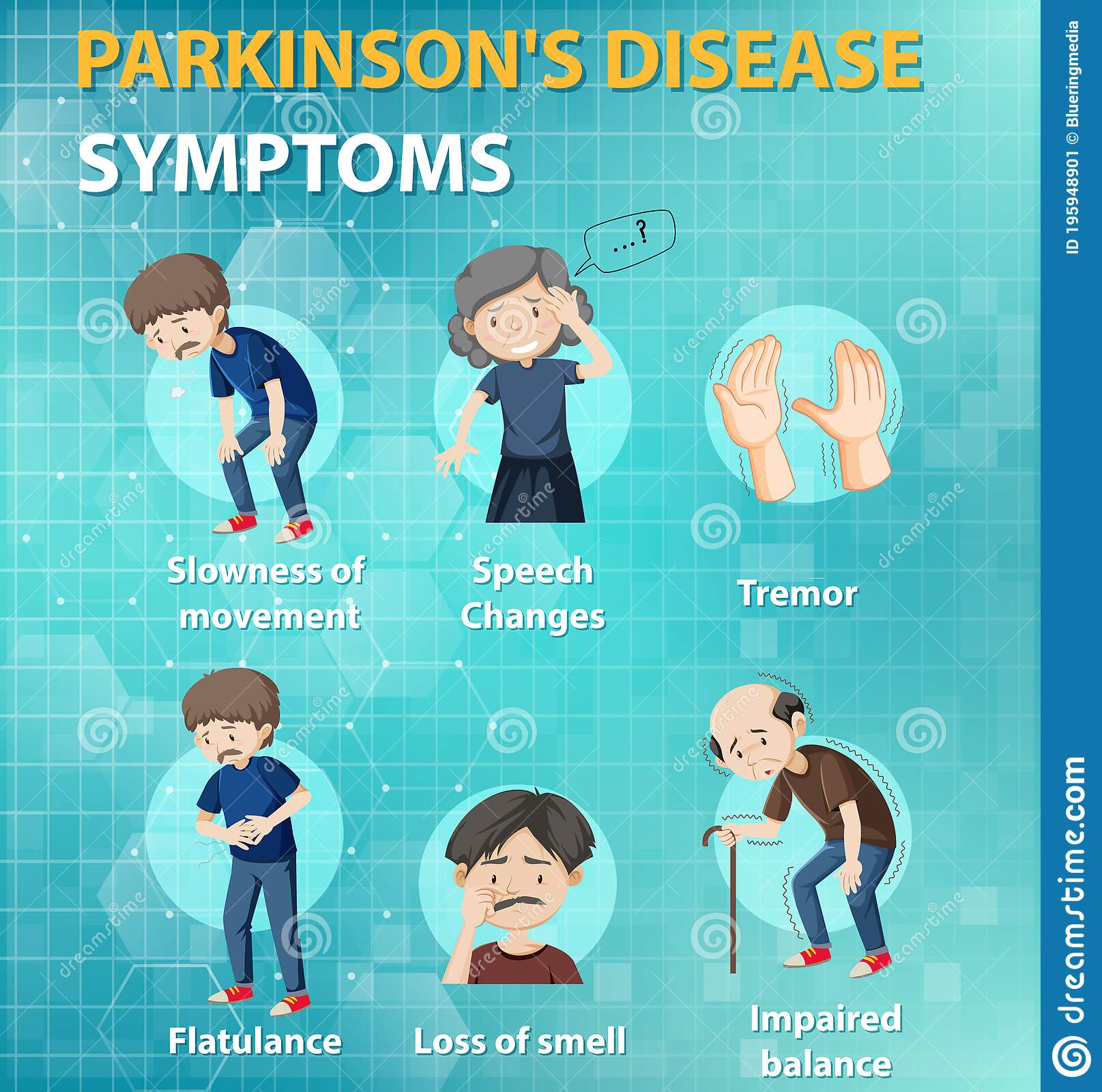
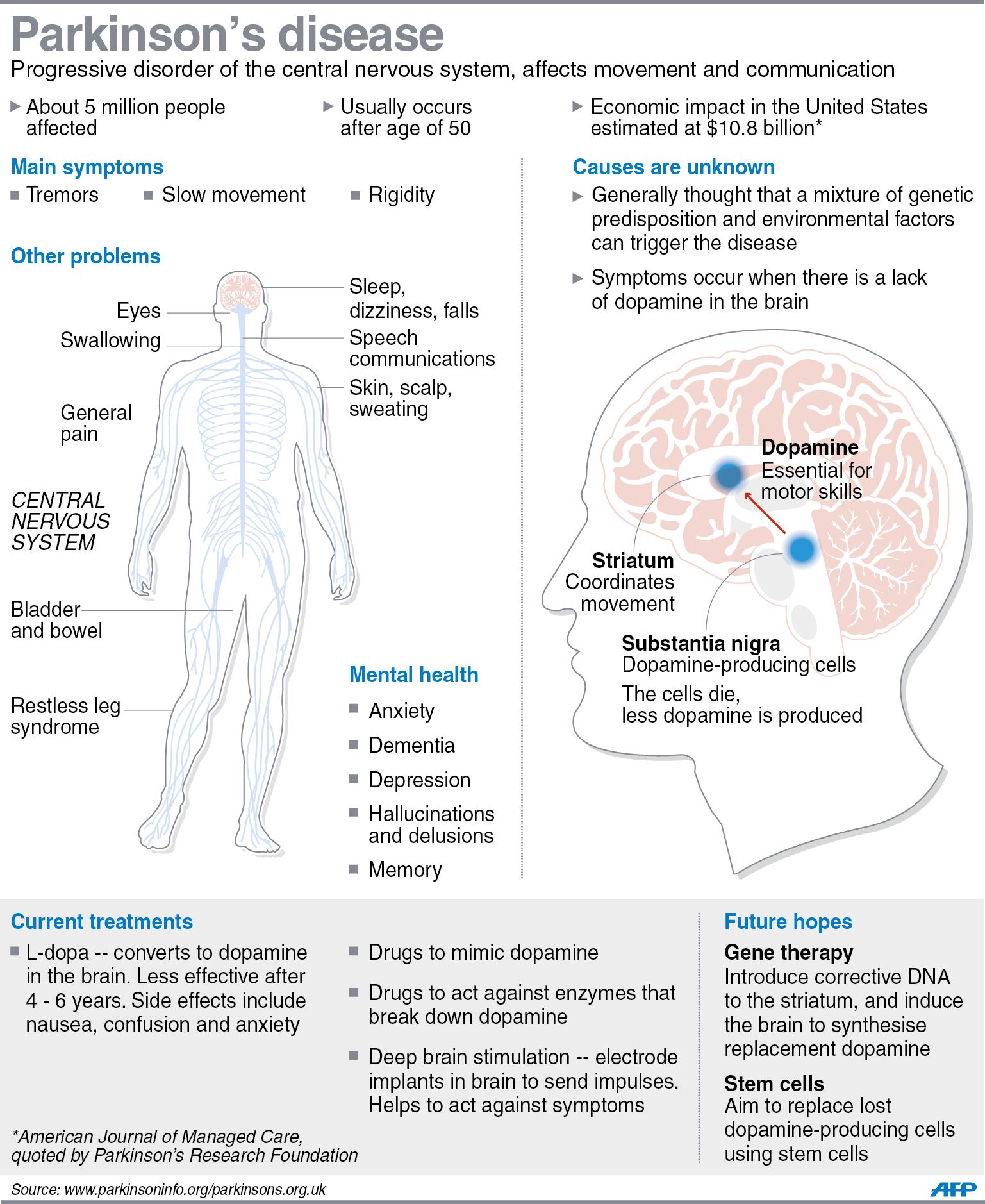
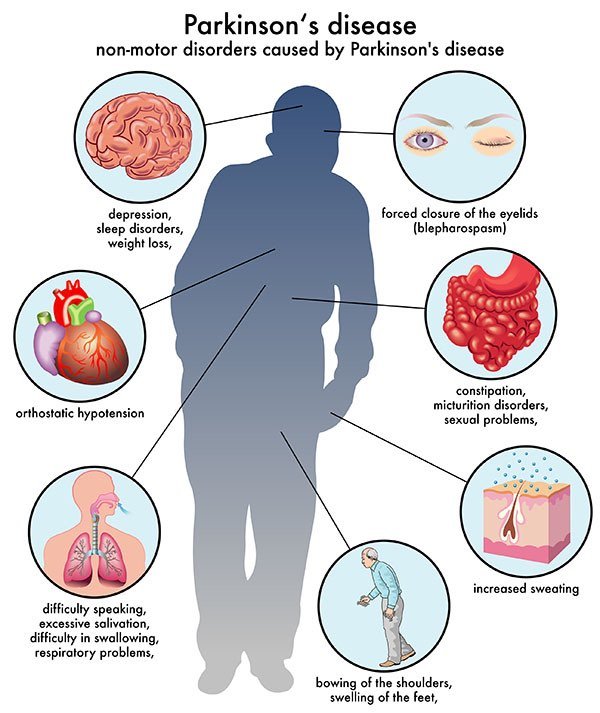
Parkinson’s disease is a type of movement disorder that can affect the ability to perform common, daily activities. It is a chronic and progressive disease, meaning that the symptoms become worse over time. It is characterized by its most common of motor symptoms—tremors , stiffness or rigidity of the muscles, and slowness of movement —but also manifests in non-motor symptoms including sleep problems, constipation, anxiety, depression, and fatigue, among others.
Donkey Kicks Parkinsons Disease And Chronic Lower Back Pain
This is one more glutes workout action that doubles as a lower-back helper.How to do it: Come down on your hands and knees, with your hands straight over your shoulders. Increase up your appropriate leg, keeping your knee at a 90-degree angle, until your leg is parallel to the ground. Slowly lower it back down to the ground. Repeat for 90 secs, then switch over legs.
What Are The Primary Motor Symptoms Of Parkinsons Disease
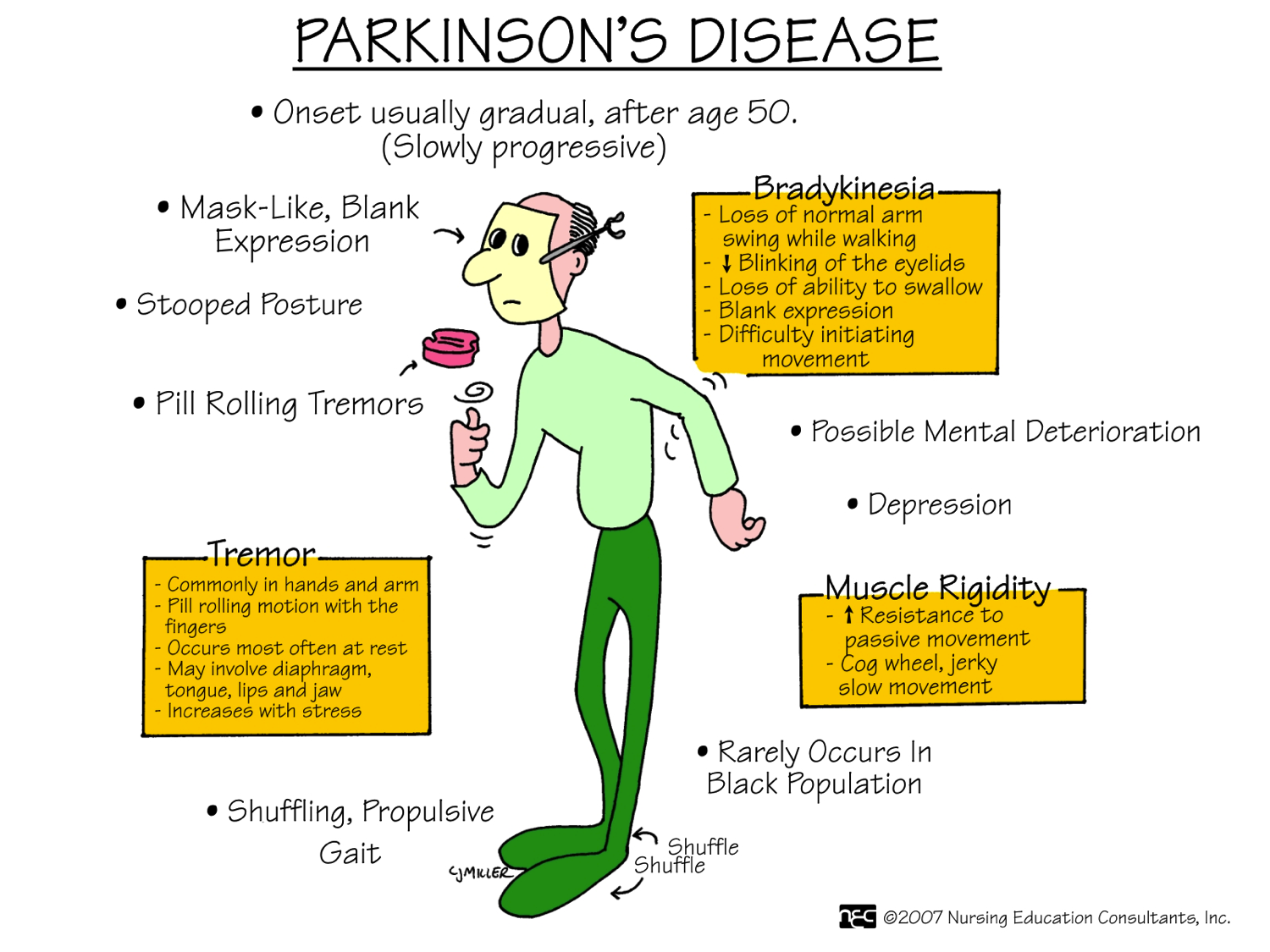
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Read more about Parkinson’s tremors
Rigidity
Bradykinesia
mask-like expression of the face
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Vacuuming Parkinsons Disease And Chronic Lower Back Pain
When it comes to reinforcing the lower back, concentrating on your transverse abdominals which are twisted around the midline of your body is one of the very best means to do it. These muscular tissues are actually type in supporting your spine and lower back. While people frequently towards problems for their transverse abs, people can inadvertently throw out their lower back if their core isn’t solid sufficient.
Just how to do it: In a standing placement, take a deep breath and also attract your tummy switch in towards your spinal column, contracting as well as engaging your ab muscular tissues as you do so. Think of if someone was mosting likely to show up and punch you in the tummy as well as you want your intestine to be tough and also able to take it; that’s what it needs to feel like. Hold it, and also release gradually. Repeat a few even more times.
Resilience Is About How You Recharge Not How You Endure
really spoke to me about my own background in this context, about my pre-diagnosis lifestyle which I do believe contributed to my chronic illness, that perhaps led to my body saying no. Hence this may serve as an example of what we’ve discussed above. Indeed, I know many people with Idiopathic Parkinson’s Disease will also identify with life-long coping styles such as “thriving on stress”, not being able to sit still, never being able to just rest and relax for long periods.
“The scientists cite a definition of ‘workaholism’ as ‘being overly concerned about work, driven by an uncontrollable work motivation, and investing so much time and effort to work that it impairs other important life areas.’ … The problem comes from a misunderstanding of what it means to be resilient, and the resulting impact of overworking. We often take a militaristic, ‘tough” approach to resilience and grit. We imagine a Marine slogging through the mud, a boxer going one more round, or a football player picking himself up off the turf for one more play. We believe that the longer we tough it out, the tougher we are, and therefore the more successful we will be. However, this entire conception is scientifically inaccurate.”
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Dopamine Suppression And The Neuroscience Of Giving Up
reveals how dopamine is not just used to reward and entrench behaviours, but also in natural mechanisms for evaluating when to “give up” on specific tasks. The neurochemical mechanism for this is via the release of a chemical called nociceptin, which suppress dopamine.
“From an evolutionary perspective, the researchers speculate that neural circuits linked to motivation and reward … are designed to preserve energy when resources are scarce. Therefore, nociceptin neurons may be a biological mechanism designed to force humans and animals to cut losses as opposed to continuing fruitless attempts to go after a reward due to sunk costs. ‘Persistence in seeking uncertain rewards can be disadvantageous due to risky exposure to predators or from energy expenditure,’ the researchers noted.”
I would suggest, at least, that perhaps at the point of diagnosis we might be given some space and time and support to reflect on our own activities and lifestyles up to that point which might be contributing to our dopamine deficiencies, and be given the tools by which we can seek to understand which parts of our lives have become totally unrewarding, but in which feel we must carry on regardless. Having then identified these issues, maybe we could be provided with the support to be able to stop and not carry on making our situation worse, interventions such as early retirement, being allowed to work from home, marriage counselling and so on.
Cool It Parkinsons Disease And Chronic Lower Back Pain
Ice is best in the first 24 to 2 days after an injury since it lowers inflammation. Although the warmth really feels excellent because it helps hide the pain as well as it does help kick back the muscular tissues, the warmth actually inflames the inflammatory procedures. After 2 days, you can change to warmth if you prefer. Whether you use heat or ice– take it off after about 20 minutes to offer your skin a remainder. If pain lingers, talk with a doctor.
Stretch Parkinsons Disease And Chronic Lower Back Pain
Do not rest dropped in your workdesk chair throughout the day. Get up every 20 mins or two and extend the various other means. Because a lot of us invest a great deal of time flexing ahead in our tasks, it is necessary to stand up and stretch backward throughout the day. Don’t fail to remember to additionally extend your legs. Some individuals find relief from their pain in the back by doing a normal extending routine, like yoga exercise. Parkinson’s Disease And Chronic Lower Back Pain
Drugs And Medication Used To Treat Parkinsons Disease
A number of different drugs can be used to treat Parkinson’s.
Levodopa
Levodopa is the most common treatment for Parkinson’s. It helps to replenish dopamine.
About 75 percent of cases respond to levodopa, but not all symptoms are improved. Levodopa is generally given with carbidopa.
Carbidopa delays the breakdown of levodopa which in turn increases the availability of levodopa at the blood-brain barrier.
Dopamine agonists
Dopamine agonists can imitate the action of dopamine in the brain. They’re less effective than levodopa, but they can be useful as bridge medications when levodopa is less effective.
Drugs in this class include bromocriptine, pramipexole, and ropinirole.
Anticholinergics
Anticholinergics are used to block the parasympathetic nervous system. They can help with rigidity.
Benztropine and trihexyphenidyl are anticholinergics used to treat Parkinson’s.
Amantadine
Amantadine can be used along with carbidopa-levodopa. It’s a glutamate-blocking drug . It offers short-term relief for the involuntary movements that can be a side effect of levodopa.
COMT inhibitors
Catechol O-methyltransferase inhibitors prolong the effect of levodopa. Entacapone and tolcapone are examples of COMT inhibitors.
Tolcapone can cause liver damage. It’s usually saved for people who do not respond to other therapies.
Ectacapone does not cause liver damage.
Stalevo is a drug that combines ectacapone and carbidopa-levodopa in one pill.
MAO-B inhibitors
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Is Parkinson’s Disease Its A Movement Disorder
Parkinson’s disease is a progressive brain illness that affects the way you move. In more clinical terms, Parkinson’s disease is a neurodegenerative disorder of the central nervous system.
Normally, there are cells in the brain that produce a chemical called dopamine. Dopamine sends signals to the parts of your brain that control movement. When approximately 60-80% of the dopamine-producing brain cells are damaged, symptoms of Parkinson’s disease appear, and you may have trouble moving the way you want.
Parkinson’s disease is a chronic illness and it slowly progresses over time. While there is no therapy or medicine that cures Parkinson’s disease, there are good treatment options available that can help you live a full life.
Learning How To Manage Daily Living With Parkinsons
Once you are diagnosed with PD, your focus should be on improving your symptoms and maintaining an active and positive lifestyle.
Although there is currently no cure for PD, it is possible to successfully manage symptoms through healthy choices, medications, and, in select cases, medical procedures.
If you’re new to Parkinson’s disease and would like a good overview to help you better understand the disease, please view our Parkinson’s Disease: The Essentials presentation. It’s a great place to get started with reliable and concise information.
- Finding local resources and support groups.
- Find upcoming classes and webinars on our Virtual Events Calendar
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
>>> Click Here For Effective Lower Back Pain Relief
Preliminary therapy in your home may include warm application as well as avoiding reinjury and heavy lifting. Prescription medicines that are sometimes utilized for severe lower back pain include non-steroidal anti-inflammatory medications, by shot or by mouth, muscular tissue relaxants,Long periods of inactivity in bed are no more recommended, as this therapy might actually reduce healing. Spinal adjustment for durations of up to one month has actually been discovered to be helpful in some clients who do not have indicators of nerve irritability.
Future injury is stayed clear of by utilizing back-protection strategies throughout activities and support devices as needed in your home or job.
Muscle Mass Strain and Ligament StrainA lower back sprain or pressure can happen all of a sudden, or can develop slowly with time from repetitive motions. Parkinson’s Disease And Chronic Lower Back Pain
Stress occur when a muscle is extended as well far and tears, harming the muscle itself.
Strains take place when over-stretching and tearing affects tendons, which connect the bones together.
For practical functions, it does not matter whether the muscle mass or tendon is damaged, as the symptoms as well as treatment coincide.
Usual causes of sprain as well as stress consist of:
While strains as well as stress do not appear major and do not typically trigger long-lasting pain, the acute pain can be fairly severe.
Does Having Rls Increase The Risk Of Developing Pd
Since RLS affects as much as 4-10% of the US adult population, it is clear that the vast majority of those with RLS do not ever develop PD.
Despite this, it still might be the case that RLS increases the risk of subsequently developing PD. There have been many studies trying to figure this out – with conflicting results. Some studies show that there is no increased risk and others show that having RLS confers about a two-fold increased risk of developing PD over the general population.
Sidebar: Ninds Steps Up Pursuit Of Pd Biomarkers
In 2012, the NINDS dramatically accelerated efforts to identify biomarkers by establishing the Parkinson’s Disease Biomarkers Program . This unprecedented program unites a range of stakeholders from basic and clinical researchers to healthcare professionals, the NINDS staff, information technology experts, and people living with PD and their families.
PDBP supports research and builds resources aimed at accelerating the discovery of biomarkers to ultimately slow the progression of PD. For example, the program has established a repository of biological specimens and a Data Management Resource system maintained by the NIH Center for Information Technology. The DMR allows researchers to access clinical, imaging, genetic, and biologic data, while a complementary PDBP-supported project develops statistical tools to analyze vast quantities of data so that patterns can be identified across these diverse sources of information.
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Forgetfulness
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. It’s clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
What Are The Symptoms Of Parkinson’s Disease
The main symptoms of Parkinson’s disease are:
- tremor or shaking, often when resting or tired. It usually begins in one arm or hand
- muscle rigidity or stiffness, which can limit movement and may be painful
- slowing of movement, which may lead to periods of freezing and small shuffling steps
- stooped posture and balance problems
The symptoms of Parkinson’s disease vary from person to person as well as over time. Some people also experience:
- loss of unconscious movements, such as blinking and smiling
- difficulties with handwriting
- drop in blood pressure leading to dizziness
- difficulty swallowing
- sweating
Many of the symptoms of Parkinson’s disease could be caused by other conditions. For example, stooped posture could be caused by osteoporosis. But if you are worried by your symptoms, it is a good idea to see your doctor.
