Infectionrelated Exacerbations Are Associated With Prolonged Neurological Deficit
We observed a significantly increased risk of major long exacerbations during the ARP. Of 56 major long exacerbations, 21 started during and 35 outside the ARP, with yearly exacerbation rates of 0.9 and 0.3, respectively, resulting in a 2.7 times higher exacerbation rate in the ARP . The yearly exacerbation rates for major short exacerbations during and outside the ARP were equal .
Exacerbations leading to sustained deterioration were even more significantly associated with infections. The rate ratio for sustained exacerbations with onset during the ARP versus exacerbations with onset outside the ARP was 3.8, whereas exacerbation rates for nonsustained exacerbations showed no difference between ARP and nonARP .
Goldstein Ni1 Golubev Vl2 And Goldstein Rn1*
*Corresponding author:Received:Accepted:
Cite this as
Main article text
Multiple Sclerosis is one of the most common chronic demyelinating diseases of the central nervous system. The disease affects and relatively quickly leads to disability in mainly people 15-40 years of age. The development of MS can occur progressively or with exacerbations and remissions. The pathogenesis of the disease is based on an autoimmune process directed against myelin or myelin-producing CNS oligodendrocytes. In recent years, in the mechanisms of death of myelin-synthesizing oligodendrocytes, more and more attention has been paid to metabolic shifts. An important role is played by the activation of astro- and microglia, impaired neurotransmitter metabolism and apoptosis. In the occurrence and enhancement of these neurometabolic changes, an important role is played by the enhancement of the endogenous processes of lipid peroxidation and the suppression of antioxidant systems .
Thus, the therapeutic effect of Parkon develops due to a complex modulating effect on the basic physiological and biochemical processes in various brain structures. All these properties of Parkon can contribute to the slowing of the pathological process, reducing the severity and duration of exacerbations, as well as reduce the external manifestations of MS. This article presents the results of the first clinical study of the efficacy and clinical safety of Parkon in patients with MS.
What You Can Expect
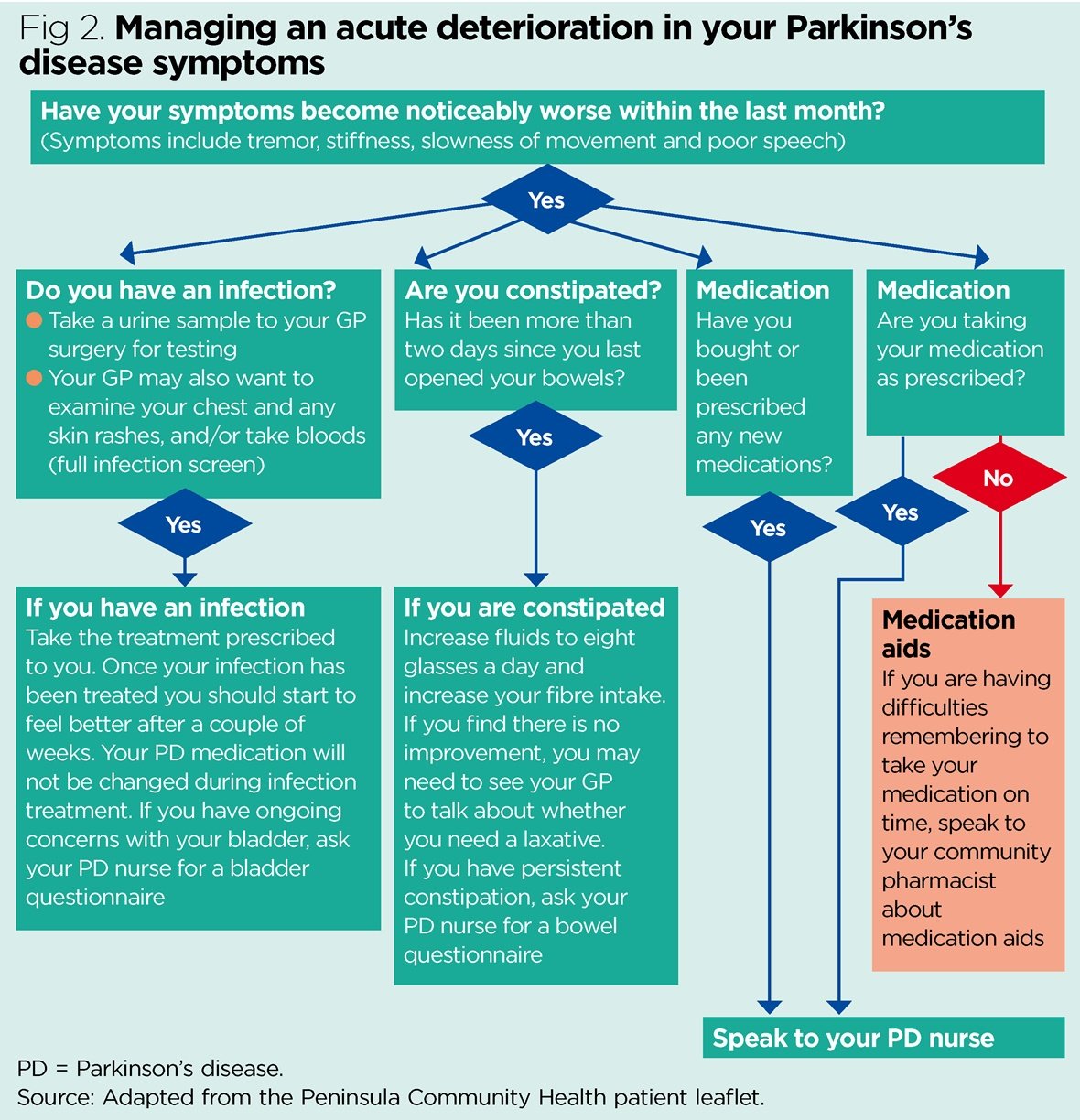
Parkinson does follow a broad pattern. While it moves at different paces for different people, changes tend to come on slowly. Symptoms usually get worse over time, and new ones probably will pop up along the way.
Parkinsonâs doesnât always affect how long you live. But it can change your quality of life in a major way. After about 10 years, most people will have at least one major issue, like dementia or a physical disability.
You May Like: What Famous Person Has Parkinson’s Disease
Viral Infections Exacerbate Active Eae
In order to study how peripheral infection can exacerbate MS, some have attempted to model the effect using the various EAE model systems. The results from these studies demonstrate that peripheral infection can exacerbate the pathogenesis of EAE. Of relevance is one study that investigated the role of murine gammaherpesvirus infection on the pathogenesis of relapsing-remitting EAE in SJL mice. The results demonstrate that infection with live HV-68 but not UV-inactivated virus exacerbated the disease course. Importantly, this effect was not attributable to viral infection of the CNS and could be recapitulated following adaptive transfer of encephalitogenic MBP-specific T-cells from non-infected animals into animals that were infected with HV-68 several days prior to transfer . However, a follow-up study by Casiraghi et al. found that infection with HV-68 5 weeks prior to EAE induction was capable of exaggerating the pathogenesis of active EAE in a manner that was independent of viral reactivation but was associated with heightened T-cell responses within the CNS . Notably, it was concluded that HV-68 was capable of altering antigen-presenting cells in such a way that infection promoted IFN production from encephalitogenic T-cells . The combined results from both studies indicate that reactivation of herpes viruses may not be required to influence the pathogenesis of EAE. However, the effect of EBV reactivation on the pathogenesis of human MS remains to be determined.
What Are Common Signs And Symptoms Of Restless Legs
People with RLS feel the irresistible urge to move, which is accompanied by uncomfortable sensations in their lower limbs that are unlike normal sensations experienced by people without the disorder.; The sensations in their legs are often difficult to define but may be described as aching throbbing, pulling, itching, crawling, or creeping.; These sensations less commonly affect the arms, and rarely the chest or head.; Although the sensations can occur on just one side of the body, they most often affect both sides.; They can also alternate between sides. The sensations range in severity from uncomfortable to irritating to painful.
Because moving the legs relieves the discomfort, people with RLS often keep their legs in motion to minimize or prevent the sensations.; They may pace the floor, constantly move their legs while sitting, and toss and turn in bed.
A classic feature of RLS is that the symptoms are worse at night with a distinct symptom-free period in the early morning, allowing for more refreshing sleep at that time.; Some people with RLS have difficulty falling asleep and staying asleep.; They may also note a worsening of symptoms if their sleep is further reduced by events or activity.
People with RLS can sometimes experience remissionsspontaneous improvement over a period of weeks or months before symptoms reappearusually during the early stages of the disorder.; In general, however, symptoms become more severe over time.
Recommended Reading: Can Parkinson’s Come On Quickly
How Is Bullous Pemphigoid Diagnosed
The diagnosis of Bullous Pemphigoid may include:
- Usually the physician is able to diagnose Bullous Pemphigoid by examining the skin condition
- Skin biopsy: A small sample of the blister may be taken to confirm the diagnosis. The tissue sample is then sent to the laboratory to be examined by a pathologist under the microscope
- Antibodies can also be shown to be circulating in blood
Many clinical conditions may have similar signs and symptoms. Your healthcare provider may perform additional tests to rule out other clinical conditions to arrive at a definitive diagnosis.
Infections And Subclassification Of Exacerbations
A total of 167 infections was recorded in 86% of the patients, an average of 1.4 infections per year. No significant difference in the yearly incidence rate for infections was found between patients with a low and a high baseline level of impairment . Of all infections, 77% were characterized by upper respiratory tract symptoms, 16% by gastrointestinal symptoms and 7% by urinary tract symptoms. In 25% of the infections, patients reported fever at some point during the course of illness.
A total of 145 exacerbations was recorded, occurring in 58 of the 73 patients and resulting in an average exacerbation rate of 1.2 per year . Fiftyfour per cent of all exacerbations were classified as major and 46% as minor. Of all major exacerbations, 72% were long and 28% short. Thirtytwo of the 54 major long exacerbations lasted >3;months and were classified as sustained, whereas 22 resolved within 3;months after onset . For two of the 56 major long exacerbations, there was insufficient followup time for adequate classification, because they occurred towards the end of the study period. Fortysix out of the total number of 145 exacerbations started during the ARP. These exacerbations started on average 9.5 days after the clinical onset of infection, only 10 exacerbations preceding the onset of infection. Fortyfive of all 167 observed infections were associated with an exacerbation.
Recommended Reading: Can Parkinson’s Cause Leg Swelling
What Is Seborrheic Dermatitis
Seborrheic dermatitis may occur on the scalp but also onsuch oily skin areas as inside or behind the ears, on the creases at thesides of the nose, or on the eyelids, eyebrows, lips, face, upperchest, or back. It also causes scales that are white or yellow. Theaffected skin may also be reddened, and it may itch.
If one family member has seborrheic dermatitis, others aremore likely to develop it. The condition seems to worsen under certaincircumstances, such as stress, fatigue, extreme weather conditions,excess skin oiliness, failure to bathe or shampoo daily, use ofalcohol-containing lotions, or presence of acne or obesity.
Future Prospects: Questions To Be Answered
The link between PD and RLS has yet to be clearly determined with clinical association studies differing widely in their findings, with some finding the incidence of RLS to be much greater in PD patients, and others finding no difference from that in the general population. These discrepancies could be addressed with prospective long-term clinical studies of PD patients who develop RLS and vice versa, with documentation of exposure to dopaminergic therapies.
With the exception of the parkin mutation, genetic studies have been failed to reveal any associations. We propose that population based genetic association studies of PD plus RLS and linkage studies of PD plus RLS as well as comparative studies of PD vs. PD-RLS vs. RLS should be conducted.
Sonographic studies reveal notable differences between PD and PD-RLS patients. Functional MRI studies have yet to focus on those patients with PD-RLS. Prospective functional imaging studies of PD vs. PD-RLS are needed to better understand the mechanisms involved in these disorders. To our knowledge, there have been no pathological studies looking at patients with PD-RLS. Establishing the pattern of decreased D2 receptor density in PD vs. PD and RLS vs. RLS may be valuable in understanding common pathophysiology. The reports purporting to DBS and RLS are conflicting, and more studies need to be done to clarify the effect, with attention to adjustments in dopaminergic medications.
Recommended Reading: Does Parkinson’s Affect Memory
What To Do After A Flare
You can recover fully after a relapse, but it might take weeks or months to get over all your symptoms. If you had a lot ofÂ;nerve damage, some symptoms might not fully go away.
You may need extra help to get back to your normal life. A rehab program can put you back on track. Your rehab team will help you with:
Season Does Not Influence The Incidence Of Arp Exacerbations
To assess whether ARP exacerbations have a specific seasonal preference, we calculated the monthly incidence rate for infections, exacerbations and ARP exacerbations. The monthly incidence of infections was 0.11 ± 0.026, with the lowest incidence in July compared with the rest of the year . As expected in this geographical area, there were significantly fewer infections in the summer months than in the autumn months . The average monthly incidence of exacerbations was 0.1 ± 0.021 and showed a peak in September, which did not reach significance compared with the rest of the year . ARP exacerbations occurred with a constant average rate of 0.03 ± 0.014 per month without any peak during the year.
Don’t Miss: What Is The Difference Between Parkinson’s Disease And Alzheimer’s Disease
Remission From Parkinsons Without Drugs
I was shocked to find out that my high-school friend Roger Long had Young-Onset Parkinsons.; Were not THAT old!
But I was super-happy to discover that his Parkinsons is in remission because of his thinking outside the box.
Not only that, but Roger climbed to the top of Mt. Kilimanjaro a few months ago without being on any medication!;
Roger and I both looked at neurological disorders ) as related to autism because of the neurological damage associated with all of them.
Once I began researching the causes of my sons SPD, I came across all sorts of information about neurological disorders.
Autism, PDD-NOS, SPD and ADHD as well as schizophrenia, bipolar disorder, depression, anxiety and OCD are the classic childrens neurological disorders.
Then there are the adult neuro disorders:; Parkinsons, Alzheimers, ALS, multiple sclerosis and Lyme.
Did you ever stop to think that there might be a connection among all of these disorders?; I did, and so did Roger.
We both thought that if kids can be recovered from autism with diet and if these orders are related in that they are all neurological disorders, wouldnt it be possible to recover from Parkinsons and SPD?
So thats what Roger did.
That is, after he spent 8 years on pharmaceuticals that left him bloated and addicted to food because of their ability to antagonize dopamine.
Roger put up with the side effects because he, like most people, believed that medication was the only way, even if it wasnt the best way.
DISCLAIMER
Do Ms And Als Have The Same Risk Factors
Age is risk factor for both ALS and MS, but ALS usually is diagnosed in older individuals , with an average age of onset of 55. While MS is diagnosed in a younger population .
ALS is more common in men by about 20%, while MS is about 2 to 3 times more likely to develop in women.Heredity plays a significant role in some individuals that develop ALS . MS is not considered to be a hereditary disease, but new data may modify this conclusion.
In addition, being a member of the military raises the risk of developing ALS. However, military service is not considered a risk factor for MS.
If you have an identical twin with MS, there is a 30% chance for you to develop MS.
You May Like: How Does Parkinson’s Disease Cause Death
How Are Als And Ms Diagnosed
To make a diagnosis, your doctor will ask for detailed information about your symptoms and your health history. There are also tests they can perform to help make a diagnosis.
If ALS is suspected, your doctor may order electrodiagnostic tests, such as an electromyography or a nerve conduction study.
These tests provide information on the transmission of nerve signals to your muscles and can show certain patterns that are consistent with a diagnosis of ALS.
A muscle or nerve biopsy may also be recommended for evaluation of ALS.
Your doctor may also order blood and urine samples, or perform a lumbar puncture to examine your spinal fluid.
MRI scans or X-rays may be ordered as well. If you have an MRI scan, you may have special images ordered to increase visualization of demyelinating areas in the brain and spine.
Doctors can use MRI results to distinguish between MS and ALS. MS targets and attacks myelin in a process called demyelination.
Demyelination prevents the nerves from performing as well as they once did, and it can be detected by an MRI scan.
On the other hand, ALS attacks the motor neurons, which doesnt appear on brain or spine MRIs.
Theres no cure for either condition, but treatments are available.
Remission Of Cognitive Deficits In Parkinsons Disease: Recovery From A Nonamnestic Mild Cognitive Impairment Or Psychiatric Symptoms Remission
Jonas Jardim de Paula
1Laboratório de Investigações Neuropsicológicas , Universidade Federal de Minas Gerais, 31270-901 Belo Horizonte, MG, Brazil
2INCT de Medicina Molecular, Faculdade de Medicina, Universidade Federal de Minas Gerais, Avenida Alfredo Balena 190, 30130-100 Belo Horizonte, MG, Brazil
3Instituto Jenny de Andrade Faria de Atenção à Saúde do Idoso, Hospital das Clínicas, Universidade Federal de Minas Gerais, 31270-901 Belo Horizonte, MG, Brazil
4Departamento de Clínica Médica, Faculdade de Medicina, Universidade Federal de Minas Gerais, 31270-901 Belo Horizonte, MG, Brazil
5Departamento de Saúde Mental, Faculdade de Medicina, Universidade Federal de Minas Gerais, 31270-901 Belo Horizonte, MG, Brazil
Academic Editor:
Abstract
1. Introduction
The concept of mild cognitive impairment in Parkinsons disease refers to a cognitive disorder where the subject shows an objective impairment in one or more cognitive domains and lack of or only mild functional impairment . Due to the absence of uniformity in diagnostic criteria, there is little agreement in the literature on what subtype of MCI is the most frequent in Parkinsons disease.
2. Case Description and Clinical Exam
| Measure |
3. Neuropsychological Assessment
3.1. Cognitive Status and Global Measures
The Dementia Rating Scale total score was chosen for global cognitive screening, since this test was well suited for the diagnosis of cognitive impairment in Parkinsons disease .
3.2. Episodic Memory
3.3. Language
You May Like: How To Lose Weight With Parkinson’s Disease
What Causes Restless Legs Syndrome
In most cases, the cause of RLS is unknown .; However, RLS has a genetic component and can be found in families where the onset of symptoms is before age 40.; Specific gene variants have been associated with RLS.; Evidence indicates that low levels of iron in the brain also may be responsible for RLS.
Considerable evidence also suggests that RLS is related to a dysfunction in one of the sections of the brain that control movement that use the brain chemical dopamine.; Dopamine is needed to produce smooth, purposeful muscle activity and movement.; Disruption of these pathways frequently results in involuntary movements.; Individuals with Parkinsons disease, another disorder of the basal ganglias dopamine pathways, have increased chance of developing RLS.
RLS also appears to be related to or accompany the following factors or underlying conditions:
- end-stage renal disease and hemodialysis
- iron deficiency
- certain medications that may aggravate RLS symptoms, such as antinausea drugs , antipsychotic drugs , antidepressants that increase serotonin , and some cold and allergy medications that contain older antihistamines
- use of alcohol, nicotine, and caffeine
- pregnancy, especially in the last trimester; in most cases, symptoms usually disappear within 4 weeks after delivery
- neuropathy .
Sleep deprivation and other sleep conditions like sleep apnea also may aggravate or trigger symptoms in some people.; Reducing or completely eliminating these factors may relieve symptoms.
Ulcerative Colitis And Va Disability Benefits
What Is Ulcerative Colitis?
Ulcerative colitis is an inflammatory bowel disease that causes ulcers and inflammation in the innermost lining of the digestive tract. Symptoms of UC usually develop over time rather than suddenly. While this condition can be debilitating and even lead to life-threatening complications in some cases, treatment can greatly reduce the symptoms associated with UC and sometimes lead to remission.
The most common symptoms associated with ulcerative colitis are:
- Abdominal pain
- Inability to defecate despite urgency
- Weight loss;
- Fatigue
- Fever
Most people with ulcerative colitis have mild to moderate symptoms, but cases of severe UC can cause the affected individual to have difficulty with daily functioning and make it difficult for him or her to maintain consistent employment. The impact ulcerative colitis can have on a persons daily life is why the VA developed a schedular disability rating system for this condition. Veterans with UC are eligible for different levels of compensation depending on the severity of their illness, which is important given that ulcerative colitis affects at least 0.2 percent of the veteran population.
Getting Service Connected For Ulcerative Colitis
How The VA Rates Ulcerative Colitis
Under 38 CFR § 4.114, the VA rates ulcerative colitis depending on the severity of the condition.
Diagnostic Code 7323: Colitis, ulcerative
Getting Help With Your VA Claim For Ulcerative Colitis;
Recommended Reading: Does Parkinson’s Cause Memory Loss
