All Up A Multidisciplinary Team Approach For Pain Management May Be Necessary In Addition To Your Movement Disorder Specialist Providers May Include Physical Or Occupational Therapists Psychiatrists And Even Pain Management Experts Each Of These Practitioners Targets A Different Aspect Of The Pain
Exercise to Relieve your Pain
Many different types of exercise can be beneficial for people with Parkinson’s disease , including non-contact boxing, tai chi, dancing and cycling, as some examples. If you have limited mobility, you can try chair yoga or other seated exercises. Whichever exercise you choose, make sure it is something safe and enjoyable so that you can stick with it.
It’s important to pace yourself and know your personal limitations. If during or after exercise you experience extreme pain you should look at modifying your routine and choose a less intensive exercise. Even the simplest exercise, including walking your dog or just puttering around the house or garden, can help alleviate symptoms of pain.
- Cycling
If you need help or advise consult with a physical or occupational therapist to help design a personalised program for you. Learn more about exercise and Parkinson’s.
Non-pharmacological pain treatments
Complementary therapies are treatments used alongside conventional medicine. They take a more holistic approach than conventional medicine, aiming to treat the whole person including mind, body and spirit, rather than just the symptoms. These include massage therapy, mindfulness and meditation techniques, acupuncture, and heat or cold application. These may be used on their own or in combination with medication.
Anti Inflammatories
Since A Back Injury In 1985 John Has Experienced Multiple Types Of Pain Some Of Which Have Been Triggered By His Parkinson’s He Was Diagnosed With The Condition In 2016
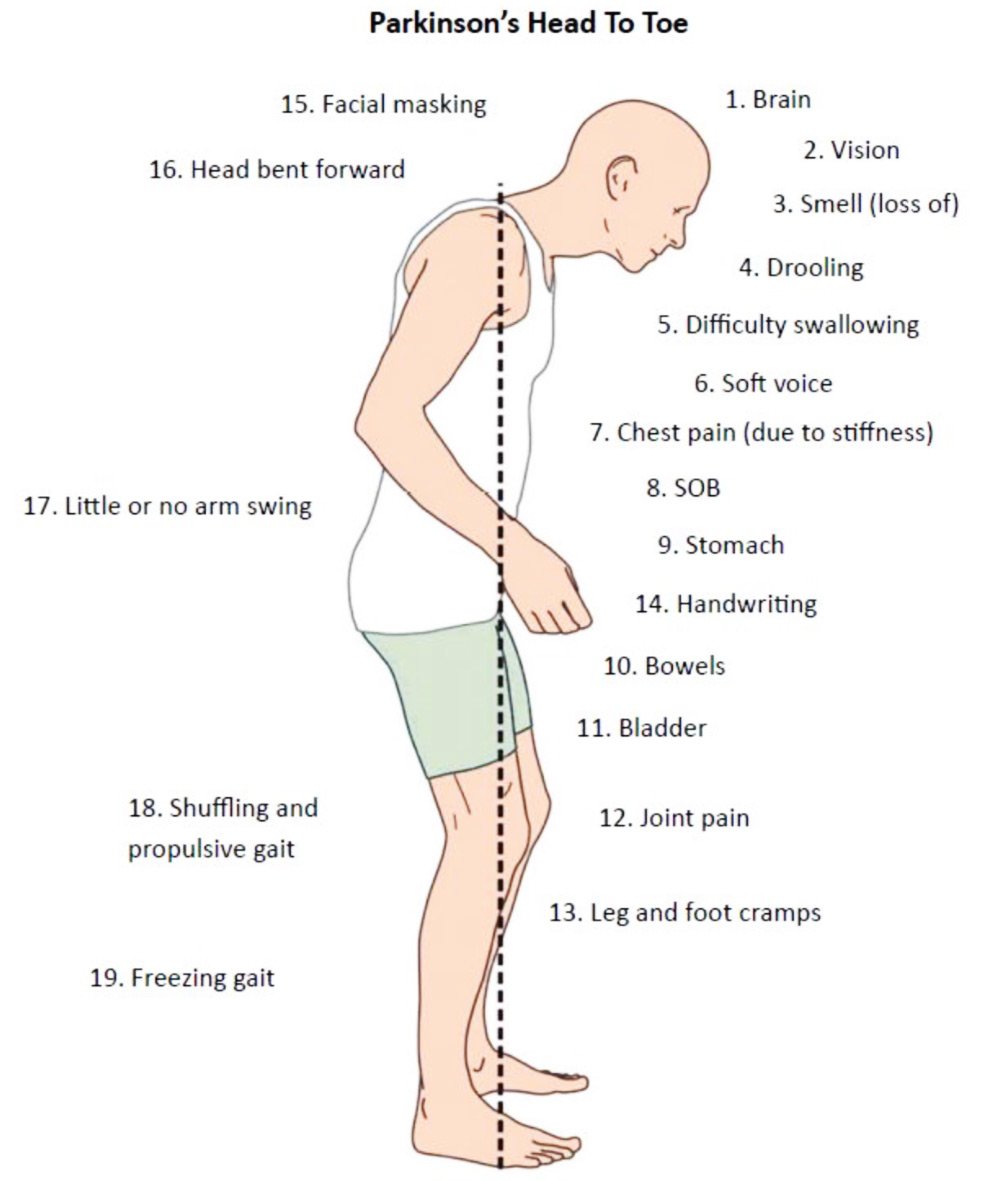
I’ve been experiencing varying degrees of pain since injuring my back, which caused me to have lower-back pain, which continues to this day. Since then, I have also developed pain in other parts of my body due to Parkinson’s, including my hands, ribs, upper back and shoulder.
The pain in my ribs is deep, aching and constant, and I get internal tremors in this area. However, the pains in my legs are sharp, intermittent and become very rigid, especially in my calves.
When I walk, the pain can get so bad that I end up having to stop and rest. On really bad days, I use a wheelchair. When I’m in a lot of pain, it affects my Parkinson’s symptoms even more, and also my spatial awareness, that I tend to lose my balance and fall or freeze.
I was referred to a pain specialist…who enrolled me on an 8-week pain management course led by a Parkinson’s-trained physiotherapist. Now I do an hour of gentle movements and stretching every morning.
I can’t stand for long enough to wash and have a shave, or to wash the dishes, so I use a perching stool. I can no longer carry out my hobby of canoeing to the same degree. While I use to be able to do it all day, I’m now lucky if I can do it for an hour.
I was referred to a pain specialist, who prescribed me medication, and advised on workable changes to my lifestyle and diet. They also enrolled me on an 8-week pain management course led by a Parkinson’s-trained physiotherapist. Now I do an hour of gentle movements and stretching every morning.
The Parkinsons Disease News Today Forums Are A Place To Connect With Other Patients Share Tips And Talk About The Latest Research Check Them Out Today
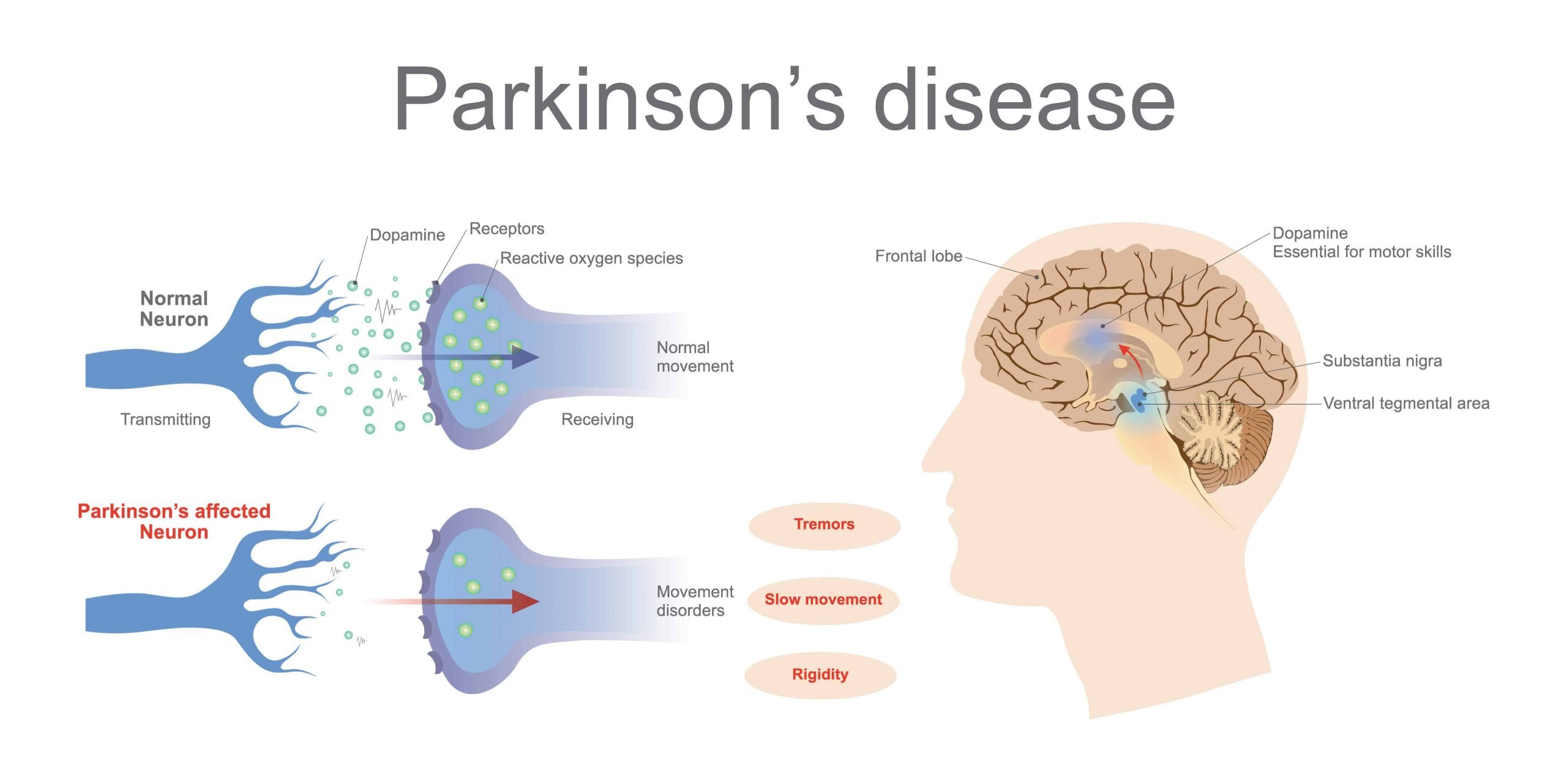
PD pain can resemble pain from other disease processes, especially as the patient ages and faces a multitude of other pain-causing conditions such as arthritis, spine degeneration, poor muscular conditioning, and such. In my case, PD pain is distinguished by the following:
- The progression of body pain correlated with the progression of the disease over time.
- Levodopa, a dopaminergic therapy, successfully reduces the pain.
- The pain is worse during “off” periods.
My PD pain also has a particular characteristic: stinging , irritating tingling, burning, and muscle heaviness with increased pain on movement. This pain happens over large regions of the body and varies in severity. At its worst, it can last several days and reach level 7, inducing spontaneous tears.
PD with episodic chronic pain is disabling in several ways. First, high levels of pain obstruct clear thinking. Second, high levels of pain induce the fight-or-flight response, which interferes with emotion management. Third, the amount of energy necessary to manage it is very tiring . Chronic PD pain entails much more than body symptoms.
I have been a “communicator” most of my life, but it remains a struggle to find words that describe the unique character of PD pain. If you experience PD pain, please share your descriptors in the comments. Together we may find a common dialogue that will help others.
***
Im In Pain But I Dont Want To Take Carbidopa/levodopa Yet Because My Doctor Says It Will Only Work For Five Years Any Advice
It is true that as time passes and your disease progresses, you will have to take higher doses to replace the dopamine your body can no longer produce. However, the rate of dopamine loss is different for everyone. What your doctor may be telling you is that after taking carbidopa/levodopa for some time, you may begin to experience side effects like dyskinesia. It is important to understand that while you may experience this unwanted side effect, for example, you still benefit from the carbidopa/levodopa. If you believe your pain is Parkinson’s-related, and you have already tried other medications and complementary therapies without relief, it is probably time to try carbidopa/levodopa.
Colm Was Diagnosed With Parkinson’s Around 3 Years Ago And Experiences 4 Different Types Of Pain Related To The Condition

The 4 different types of pain I experience all affect my muscles and joints. This includes sudden-onset joint pain – typically a frozen shoulder, or pain when I bend an elbow or knee. It usually lasts between 6-8 weeks and will usually go away for a week or 2, only to reappear in another joint. It greatly restricts my movement and its constant nature can be frustrating.
I also have issues with leg cramps and dystonia, which I frequently experience when waking in the morning, or when moving between different ground surfaces. The cramps are very severe with sudden onset, but slowly wear off after some minutes.
My Parkinson’s has worsened certain pre-existing conditions, including back problems, which were caused by a childhood injury. This has caused me painful episodes throughout my life, but my Parkinson’s seems to have exacerbated this to the point where I’m totally incapacitated with pain and stiffness.
As a carer, I have no option but to try and carry on with my normal duties…I find it helps to wake about 2 hours earlier than normal to take my medication.
I keep an armchair and some dressing aids in my bedroom, as a bout of very severe back pain makes getting in and out of bed or dressing myself difficult.
I also experience muscle stiffness and inflexibility, which cause me pain due to over-exertion. This happens if I don’t take regular breaks throughout the day. As a carer myself for 3 disabled family members, this can prove very difficult.
Join The Parkinsons Forums: An Online Community For People With Parkinsons Disease And Their Caregivers
Chronic pain between the two groups was assessed using the Brief Pain Inventory , which measures pain severity , pain interference and pain frequency. A qualitative description of pain was also conducted.
Patients described pain as “exhausting,”“tiring,”“penetrating,”“miserable” and “unbearable” significantly more often than controls.
Among patients, those with depressive symptoms — as evidenced by a score of eight or higher in the Hospital Anxiety and Depression Scale — reported pain as tender more frequently than those without depression. Controls with depressive symptoms were more likely to report pain as stabbing, tender and tiring compared to those without evidence of depression.
“These descriptions indicate a significant impact of pain on the psychological well-being of the patient,” the researchers wrote.
Subsequent analysis showed that patients overall scored higher than controls in “worst pain felt since last week” and in global pain severity. Among all participants with depressive symptoms, those with Parkinson’s had higher scores of worst pain felt and average pain felt since last week, as well as higher reported pain levels at the time of assessment and global pain severity than those in the control group.
Symptoms of depression led to similar differences – plus an additional higher impact on social relations – between patients and controls. Of note, depression was associated with greater difficulties in walking in the group without Parkinson’s.
Negative Impact Of Severity Of Pain On Mood Social Life And General Activity In Parkinson’s Disease
This case control study designed for clinicians and rehabilitation specialists to effectively identify pain from the patient’s point of view determined that PD patients had significantly higher pain severity scores compared to controls. PD patients with depressive symptoms had significantly higher pain severity and pain interference scores than controls without depressive symptoms. PD patients reported greater scores on Global BPI pain interference and all components of the pain interference subscale. Therefore, PD and depression seem to be correlated with higher perceived pain, severity and interference. A report on this study, by Jose Marques Lopes, PhD., was published in Parkinson’s News Today, September 21, 2018.
James* Was Diagnosed With Parkinson’s In 2011 His Pain Has Worsened As His Condition Has Progressed
When I was diagnosed with Parkinson’s, I initially felt little to no pain. It’s only now, in the advanced stages of the condition, that I’ve started feeling pain, coupled with the normal ageing process.
One of the worst pains I experience is dystonia and dyskinesia of the upper body, especially in my neck and head. It usually starts with a pulsing headache, followed by jerking of the muscles in my face, neck, upper torso and hands. It’s particularly severe in my arthritic finger and my neck. It can be severe to mild, often very distressing, and can last up to 2 hours.
I also have mild to moderate, uncontrollable movements – or swaying – associated with dyskinesia. It’s more prominent when I’m sitting down at a table or working on my laptop. Strangely, I feel this pain at its worst when I’m on the phone, or trying to explain something, or if I’m feeling over-excited or anxious – which is when I become severely dyskinetic. There’s now a dull, continuous pain in my neck, caused through the movement, which gets sharper during bouts of the symptom.
I also experience pain when standing, mostly during a ‘wearing off’ period. My knees pull towards each other and the pain is so severe that I can’t walk. Luckily it only lasts a minute or 2, but the pain can be distressing.
To ease the pain, I take paracetamol as and when, occasionally co-codamol, and very occasionally an anti-inflammatory, for the arthritis. I previously tried cannabis oil but it was of no benefit to me.
Interested In Parkinsons Disease Research Sign Up For Our Forums And Join The Conversation
A total of 97 Parkinson’s patients at a mean age of 67.7 years, including 60 men, and 97 individuals used as controls at a mean age of 67.5 years, including six men, without the disorder or other neuromuscular diseases, filled out a questionnaire on the intensity of local lumbar back pain. The intensity of leg radicular pain — caused by inflammation and/or injury to a spinal nerve root – was quantified by the visual analogue scale — a continuous scale used to measure pain intensity.
In addition, the participants’ permanent functional disability was assessed via the Oswestry Low Back Pain Disability Questionnaire — a self-completed questionnaire that includes 10 different topics: intensity of pain, lifting, ability to care for oneself, ability to walk, ability to sit, sexual function, ability to stand, social life, sleep quality, and ability to travel.
Patients were further asked to describe the painful sensation they experience as pricking, tingling, burning, paresthesia — often described as feelings of pins and needles, or numbness — or other.
The team also assessed Parkinson’s duration, medications being used, severity of motor symptoms — as assessed by the Unified Parkinson’s disease rating scale part III — and the Hoehn and Yahr stage, which is a system used to assess symptom progression.
According to the ODI results, minimal disability was reported by 43.8% of Parkinson’s patients, moderate disability by 27.5%, severe disability by 22.5%, and “crippled” by 6.3%.
Revisiting Pain In Pdthe 50 Shades Of Pain Experienced By Parkinsons Patients
Pain is a quality of life issue for people with Parkinson’s disease and can be under treated by doctors who may assume that is worsens as the disease progresses, although for some pain is an initial symptom of PD. This article helps focus your physician’s attention in the right direction to accurately diagnose your pain.
Pain Management In Patients With Parkinsons Disease: Challenges And Solutions
This review focuses on the diagnosis and management of Parkinson-related pain. It reviews the incidence and prevalence of PD, general pain and PD-related pain, the pathophysiological pathways of pain in PD, physiological pathways of pain relief, measurements of pain, clinical diagnosis of PD-related pain, and treatment strategies.
Pain: Does Parkinsons Cause Pain Or Does Pain Make Other Pd Symptoms Worse
Is pain a symptom of Parkinson’s?
Or do the motor symptoms of PD directly or indirectly cause pain?
Or is pain a symptom of something else? Arthritis? Aging?
Or is pain a result of lack of exercise? Over exercise? Improper exercise form? Improper exercise instruction? Some combination of factors?
Those are interesting questions, but more importantly does pain contribute to the severity of other Parkinson’s symptoms?
Is pain a symptom of Parkinson’s? If it is, is it a motor symptom or a non-motor symptom?
Do the motor symptoms of PD directly or indirectly cause pain?
Or is pain a symptom of something else? Arthritis? Aging?
Or is it a result of lack of exercise? Over exercise? Improper exercise form? Improper exercise instruction? Some combination of factors?
Does pain contribute to the severity of other Parkinson’s symptoms?
If you’re looking for a conclusive answer, I’ll save you some time…there is no single answer, because pain, like Parkinson’s, is as unique to an individual as a fingerprint.
Doctors know that people with Parkinson’s experience pain. Estimates of people with PD who experience pain range from between 40% and 85% in various studies of the topic. This significant disparity is most likely due to variances of what qualifies as pain, and how questions about pain experience are worded, as pain can only be reported and measured by the individual experiencing it.
Ranking of the ten most bothersome PD-related symptoms :
| Rank | |
|---|---|
| 3 | 8 |
Additional recommended reading:
What Are The Different Types Of Pain Experienced By People With Parkinsons
Five main types of pain are common for people with Parkinson’s. Multiple types may be present simultaneously or occur at different points throughout a person’s path with Parkinson’s. Recognizing which kind of pain is present can help you optimize treatment, as can paying attention to what activities or times of day make your pain better or worse.
Musculoskeletal pain
Musculoskeletal pain that affects muscles, bones, tendons, ligaments, and/or nerves. The pain can be localized or generalized and can fade or intensify at different times. Existing musculoskeletal pain can be exacerbated by Parkinson’s.
Neuropathic pain
Rather than being caused by a physical injury, this type of pain is caused by damage to the somatosensory nervous system or a disease affecting the somatosensory nervous system, which responds to external stimuli like touch, temperature, and vibration. It tends to be fairly consistent throughout the day and is present no matter what activity you’re doing. Unlike the aching you may feel when you’re doing a strenuous physical activity, neuropathic pain feels more like a tingly, crawly, uncomfortable sensation.
Dystonic pain
Dystonia, the movement disorder in which involuntary muscle contractions cause repetitive or twisting motions, is often very painful. Many people with Parkinson’s experience dystonia as a motor symptom, whether it’s localized , in multiple nearby body parts , or all over .
Akathisia
Central pain
Fibromyalgia Vs Lupus: Complications Mortality Hospitalization And Costs
Over the period between 1979 and 1998, the Centers for Disease Control and Prevention reported approximately 23 annual deaths from fibromyalgia. Mortality among fibromyalgia patients is usually on par with the general population, but suicide rates and injuries are higher among fibromyalgia patients.
In 1997, fibromyalgia hospitalizations accounted for 7,440 patients and annually fibromyalgia costs each person $3,400 to $3,600.
During the same time period, lupus mortality accounted for 879 to 1,406 deaths annually, with rates rising. Estimations of lupus-related hospitalizations were 39,400 in 2010, and an average cost to the U.S. healthcare system was estimated to be $13.3 billion.
Fibromyalgia complications result from lack of sleep, which can interfere with daily function as being tired can impair memory, focus, and increase the risk of injury. Other complications may include depression and anxiety, and the disease is still very much misunderstood.
Complications of lupus include severe kidney damage, damage to the brain and central nervous system, problems with the blood and blood vessels, inflammation of the lungs and chest cavity, inflammation of the heart, increased risk of infection, cancer, bone tissue death, and pregnancy complications.
Q Are There Any Alternative Therapies That Are Effective For Pain In Pd
Dr. Fleisher: Although alternative therapies may be helpful, there is little evidence-based research to support their use. Certainly massage therapy, anecdotally, seems to be helpful for managing pain. Small studies suggest that acupuncture might improve sleep in patients with PD, but data on the effects on pain in PD is lacking. Larger, more well-controlled and reproducible studies of these therapies are needed.
Patients frequently ask about the effects of medical marijuana in managing PD, including pain symptoms. Several studies have looked at efficacy of marijuana in PD and have found that it probably is ineffective for most PD symptoms.11 However, we just don’t have enough evidence to know for sure. The most rigorous study of medical marijuana in PD showed a trend toward worsening tremor.11,12
For most people, stress and anxiety worsen tremor, and anything that relieves anxiety will improve tremor. Thus, modalities such as yoga, meditation, and mindfulness training will improve tremor. Similarly, medical marijuana may improve tremor in certain people by temporarily reducing anxiety and stress, but the evidence has not borne this out yet.
Fibromyalgia Vs Lupus Differences In Symptoms Pain Causes And Treatment
Fibromyalgia and lupus are two conditions that can cause pain, but it’s important to recognize the many significant differences between the two. Systemic lupus erythematosus , or lupus, is an autoimmune systemic disorder, which affects the joints, skin, and practically any organ in the body. Fibromyalgia affects the muscles causing pain, tender points, and extreme fatigue, and can contribute to anxiety or depression.
Both lupus and fibromyalgia are difficult to diagnose, and many patients with fibromyalgia are often wrongly diagnosed with lupus and vice versa. Furthermore, the two diseases can actually overlap one another, and there is a higher risk of rheumatic disease in fibromyalgia patients.
Fibromyalgia affects roughly two percent of the population and women are more likely to develop fibromyalgia than men. Estimates of lupus cases in the U.S. are 161,000 with definite lupus and 322,000 with definite or probable lupus. Like fibromyalgia, lupus often affects women more than men, too.
Fact: Fibromyalgia Does Not Damage Muscles Joints And Connective Tissue
Rheumatologists consider fibromyalgia to be a musculoskeletal disease because of the discomfort in the muscles and joints, says Don Goldenberg, M.D., director of the Arthritis-Fibromyalgia Center, Newton Wellesley Hospital, Newton, Mass., and a medical adviser to the Arthritis Foundation. “But there is no specific disease in those areas. Evidence suggests that most of the pain has to do with changes in pain processing.”
Q What Is The Pain Experience In Pd And Does It Differ Between Genders
Dr. Fleisher: As with almost everything else in PD, the pain experience is highly individualized, and no 2 people, regardless of gender, will have the same symptoms. Female gender appears to be an independent risk factor for chronic pain in PD, even though PD is more common in men than in women.2 Pain intensity also is higher in women than in men with PD.1
There is a lot of interesting research examining the contributions of hormones to the greater prevalence of PD in men or, conversely, the lower prevalence in women.3 Once we better understand the roles of sex hormones in the pathophysiology of PD, we may better understand whether hormones also play a role in the higher incidence of chronic pain in women with PD.
Q Are There Any Gender Disparities In The Treatment Of Pain In Pd
Dr. Fleisher: I don’t think there is any literature demonstrating gender disparities in pain treatment among patients with PD, but we do know that there are certainly gender disparities overall in the treatment of women with PD, so it would not be surprising to learn that women with PD-related pain are at a disadvantage and not getting the appropriate care that they need.
Towards An Understanding Of The Concept Of Comorbid Fibromyalgia
There are three scenarios that should be taken into consideration when FM associates with some other medical condition. Firstly, FM may have predated the disease, but it is unknown whether pre-existing FM specifically affects disease expression. However, to borrow from the legal tradition, a ‘thin-skull’ diathesis does suggest a particular fragility that may influence the impact of a new disease. The effect may simply be additive of the individual components of each disease, or may even be an exaggerated effect that compounds the overall burden of suffering.
Secondly, the individual may possess a pain prone phenotype with any pain able to initiate sensitization resulting in amplification of pain intensity and location. For example, persons with OA localized pain exhibit hyperalgesia even at sites distant from the OA site, indicating widespread multimodality changes in the nociceptive system . ‘Remaining pain’ in RA, reported to occur for about 60% of patients with well-controlled inflammatory disease, may also reflect this pain prone phenotype . Although reports of remaining pain have not specifically invoked FM, the hypothesized mechanism of peripheral nerve sensitization represents a pathogenesis similar to FM.
Innovative Treatment Modalities For Managing Pain In Parkinsons
Botulinum toxin
Non-dopaminergic pharmacotherapy may benefit patients with PD-related pain. Botulinum toxin , both A and B derivatives, should be considered in patients who do not respond to dopaminergic treatment optimization.1,8 Botulinum toxin injection provides localized treatment by blocking the release of acetylcholine at the neuromuscular junction.4 Local injections of BTX type A or B can be effective for persistent dystonia-related pain and central pain, based on its neuromuscular action in movement disorders plus analgesic mechanism.
A randomized, double-blind, crossover, placebo-controlled trial concluded that BTX-A in patients with PD is safe and potentially useful in treating limb pain.29 The study was conducted in patients with PD over the age of 30 years with painful limbs not responding to the optimization of anti-Parkinsonian medications. Patients were randomized to receive BTX-A injection or placebo, followed by the other treatment per the crossover design. Depending on the location of pain, patients received up to 200 units in upper limbs or up to 300 units in lower limbs. Patients experienced a significant reduction in their self-reported numerical pain score 4 weeks after the BTX-A injection , but not with placebo . There was no difference between the change with BTX-A compared to placebo . This study demonstrated that targeted BTX-A injections are safe in patients with PD.
Cannabinoids
Can Emotional Stress Cause Symptoms That Resemble Transient Pd
Sayings such as ‘shaking in fear’, ‘staring in disbelief’ or ‘frozen with fear’ exist in many languages and suggest that acute emotional stress can mimic some features of PD.
Dramatic examples of reversible parkinsonism were frequently reported among the casualties of ‘shell shock’ and ‘war neurosis’ that in Germany were referred to as ‘Kriegszitterer’ . In the surviving cine films, most of these handicaps resembled a psychogenic movement disorder and suggestion therapy led to an improvement in most cases.27
A few cases, however, closely resembled PD and neurologists described some World War I soldiers as follows: “The eyes were wide open and had a pained vacant stare. He cannot move his legs, which are rigid. As in many of these patients the sole of the foot is shuffled along the ground. Another form of tremor which is coarser and less rapid than the preceding, viz. 5–6 per sec, is that which resembles paralysis agitans.”28 Others observed similar findings reporting “balance is maintained with difficulty since the trunk is flexed anteriorly and the legs are partially bent at the knees. The arms hang low and stiffly at the sides, giving a simian appearance to the whole posture. Coarse tremors develop in the hands and legs , the facies are mask-like without expression.”29
Same patient without any dopaminergic therapy showed significant improvement in handwriting after chronic stress has been resolved.
Fact: Treatment Involves Antidepressants And Antiseizure Drugs
The notion that people with fibromyalgia have a predisposition to both pain and depression led to the idea that antidepressants might help. Antiseizure drugs are thought to improve brain neurotransmitter issues in fibromyalgia, Goldenberg says.
But opioids don’t work, says Clauw: “The body’s opioid system may be driving part of the underlying of the disease, so giving patients opioids may make their fibromyalgia worse.” In a 2013 Stanford study, when 31 women with fibromyalgia took low doses of naltrexone, a drug which blocks the body’s opioids, they saw a 29 percent reduction in pain compared with an 18 percent reduction in those that took a placebo.
Pain Is A Common But Overlooked Problem In Parkinsons Disease
Pain is an often overlooked non-motor symptom of Parkinson’s disease . Studies show that between 40-80% of people with PD report pain, which is likely why it is often suggested as a topic for this blog.
One of the reasons why the topic of pain and PD is difficult to address is that it is sometimes tough to discern whether a particular pain is due to PD or not. Chronic pain is such a common symptom among the general population, and people with PD are not immune to common problems as well. However, there are aspects of PD that may exacerbate the pain experienced from a common problem. In addition, there are particular types of pain that may be unique to people with PD.
Q What Is The Role Of Depression In The Pain Experience In Pd
Dr. Fleisher: Depression is one of the most overlooked symptoms of PD, and it can affect over 30% of people with the disease at some point in their illness.5 I think there is a misconception that depression results from an adjustment disorder following diagnosis. While that may be partially true, patients with PD have alterations in various neurotransmitters—including serotonin and norepinephrine in addition to dopamine—that predispose them to depression.6,7
Depression is the primary factor related to quality of life in PD and is an independent risk factor for medication nonadherence. A physician could prescribe the most comprehensive regimen to control Parkinson’s symptoms, including pain, but if depression symptoms are not being addressed simultaneously, the likelihood that that person is going to take that regimen is pretty minimal.
Given the link between depression and chronic pain, patients who are depressed should be screened for chronic pain and vice versa. In my practice, we screen every patient with the Unified Parkinson’s Disease rating scale , which has both a patient-reported subjective component that includes questions about depression, pain, and altered sensation, as well as an objective component that includes a physical examination and questions about potential medication adverse effects . The patient fills out the subjective component every single time they come to the office.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Fact: People With Fibromyalgia Need Exercise But Not Too Much
“Exercise is the most effective ‘drug’ for fibromyalgia,” Clauw says. “It works like the drugs for fibromyalgia, raising chemicals in the body that are connected to feeling good. But as with drugs, if you ‘take’ too much exercise, your fibromyalgia symptoms may become worse. Start at a low level of exercise and increase slowly.”
Clauw’s not suggesting that you sign up for sweating sessions in the gym. “Just get up and move, walk, take the stairs instead of the elevator. It will improve all your symptoms — pain, fatigue, sleeplessness — in part because it alters the levels of neurotransmitters that affect pain and mood.”
Dorothy Foltz-Gray is a freelance writer.
Does Taking Certain Medications Risk Lowering Dopamine Levels
Neuroleptic medications typically lower dopamine levels. If you’re taking any of them, check with your doctor about any symptoms you may have that could be due to low dopamine levels. You’ll want to work with your doctor to balance benefits and side effects of these medications. Common medications in this class include:??
- Clozaril
Supplements believed to help raise dopamine levels include:??
- Rhodiola rosea, an herb sometimes called golden root or Arctic root
- L-theanine, also known as suntheanine, an amino acid derived from tea leaves
