The Efficacy And Safety Of Antipsychotic Medications In The Treatment Of Psychosis In Patients With Parkinsons Disease

Nevena Divac
1Department of Pharmacology, Clinical Pharmacology and Toxicology, Faculty of Medicine, University of Belgrade, Dr. Suboti?a Starijeg 1, 11000 Belgrade, Serbia
2Clinic of Psychiatry, Clinical Center of Serbia, Faculty of Medicine, University of Belgrade, Pasterova 2, 11000 Belgrade, Serbia
Abstract
1. Introduction
Parkinson’s disease is a complex neurobehavioral disorder. Among behavioral problems, psychotic symptoms are highly relevant because they significantly affect the quality of life and complicate the treatment of motor symptoms by limiting the use of medications .
Psychotic symptoms are present in up to 50% of patients with PD, but estimates vary widely . They are usually associated with other correlates such as older age, more advanced age at the onset of the disease, duration of disease, disease staging, cognitive decline, presence of depression, and the use of antiparkinson medication . Psychotic symptoms in PD patients are also associated with increased caregivers’ stress, increased rates of nursing home placement, and poor clinical prognosis . Therefore, psychotic symptoms in patients with PD require treatment. The reduction of antiparkinson medication is usually the first step but is usually ineffective and accompanied with worsened motor symptoms . When reduction of antiparkinson drugs does not improve psychotic symptoms, antipsychotic agents should be considered .
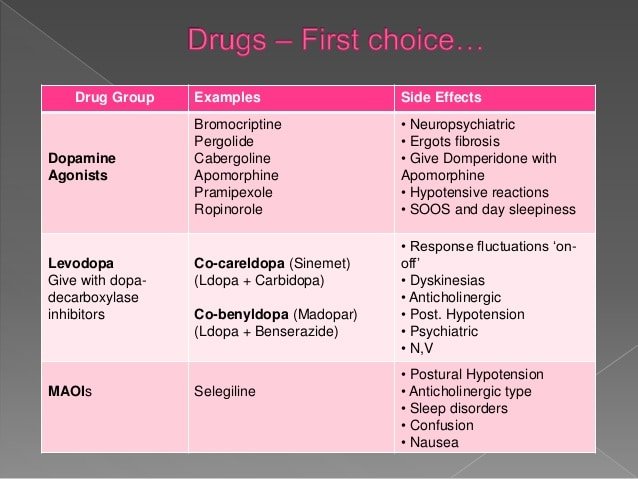
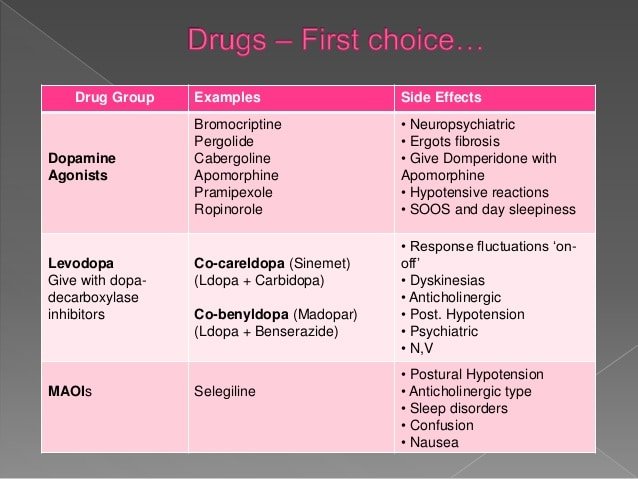
3. Antipsychotic Medications in Patients with PD
5. Conclusion
Competing Interests
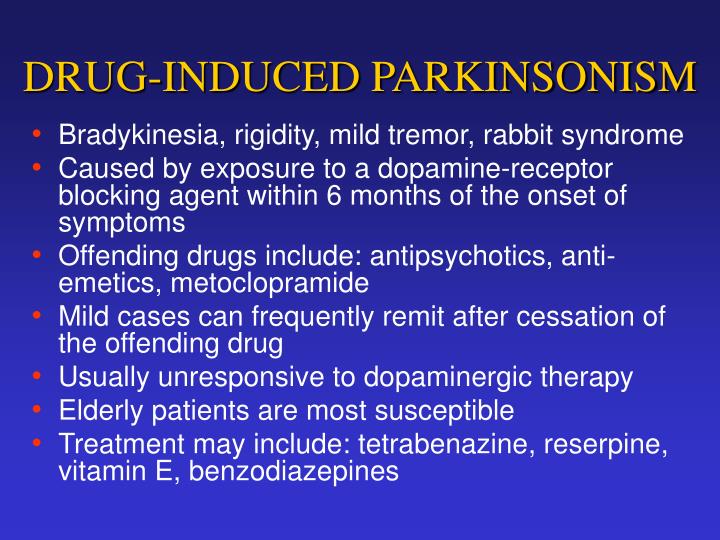
What Is The Difference Between Drug Induced Parkinsons Disease And Typically Occurring Parkinsons Disease
It has been seen that drug-induced Parkinsonism usually occur on both sides of your body while usual Parkinson’s starts from one side of the body. Apart from this, the medication-induced signs generally are seen to go away after the medicine is finished. However, it may take few months to stop, but is does stop eventually. On the contrary, the typically occurring Parkinson’s disease cannot be reversed. Another thing to be kept in mind is that medication-induced Parkinson’s disease is not progressive, unlike the typical Parkinson’s disease.
Antipsychotics For The Management Of Psychosis In Parkinson’s Disease: Systematic Review And Meta
- CT1 SHO in General Medicine, Nottingham University Hospitals NHS Trust, Queen’s Medical Centre, Nottingham, UK
- Oluwademilade A. Onalaja
- Stratford Healthcare, Arden Street, Stratford-Upon-Avon, UK
- Corresponding
Antipsychotics can exacerbate motor symptoms in Parkinson’s disease psychosis.
To systematically review the literature on the efficacy and acceptability of antipsychotics for Parkinson’s disease psychosis.
Randomised controlled trials comparing an antipsychotic with placebo were systematically reviewed.
The final selection list included nine studies using quetiapine , clozapine , olanzapine and pimavanserin . A narrative synthesis and meta-analyses were presented for each antipsychotic. Clozapine demonstrated superiority over placebo in reducing psychotic symptoms. Quetiapine and olanzapine did not significantly improve psychotic symptoms. All three antipsychotics may exacerbate motor symptoms. Quetiapine studies were associated with high drop-out rates due to adverse events. Pimavanserin is a novel treatment that warrants further investigation.
Further research is needed. Clozapine and pimavanserin appear to be a promising treatment for Parkinson’s disease psychosis.
Serotonin Reuptake Blocking Antidepressants Fluoxetine Sertraline And Paroxetine
Several other medications have been reported to cause drug-induced parkinsonism and to worsen parkinsonism in people with Parkinson disease, including the serotonin reuptake blocking antidepressants fluoxetine, sertraline, and paroxetine. Two calcium channel blockers available in Europe and South America , which are piperazine derivatives, are thought to cause drug-induced parkinsonism by blocking dopamine receptors. Reports of parkinsonism induced by other drugs, such as lithium and amiodarone, are so rare that only after parkinsonism has developed should the possible drug effect be taken into account. Because lithium is not known to block dopamine receptors, another mechanism is likely. Some animal data implicate an effect of lithium on intercellular signalling via G-protein coupled receptors . One antidepressant, amoxapine, has dopamine receptor-blocking properties and, therefore, may induce parkinsonism. Parkinsonism as a transient side effect of alcohol withdrawal has been reported without later development of Parkinson disease, but it is unknown how common this is .
Any Medication That Blocks Dopamine In The Body Can Cause Parkinsons Symptoms
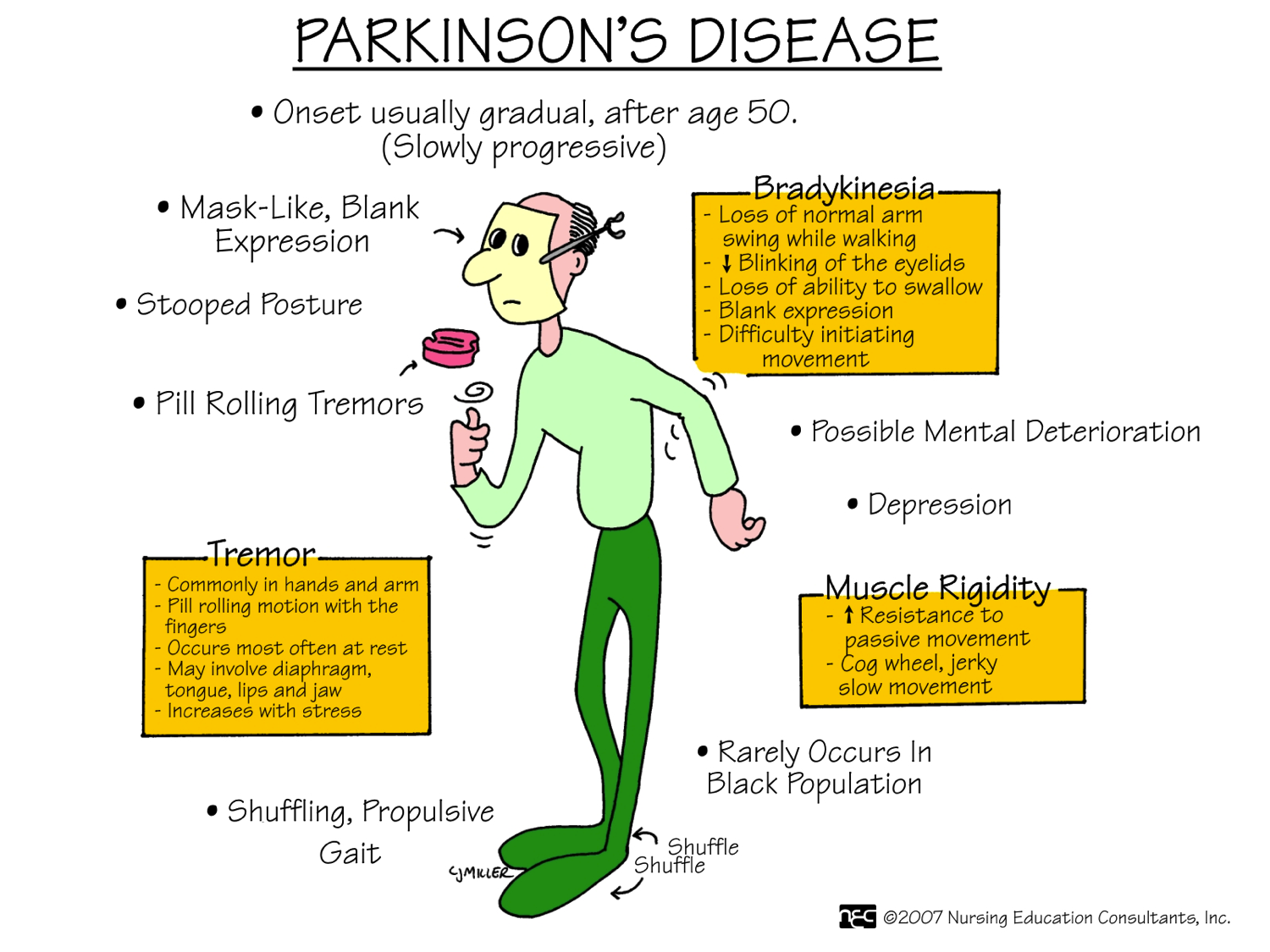
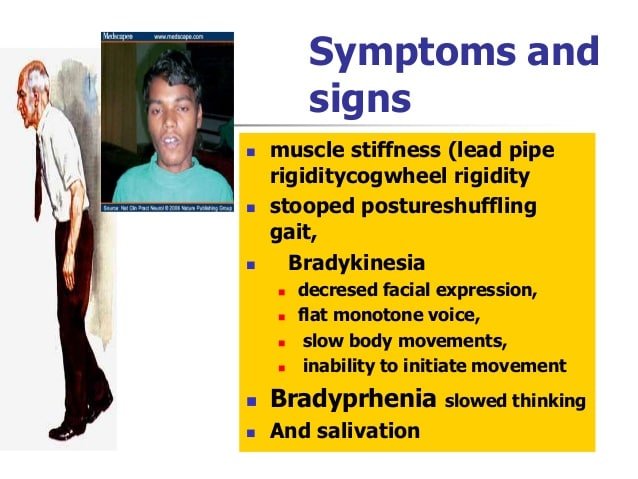
You may have heard of Parkinson’s disease , a movement disorder. Someone with it may have characteristic signs, such as a pill-rolling tremor in the fingers or a hunched forward posture. You may recognize someone with this disease from the faltering, tiny steps they take when they walk or by their rigidly emotionless face.
The cause of Parkinson’s disease is mostly unknown. Some people develop Parkinson’s-like symptoms after treatment with certain medications. This is called drug-induced parkinsonism or secondary parkinsonism. Certain medications can also worsen symptoms in someone who already has Parkinson’s disease.
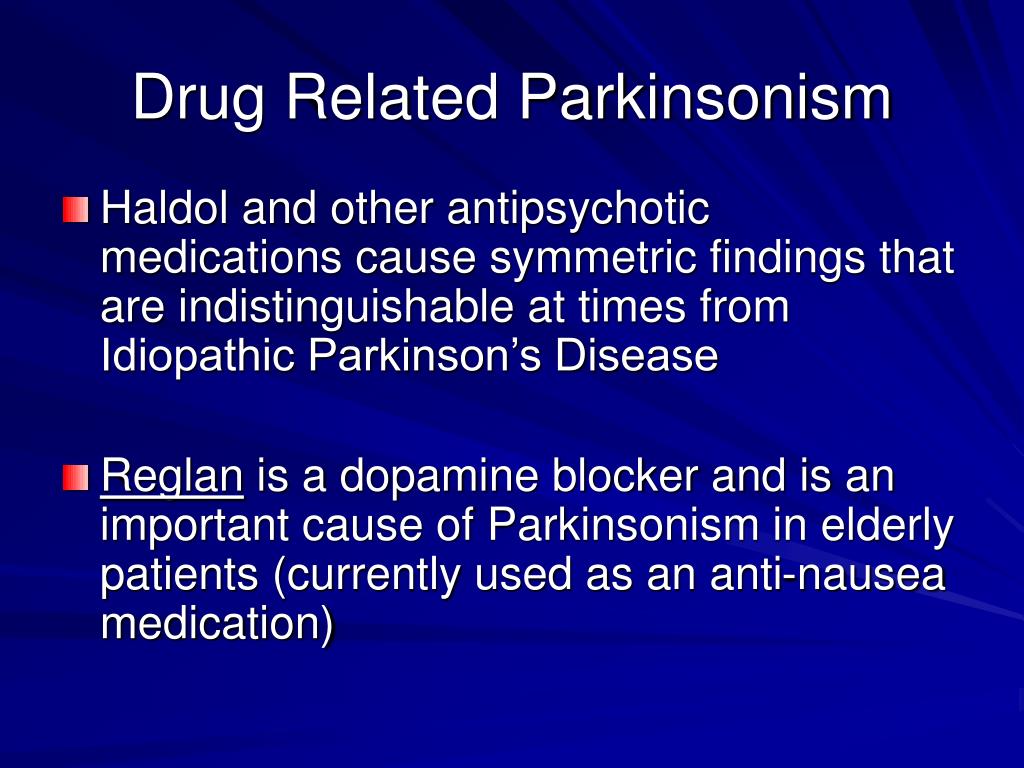
Any medication that blocks dopamine in the body can cause Parkinson’s symptoms. Dopamine is a brain chemical that helps control movement. Common dopamine-blocking drugs are antipsychotics. They are used to treat certain mental illnesses or severe nausea. Less commonly, certain types of calcium channel blockers cause drug-induced parkinsonism. These drugs may be used to treat chest pain and high blood pressure, or irregular heart rate.
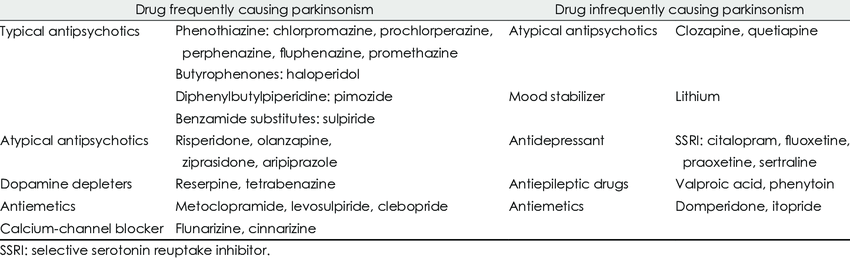
Drugs Associated With Parkinsonism And Other Abnormal Involuntary Movements
There are numerous drugs and drug classes that are associated with the development of parkinsonism and other abnormal involuntary movements. Drug-induced parkinsonism is often not recognised, especially in the non-psychiatric patient , The side effect often develops within 1 month of the start of treatment, with 60% of patients developing it by this time point and 90% within 3 months .The potency of antipsychotics is defined by their ability to block the D2 receptors. Therefore, high-potency neuroleptics tend to have a greater propensity to cause extra-pyramidal side effects. However, some high-potency neuroleptics that also have anticholinergic properties are associated with fewer motor side effects. Atypical antipsychotics tend to have broader pharmacodynamic effects, and it is thought that their activity at 5HT2a receptors mediate efficacy with less need for blocking of the D2 receptors in the mesolimbic pathways and therefore in the substantia nigra.
The evidence surrounding iatrogenic dystonias is less well developed. Conventional neuroleptics are clearly implicated as are calcium channel blockers. Additionally, there are several case reports noting an association with olanzapine, carbamzaepine, lithium, imipramine, gabapentin and ziprasidone. Other dystonias are less clearly associated with iatrogenic causes.
What Are The Other Forms Of Medicines That Can Cause Parkinsons Disease
Some of the other common medicines which can cause Parkinson’s disease may include some forms of anti-depressants, anti-nausea drugs, drugs used for the treatment of vertigo, drugs used for epilepsy and anti-arrhythmics. It should be remembered that not all drugs in these classes may cause signs of Parkinsonism. The doctor generally makes the patient aware of the side-effects before prescribing a certain form of drugs. Nevertheless, it is important from the patient’s part to ask about the side-effects of the prescribed medicines.
Not All Drugs In These Classes Will Cause Symptoms Of Parkinsonism
What’s the difference?
Drug-induced parkinsonism usually develops on both sides of the body, while typical Parkinson’s disease does not. Also, drug-induced parkinsonism usually does not progress like typical Parkinson’s.
Unlike Parkinson’s, drug-induced symptoms usually go away after the drug is stopped. It may take several months, though, for the symptoms to completely stop. If the symptoms remain, then it is possible that the drug may have “unmasked” underlying Parkinson’s disease.
Who is at risk?
- Female: Women are twice as much at risk as men.
- Elderly: Older people are more likely to be on multiple medications or to have underlying Parkinson’s disease.
- Those with a family history of Parkinson’s disease.
- People with AIDS.
Antipsychotics To Induce Dyskinesia And Similar Symptoms
Usage of antipsychotics drugs in Parkinson’s disease patients is complicated because of their tendency to block D2 i.e. dopaminergic receptors, which are responsible to induce dyskinesia and related extra pyramidal symptoms. Antipsychotic drugs highlight significant difference associated with the affinity towards D2 receptors.
Who Are At Risk Of Developing Drug Included Parkinsonism
Some patients may be at a higher risk of developing medication-induced Parkinson
ism than others. Some of the risks include-
Women: Women are seen to be two times as much at risk of having drug inducing Parkinson’s disease than men.
AIDS Patients: People with AIDS are at a higher risk.
Family History: Patients having a family history Parkinson’s disease are at a higher risk of having drug induced Parkinsonism.
Elderly: Since elder people are usually on multiple medicines, they are at risk of having drug induced Parkinsonism.
Cholinesterase Inhibitors Widely Used To Treat Dementia
Cholinesterase inhibitors, widely used to treat dementia, may cause worsened parkinsonism, primarily increased tremor . Large double-blind trials of rivastigmine, a cholinesterase-inhibiting drug, in both dementia with Lewy bodies and Parkinson disease dementia have demonstrated that rivastigmine is well tolerated without significant worsening of motor function overall, although tremor may increase . The other cholinesterase inhibitors have been less well studied but appear to have similar benefits and side effects.
How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue with someone who is experiencing a hallucination or delusion. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Chauncey Spears, Movement Disorders Fellow at the University of Florida, a Parkinson’s Foundation Center of Excellence.
What Are The Treatment Options For Parkinsons Psychosis
Because Parkinson’s drugs can cause psychosis, your doctor will likely start by taking you off your medications, one at a time, or adjusting the dose. Changing your medication may make your movement symptoms worse.
Your doctor will keep adjusting your medication. The goal is to get you to a dose that improves your movement without causing hallucinations and delusions.
If changing your medication doesn’t work, the next step is to go on an antipsychotic medication. These drugs prevent psychosis symptoms by altering levels of chemicals in your brain.
Older antipsychotic drugs can make Parkinson’s movement symptoms worse. Newer drugs, called atypical antipsychotics, are less likely to affect your movement. These drugs are off-label, meaning they’re not approved to treat Parkinson’s specifically. They include:
- clozapine
- quetiapine
In 2016, the Food and Drug Administration approved pimavanserin . It’s the first drug designed specifically to treat Parkinson’s disease psychosis. Nuplazid reduces the number of hallucinations and delusions without affecting movement.
Nuplazid and other newer antipsychotic drugs do carry a black box warning. They can increase the risk of death in older people who have psychosis related to dementia. Your doctor will consider this and other risks before prescribing one of these drugs.
Implications For Clinical Practice And Future Research
In this review, quetiapine has not demonstrated statistically significant efficacy or tolerability, but is associated with troublesome side-effects and high drop-out rates. It is, however, important to note that these studies were small and that there is anecdotal evidence of efficacy. Quetiapine should therefore be used with caution. Olanzapine also requires caution due to an increased risk of parkinsonism and cerebrovascular accidents. Clozapine is associated with an antipsychotic effect. To facilitate its use clinically services need to be developed and integrated to ensure that patients can be appropriately followed-up and monitored. A retrospective chart review of a clozapine clinic for patients with Parkinson’s disease found a 66% response rate to clozapine.Reference Hack, Fayad, Monari, Akbar, Hardwick and Rodriguez30 However, there was a 41% retention rate to the service due to the inconvenience associated with frequent blood monitoring. Pimavanserin is novel treatment that warrants further investigation.
Atypical Parkinsonism Or ‘parkinson’s Plus Syndromes’
“Parkinson’s Plus Syndromes” are less common than Parkinson’s disease.
Some atypical parkinsonism syndromes include:
Multiple system atrophy This is a category of several disorders in which one or more body systems deteriorate.
Your doctor may classify you as having MSA-P, in which parkinsonian symptoms are dominant; or MSA-C, in which dysfunction of the cerebellum is dominant.
The names of some of these syndromes include olivopontocerebellar atrophy , Shy-Drager syndrome , and striatonigral degeneration .
Progressive supranuclear palsy Symptoms of this condition usually begin after age 50 and proceed more rapidly than Parkinson’s disease.
In people with PSP, problems with eye movement can lead to blurry vision. Falls tend to occur early in the course of the disease, and dementia may occur later in the disease.
Corticobasal degeneration This condition may cause jerking and loss of control in a limb, often without weakness in that limb.
If you have this disorder, you may be given Botox to help your limb relax.
Lewy body dementia LBD is the second leading cause of dementia in the elderly, after Alzheimer’s disease.
In this condition, the same Lewy bodies occur in the brain as in Parkinson’s disease, but in multiple areas of the brain.
If you have LBD, you may experience speech problems, hallucinations, and gradual cognitive decline.
Antipsychotics Used For Parkinson’s Despite Warnings
Doctors Still Prescribe Antipsychotics Despite Risks for Some Parkinson’s Patients
July 11, 2011 — Doctors continue to prescribe antipsychotic drugs to their patients with Parkinson’s disease and psychosis, despite “black box” warnings from the FDA linking them to increased risk of death among patients with dementia, a study shows.
A black box warning is the strongest drug warning issued by the FDA.
“My sense is that the black box warnings don’t factor into decision making,” says study researcher Daniel Weintraub, MD, an associate professor of psychiatry at the University of Pennsylvania.
The study is published in the Archives of Neurology.
The black box warning for antipsychotics says the drugs are associated with an increased risk of death for those with dementia, which is common among people diagnosed with Parkinson’s. Some commonly prescribed antipsychotics also worsen symptoms of Parkinson’s.
Risperdal and Zyprexa , for example, are two such drugs, and neither has been shown to be very effective. Yet according to the study, nearly 30% of patients with Parkinson’s and psychosis take them.
Clozaril , the only drug known to be both effective and well-tolerated for treating psychosis in Parkinson’s patients, is prescribed to less than 2% of those with the disease.
“Quetiapine is the No. 1 choice without clear evidence that it’s effective,” says Weintraub.
Biological Basis Of Iatrogenic Movement Disorders
The biological basis of the movement disorders is complex. However, those listed above as secondary to medication are characterised by the action of drugs on central nuclei and in particular pathways and nuclei associated with the basal ganglia, a functional unit located at the base of the forebrain.
The basal ganglia have principal connections to the cortices and thalamus. Although involved in multiple functions including cognition and emotional function, it is their role in the control of involuntary movements that is relevant to this chapter. The other functions, though, are clinically important and discussed elsewhere in this book. At rest, the structures of the basal ganglia can be considered to provide a tonic inhibition of motor activity. This inhibition is released through conscious activity via an increased release of dopamine from the substantia nigra, thereby allowing voluntary control of motor activity in the necessary area.
However, cholinergic pathways elsewhere are involved in cognition, vigilance and emotional modulation and degenerate in Parkinson’s disease – while anticholinergic medication may therefore be associated with an improvement in movements, it is at the expense of deterioration in cognition in this disease, as well as in patients with psychosis, where anticholinergic medication may additionally mediate confusion and psychotic symptoms.
Section Header Managing Psychosis With Medication
Don’t keep hallucinations or delusions a secret from your doctor. Medications — or changes to the medications you take — can help manage Parkinson’s psychosis.
Streamlining your meds. The first thing your doctor may want to do is stop or lower your Parkinson’s medication dose. They may boost dopamine levels in your brain. That improves motor symptoms but can also cause changes in your emotions or the way you act.
Antipsychotics. These medications balance your brain chemicals. Only a few are considered safe for people with Parkinson’s disease. These include quetiapine and clozapine .
Pimavanserin . Another antipsychotic, this first-in-class drug was approved by the FDA in 2016 to treat hallucinations and delusions in Parkinson’s disease linked with psychosis.
If you see a doctor who isn’t part of your usual care team — say, in the emergency room or an urgent care setting — tell them you have Parkinson’s disease and what medications you take for it.
Antipsychotics In Parkinsons A No Win Situation
Date July 29, 2018Author By Eric ChristiansonCategory Uncategorized
Spending a good chunk of my time in geriatrics, we get into these situations where there are options on the table, but we may not like any of them. Selecting antipsychotics in Parkinson’s is one of those crappy situations. If you remember the pharmacology and physiology of Parkinson’s, we have a shortage of dopamine in the brain. This is an oversimplification, but I think it helps create a simple visual. If you remember in schizophrenia, we have an overabundance of dopamine.
In Parkinson’s we naturally try to replace the deficient dopamine stores by giving carbidopa/levodopa , the gold standard in Parkinson’s care at this time. In schizophrenia, we use dopamine blocking agents. These are called antipsychotics. Risperidone, quetiapine, aripiprazole are a few common examples of antipsychotics.
In a patient with Parkinson’s disorder, there may be symptoms of hallucinations and delusions. This may be due to the disease itself and/or it may be due to excessive dosing of Sinemet. In patients that have hallucinations and are receiving Sinemet, the first step is usually to look at the dosing and potentially reduce it. This reduction in Sinemet has the potential to help reduce the hallucinations, but it can also increase the symptoms of Parkinson’s disease. Remember the acronym TRAP for symptoms of Parkinson’s disease .
Parkinsonism Due To Other Neurological Disorders
The following neurological disorders are known to cause parkinsonian symptoms:
Vascular parkinsonism Also known as arteriosclerotic parkinsonism, this condition is caused by multiple small strokes.
The onset of symptoms can be sudden or gradual, and often includes mobility problems in your legs. Symptoms may level off for a period of time.
Vascular parkinsonism has the slowest rate of progression of all atypical parkinsonisms. It doesn’t usually cause tremors, either.
Post-traumatic parkinsonism Also known as post-traumatic encephalopathy or “punch-drunk syndrome,” this condition may be caused by a severe head injury or by frequent head trauma, such as from boxing or football.
Post-traumatic parkinsonism can lead to a type of dementia called chronic traumatic encephalopathy . In March 2016, the National Football League admitted that there might be a link between CTE and head trauma.
Essential tremor This is a tremor that tends to run in families and become worse over time. It’s usually seen most severely in the hands, especially when the hands are moving.
Normal pressure hydrocephalus This condition is caused by an abnormal increase in fluid in the cavities of the brain.
NPH can sometimes be treated by draining the extra fluid into your abdomen using a shunt.
Environmentally Caused Parkinsonism
The following disorders are caused by outside factors like drugs and infection:
The following substances can cause drug-induced parkinsonism:
What Are The Types Of Parkinsons Hallucinations
Hallucinations can affect any of the five senses:
- Sight . Seeing something that isn’t there, such as insects crawling on the walls or a deceased relative.
- Hearing . Hearing voices or sounds that aren’t real.
- Smell . Smelling an odor that isn’t there, like cookies baking or a skunk’s spray.
- Feeling . Feeling imaginary things, like bugs crawling on your skin.
- Taste . Having a strange taste in your mouth that isn’t from something you’ve eaten or a medical condition.
Some people sense the presence of a person or an animal nearby. Others see real objects transform into other things — for example, a vase changes into a dog.
It’s more common to have hallucinations at night, when the darkness creates shadows. Hallucinations can last anywhere from a few seconds to a few minutes.
Early in the disease, most people with Parkinson’s psychosis have insight, which means they understand that what they’re experiencing isn’t real. Later in the disease, often people lose insight and believe that what they see, hear, or feel is real.
Antipsychotics Might Cause Cognitive Impairment
A friend of mine recounted a pretty terrifying description of his experience being on antipsychotics for years as a child:
There are also cases of antipsychotics causing autistic catatonia, in which an autistic person, upon treatment with antipsychotics, suddenly loses speech and motor skills. See examples: personal narrative, case study, case study.
So, a natural question is: does this happen often? Do antipsychotics actually cause cognitive problems?
And here I’m referring to long-term cognitive problems. Many medications, including most atypical antipsychotics, are sedating; nobody thinks as clearly when they’re sleepy. But when you stop taking a sedative, you generally become alert again. Do antipsychotics have any permanent effects?
Now, a major confounder is that schizophrenia causes cognitive impairment in itself, and antipsychotics seem to slightly relieve those problems.
Overall, atypical antipsychotics seem to help cognition in schizophrenia
One study of 533 patients having their first psychotic episode and randomized to either risperidone or haloperidol found that, on both drugs, there were slight but significant improvements in most cognitive tests after 3 months of treatment and patients did not significantly worsen on any tests.
There are dozens of studies like this. A meta-study found that various atypical antipsychotics were found to improve cognitive functioning in roughly half of studies, most of which were short-term .
Typical Vs. Atypical Side Effects
Antipsychotics To Deal With Psychotic Symptoms
Psychotic symptoms remain present in approximately half of the patients dealing with Parkinson’s disease. These symptoms create detrimental effects on the quality of life lead by patients and their caregivers, while result in mortality in some cases. Pathogenesis associated with psychotic symptoms in Parkinson’s disease is complicated and usage of antipsychotics i.e. dopaminergic medications involve many risk factors. Treatment for psychotic symptoms in patients dealing with Parkinson’s disease is complicated because of the property of any antipsychotic medicine to make motor symptoms worse.
Diagnosis Of Dip And The Role Of Dat Imaging
The clinical diagnostic criteria for DIP are defined as 1) the presence of parkinsonism, 2) no history of parkinsonism before the use of the offending drug, and 3) onset of parkinsonian symptoms during use of the offending drug. Since asymmetrical rest tremors are common in many DIP patients and symptoms persist or progress after cessation of the offending drug, patients clinically diagnosed with DIP may include individuals in the preclinical stage of PD whose symptoms were unmasked by the drug.15,41,58,59
DATs are presynaptic proteins in the membrane on terminals of dopaminergic neurons. They take up dopamine from the synaptic cleft projections that extend from the substantia nigra to the striatum. These transporters control dopaminergic transmission by spatial and temporal buffering, rendering the molecule an imaging target in diseases affecting the dopaminergic nigrostriatal pathway. Single-photon-emission computed tomography and positron-emission tomography scans are available using several DAT ligands.6,60 SPECT radioligands include 123I-N-3-fluoropropyl-2?-carbomethoxy-3?-nortropane , 123I-ioflupane, DaTSCAN, and 123I-2?-carbomethoxy-3?-tropane .61 PET scans may be superior to SPECT for imaging DATs, in that the lower energy of positrons provides higher resolution, resulting in better image quality with widespread clinical applications.60 However, most DAT imaging studies, including those in patients with DIP, have utilized SPECT.53,62–64
Can Antipsychotics Cause Parkinsons Disease

Antipsychotics are mainly useful in the management of psychosis, such as disordered thoughts, paranoia, hallucinations, delusions, principally in bipolar disorder and schizophrenia. Doctors usually call them as neuroleptics or major tranquilizers and recommend them to manage various conditions. In addition, such medicines relieve psychosis symptoms on a short-term basis.
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinson’s report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include “delirium,” in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and “isolated minor symptoms” or “minor hallucinations,” including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinson’s. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinson’s not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinson’s is a complex disease and as it progresses the percentages and risk of symptoms will change.
How Can Caregivers Support Their Loved Ones
Caring for someone who sees, hears, or believes things that aren’t real can be very difficult. Try to be as patient and calm as you can.
Avoid arguing with the person. If they still have insight, gently explain that what they’re seeing isn’t real. Tell anyone who cares for or visits your loved one what to expect, and how to respond.
Stay in close contact with the person’s doctor. If their symptoms don’t improve, ask whether they need a medication adjustment.
Check whether the person needs hearing aids or glasses. Poor hearing or vision can sometimes lead to hallucinations. It can also help to turn on bright lights at night, to prevent the shadows that may trigger visual illusions.
Secure any dangerous objects, and keep pathways in the home clear to prevent falls and injuries. If you ever feel like the person is a risk to themselves or others, call their doctor.
Antipsychotics Are Dopamine Blocking Drugs
A few people develop Parkinson’s disease like symptoms after they undergo treatment with specific type of medicines. This type of medicine refers to drug-induced Parkinsonism or DIP i.e. secondary type of Parkinsonism. Specific medicines, including antipsychotics may make the symptoms worse in patients, who already suffer from Parkinson’s disease.
Almost every medicine responsible to create blockage of dopamine in humans may create symptoms related to Parkinson’s disease. Dopamine refers to a brain chemical that mainly controls body movements. Antipsychotics are common types of dopamine blocking drugs, which are useful in the treatment of specific mental illnesses or nausea in its severe form. In less common cases, calcium channel blockers medicines may result in drug induced Parkinsonism. These drugs are helpful in the treatment of high blood pressure, chest pain as well as irregular heart beat rate.
What Side Effects Can Antipsychotics Cause
Every antipsychotic has its own possible side effects. Not everyone who takes antipsychotics will experience side effects, but many people do.
This page lists the most serious side effects that are possible with any antipsychotic drug. Some of these side effects are rare.
- antimuscarinic effects
Certain types of antipsychotic may also have other side effects which aren’t listed here.
Can Drug Induced Parkinsonism Be Prevented
Although there is no surety in the prevention of drug-induced parkinson’s disease, but efforts may be made to check the dosage of drugs so prescribed-
Be Cautious with Antipsychotics: The patient or in some cases the caregiver should make sure that antipsychotic drugs are given at their least effective dosage.
Inform the Doctor: The doctor should be informed well before in case the patient already has symptoms of Parkinson’s disease so that they do not appear to get worse with the starting of some prescribed drugs.
Abrupt Stoppage of Medicine: It is never a wise decision to stop taking a medicine by oneself. It is important to talk to the doctor in case of any concerns.
Treatment Of Parkinsons Disease Psychosis
Andrew Schleisman, PharmD Candidate 2017
Mikayla Spangler, PharmD, BCPSAssociate Professor of Pharmacy Practice
Emily Knezevich, PharmD, BCPS, CDEAssociate Professor of Pharmacy PracticeCreighton University School of Pharmacy and Health ProfessionsOmaha, Nebraska
US Pharm. 2016;41:HS20-HS26.
ABSTRACT: Delusions and hallucinations in patients with Parkinson’s disease, a condition known as Parkinson’s disease psychosis , have historically been treated with clozapine and quetiapine because of their relatively low likelihood of worsening motor symptoms. Although clozapine is considered the drug of choice, it is underused in this population because of the need for frequent monitoring. Quetiapine, on the other hand, is generally first-line treatment despite its questionable efficacy. Consequently, in 2006, the American Academy of Neurology identified a need for the development of a novel antipsychotic with evidence of both safety and efficacy in patients with PDP. Pimavanserin, which has shown promise in clinical trials, recently became the first agent to receive FDA approval for the treatment of PDP.
Key Aspects Of Drug Induced Parkinsonism
- Drug induced Parkinsonism is relatively less likely to produce the problem of tremor than its counterpart idiopathic Parkinson’s disease.
- DIP is highly symmetric, but doctors usually fail to distinguish the 2 syndromes in case of an individual therapy.
- The problem of DIP persists in patients for a few weeks to up to many months even when a patient stops the consumption of respective offending drug.
- Drug induced Parkinsonism has a longstanding and a significant effect on the daily lives of a patient. Hence, doctors should essentially stay cautious while prescribing the drugs of depaminergic receptor blockers to their patients.
Also Read:
What To Do If Your Senior Has Parkinsons
If you notice Parkinson’s-like symptoms in your older adult, the first thing to do is talk with their doctor. The doctor should review their complete medication history and you should let them know about any other symptoms or changes.
Important: Don’t make any changes to medications without doctor approval – that could cause serious problems.
