Research Design And Methods
Six independent cross-sectional population surveys were carried out in five geographic areas of Finland in 1972, 1977, 1982, 1987, 1992, and 1997 . In 1972 and 1977, a randomly selected sample making up 6.6% of the population born between 1913 and 1947 was drawn. Since 1982, the sample was stratified by area, sex, and 10-year age-group according to the World Health Organization MONICA protocol . The subjects included in the six surveys were 2564 years of age, and the 1997 survey also included subjects aged 6574 years. Subjects who participated in more than one survey were included only in the first survey cohort. The total sample size of the six surveys was 53,166. The participation rate varied by year from 74 to 88% . After excluding 123 subjects because of prevalent Parkinson’s disease at baseline, 112 subjects because of prevalent type 1 diabetes at baseline or during follow-up, and 1,379 subjects because of incomplete data on any variables required, the present analyses comprise 25,168 men and 26,384 women. The participants gave informed consent . These surveys were conducted according to the ethical rules of the National Public Health Institute, and the investigations were performed in accordance with the Declaration of Helsinki.
Drinking Well Water Is Linked With A Higher Likelihood Of Developing Parkinson’s
A growing body of research suggests that there is a correlation between drinking well water and later in life. One particular study, conducted by a team at UCLA and published in the journal Environmental Health Perspectives, found that those who consume well water are statistically more likely to develop PD. After reviewing the medical records and personal histories of 700 people living in California’s farm belt between 1974 and 1999, they determined that those who ultimately developed PD had consumed private well water on average 4.3 years longer than those who did not.
Diagnosis Of Parkinsons Disease
A number of disorders can cause symptoms similar to those of Parkinson’s disease. People with Parkinson’s-like symptoms that result from other causes are sometimes said to have parkinsonism. While these disorders initially may be misdiagnosed as Parkinson’s, certain medical tests, as well as response to drug treatment, may help to distinguish them from Parkinson’s. Since many other diseases have similar features but require different treatments, it is important to make an exact diagnosis as soon as possible.
There are currently no blood or laboratory tests to diagnose nongenetic cases of Parkinson’s disease. Diagnosis is based on a person’s medical history and a neurological examination. Improvement after initiating medication is another important hallmark of Parkinson’s disease.
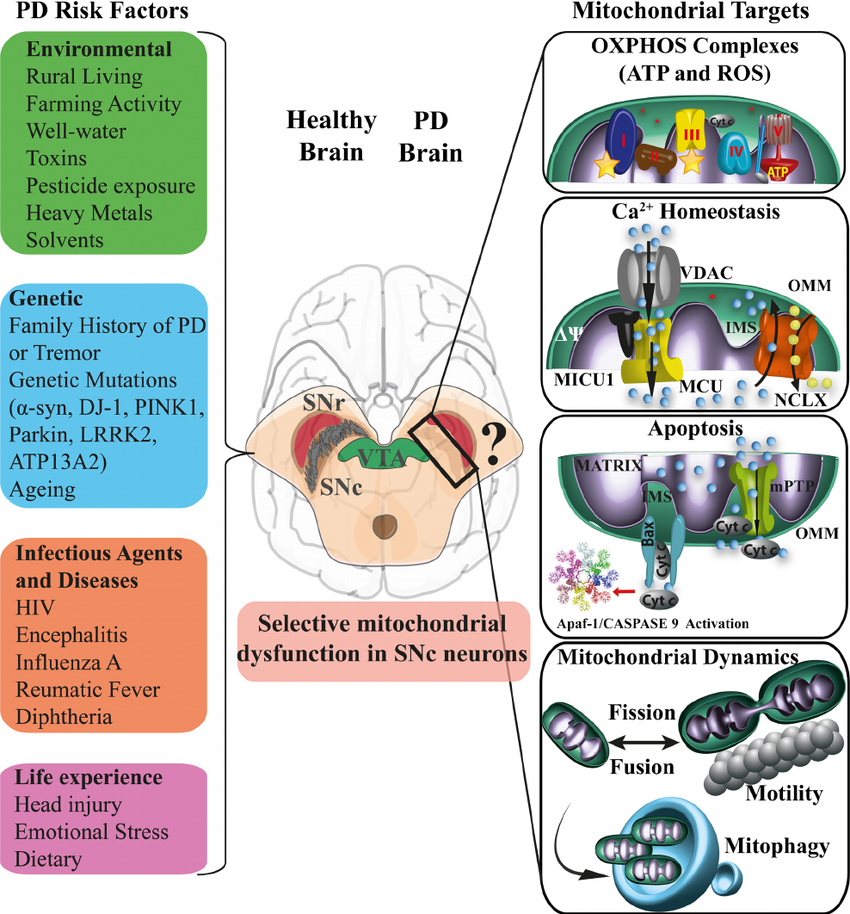
Environmental Factors And Exposures
Exposure to and a history of head injury have each been linked with PD, but the risks are modest. Never having smoked cigarettes, and never drinking caffeinated beverages, are also associated with small increases in risk of developing PD.
Low concentrations of in the blood is associated with an increased risk of PD.
Drug-induced parkinsonism
Different medical drugs have been implicated in cases of parkinsonism. Drug-induced parkinsonism is normally reversible by stopping the offending agent. Drugs include:
The Danger Of Paraquat Today
The United States banned DDT, Agent Orange, and heptachlor in the 1970s and 1980s. However, the United States has not banned all pesticides linked to Parkinsons. The one with perhaps the strongest link to the disease is still in widespread use: paraquat.
The United States has not banned all pesticides linked to Parkinsons. The one with perhaps the strongest link to the disease is still in widespread use: paraquat.
Paraquat has been used as a pesticide since the 1950s and is marketed as an alternative to the worlds most popular weed killer, glyphosate, more commonly known as Roundup. Paraquat takes care of weeds that not even Roundup can kill. Today, it is used on farm fields across the United States, and its use continues to increase. The pesticides primary uses are for corn, soybeans, wheat, cotton, and grapes.
Portraits of several Parkinsons patients show the many faces of people with the diagnosis. It affects people from all walks of life.
Robert Dein
In the laboratory, paraquat reproduces the features of Parkinsons disease. In a 1999 study in Brain Research, A. I. Brooks of the University of Rochester and colleagues gave paraquat to mice, and their activity decreased. Paraquat also killed dopamine-producing nerve cells in the rodents substantia nigras. The greater the amount of paraquat administered, the greater the number of nerve cells lost.
Table adapted from: .
Figure adapted from R. Dorsey et al., 2020.
Lewy Bodies And Alpha
In addition to the dopamine deficiency and neuronal loss, PD is also associated with a buildup of intracellular inclusions inside the neurons, called Lewy bodies. Studies have shown that the Lewy bodies are made mainly of a protein called alpha-synuclein.
They are not seen in brain imaging studies but have been detected in research studies that examine the brains of people who had PD and donated their own brains to science for the purpose of research.?? There is no known treatment or method of removing the Lewy bodies at this time.
In PD,Lewy bodies are found in the substantia nigra as well as other areas, including the amygdala and locus coeruleus , the raphe nucleus , and the olfactory nerve . The functions controlled by these regions can be impaired in PD, although the symptoms arent as noticeable as the tremors and muscle stiffness.
Lewy bodies are also present in the brains of people who have Alzheimers disease and other types of dementia, and they are considered a sign of neurodegeneration.??
Certain Chemicals Lead To More Dangerous Contamination
Those who consumed well water in close proximity to certain pesticides were found to be at a higher risk than others. In particular, the UCLA study found that people drinking well water within 500 meters of fields sprayed with pesticides had a 66 percent increased risk of later developing PD. Those drinking well water near land treated with the insecticides propargite or chlorpyrifos had a 90 percent higher risk. This translates into a nearly doubled risk of someday .
“The chemical with the most data linking it to an increased PD risk is paraquat,” says the APDA, referring to a chemical herbicide used to kill weeds. Exposure to paraquat is “associated with a 2-3 fold increased PD risk over the general population,” the organization warns.
If you regularly consume well water, especially in areas being sprayed with chemical pesticides or herbicides, be sure to have your water filtered and regularly tested.
How Does Environment Come Into It
Your environment is a hard one to pin down. Partly, that’s because it covers a lot of ground. It’s everything that’s not your genes, which could mean where you live, what you eat, chemicals you’ve come into contact with, and more.
Not only that, but it could take years for the effects from something in your environment to show up. So far, doctors have a lot of clues but no smoking gun. So you could have people who live or work in an area around chemicals tied to Parkinson’s, but many of them don’t get it.
Some research shows links between Parkinson’s and:
- Agent Orange, a chemical used to destroy trees and crops in the Vietnam War.
- Certain chemicals used in farming, such as insecticides, herbicides, and fungicides.
- Some metals and chemicals used in factories, such as manganese, lead, and trichlorethylene .
These can come into play based on where you live, what you do for work, or if you served in the military. Sometimes, these chemicals seep into well water, so that’s one more way they can affect you.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
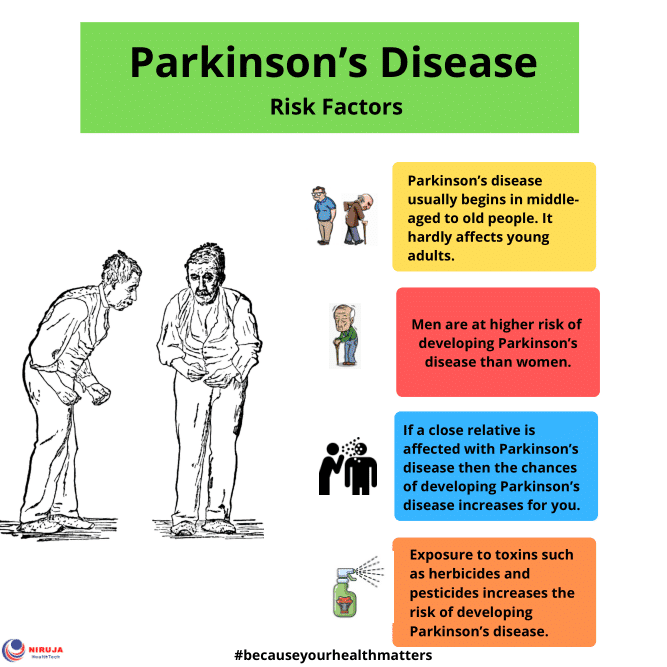
Who Is Most At Risk For Parkinsons Disease
Parkinsons disease is a progressive movement disorder that affects an estimated 1 million people in the U.S. With PD, nerve cells in the brain break down or die. Many of these nerve cells produce , a chemical messenger in the brain. This causes abnormal brain activity and impairs movement along with other PD symptoms. Risk factors include age, heredity, and gender. Some of these are clear; others are not. Lets look at who is at most risk for developing Parkinsons disease.
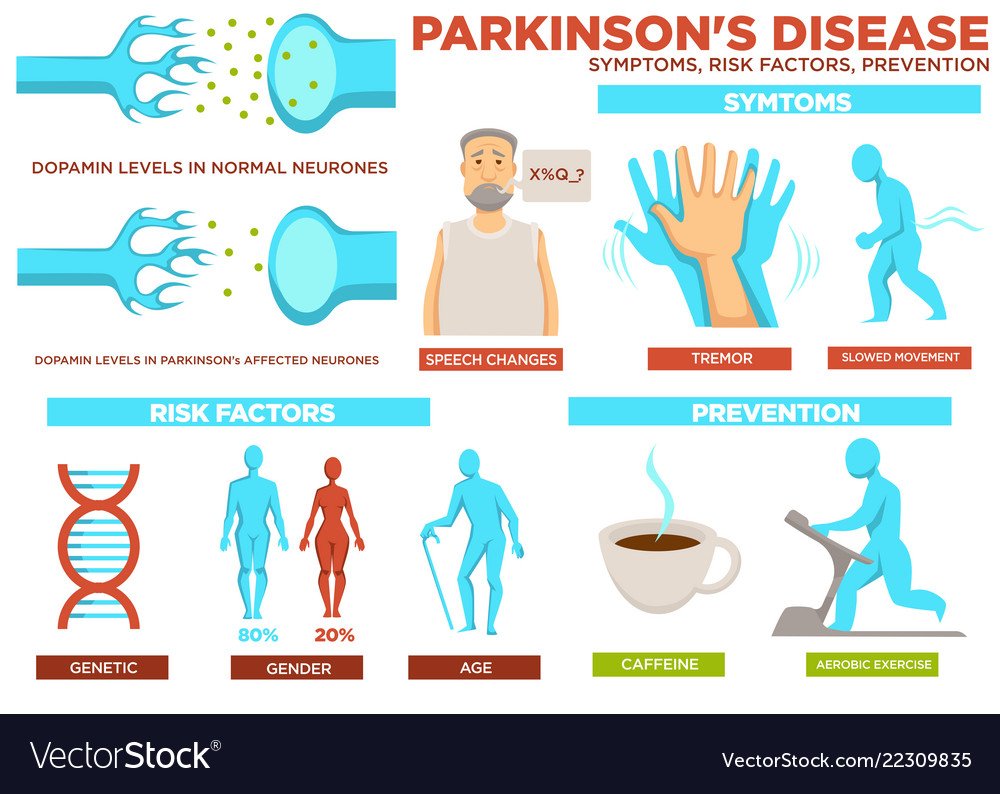
Symptoms Of Parkinsons Disease
Parkinson’s disease has four main symptoms:
- Tremor in hands, arms, legs, jaw, or head
- Stiffness of the limbs and trunk
- Slowness of movement
- Impaired balance and coordination, sometimes leading to falls
Other symptoms may include and other emotional changes; difficulty swallowing, chewing, and speaking; urinary problems or ; skin problems; and sleep disruptions.
Symptoms of Parkinsons and the rate of progression differ among individuals. Sometimes people dismiss early symptoms of Parkinson’s as the effects of normal aging. In most cases, there are no medical tests to definitively detect the disease, so it can be difficult to diagnose accurately.
Early symptoms of Parkinson’s disease are subtle and occur gradually. For example, affected people may feel mild tremors or have difficulty getting out of a chair. They may notice that they speak too softly, or that their handwriting is slow and looks cramped or small. Friends or family members may be the first to notice changes in someone with early Parkinson’s. They may see that the person’s face lacks expression and animation, or that the person does not move an arm or leg normally.
People with Parkinson’s often develop a parkinsonian gait that includes a tendency to lean forward, small quick steps as if hurrying forward, and reduced swinging of the arms. They also may have trouble initiating or continuing movement.
Does Parkinsons Disease Protect From Smoking
What if cigarette smoking does not actually confer a positive biological effect on the brain to protect from PD, but rather some aspect of PD biology leads to less of a tendency to smoke? Dopamine is the main addiction chemical in the brain, so it stands to reason that in a PD brain, with a reduced amount of dopamine, there will be less of a tendency for addiction. Other hypotheses suggest that people with PD may have alterations in how their brains utilize nicotine, or how the nicotine interacts with the dopaminergic neurons, leading to less of a tendency to become addicted to it.
This possibility was explored in a that demonstrated that people with PD who did smoke found it easier to quit smoking as compared to controls, and people with PD utilized reduced amounts of nicotine substitutes in order to quit as compared to controls. This suggested that people with PD have a less intense addiction than controls, leading to the overall decreased smoking rates.
Smoking And Parkinsons Disease
Epidemiologic studies of Parkinsons disease that explore the distribution of the disease in various populations, have consistently found, over a number of decades, that cigarette smokers have lower rates of PD than non-smokers. People are taken aback when they first hear this as it is counter-intuitive. Could it be that a habit so clearly linked to poor health can also provide a health benefit?
There are two potential ways to view this association. The first is that smoking has a biological effect that protects a person from PD. The second is that part of the biology of PD makes it less likely that a person would smoke.
Viral Infections And Pd Risk
The notion of a viral etiology to PD has been mooted for many years. One early example, and poi-gnant today in light of the recent SARS-CoV-2 pandemic, was the emergence of a parkinsonian disorder, encephalitis lethargica , that has been linked to the 1918 influenza pandemic. Viruses, particularly those that are neurotropic, are plausible causal agents of PD but have been relatively understudied compared to genetic risk factors and other environmental risk factors for PD. In this section we will consider the viruses that have been linked to PD in observational studies and evaluate the strength of evidence to support a causal link.
Hepatitis B and C viruses have also been investigated for their associations with PD in recent epidemiological studies. Understanding such associations are important given the prevalence of these infections. Hepatitis C virus is an RNA virus of the Flavivirus family and is estimated to infect 143 million people worldwide. It primarily involves the liver with chronic infection resulting in cirrhosis and hepatocellular carcinoma . Extrahepatic manifestations include a myriad of inflammatory and immune-mediated disorders .
What Else Do We Know
As scientists try to learn what’s at the root of Parkinson’s, they’re looking far and wide to pick up clues where they can.
They’ve found that people with Parkinson’s tend to have something called Lewy bodies in their brain. These are unusual clumps of a protein called alpha-synuclein. The protein itself is normal, but the clumps are not. And they’re found in parts of the brain that affect sleep and sense of smell, which could explain some symptoms of Parkinson’s not related to movement.
Your gut may also have a part in it, as some of its cells make dopamine, too. Some doctors think that this might be where the earliest signs of Parkinson’s show up, but that idea needs more research.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinsons disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinsons disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinsons disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinsons disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinsons disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet is available in an immediate release formula and a long-acting, controlled release formula. Rytary is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Type 2 Diabetes And The Risk Of Parkinson’s Disease
What This Study Adds
-
The disease rate was higher in rural areas compared to urban areas.
-
The odds of developing PD was lower in smokers and people having exposure to tobacco products. In drivers, the disease rate was significantly lower, while in farmers, this rate was significantly higher. Moreover, the disease rate was higher in individuals having exposure to aldrin. Furthermore, this study also revealed the association between PD and exposure duration to risk factors.
-
The disease rate was higher in individuals having depression, hypertension, or a familial history of PD.
-
In Pakistan, levodopa therapy is commonly used to treat PD patients.
Problems With Balance Or Walking
Bradykinesia can also contribute to increasing instability, walking difficulties and changes in gait. An early symptom of this is a decrease in the natural swing of one or both arms when walking. As things progress, the steps you take may become slower and smaller, and you may start shuffling your feet.
Some people with Parkinsons disease may also experience freezing episodes where it can feel like their feet are stuck in place, which can increase the risk of falling.
What Is The Number One Risk Factor For Parkinson’s
Age is the greatest risk factor. About 1% of those over 60 and 5% of those over 85 are diagnosed with it. The increased risk is due to decreasing levels of metabolism and other changes that make the neurons vulnerable.
Reeve A, Simcox E, Turnbull D. Ageing and Parkinsons disease: Why is advancing age the biggest risk factor?Ageing Research Reviews. 2014;14:19-30. doi:10.1016%2Fj.arr.2014.01.004
What About Cigarettes Parkinsons Smoking And Risk Of Cancer
As I mentioned in a previous blog, there is also an inverse relationship between cigarette smoking and PD. It is unclear whether that is because an ingredient of cigarette smoke protects smokers from PD, or because the lack of dopamine in people with PD make them more risk-averse as a group, and therefore less likely to smoke.
Regardless, because it is clear that smoking increases the risk of multiple types of cancer, any study that investigates the cancer rates of people with PD must always account for the fact that people with PD tend to smoke less than people without PD. The most recent study which analyzes the relationship between cancer risk and PD, as referenced above, takes great pains to remove this confounding factor in its statistical analysis. Even with taking differences in smoking rates into account, the conclusion of the study is that people who have had cancer are less likely to develop PD. It is also the case that rates of certain types of cancers that have not been linked to smoking are lower in people with PD. This fact supports the conclusion that the lower rates of smoking among PD patients is not the cause of the lower rates of cancer. Regardless of any study results, cigarette smoking is linked to numerous deadly diseases and must be avoided.
Family History & Genetics
Researchers have been able to identify certain genetic mutations that can increase the risk of developing Parkinsons disease.
These are the two types of Parkinsons disease, from a genetic standpoint:
- Hereditary Parkinsons disease: Roughly 15% of all cases of Parkinsons disease are inherited. In these cases, mutations in certain genes are passed down through families and increase the individuals risk of developing this condition.
- Sporadic Parkinsons disease: On the other hand, cases in which people dont have a family history of Parkinsons disease are referred to as sporadic cases. These cases are in fact the majority. Scientists have found that alterations in certain genes may also play a role in sporadic cases, in addition to other environmental and lifestyle-related factors.
However, the role that these genetic mutations play in the development of the condition hasnt been fully understood yet.
Clinical History And Testing
Diagnostic tests can be used to establish some features of the condition and distinguish them from symptoms of other conditions. Diagnosis may include taking the person’s , a physical exam, assessment of neurological function, testing to rule out conditions that may cause similar symptoms, brain imaging, to assess cognitive function,, or myocardial scintigraphy. Laboratory testing can rule out other conditions that can cause similar symptoms, such as abnormal , , , or vitamin deficiencies that may cause symptoms similar to dementia.
Dementia screening tests are the and the . For tests of attention, , , and can be used for simple screening, and the Revised Digit Symbol Subtest of the may show defects in attention that are characteristic of DLB. The , and are used for evaluation of executive function, and there are many other screening instruments available.
If DLB is suspected when parkinsonism and dementia are the only presenting features, PET or SPECT imaging may show reduced dopamine transporter activity. A DLB diagnosis may be warranted if other conditions with reduced dopamine transporter uptake can be ruled out.
Since 2001, – has been used diagnostically in East Asia , but not in the United States. MIBG is taken up by nerve endings, such as those that innervate the heart, and is for scintigraphy with radioactive 123iodine. Autonomic dysfunction resulting from damage to nerves in the heart in patients with DLB is associated with lower cardiac uptake of 123I-MIBG.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Medicines For Parkinson’s Disease
Medicines prescribed for Parkinson’s include:
- Drugs that increase the level of dopamine in the brain
- Drugs that affect other brain chemicals in the body
- Drugs that help control nonmotor symptoms
The main therapy for Parkinson’s is levodopa, also called L-dopa. Nerve cells use levodopa to make dopamine to replenish the brain’s dwindling supply. Usually, people take levodopa along with another medication called carbidopa. Carbidopa prevents or reduces some of the side effects of levodopa therapysuch as nausea, vomiting, low blood pressure, and restlessnessand reduces the amount of levodopa needed to improve symptoms.
People with Parkinson’s should never stop taking levodopa without telling their doctor. Suddenly stopping the drug may have serious side effects, such as being unable to move or having difficulty breathing.
Other medicines used to treat Parkinsons symptoms include:
- Dopamine agonists to mimic the role of dopamine in the brain
- MAO-B inhibitors to slow down an enzyme that breaks down dopamine in the brain
- COMT inhibitors to help break down dopamine
- Amantadine, an old antiviral drug, to reduce involuntary movements
- Anticholinergic drugs to reduce tremors and muscle rigidity
What Raises Someone’s Risk For Parkinson’s
It’s a complex picture, but you may be more likely to get Parkinson’s based on:
Age. Since it mostly affects people 60 and older, your risk goes up as the years go by.
Family history. If your parent, brother, or sister has it, you’re a little more likely to get it.
Job. Some types of work, like farming or factory jobs, can cause you to have contact with chemicals linked to Parkinson’s.
Race. It shows up more often in white people than other groups.
Serious head injury. If you hit your head hard enough to lose consciousness or forget things as a result of it, you may be more likely to get Parkinson’s later in life.
Gender. Men get it more than women. Doctors aren’t sure why.
Where you live. People in rural areas seem to get it more often, which may be tied to chemicals used in farming.
Risk Factors For Parkinson’s Disease
While the exact causes arent fully understood, researchers have identified characteristics that increase a persons risk of developing Parkinsons, including gender, age, race, and genetic factors. However, it is worth noting that the vast majority of cases of PD are considered idiopathic Parkinsons disease. Idiopathic means a condition that arises spontaneously or for which the cause is currently unknown. Major advances in and science are continuing to reveal more underlying causes for PD.1,2
