What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Understanding Parkinsons Disease: Getting A Parkinsons Diagnosis
Once you start noticing some changes in your body that impact your daily life or are just simply bothersome, you should begin the process of figuring out if you have Parkinson’s disease. It may seem like a daunting undertaking, but don’t let fear stop you. Once you are diagnosed, you can start treating your symptoms and learning strategies that will help you feel better.
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
General Strategies For Getting The Most Out Of Your Care Team
It’s important to be an active partner in your care. Try to resist adopting the role of a passive patient who just follows the orders of the doctors. Ask questions. But ask them in a cordial way in order to learn. Ask questions so that you can maximize the benefits of any treatment you undergo. Try also to avoid the opposite danger of asking too many questions and of taking over the role of doctor yourself. You will have to learn to accept the care of others. Let them do their job. Learn from them. Partner with them. If you can establish this kind of partnership with your care team you and your family will find it easier to cope with all the challenges that PD will throw at you over the years.
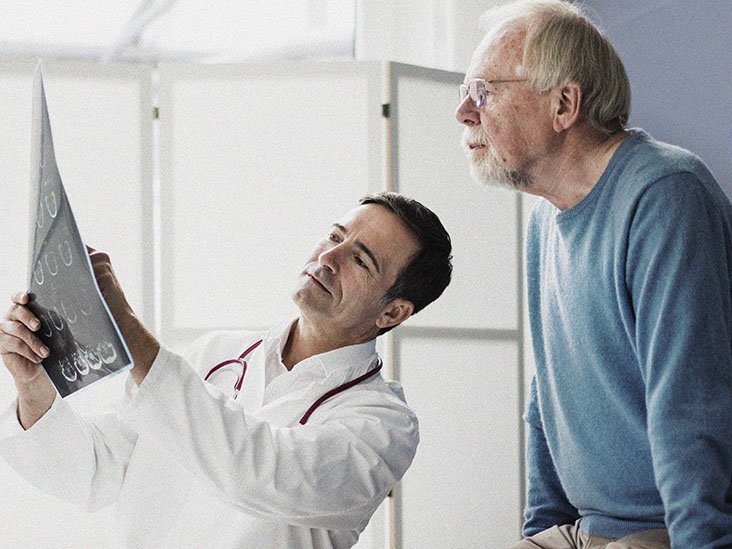
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Choose A Neurologist Who Specializes In Movement Disorders
Your first task is to find a neurologist who specializes in movement disorders . You need someone who can tell you what to anticipate and who can put you in touch with the best resources and treatment options available. This neurologist will know when to start medications and when to adjust the dosages of those medications to achieve maximum benefit and so forth. So how do you find such a specialist?
First, ask your primary care doctor for a referral to a Parkinson’s specialist. Your primary care doctor will certainly be able to point you in the right direction.
You can also find a local support group for Parkinson’s patients and ask those individuals for recommendations on specialists. You can get information on local support groups as well as local specialists from the local or regional chapters of a national Parkinson’s disease organization. If you can’t find a support group in your community, check out the online support communities for people with Parkinson’s disease who live in your area. You may even be able to get an idea of a neurologist who would meld well with your own personality by asking questions and hearing others talk about their experiences.
Conditions That May Be Mistaken For Parkinsons Disease
There are a few conditions that may be confused with Parkinson’s disease. These conditions can cause similar symptoms, and because there is no definitive test that proves you have Parkinson’s disease or any of these “similar” conditions. As you might imagine, this can make it challenging at times for doctors to figure out which condition you have. A few of the most common conditions that might look like Parkinson’s are:
How To Find The Right Doctors For Parkinson’s Disease
When you’ve been diagnosed with Parkinson’s disease, you’ll need to find the right care team. Ideally, you’ll want a team of clinicians who will manage your medical care over the course of the next few years. This team should be headed by a neurologist with expertise in treating Parkinson’s patients.
While you can always change members of the team, putting some amount of thought and planning into assembling the initial team will pay dividends for you down the road if that team can rapidly and effectively address your early symptoms and needs.
The following suggestions will help you to assemble the care team that is best for you, and will also provide some ideas on how best to interact with your care team.
What To Look For In A Parkinsons Disease Neurologist
Here is a checklist of basic questions for your prospective neurologist:
- How long have you worked in the field? How many Parkinson’s patients do you see a year?
- Do you have special training in movement disorders? Are you board-certified in neurology?
- Who do I see when you are not available?
- What hospital do you use for treating patients?
It’s important to understand that the online rating systems for doctors are not very accurate. Or they are, in some ways, and it is not the information you are looking for. For example, many of these ratings rank a doctor high if he is always on time and never backed up. If you think about the clinic setting and the inability to really control what happens in a typical day, and the doctor who is always time may be the doctor who never has that extra minute to give you when you need it. These ratings also often include how easy it is to get an appointment.
Of course, the doctor who is exceptional that everyone wants to see ranks poor on this measure, and the doctor who doesn’t have a strong following ranks high. If you do look at these rankings, make sure to read the comments, and realize that one bad comment could simply represent one patient having a bad day after being given a diagnosis he didn’t want.
What Parkinsons Diagnosis Criteria Do Doctors Use
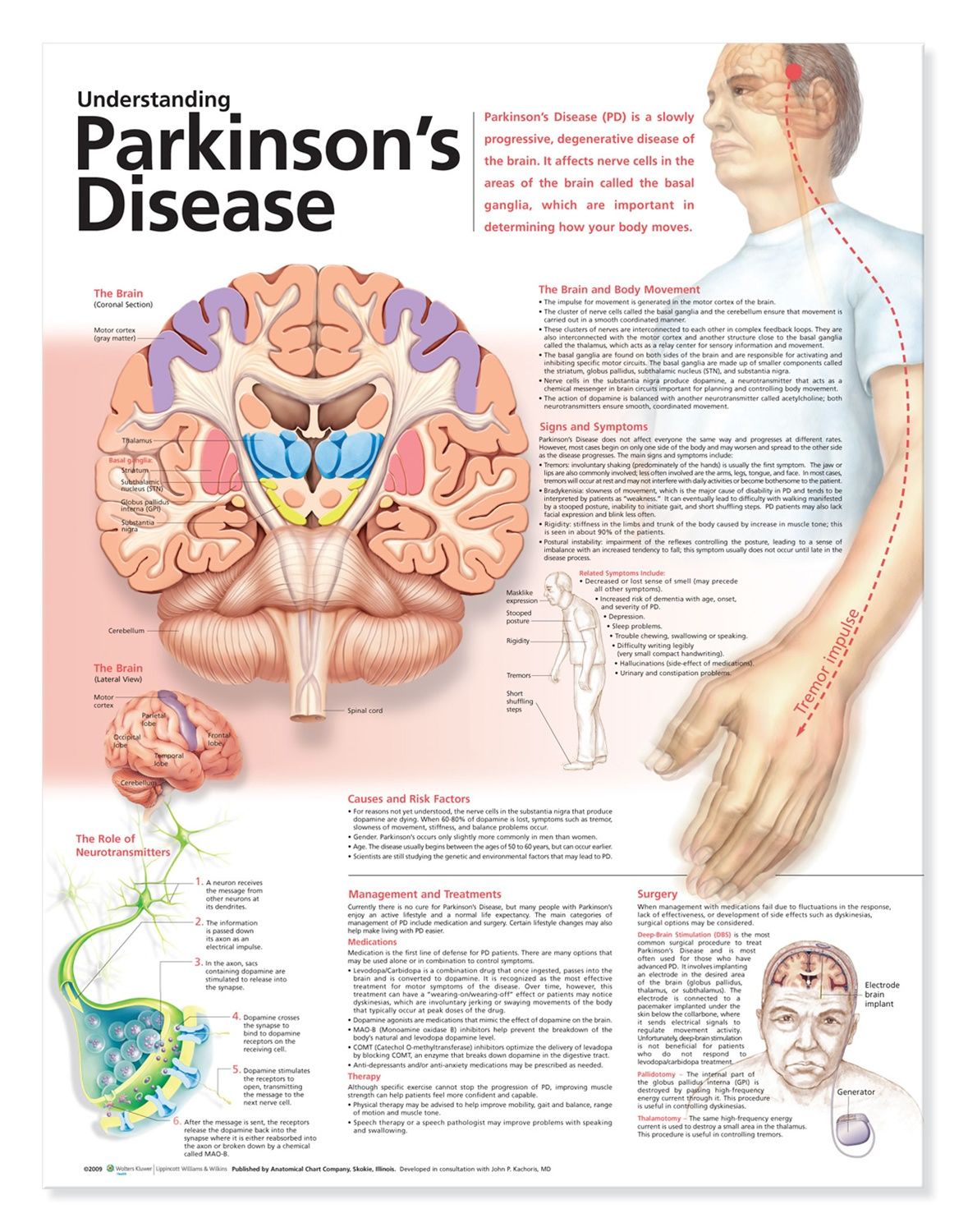
Until the 1980s, there was no formal diagnostic criteria for Parkinson’s disease. Beginning with James Parkinson’s 1817 article, “An Essay on the Shaking Palsy,” and Margaret Hoehn and Melvin Yahr’s description of the five stages of motor progression in 1967, scientists focused on the unique ways Parkinson’s disease affects movement. A few scientists also noted non-motor symptoms like issues with automatic body functions, such as heart rate and blood pressure.
With the discovery in the 1950s of levodopa, a drug that gets turned into dopamine in your brain and thus replaces some of the dopamine that is lost due to PD, and the discovery of how dramatically levodopa improves motor symptoms, the medical community continued to focus more of their efforts on defining and treating Parkinson’s as a motor condition.7
Other Challenges Of Diagnosing Parkinsons Disease
Parkinson’s disease progresses slowly, often with non-motor symptoms appearing months or years before motor symptoms. This can make it challenging for doctors to diagnose you in the early stages, especially since the diagnostic criteria is based mostly on motor symptoms. You may have to wait until your symptoms progress for you and your doctor to confirm your diagnosis.14
Age and gender can be another issue. Since Parkinson’s is associated more with older men, doctors may not think their younger or female patients have Parkinson’s.5 On the other hand, since the disease is associated with aging, your symptoms may be blamed on “getting older.”
Remember that movement disorder specialists are extremely knowledgeable about Parkinson’s disease and can help put the pieces together where other more generalized doctors may not. Never hesitate to fight for the care you deserve.
Related: Here’s what’s important to remember if you were just diagnosed with Parkinson’s disease.
What Doctors Look For When Diagnosing Parkinsons
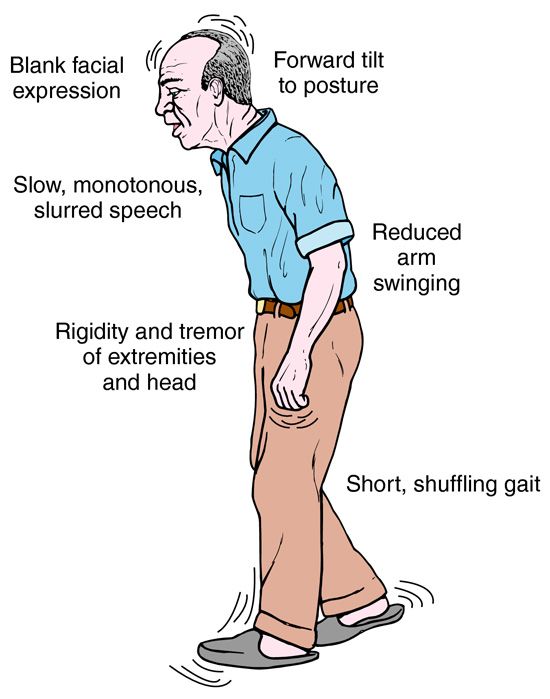
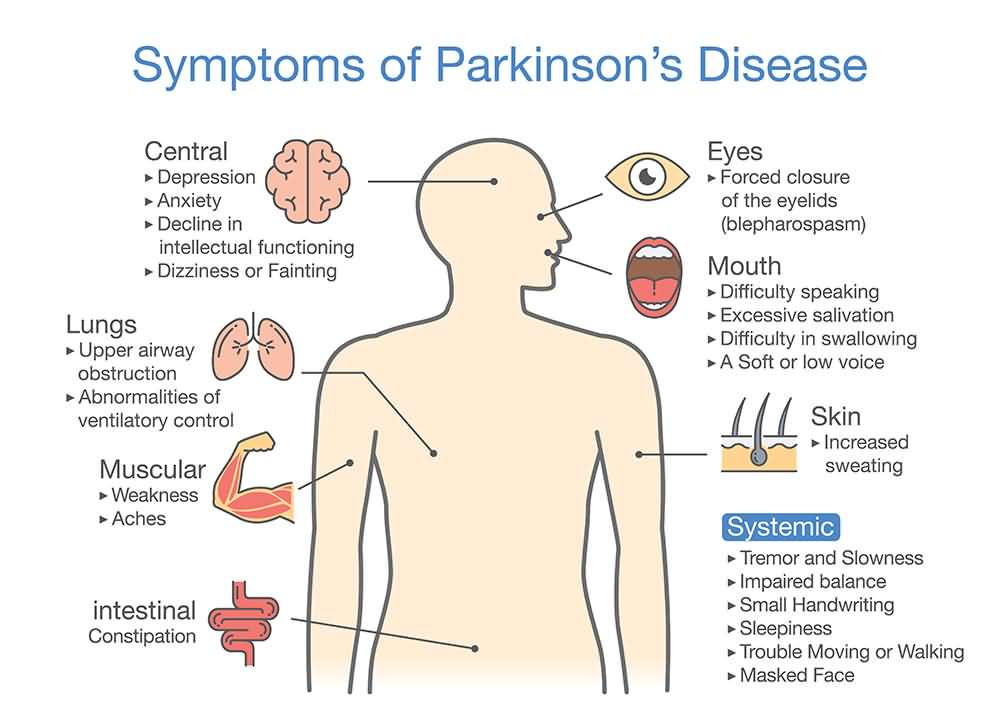
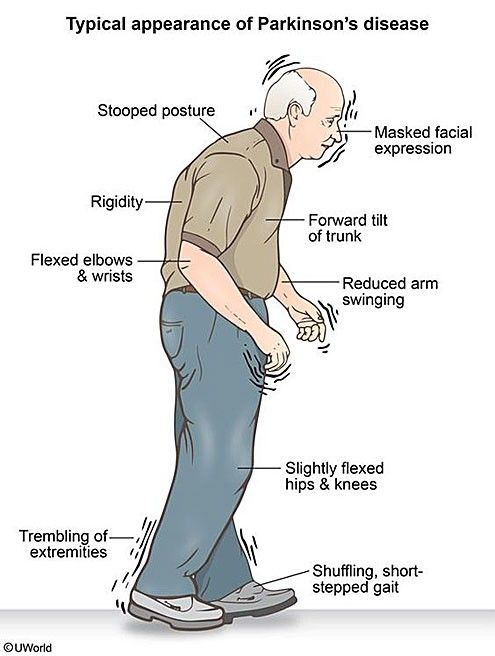
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
If Its Not Parkinsons Disease What Could It Be

Here are some possibilities:
Side effects of medication: Certain drugs used for mental illnesses like psychosis or major depression can bring on symptoms like the ones caused by Parkinson’s disease. Anti-nausea drugs can, too, but they typically happen on both sides of your body at the same time. They usually go away a few weeks after you stop taking the medication.
Essential tremor: This is a common movement disorder that causes shaking, most often in your hands or arms. It’s more noticeable when you’re using them, like when you eat or write. Tremors caused by Parkinson’s disease usually happen when you’re not moving.
Progressive supranuclear palsy: People with this rare disease can have problems with balance, which may cause them to fall a lot. They don’t tend to have tremors, but they do have blurry vision and issues with eye movement. These symptoms usually get worse faster than with Parkinson’s disease.
Normal pressure hydrocephalus : This happens when a certain kind of fluid builds up in your brain and causes pressure. People with NPH usually have trouble walking, a loss of bladder control, and dementia.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
How Is Parkinsons Disease Tested And Diagnosed
At Banner Health, our neurologists have years of experience in testing and diagnosing Parkinson’s disease. Our team of compassionate experts knows that each patient is different, so we work with you to quickly find the right diagnosis to begin building your treatment plan.
Parkinson’s is not simple to diagnose. No test exists to diagnose Parkinson’s disease. Doctors test and diagnose Parkinson’s based on your medical history, symptoms and neurological and physical exams.
Many times a primary care provider is the first to suspect a Parkinson’s diagnosis. If you’re experiencing symptoms such as tremors, shaking, slow movement, stiffness and/or trouble with balance, talk to your doctor or seek the opinion of a neurologist. Banner Health neurologists are movement disorder specialists, who have experience and specific training to assess and treat Parkinson’s.
Learn More About Parkinsons Disease: Overview
Tests For The Diagnosis Of Parkinsons Disease
There’s no specific single test that allows a direct diagnosis of Parkinson’s disease. This means that it can’t be detected by a blood, urine, or cerebrospinal fluid test, as well as an imaging test.
We hope that, in the future, researchers will be able to detect a biomarker that will facilitate direct diagnosis. However, for the time being, we have to use what’s available.
The Michael J. Fox Foundation explains to us that the diagnosis is made from the patient’s symptoms, their history, the answers to certain questions, and the findings found in the check-up. The experience and knowledge of the specialist play a key role in this. For this reason, they recommend consulting a specialist in movement disorders or a neurologist with specialized training in Parkinson’s.
On the other hand, the MSD Manual points out that when Parkinson’s disease isn’t certain, the doctor may prescribe a drug called levodopa. If the person shows a clear improvement after taking it, then the diagnosis is that they have Parkinson’s.
How Does Alcohol Affect Parkinsons Medication
The interaction between Parkinson’s medications and alcohol is a common topic on MyParkinsonsTeam. “I miss my red wine and whiskey on occasion,” one member wrote. “I found that it just makes my meds stop working.” Another member said, “My husband has been told he shouldn’t drink with his meds.”
Alcohol can exacerbate the side effects of one of the most common Parkinson’s medications, levodopa/carbidopa. Many neurologists recommend avoiding alcohol while taking this drug.
“I have to limit myself to one Scotch on the rocks now,” a MyParkinsonsTeam member said. “I used to have three or four, but the side effects are too bad.” Another wrote, “Never really a good idea to mix alcohol with meds.”
Whether you decide to continue your current drinking habits, cut down, or eliminate alcohol altogether, it’s important to listen to your body and have open conversations about these topics with your neurologist.
If you find yourself drinking alcohol to cope with other issues, such as depression and anxiety, you may find that healthy practices such as physical activity can help. In addition, participating in activities such as tai chi, yoga, and meditation may help ease the symptoms and complications of PD.
What Is The Prognosis For Parkinsons Disease
The rate at which Parkinson’s progresses varies from patient to patient. Some patients experience its changes over 20 years or more. While others find the disease advances quicker.
Parkinson’s is not a fatal disease. However, secondary complications from symptoms may increase falls, blood clots or pneumonia, which can be life-threatening. These are more common in later stages of Parkinson’s.
In general, the average life expectancy of Parkinson’s patients is similar to people without the disease.
Parkinson’s Symptoms That Lead To Diagnosis
The biggest clues your doctor will look for involve observing you as you sit and speak during an exam for PD, as well as how you perform movement tasks that your doctor may ask you to do. This will help your doctor determine if you have the hallmark symptoms of PD:
-
Balance and posture problems
-
Stiffness, or rigidity
-
Tremor, or uncontrolled shaking
For example, your doctor will likely look for any signs of tremor as you sit with your hands relaxed in your lap. Such hand tremors normally occur in only one hand, as PD tends to impact one side of your body more than the other. In addition, your doctor will take note of your facial expressions. PD symptoms can affect your facial muscles, and people with PD often smile and blink less often than people who do not have the disease. Other signs that can be picked up during an exam include:
How Does Alcohol Affect Parkinsons Symptoms
In general, alcohol can be harmful to people with chronic conditions. According to the Centers for Disease Control and Prevention , overconsuming alcohol can be a long-term risk factor for a weakened immune system, learning and memory problems, high blood pressure, digestive issues, and various types of cancer. When looking specifically at Parkinson’s symptoms, however, reports differ on how alcohol and PD may be linked.
The type of alcoholic beverage consumed may affect whether drinking has an impact on PD. A 2013 study found that the risk for developing Parkinson’s disease appeared to increase depending on the amount of liquor consumed, although no link was conclusively found between drinking wine and the development of PD.
In terms of how long-term alcohol use affects the risk of PD, one study published in 2013 followed people who had been admitted to the hospital with alcohol use disorders for up to 37 years. The study authors found that a history of alcohol abuse increased the risk of admission into the hospital for Parkinson’s for both men and women. The study authors suggested that chronically drinking too much alcohol can have neurotoxic effects on dopamine, the neurotransmitter in the brain that is relevant to Parkinson’s disease.
There may also be factors other than observable symptoms — such as how alcohol interacts with your medication — that are important to consider when making decisions about your lifestyle and drinking habits.
Surgery For People With Parkinsons Disease
Deep brain stimulation surgery is an option to treat Parkinson’s disease symptoms, but it is not suitable for everyone. There are strict criteria and guidelines on who can be a candidate for surgery, and this is something that only your doctor and you can decide. Surgery may be considered early or late in the progression of Parkinson’s. When performing deep-brain stimulation surgery, the surgeon places an electrode in the part of the brain most effected by Parkinson’s disease. Electrical impulses are introduced to the brain, which has the effect of ‘normalising’ the brain’s electrical activity reducing the symptoms of Parkinson’s disease. The electrical impulse is introduced using a pacemaker-like device called a stimulator. Thalamotomy and pallidotomy are operations where the surgeon makes an incision on part of the brain. These surgeries aim to alleviate some forms of tremor or unusual movement, but they are rarely performed now.
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinson’s disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinson’s disease management. But generalist teams are becoming more aware of how to help people with Parkinson’s disease.
Parkinsons Disease And Alcohol: Your Guide
If you have Parkinson’s disease , you may be wondering whether alcohol consumption affects the development or progression of your condition. Some people may wonder if they should avoid drinking completely. As one MyParkinsonsTeam member asked, “How does alcohol affect Parkinson’s — how much can I drink? Or should I avoid drinking altogether?”
Some studies haven’t found that small amounts of alcohol are associated with a higher PD risk, while others highlight the dangers alcohol can pose for anyone with a chronic condition. In addition, there may be adverse interactions between alcohol and common Parkinson’s medications. Because of conflicting information, people with PD may feel confused about whether or not to drink.
“I’ve been told by more than one doctor that I should not have any alcohol,” one MyParkinsonsTeam member wrote. “And at this point, I don’t remember which doctor or specifically why.”
So, how do you decide what approach to take?
If you have Parkinson’s disease and are trying to decide whether or not to reduce your drinking — or quit alcohol completely — here are some things to consider.
Obtaining A Parkinson’s Disease Diagnosis
During the exam, the neurologist will look for cardinal symptoms of the disease. Facial expressions and features will be assessed. The doctor will look for signs of tremor while the patient is at rest. The doctor may watch how easily the patient stands up from sitting in a chair. The doctor may also stand behind the patient and gently pull back on the patient’s shoulders and look for how easily the patient can regain balance. Good responsiveness to levodopa also helps support the diagnosis of PD. However, taking levodopa may exclude patients from clinical studies that need to recruit recently diagnosed patients who have not yet had treatment . Participation in a clinical trial should be discussed with the doctor.
PD can be challenging to accurately diagnose, particularly in early stages of the disease, which is why a neurologist trained in movement disorders is critical. Approximately 5-10% of patients with PD are misdiagnosed, as many of the symptoms of PD are similar to other diseases. If the patient thinks that he or she has been misdiagnosed, a second opinion may help.1,2
New Diagnostic Standards For Parkinsons
Until recently, the gold-standard checklist for diagnosis came from the U.K.’s Parkinson’s Disease Society Brain Bank. It was a checklist that doctors followed to determine if the symptoms they saw fit the disease. But that’s now considered outdated. Recently, new criteria from the International Parkinson and Movement Disorder Society have come into use. This list reflects the most current understanding of the condition. It allows doctors to reach a more accurate diagnosis so patients can begin treatment at earlier stages.
Be Honest With Yourself And Your Doctor
It is important to discuss alcohol consumption with your doctor to make sure you are approaching it safely. Elements of PD, including motor symptoms such as bradykinesia and dyskinesia , will vary from person to person, so it’s important to make decisions based on your medical history.
Taking into account environmental factors such as how central alcohol is to your social life can affect the decisions you make. Be honest with your doctor about your habits and preferences — remember, your doctor wants to work with you to make your symptoms as manageable as possible, not to judge or shame you.
As you decide how alcohol may fit into your life post-diagnosis lifestyle, there are many factors to consider, such as the type of alcoholic beverage, your other risk factors, and your neurologist’s recommendations specific to your medical history. Most importantly, monitor how you feel when you drink alcohol and be willing to have open and honest conversations about drinking with your doctor and other important people in your life.
“I am not even a big drinker, but miss the odd one,” wrote a MyParkinsonsTeam member. “So, I had an alcohol-free beer, which tasted OK, to be honest.”
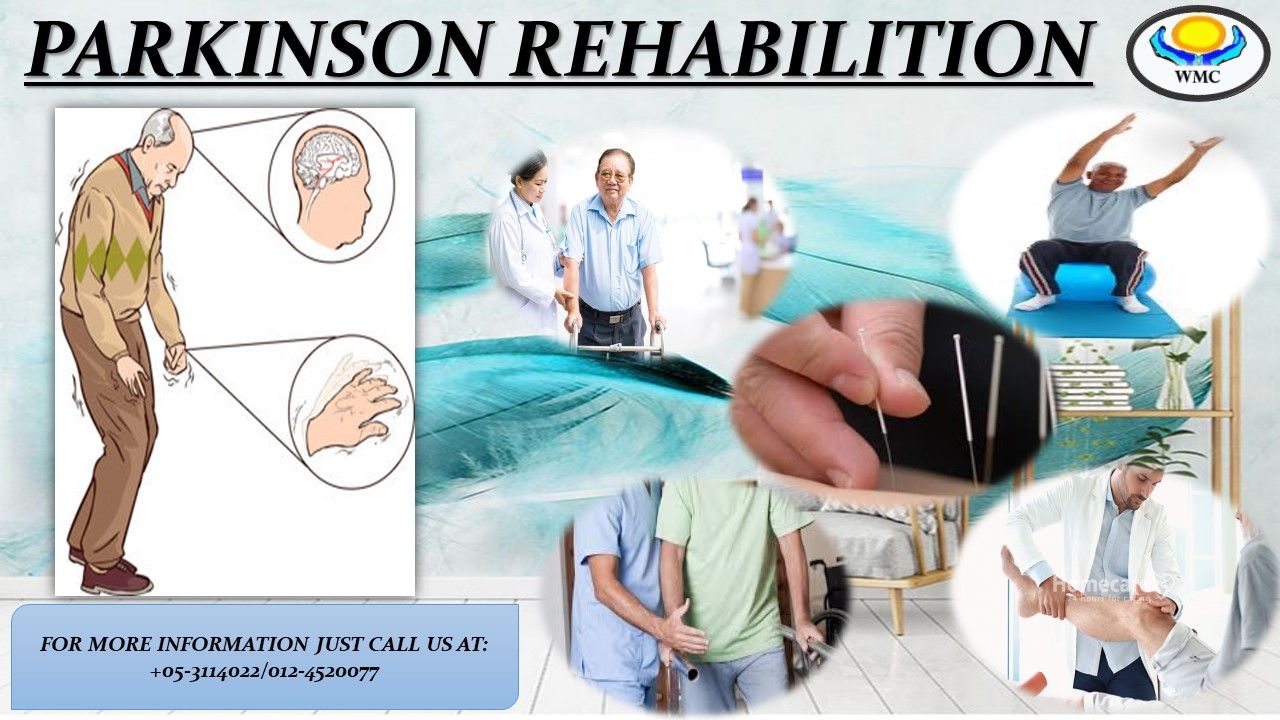
Rehabilitation For Parkinsons Patients
Parkinson’s disease patients may find that rehabilitation services, including physical therapy, ease symptoms. Therapy focuses on helping patients build strength and move more easily. Goals may include improving walking, balance and overall movement.
Ask your doctor or specialist about getting a referral for rehabilitation with a therapist. Often rehabilitation services are close to home, in your community.
MaineHealth has home care services that support patients in their homes. Services may include:
- Nurses
- Help with laundry and household chores
- Counseling and emotional support
- Personal care help with daily activities
- Telehealth
Brain Imaging Can Help With Diagnosis
Doctors use two tests that take detailed pictures of your brain. Each one may help your doctor make a diagnosis. These tests are:
- PET scan: This shows how your brain functions. It shows how the brain uses sugar. This scan can help tell the difference between Parkinson’s and dementia.
- DaTscan: This shows problems with brain cells that make dopamine. Healthy brain cells light up during the test. Cells without enough dopamine appear dark. This scan can help your doctor tell the difference between Parkinson’s and a brain disease called essential tremor.
Imaging studies are a newer way to diagnose Parkinson’s. However, not every healthcare facility can do them. It takes an experienced doctor to interpret the scans accurately. These scans also can be very expensive. Be sure to check with your insurance company ahead of time to see whether you are covered and what your out-of-pocket costs will be.
Trying Parkinsons Disease Medications
One of the features of PD is that it will significantly and consistently improve when you begin taking medication that targets your dopamine system.10 Your doctor may ask you to try taking Parkinson’s medication, like carbidopa-levodopa, to help confirm a PD diagnosis. Levodopa is a drug that is converted into dopamine in your brain, replacing some of the dopamine you lose due to the disease. Levodopa is frequently paired with carbidopa, which helps prevent levodopa from breaking down before it reaches your brain. Your doctor will observe if carbidopa-levodopa helps your motor symptoms. Carbidopa-levodopa is typically very effective at treating motor symptoms, so a significant response to the medication used to treat it helps confirm the diagnosis. Parkinson’s medications are generally very safe and the risk of taking them is low, while the benefit is great because it might help if you do have Parkinson’s and improve your mobility.10
Related: What you can do before you see your doctor next.
Physical And Neurological Examination
Your doctor will conduct a physical and neurological examination. This can involve observing your behavior, movements, and mental state and conducting tests or asking you to perform certain exercises.
These are some of the symptoms of Parkinson’s your doctor can determine visually:
- Fewer spontaneous movements or hand gestures
- Reduced frequency of blinking
- Tremors in your hands while they are at rest, often only in one hand
- Hunched posture or forward lean while walking
- Stiff movements
These are some of the exercises your doctor may ask you to do to evaluate your movements, balance, and coordination:
- Opening and closing your fist
- Tapping your fingers, toes, and heels
- Holding your arms out in front of you
- Moving your finger from one point to another
- Rotating your wrists or ankles
- Standing from a chair
Deep Brain Stimulation Benefits for Parkinson’s Can Last at Least 15 Years