The 2016 Edition Of The Researchers Days Organised By The Fnr Attracted A Large Audience That Took Part In Fascinating Scientific Experiments And Had The Opportunity To Mingle With The Present Researchers The Luxembourg Parkinson Study Was Of Course There Too With A Booth Called What Parkinsons Disease Feels Like We Took A Closer Look

In order to see how Parkinson’s disease feels like, hundreds of visitors tried on a Parkinson suit which simulates the two most representative motor symptoms of Parkinson’s disease: the muscle rigidity and the tremors. At first glance, the suit looks like a race car driver’s outfit. But together with the elbow and knee bands, and the ankle, wrist and chest weights, this suit shows how rigid the muscles and articulations can be, and how difficult it is for Parkinson’s disease patients to move.
Connect With Other Patients And Share Tips On How To Manage Parkinsons Disease In Our Forums
Up to 44 percent of those with PD have experienced internal tremors. This also is what young-onset Parkinson’s disease can look like. In my early 20s, the tremors continued, and I started having gut troubles. I didn’t think much of it, but looking back on my medical history, my doctor felt confident that PD was playing a quiet role way back when.
Fiona MacDonald, of ScienceAlert, says, “Researchers have noticed that people with Parkinson’s often report … digestive problems up to 10 years before they notice tremors. There’s also evidence that people with Parkinson’s disease have different gut bacteria to other healthy adults.” This also is what PD can look like — but you can’t see it.
I began reading through my journals and began to see my symptoms actually did begin in high school. But they were subtle. They were unpronounced, minimal, silent, unassuming. There was some rigidity. Internal tremors. Gut problems. Not much, but enough to put a connection to. This is what young-onset Parkinson’s disease can feel like.
When I was 32, I was misdiagnosed with lupus and medicated with pills that didn’t make a difference. This is not uncommon.
I don’t have time to wallow in a sea of sorrow over a disease I have, but would rather not have. Since I do have it, I recognize there are times when it’s OK to be treated differently and to need help. It’s really OK, because …
… that’s what PD can look like.
***
Interested In Parkinsons Disease Research Sign Up To Our Forums And Join The Conversation
Don’t give up.
At times, not giving up is easier said than done, especially when you feel alone and abandoned. You may feel your friends and family have abandoned you, but it’s often more a case of them not understanding your new journey. It’s probably best to give those people in your life a free forgiveness pass and move on as you make new friends in the PD community who truly understand what living with PD is like.
Parkinson’s disease causes grief, but we can choose to live joyfully and intentionally in spite of what we feel has been taken from us. It is not a death sentence, and we must learn to readjust to our “new” life. And a new life brings new opportunities. As one person said, never lose hope and keep the faith because God is doing miracles every day and you may be the one He is working through to accomplish just that.
***
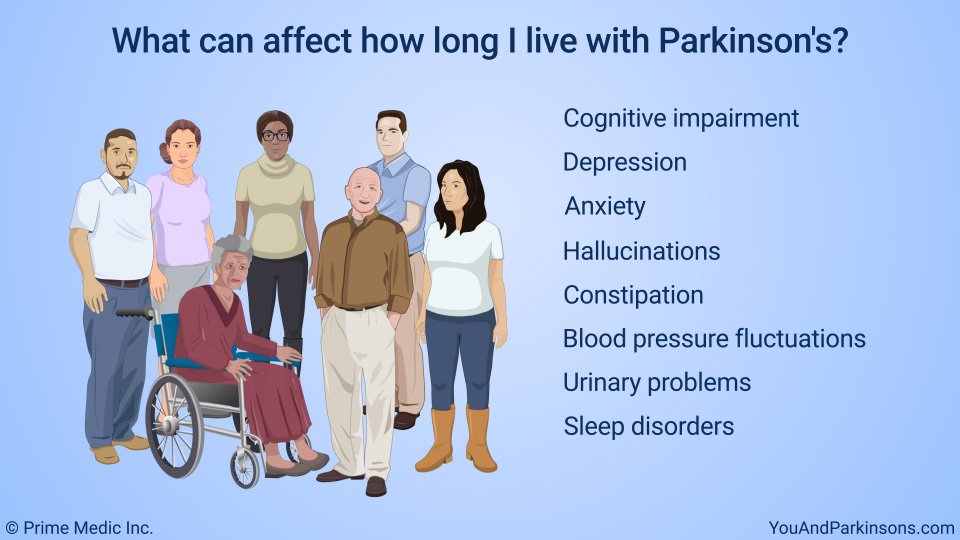
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
Learn More About How Parkinsons Affects Families & Relationships
Much more can be found in a powerful new edition of Davis Phinney Foundation’s free Every Victory Counts® manual. The Every Victory Counts manual has an entire section on Parkinson’s and the family along with tools care partners may find useful along their caregiving journey.
It’s jam-packed with up-to-date information about everything Parkinson’s, plus an expanded worksheets and resources section to help you put what you’ve learned into action. Color coding and engaging graphics help guide you through the written material and point you to complementary videos, podcasts and other materials on the Every Victory Counts companion website. And, it is still free of charge thanks to the generosity of our sponsors.
Request your copy of the new Every Victory Counts manual by clicking the button below.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Your Most Important Relationships: Your Spouse And Yourself
The most important relationship you will have throughout your Parkinson’s is your relationship with yourself. You will need to find ways to nourish your spirit despite much adversity. You will need to find an inner spiritual core that can sustain you while you struggle to maintain a normal life despite Parkinson’s daily intrusions.
No one can tell you how to do this. No one but you knows what really recharges your batteries and imparts to you an inner calm, strength, and fierceness. Whatever that thing is, that thing that gives you strength and a zest for life, you will need to nurture it and rely on it both to fight the illness and to keep your other relationships healthy and nourishing.
The second most important relationship for you, if already part of your life, will be your ‘significant other’ – your spouse, partner or primary companion. This person is the one who will witness your hardest moments and your brightest. You have got to find ways to graciously accept all of the help your companion is willing to give to you. You also need to learn the ropes of coping with Parkinson’s together. As much as you can, help that person learn about Parkinson’s, keep spirits up and remain intimate with you.
Your partner needs you and you need your partner. Rejoice in that fact. Believe it or not, Parkinson’s disease and its challenges can actually deepen and strengthen your relationship.
What Are The Primary Motor Symptoms Of Parkinsons Disease
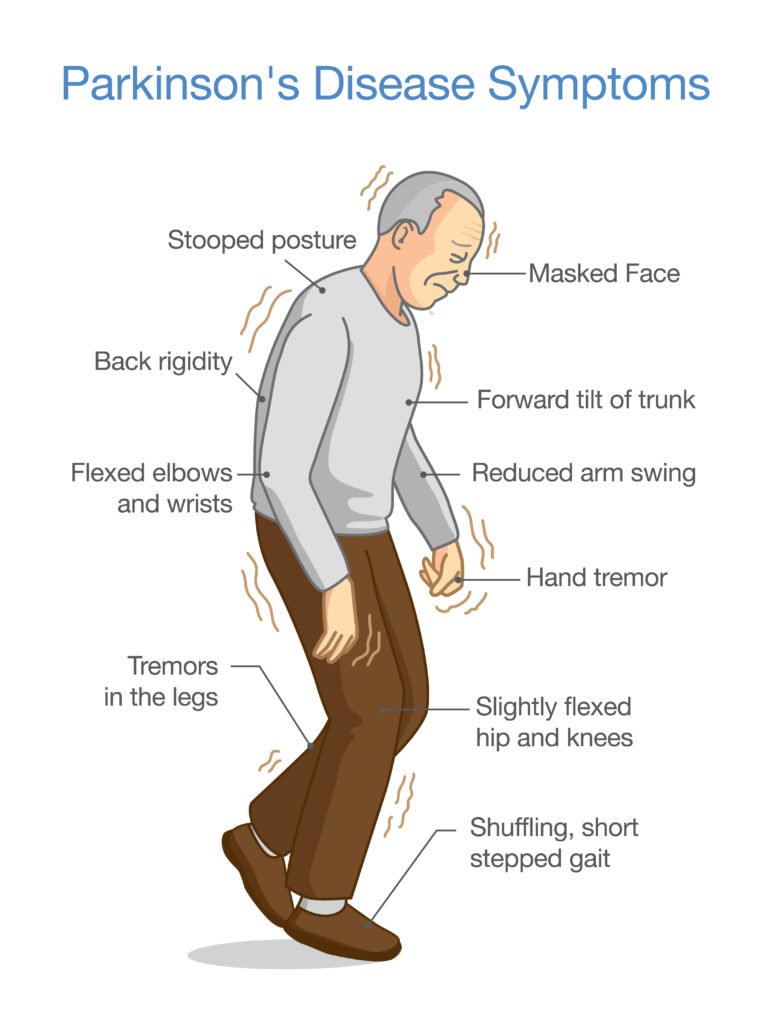
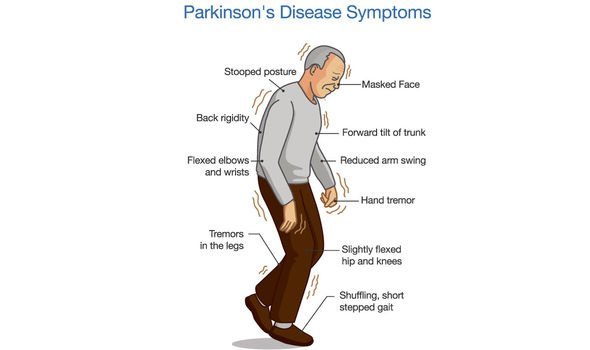
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Read more about Parkinson’s tremors
Rigidity
Bradykinesia
mask-like expression of the face
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
What Does It Really Feel Like To Have Parkinson’s Disease
Rationalizing it away
One morning you look at your right hand and notice that your ring finger is shaking or tremoring by itself. Perhaps your entire hand is shaking. “Oh, it’s just nerves….I’ve been under a lot of stress lately at work and it will settle down once I take a day or two off.” But it doesn’t. In fact, it is getting worse.
Okay, I’ll go see the doctor about it. She’ll probably laugh and tell me it is just my nerves. So, you find yourself sitting on the examination table and your ring finger is at it again. You justify work as being the cause. She looks at it closely and compares with your other hand. She looks at your fingers next to your shaking ring finger. “Sure, they’re not moving, but it’s just nerves, right?” She frowns as she asks you to do some dexterity exercises. She writes down a neurologist’s name and tells you to see him as soon as possible. You’re concerned because SHE is concerned.
Next thing you know, you are on the neurologist’s exam table. He looks at your shaking finger, does more dexterity tests. Checks your reflexes. Watches you walk down the hallway. He sits on his stool and watches your face for a long period of time. You try to tell him, “Doc, really….it’s just nerves” but he continues his exam. He swivels around, writes in your chart and prescribes medication.
The Diagnosis
You make it to the car and sit inside for a few stunned moments. Then you cry.
So What Does it Feel Like? What are some Symptoms besides Shaking?
Is PD fatal?
How Does Exercise Make People With Parkinsons Feel Better
Dear Patrick,
I was diagnosed with PD two years ago. Lately, I’ve been feeling depressed. Any suggestions? Can exercise help?
April B., 58, Los Angeles
Hi April,
I recently wrote an article on the topic of whether or not exercise can help symptoms associated with Parkinson’s disease. The article, which confirmed that it can, received far more readership than normal. This is obviously a subject which resonates with the community.
I reread the article myself yesterday, and I realized that while I answered the question of can exercise help with Parkinson’s disease. I did not discuss how exercise helps those with Parkinson’s live happier and healthier lives.
My focus in this article is to not necessarily discuss the medical benefits, but rather shine a light on the ‘feel better’ aspects of exercise.
The question, “how does exercise help” is as important as “can exercise help?.” In this article I discuss some of the specific ways in which exercise, properly performed, can make you feel better..
Impact on depression
One of the most common symptoms associated with Parkinson’s is depression. A recent study by a movement disorder neurologist at The Ohio State University Wexner Medical Center found that long term exercise improved depression among patients with Parkinson’s. “Our findings demonstrate that long-term group exercise programs are feasible in the Parkinson’s disease population.
The study concluded:
Patrick’s Exercise Recommendations:
Strength Training
Boxing
Yoga
Biking
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
What Medications Are Used To Treat Parkinsons Disease

Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Which Medicines Are Used To Treat Parkinson’s Disease
Guidelines released by the Scottish Intercollegiate Guidelines Network recommend starting with a dopamine agonist, levodopa with a dopa-decarboxylase inhibitor or a monoamine-oxidase inhibitor. Other medicines are also sometimes used, usually in addition to one of these three main types of medication.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
A Day In The Life Of A Parkinsons Disease Sufferer
A Typical Morning
What is Parkinson’s disease?
Parkinson’s disease is largely thought of as a condition of affecting motor control. James Beck, PhD, vice president of scientific affairs for the Parkinson’s Disease Foundation , says that while every case is different, the four cardinal signs of the disease are tremor, muscle rigidity, bradykinesia or akinesia , and problems with walking and balance. These symptoms occur as cells in a part of the brain known as the substantia nigra begin to die off, for reasons that remain unknown. These cells produce an important chemical neurotransmitter known as dopamine. Without dopamine, the brain is unable to control muscle movement. But dopamine is so much more than that. You may have heard it referred to as the “happiness” neurotransmitter, so it’s no surprise that two of the non-motor symptoms of Parkinson’s disease are depression and apathy. Add to that pain from rigid muscles, blood pressure instability, drooling, sweating, constipation, impaired cognition, and absolutely crushing fatigue, and you’ve got yourself a disease that affects just about every facet of life. “A person with mid-stage Parkinson’s disease walking around may look like they are drunk,” says Dr. Beck. “They commonly have slurred speech, and swallowing is another problem, which can contribute to drooling. This constellation of motor effects looks like drunkenness, but their minds are clear.”
Treatment for Parkinson’s
Getting Help
What Not To Say To Someone With Parkinsons Disease

- Reactions 0 reactions
We all do it—we all say that thing, putting our foot in our mouths, and then immediately regret it. We tend to do it more often when we don’t know what is acceptable to say and ask. Every diagnosis, Parkinson’s included, has its own vocabulary and no-no’s when it comes to communication.
The good news is that you’re reading this! That’s a great first step. Read on to see what we’ve found are key questions to avoid when talking with someone with PD.
How Do Symptoms Progress And What Is The Outlook
The symptoms of PD tend to become gradually worse over time. However, the speed of progression varies greatly from person to person. When symptoms first begin, you may not need treatment when symptoms are relatively mild.
Most people with PD can expect to have some time of relatively mild symptoms. Then, when the symptoms become worse, they can expect several years of good or reasonable control of the symptoms with medication. But everyone is different and it is difficult to predict for an individual how quickly the disease will progress. Some people may only be slightly disabled 20 years after PD first begins, whereas others may be very disabled after 10 years.
Research into PD is active. For example, one main aim of research is to find medicines that prevent the damage to the affected cells, rather than just treating the symptoms, which is the main value of treatment at present. Further research on these chemicals continues. Research is underway using stem cell therapy to help treat PD. Other researchers are looking at alpha synuclein, a protein that gathers around the junction between nerve cells and is thought to affect the way messages are conducted between the brain and the nerves controlling movement.
Further reading and references
Tremors Are Not The Only Symptom Of Parkinson’s
Most people don’t know much about Parkinson’s disease beyond the tremors, so it makes sense that they associate PD with tremors. If you can, just give your friend or loved one some space, and if they want to talk about this with you, they will. Or, you could bring it up gently. “I’ve noticed you don’t have tremors. If you’re open to it, I’d be curious to hear more about your experience with Parkinson’s.” This puts the subject in their court, letting them answer when and if they choose.
What Are The Treatments For Parkinson’s Disease
There is no cure for PD, and no treatment prevents the disease from progressing. However, treatments can usually ease symptoms.
- At first, you may not need any treatment when the symptoms are mild. A specialist may simply see you every now and then to monitor how the disease is progressing.
- A medicine that eases symptoms is usually started when symptoms become troublesome.
- Therapies such as physiotherapy, occupational therapy and speech therapy may also be useful as the disease progresses.
- Surgery may be an option for severe cases.
Coping With The Symptoms Of Parkinsons Disease

In addition to medication, there are steps you can take to help manage the symptoms. For example, there are several techniques you can learn that can be useful in overcoming “freezing,” a sudden, but temporary, inability to move. If you experience changes to your voice, there are voice exercises that can help.
Impact Of Parkinson’s Disease On Relationships
If you have Parkinson’s disease, you probably realize that all of your relationships – those with your spouse, partner, family, friends, colleagues, and acquaintances – can change. They can change in a good way or in a bad way .
The most important thing to remember when reflecting on how Parkinson’s influences your relationships is that you have some say in the matter. While you cannot control how people react to your condition, you can speak up when people start to treat you in ways that are incompatible with your dignity or independence.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
Trying Cbd Oil To Manage Parkinson’s Symptoms
Your heart is likely in the right place when you make suggestions to your friends and loved ones who live with PD, but the question, “Have you tried CBD oil?” is one that they’ve likely heard a few too many times.
ParkinsonsDisease.net author Dan Glass lists this as one of biggest pet peeves. He says, “I think people feel that if I use medical marijuana or have it, they can come over and we’ll listen to Bob Marley together while I share it with them.” Not so.
Rather, a more thoughtful way of showing support might be to ask if your friend or loved one would like any suggestions or help with researching therapies. Better still, simply ask how you can show support.
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
What Are The Symptoms Of Parkinson’s Disease
The symptoms of Parkinson’s disease include tremors or trembling ; difficulty maintaining balance and coordination; trouble standing or walking; stiffness; and general slowness.
Over time, a person with Parkinson’s may have trouble smiling, talking, or swallowing. Their faces may appear flat and without expression, but people with Parkinson’s continue to have feelings — even though their faces don’t always show it. Sometimes people with the disease can have trouble with thinking and remembering too.
Because of problems with balance, some people with Parkinson’s fall down a lot, which can result in broken bones. Some people with Parkinson’s may also feel sad or depressed and lose interest in the things they used to do.
The symptoms of Parkinson’s disease appear gradually and get worse over time. But because Parkinson’s disease usually develops slowly, most people who have it can live a long and relatively healthy life.
Caregiving For People Living With Parkinsons
Caring for a loved one with PD can be a challenging job, especially as the disease progresses. Former caregivers of a loved one with PD suggest doing the following : Get prepared, Take care of yourself, Get help , Work to maintain a good relationship with your loved one, and Encourage the person with PD for whom you care, to stay active.
Preparing for caregiving starts with education. Reading this fact sheet is a good start. More resources are available to you in theResources section of this fact sheet. Early Parkinson’s disease usually requires more emotional support and less hands-on care. It is a good time for family members/caregivers to educate themselves about the disease.
How Does Parkinsons Disease Affect The Brain

The part of the brain that is affected is called the basal ganglia, which functions like the autopilot of your brain, facilitating subconscious movements. Because PD causes the brain cells in this deep circuitry to deteriorate, patients’ natural movements become slow and stiff. Many patients describe feeling as if they had aged overnight.
What Are The Symptoms Of Parkinsons Disease
Symptoms of Parkinson’s disease and the rate of decline vary widely from person to person. The most common symptoms include:
Other symptoms include:
- Decreased facial expressions: You may not smile or blink as often as the disease worsens; your face lacks expression.
- Speech/vocal changes: Speech may be quick, become slurred or be soft in tone. You may hesitate before speaking. The pitch of your voice may become unchanged .
- Handwriting changes: You handwriting may become smaller and more difficult to read.
- Depression and anxiety.
- Sleeping disturbances including disrupted sleep, acting out your dreams, and restless leg syndrome.
- Pain, lack of interest , fatigue, change in weight, vision changes.
- Low blood pressure.
Increased Feelings Of Anxiety Or Depression
Anxiety and depression have been linked to Parkinson’s. In addition to movement problems, the disease can also have an impact on your mental health. It’s possible that changes in your emotional well-being can be a sign of changing physical health as well.
If you are more anxious than usual, have lost interest in things, or feel a sense of hopelessness, talk to your doctor.
Coping With The Side Effects Of Medications
Levodopa-carbidopa therapy is the most effective treatment for alleviating the motor symptoms of PD, however, long-term treatment with levodopa may cause dyskinesia . Dyskinesia can greatly impact a person’s quality of life, and some people find it very disturbing. While there are currently no treatments for dyskinesia, it is an ongoing area of research. For those people who experience dyskinesia, medications may be adjusted or deep brain stimulation may be an option.2,3
Some medications used to treat PD can cause impulse control disorders, behavioral disorders in which the person acts out repetitively, excessively, and compulsively in ways that interfere with major areas of life functioning. The most common impulse control disorders seen in people with PD are excessive shopping, unusual or increased sexual behavior, compulsive gambling, and compulsive eating. Identification and treatment of these behaviors is critical as they can have devastating effects on the patient’s and caregiver’s lives.1
