Caregiving In The Late Stages Of Parkinsons Disease
In late-stage PD, patients have significant mobility challenges. Caregivers likely need to provide more hands-on assistance to help them get around the house. Its important that caregivers learn safe and effective methods to provide help without injuring themselves. Physical therapists can be a great resource to assess an individual situation and teach effective ways of giving assistance.3
Freezing, a sudden but temporary inability to move, can become more common in late-stage PD. Freezing often happens when initiating movement or navigating around obstacles, and freezing episodes contribute to falls. Caregivers can help their loved one overcome freezing by providing a visual cue to step over, like a laser pointer, or using music or rhythm for the person with PD to walk to.3
Late stage PD can make daily activities, such as getting dressed, much more challenging. Caregivers can make getting dressed easier by ensuring adequate time to account for slow movement, choosing a time when medications are “on” and working well, and assembling all necessary items close to the person. Allowing the person with PD to do as much as they can gives them a sense of participation in the process.3
Management Of Gait And Balance Problems
Gait problems are mostly unresponsive to Parkinsons medication. However, physiotherapy and occupational therapy can be useful in the management of gait problems. Physiotherapists can help develop specific exercise plans focusing on breaking down the walking motion into small, discrete steps that are consciously executed by the patient following verbal and non-verbal cues.
Some physiotherapists can devise special cues to facilitate movement and manage the freezing of gait symptoms. These can include asking the patient to step over imaginary lines and using rhythmic music as a cue to initiate movement.
The use of mobility aids and assistive devices can also alleviate some gait problems. It is important to consult with a physiotherapist and occupational therapist to determine which devices are best for the patient. It is important to consult with a neurologist who can refer the patient to a qualified physiotherapist.
Parkinsons News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis, or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health providers with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Also Check: Stage 5 Parkinson’s Disease Life Expectancy
What Causes Parkinsons Disease
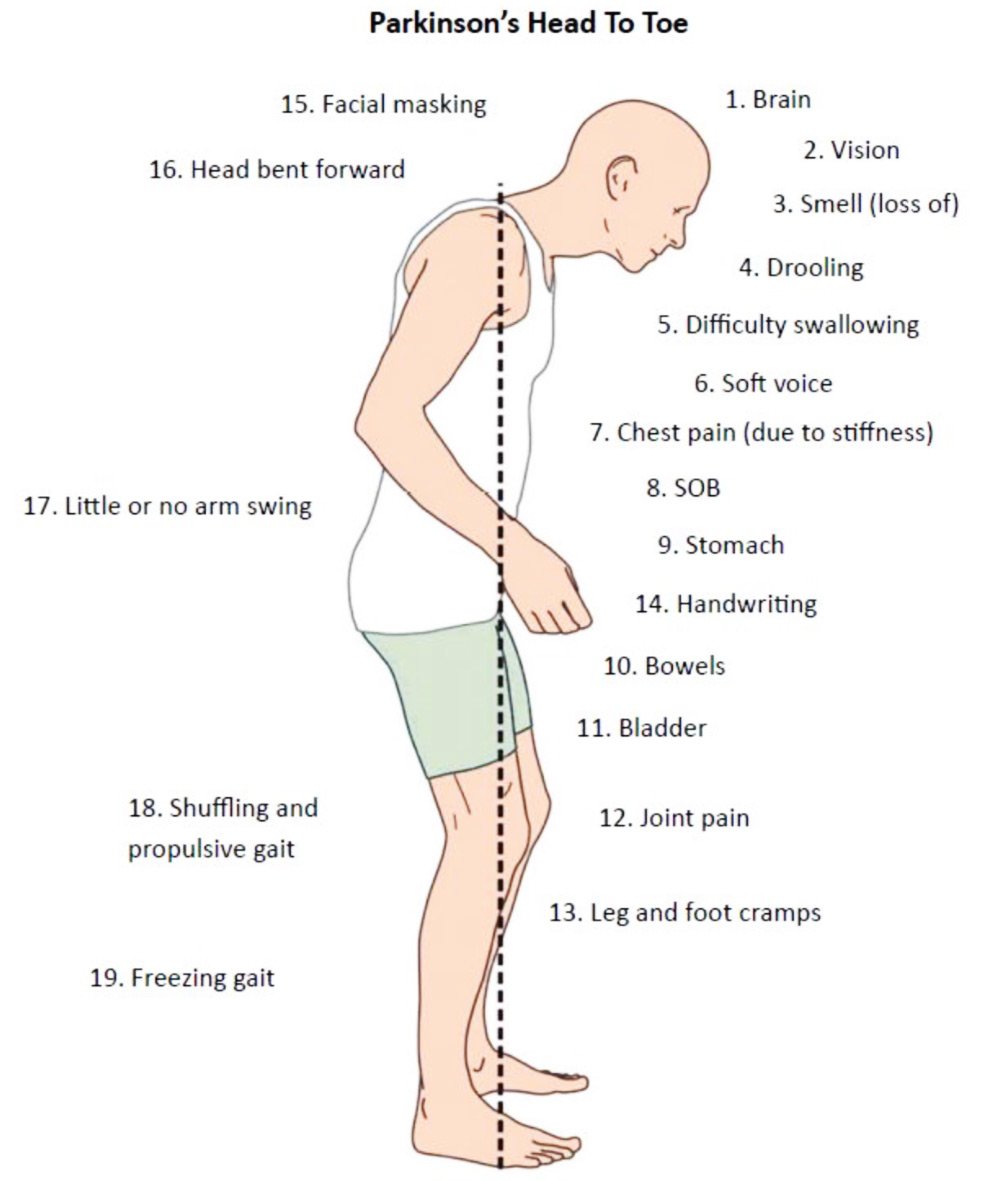
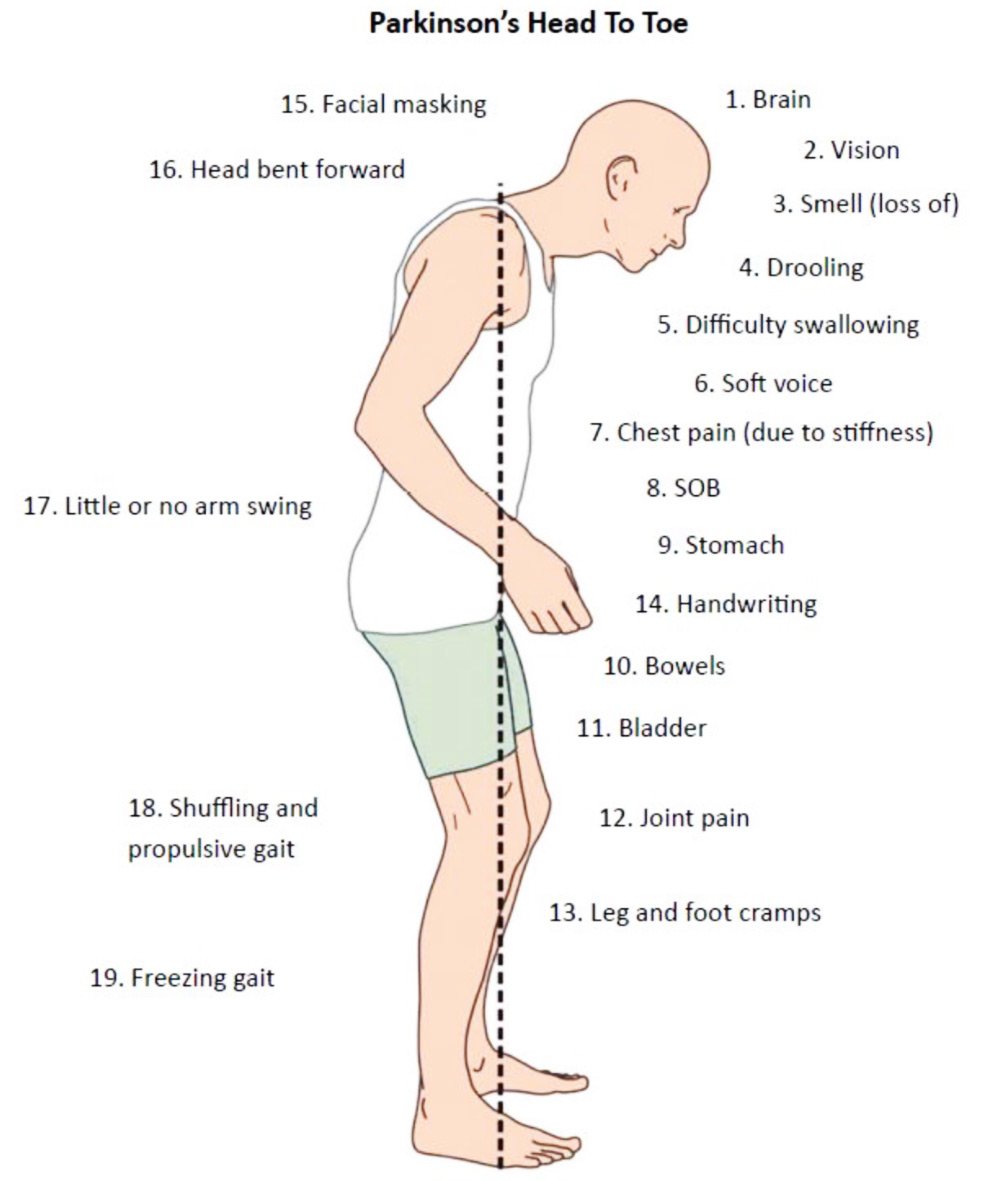
Parkinsons disease occurs when nerve cells in an area of the brain called the substantia nigra become impaired or die. These cells normally produce dopamine, a chemical that helps the cells of the brain communicate . When these nerve cells become impaired or die, they produce less dopamine. Dopamine is especially important for the operation of another area of the brain called the basal ganglia. This area of the brain is responsible for organizing the brains commands for body movement. The loss of dopamine causes the movement symptoms seen in people with Parkinsons disease.
People with Parkinsons disease also lose another neurotransmitter called norepinephrine. This chemical is needed for proper functioning of the sympathetic nervous system. This system controls some of the bodys autonomic functions such as digestion, heart rate, blood pressure and breathing. Loss of norepinephrine causes some of the non-movement-related symptoms of Parkinsons disease.
Scientists arent sure what causes the neurons that produce these neurotransmitter chemicals to die.
How Long Does It Take To Get Good At Shuffling
I would say 23 months of practice would get you really good. After that you would move on to flaps and carry overs and eventually pull backs and youll be a master tapper in no time. Learning shuffles can be really frustrating but once you get them down to a science, youll begin to excel immensely.
You May Like: Lifespan Of Someone With Parkinson’s
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
How Is Parkinsons Disease Diagnosed
Diagnosing Parkinsons disease is sometimes difficult, since early symptoms can mimic other disorders and there are no specific blood or other laboratory tests to diagnose the disease. Imaging tests, such as CT or MRI scans, may be used to rule out other disorders that cause similar symptoms.
To diagnose Parkinsons disease, you will be asked about your medical history and family history of neurologic disorders as well as your current symptoms, medications and possible exposure to toxins. Your doctor will look for signs of tremor and muscle rigidity, watch you walk, check your posture and coordination and look for slowness of movement.
If you think you may have Parkinsons disease, you should probably see a neurologist, preferably a movement disorders-trained neurologist. The treatment decisions made early in the illness can affect the long-term success of the treatment.
Also Check: Parkinson Symptoms Come And Go
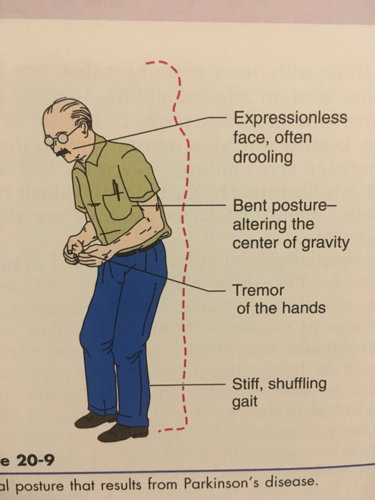
What Is Parkinsonian Gait
Parkinsonian gait is a defining feature of Parkinsons disease, especially in later stages. Its often considered to have a more negative impact on quality of life than other Parkinsons symptoms. People with Parkinsonian gait usually take small, shuffling steps. They might have difficulty picking up their feet.
Parkinsonian gait changes can be episodic or continuous. Episodic changes, such as freezing of gait, can come on suddenly and randomly. Continuous changes are changes in your gait that happen all the time while walking, such as walking more slowly than expected.
Why Is My Ipod Touch Shuffling Songs
Reboot. If your iPod continues to shuffle, turn your iPod off and then turn it back on. Rebooting your iPod may free up shuffling and allow your unit to function normally. If the shuffling continues to be a problem, you may want to consider checking Apples website for new firmware updates to correct the problem.
You May Like: What Is The Life Expectancy Of Someone With Parkinson’s Disease
How Quickly Do Parkinson’s Symptoms Progression
In most cases, symptoms change slowly, with substantive progression taking place over the space of many months or years. Many people with PD have symptoms for at least a year or two before a diagnosis is actually made. The longer symptoms are present, the easier it is to predict how a person with PD will do over time.
Walking With Parkinsons: Freezing Balance And Falls
Parkinsons disease can change the way a person walks. Movement Symptoms like stiff muscles, rigidity and slow movement make it harder to take normal steps. In fact, short, shuffling steps are a common sign of PD, as is freezing, the feeling that your feet are stuck to the floor, for people with mid-stage to advanced PD.
On their own, these changes are distressing enough. But add the fact that Parkinsons affects balance and they also become dangerous, putting people with PD at risk of falling. The good news is that with exercise and physical therapy, people with PD can improve their balance. What can you do to minimize freezing and avoid falls? Read on to find out.
The following article is based on the latest research and a Parkinsons Foundation Expert Briefings about Parkinsons-related freezing, balance and falls hosted by Fay B. Horak, PhD, PT, Professor of Neurology at the Oregon Health & Science University, a Parkinsons Foundation Center of Excellence.
Recommended Reading: How To Use Hemp Oil For Parkinson’s
What Is Lewy Body Dementia
Lewy body dementia , is a common form of dementia combining Alzheimers-like cognitive symptoms and Parkinsons-like motor issues. A neurodegenerative disease, it is the second most prevalent type of dementia after Alzheimers disease. Combining cognitive symptoms similar to Alzheimers with the motor features of Parkinsons, LBD is estimated to affect 1.3 million people in the United States.
The diseases name refers to abnormal protein deposits that occur in the brain discovered by neurologist Dr. Frederic Lewy. These Lewy body inclusions are present in both Parkinsons disease and LBD. Lewy body dementia refers to both Dementia with Lewy Bodies and Parkinsons disease Dementia, which are pathologically similar.
Associations Among The Different Gait Features
One question that has often piqued the interest investigators of gait dynamics is the role of stride length ., To paraphrase, if stride length is a fundamental property of gait, perhaps other features depend, to a large degree, on this characteristic. Table summarizes the associations between different gait features among 118 patients with varying degrees of PD . A strong correlation between gait speed and stride length is seen, as expected. Measures of gait variability are moderately associated with gait speed and stride length, i.e., subjects who had a higher gait speed tended to have lower stride-to-stride variability however, less than 25% of the variance in variability could be explained by stride length. Further, the fractal scaling index was not significantly correlated with variability, gait speed, or stride length. We also confirmed that compared to age-matched healthy controls , all of these measures were significantly altered in the patients with PD .
You May Like: Parkinson’s Short Term Memory Loss
What To Expect In The Late Stages Of Parkinsons Disease
The late stages of PD are medically classified as stage four and stage five by the Hoehn and Yahr scale:
- Stage Four of Parkinsons Disease In stage four, PD has progressed to a severely disabling disease. Patients with stage four PD may be able to walk and stand unassisted, but they are noticeably incapacitated. Many use a walker to help them. At this stage, the patient is unable to live an independent life and needs assistance with some activities of daily living. The necessity for help with daily living defines this stage. If the patient is still able to live alone, it is still defined as Stage Three.
- Stage Five of Parkinsons Disease Stage five is the most advanced and is characterized by an inability to arise from a chair or get out of bed without help. They may have a tendency to fall when standing or turning, and they may freeze or stumble when walking. Around-the-clock assistance is required at this stage to reduce the risk of falling and help the patient with all daily activities. At stage five, the patient may also experience hallucinations or delusions.1,2
Can Parkinsons Disease Be Prevented
Unfortunately, no. Parkinsons disease is long-term disease that worsens over time. Although there is no way to prevent or cure the disease , medications may significantly relieve your symptoms. In some patients especially those with later-stage disease, surgery to improve symptoms may be an option.
Also Check: Cardinal Features Of Parkinson’s
Baseline Brain Perfusion In Parkinson’s Disease Patients
The Parkinson’s disease patients showed a reduction in HMPAO uptake in the parieto-occipital areas during rest, as reported previously . Since the subjects kept their eyes open during the rest, this might reflect possible involvement of the retina in Parkinson’s disease . Otherwise, the present patients might have been affected by cortical Lewy body pathology, which has been reported frequently to involve clinically diagnosed idiopathic Parkinson’s disease . This is implicated by the fact that the hypoperfusion pattern in the present patients resembles the hypometabolic pattern seen in patients with dementia with Lewy bodies .
Neural substrates underlying locomotion on treadmill
Dorsal brainstem
Cortical motor areas
Various gait disorders are ascribed to cerebral cortical lesions in humans, especially those involving the frontal lobe. The present study showed gait-induced activation in most of the known motor-related cortical areas , supporting the view that the projections from the primary motor areas, the lateral premotor cortex, the SMA and the anterior cingulate cortex to the brainstem reticular formation may provide parallel inputs to maintain gait .
Other areas
Gait And Balance Problems
Parkinsons disease is a neurodegenerative disorder characterized by progressive damage to dopamine-producing nerve cells in a specific region of the brain. Dopamine is a neurotransmitter, or cell signaling molecule, that relays information between nerve cells and muscles. One of the most debilitating effects of Parkinsons disease is the loss of coordination and control in body movements, which in many cases leads to severe walking disabilities.
Read Also: How To Take Mannitol For Parkinson’s
Why Do Seniors Develop A Shuffling Gait
By Sue Arsenault 9 am on December 13, 2018
As seniors reach the golden years, they sometimes develop a shuffling gait. While family caregivers may view this development as normal, any changes in your aging loved ones gait shouldnt be ignored. Your loved ones tendency to drag his or her feet could be linked to one of the following issues that needs to be addressed right away.
Vertical Ground Reaction Force
In normal gait, the vertical ground reaction force plot has two peaks â one when the foot strikes the ground and the second peak is caused by push-off force from the ground. The shape of the vertical GRF signal is abnormal in PD. In the earlier stages of the disease, reduced forces are found for heel contact and the push-off phase resembling that of elderly subjects. In the more advanced stages of the disorder where gait is characterized by small shuffling steps, PD patients show only one narrow peak in the vertical GRF signal.
Read Also: Is Parkinson Hereditary
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
Does Parkinson’s Affect Your Walking
4.9/5Parkinson’stheParkinson’saffect yourwalkingaffectParkinson’sread here
Certain exercises may be helpful for specific motor symptoms of Parkinson’s:
- For balance, consider tai chi and yoga.
- To improve coordination and agility, look into dancing or boxing.
- For significant balance problems or limited mobility, seated aerobic exercises can give a challenging workout that raise the heart rate.
One may also ask, how does Parkinson’s affect mobility? The most common Parkinson’s disease symptoms affect mobility or motor skills, in various parts of the body, but many people have non-motor symptoms as well. Rigidity , which may affect mobility, daily tasks such as getting dressed , and cause musculoskeletal pain and discomfort.
Likewise, why do Parkinson’s patients shuffle?
Parkinsonian gait is a defining feature of Parkinson’s disease, especially in later stages. It’s often considered to have a more negative impact on quality of life than other Parkinson’s symptoms. People with Parkinsonian gait usually take small, shuffling steps. They might have difficulty picking up their feet.
How does Parkinson’s affect movement?
Parkinson’s disease is a type of central nervous system disorder that affects your movement, causing symptoms such as tremors, slowness, stiffness, and more. These involuntary movements begin, in part, in the brain, where the production of dopamine is impaired.
Recommended Reading: Sam Waterston Parkinson’s 2018

