Tom Thought That Because Some Pink Tablets Relieved His Symptoms This Meant He Was Ok He Didn’t
I first suspected there was something wrong when I was travelling and I was writing a postcard to a friend of mine in, in Australia whose name is Anthony Diecopolis. And, and I got to the Anthony Diec and I couldn’t finish the opolis. And it’s very strange my hand had sort of gone into a sort of spasm and it just wouldn’t, wouldn’t finish writing the, the, the word. And so that’s a bit strange.
And so I went when, when I got I, I went to the doctor and said, “What on earth’s going on?” And I had since then I’d also developed this slight tremor in my right hand. He said, “Well it’s probably, Essential Tremor or trapped nerve or something like that”. And anyway, then it got a bit worse and then I was, I was recommended to go to a neurologist. And the neurologist had a look at me and gave me some pills. And he said, “Come back and tell me if these work”.
This is about, about sort of, nine months after my, my not being able to finish the, the postcard. And, and he said, “Take these pills”. And the pills worked. Magically the tremors stopped and I thought this is wonderful. And so I went back to the neurologist and I said, “Yes everything’s fine now. The pills have, the pills have worked.” And far from looking happy about this he looked rather, rather grave and he said, “I think you’d better go to another neurologist.”
Comparison Of Patients In Whom A Diagnosis Of Parkinson’s Disease Was Maintained Or Rejected
Patients in whom a diagnosis of Parkinson’s disease was confirmed had more severe disease as measured by the Hoehn and Yahr stage , more often had a tremor at rest or a classical pill rolling tremor , and more often reported a good initial and sustained response to levodopa than those in whom it was rejected.
Patients in whom the diagnosis was changed to non-parkinsonian tremor had no other parkinsonian features such as rigidity, bradykinesia, hypomimia, or monotonous speech. They also reported falls significantly less frequently and had higher mini-mental state scores . Those in whom the diagnosis was changed to atypical parkinsonism had more severe akinesia , rigidity , and postural instability , less commonly reported an initially or currently good response to levodopa , but more often had incontinence and additional features incompatible with Parkinson’s disease. Those in whom the diagnosis was changed to vascular parkinsonism were older than those in whom a diagnosis of Parkinson’s disease was confirmed , had a larger number of smoking years , more often had gait difficulties as their first complaint , and had more severe postural instability ; they never had a rest tremor.
Sensitivity Specificity And Predictive Value Of A Previous Diagnosis Of Parkinson’s Disease
Of 126 patients with a pre-existing clinical diagnosis of probable and possible Parkinson’s disease in the overall sample , 111 were confirmed as having Parkinson’s disease, resulting in a sensitivity of 88.1% ; similarly, it was confirmed that 54 of 74 patients did not have Parkinson’s disease, resulting in a specificity of 73.0% . The positive and negative predictive values of a previous clinical diagnosis of Parkinson’s disease were 84.7% and 78.3% . In other words, in 85% of patients with a previous diagnosis of Parkinson’s disease this diagnosis was confirmed, and 78% of patients with a diagnosis other than Parkinson’s disease did not have the disease .
When this was broken down by a specialist or other doctor diagnosis, the diagnostic validity was as follows. Neurologists and geriatricians had a sensitivity and specificity of 93.5% and 64.5% , respectively, compared with 73.5% and 79.1% for non-specialists. The positive predictive values were greater for specialists than for other doctors , but the negative predictive values were equivalent v non-specialist 79.1% ).
I Wish I Knew How Vital Stress Management Is To Slowing The Progression Of Parkinsons
Lisa Cone, 57, of Wheat Ridge, Colorado, first experienced Parkinson’s symptoms 12 years ago. Her neurologist later explained that the tremors, insomnia, and intense pain that came with her diagnosis issues could be linked to stress; in fact, research shows that stressful life events may increase the risk of the disease and result in more severe symptoms.
While Cone doesn’t believe stress was the root cause of her Parkinson’s, she’s a firm believer that stress management and listening to your body is vital to one’s wellbeing. “I also wish I’d known I’d have to make difficult life-changing decisions like leaving a high pressure job and a bad marriage in order to reduce my stress—but these changes are worth it,” Cone says.
How Is Constipation An Early Warning Sign Of Parkinson’s It’s Such A Common Problem
A: It’s not as specific as other prodromal symptoms, like anosmia. The rate at which people with chronic and unexplained problems with constipation develop Parkinson’s disease is not as easy to pin down. But if someone has unexplained, persistent constipation, it should at least be noted, as it could be considered prodromal.
You Can Live A Great Life With Parkinsons But You Have To Accept Help Along The Way
After Kelly Weinschreider, 47, of Chicago, Illinois, was diagnosed with Parkinson’s disease at just 29 years old, she was prescribed several medications that lessened her symptoms. Since she felt fine, it made it easier for her to ignore what was going on, especially since she didn’t tell many people about it. “I didn’t want people to feel sorry for me, or for my diagnosis to change my relationships, personally or professionally, ” she said.
That denial—plus side effects from the medicine and the disease’s progression—forced her to leave her job as a quality manager 10 years later. “I should have been seeing a behavioral health specialist to understand how Parkinson’s affected me and how to accept it,” she says. “Instead, I took my medications sporadically. I mismanaged time and commitments, and I had trouble performing my job and, ultimately, spun out. I wish I would have been more forthcoming with family and friends as to how the disease was affecting me.”
After living with the condition for 18 years, Weinschreider came to terms with her diagnosis. She also realized it truly takes a village to live life with Parkinson’s to its fullest and started to communicate with friends and family when she needed help. “You need the support of family and friends, the care of multiple specialists, and the foresight to plan for the future. You can live a great life with Parkinson’s, but you have to accept help along the way,” Weinschreider says.
Patients In Whom A Diagnosis Of Parkinson’s Disease Was Or Was Not Previously Made
Patients in whom a diagnosis of Parkinson’s disease was previously made had a longer disease duration and greater disease severity , with more severe akinesia , postural instability, and rigidity than those in whom the diagnosis was not made before. They were also more likely to be depressed , to have experienced dyskinesias , and to live alone or with their family than in a nursing home .
Sidebar: Morris K Udall Centers Of Excellence For Parkinson’s Disease Research
The Morris K. Udall Parkinson’s Disease Research Act of 1997 authorized the NIH to greatly accelerate and expand PD research efforts by launching the NINDS Udall Centers of Excellence, a network of research centers that provide a collaborative, interdisciplinary framework for PD research. Udall Center investigators, along with many other researchers funded by the NIH, have made substantial progress in understanding PD, including identifying disease-associated genes; investigating the neurobiological mechanisms that contribute to PD, developing and improving PD research models, and discovering and testing potential therapeutic targets for developing novel treatment strategies.
The Udall Centers continue to conduct critical basic, translational, and clinical research on PD including: 1) identifying and characterizing candidate and disease-associated genes, 2) examining neurobiological mechanisms underlying the disease, and 3) developing and testing potential therapies. As part of the program, Udall Center investigators work with local communities of patients and caregivers to identify the challenges of living with PD and to translate scientific discoveries into patient care. The Centers also train the next generation of physicians and scientists who will advance our knowledge of and treatments for PD. See the full list of Udall Centers.
Depression And Anxiety Are Also Early Warning Signs Of Parkinson’s How So
A: Like the other symptoms discussed here, late-onset depression and anxiety are nonmotor prodromal manifestations of the condition. It’s not that everyone who is depressed will get Parkinson’s, and the numbers are lower than they are for symptoms like anosmia and REM behavior disorder. But the link is important to explore, and we are doing more research on it all the time.
What Is Rem Behavior Disorder And How Is It Connected To Parkinson’s
A: REM behavior disorder is different than other sleep problems, like insomnia. People who have it may jerk or kick — it’s as though they are acting out their dreams. In a similar pattern to anosmia, people with idiopathic REM sleep behavior disorder have at least a 50 percent chance of eventually developing Parkinson’s disease.
I Wish I Knew That Depression Can Very Much Be A Part Of Parkinsons
Lou Eisenbrandt, 73, of Overland Park, Kansas was 55 when she was diagnosed with Parkinson’s after dealing with symptoms like a tremor, stiff muscles, and difficulty walking. She was diagnosed with depression shortly after that. “My depression set in a few days after my Parkison’s diagnosis. I was caught off guard—I would cry without knowing why, I had trouble concentrating, and I was dealing with fatigue and anxiety, all of which I’d never experienced before,” Eisenbrandt says.
Her neurologist prescribed an antidepressant, and she also learned holistic ways to minimize her depressive episodes. In addition to doing a bit of exercise each day to keep up her spirits, Eisenbrandt keeps busy with projects that she enjoys, like gardening and cooking. “I also journal and write regularly, sometimes just a line or two about a positive happening during the day,” she says. “Meditation as well as spending time with friends and grandchildren are beneficial for warding off depression, too.”
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
Patients With A Previous Diagnosis Other Than Parkinson’s Disease

Among all patients seen, two were referred for diagnostic purposes without a previous diagnosis, and 69 of 202 patients had a previous diagnosis other than Parkinson’s disease . Among these, 56 patients had been given a diagnosis of non-parkinsonian tremor, two of vascular parkinsonism, one of atypical parkinsonism, and 10 had been prescribed an antiparkinsonian drug for parkinsonian features without a specific diagnosis . Thirteen of the 69 patients with different diagnoses and the two patients referred for diagnostic purposes fulfilled strict clinical criteria for Parkinson’s disease . In two additional patients who had a previous diagnosis of non-parkinsonian tremor, a diagnosis of “possible Parkinson’s disease” was made . If only patients who had at some point in the past seen a specialist were considered, the diagnosis was changed to probable Parkinson’s disease in five and to possible Parkinson’s disease in one .
Sensitivity, specificity, and predictive values for the overall sample* and by type of clinician
Do People Actually Lose Their Sense Of Smell With Parkinson’s
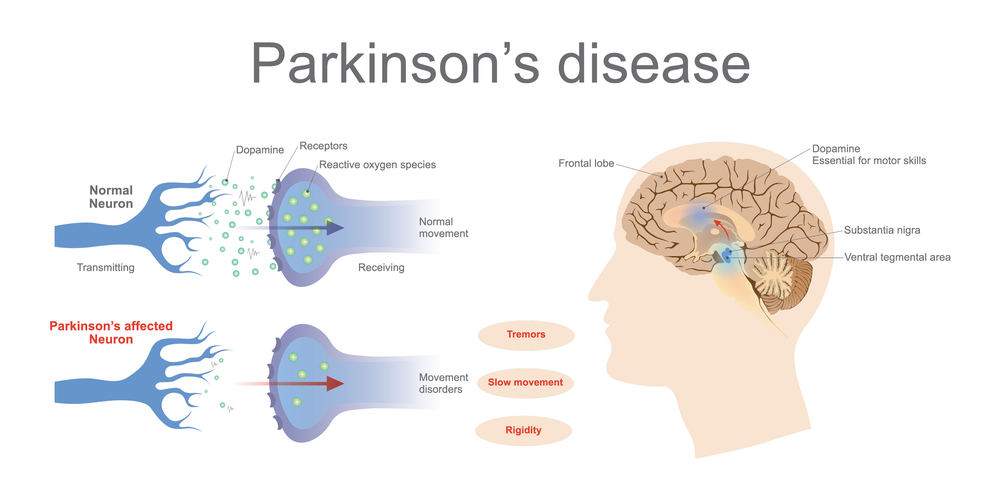
A: Yes. It’s a condition called anosmia, and if you have it with no other disease , you have at least a 50 percent chance of developing Parkinson’s disease in the next five to 10 years. What happens is that alpha-synuclein, the protein that clumps in the part of the brain that regulates dopamine and leads to Parkinson’s disease, also aggregates in the olfactory bulb, the part of the brain responsible for your sense of smell. This happens well before the protein accumulations cause motor symptoms.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Pathological Progression Of Pd And Neuroprotective Therapies
Although lesions in the substantia nigra remain the pathological hallmark of PD, Heiko Braak’s work suggested that the pathology spreads by cell to cell contact. It is postulated that pathology spreads from the periphery into the medulla and olfactory system , progressing further into the brainstem and basal ganglia and ultimately progressing to the limbic system and cortex .
The Braak hypothesis suggests a progression of PD from those who have Lewy pathology without clinical features of PD, to those with end-stage disease and raises the hope of, as Parkinson himself suggested:
‘some remedial process may ere long be discovered by which at least the progression of the disease may be stopped’.
Sadly, convincing disease modifying therapies remain elusive. An extensive list of agents have been tested . Drugs without dopaminergic effect have been unsuccessful. Those with dopaminergic effect are probably effective by masking symptoms rather than actually modifying disease progression. Furthermore, the majority of clinical trials of potential disease modifying agents have been performed in patients with established PD. In these groups, the majority of dopaminergic neurons have been lost potentially meaning that by the time the clinical trial is performed it is too late. Parkinson noted that interventions would only be expected to provide, ‘cure if employed early enough’.
Patients With A Previous Diagnosis Of Parkinson’s Disease
The diagnosis of probable Parkinson’s disease was confirmed in 109 of the 131 patients with this diagnosis , including three in whom atypical features were found but were insufficient to invalidate the diagnosis of Parkinson’s disease . Two additional patients were found to have possible Parkinson’s disease. However, in 20 of the 131 patients the diagnosis of Parkinson’s disease was unequivocally rejected . The alternative diagnoses were non-parkinsonian tremor in four patients , vascular parkinsonism in six , progressive supranuclear palsy in four , and multiple system atrophy in three . Two patients received a diagnosis of idiopathic torsion dystonia, and one of dementia without parkinsonism. When only those patients who had seen a specialist at some point in the past were considered, the diagnosis was changed from Parkinson’s disease to a different diagnosis in 11%.
Patients with an initial diagnosis of Parkinson’s disease
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Treatment Options For Early Onset Parkinsons Disease
Parkinson’s treatment aims to slow the disease’s progression. Medication treatment options may include the following:
- Levodopa is a chemical that’s converted to dopamine in the brain. People with early onset Parkinson’s may experience more negative side effects, such as involuntary movements.
- MAO-B inhibitors can help reduce the breakdown of dopamine in the brain.
- Catechol-O-methyltransferase inhibitors can help extend Levodopa’s effects on the brain.
- Anticholinergics can help reduce tremors.
- Amantadine may be used to improve muscle control and relieve stiffness.
Defining Populations At Risk For Parkinsons Disease
One of the areas of research that aims to aid in the early detection and treatment of PD is seeking to identify “biomarkers”—protein or chemicals in the blood, urine, or cerebrospinal fluid that reliably help diagnose PD, particularly at the early stage. For example, a recent study detected aggregates of alpha-synuclein in the cerebrospinal fluid. These aggregates were found in PD patients but not patients with other neurologic disorders. Many research studies are attempting to identify new biomarkers, particularly those that may even predict whether someone will develop PD over time.5
Tips For Caring For Someone With Parkinsons Disease
Caring for a loved one with early onset Parkinson’s can be difficult. If you’re a caregiver for someone with this condition, it’s important that you remember your own emotional and physical health.
Not only are you dealing with a difficult diagnosis, you’re also managing an increased number of responsibilities. Burnout is common in caregivers, so make sure you’re checking in with your own needs.
The Michael J. Fox Foundation Center for Parkinson’s Research recommends these tips for caregivers:
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Likelihood Of Referral According To Final Diagnosis
Overall, 74% of all cases with a diagnosis of Parkinson’s disease had been seen by a specialist. However, when these cases were classified by final diagnosis , it was observed that, paradoxically, fewer cases with atypical disease had been seen by a specialist compared with those with classical Parkinson’s disease ; p = 0.02).
Braaks Hypothesis On How Parkinsons Disease Begins
Braak’s hypothesis, named for professor Heiko Braak, MD, who outlined the theory in 2003, suggests that rather than beginning in the brain, Parkinson’s disease begins in the periphery of the body. Braak’s hypothesis proposes that the earliest signs of PD are found in the gut and the olfactory bulb, an area of the brain involved in the sense of smell.2-4
The accumulation of the protein alpha-synuclein is believed to begin in the gastrointestinal tract or the olfactory bulb before progressing to other areas of the brain. After the aggregates of alpha-synuclein have formed, they appear to be capable of growing and spreading from nerve cell to nerve cell across the brain.2-4
The appearance of alpha-synuclein aggregates coincides with the appearance of symptoms: alpha-synuclein aggregates in the brainstem correlates with the onset of motor symptoms. Appearance of alpha-synuclein aggregates in the cortex correlates with dementia and cognitive dysfunction.2-4
What Doctors Look For When Diagnosing Parkinsons
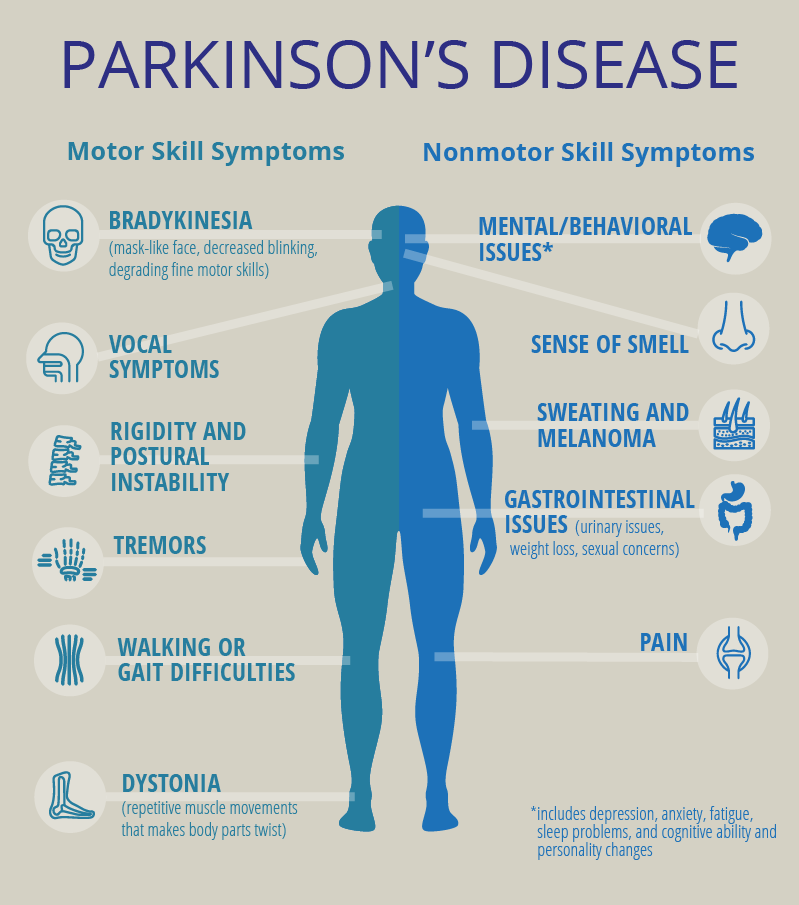
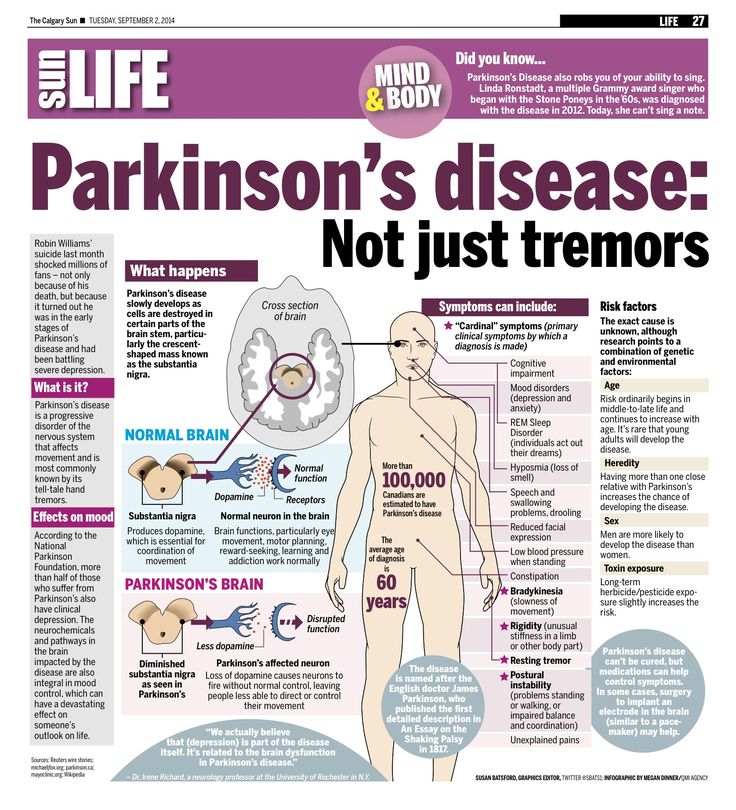
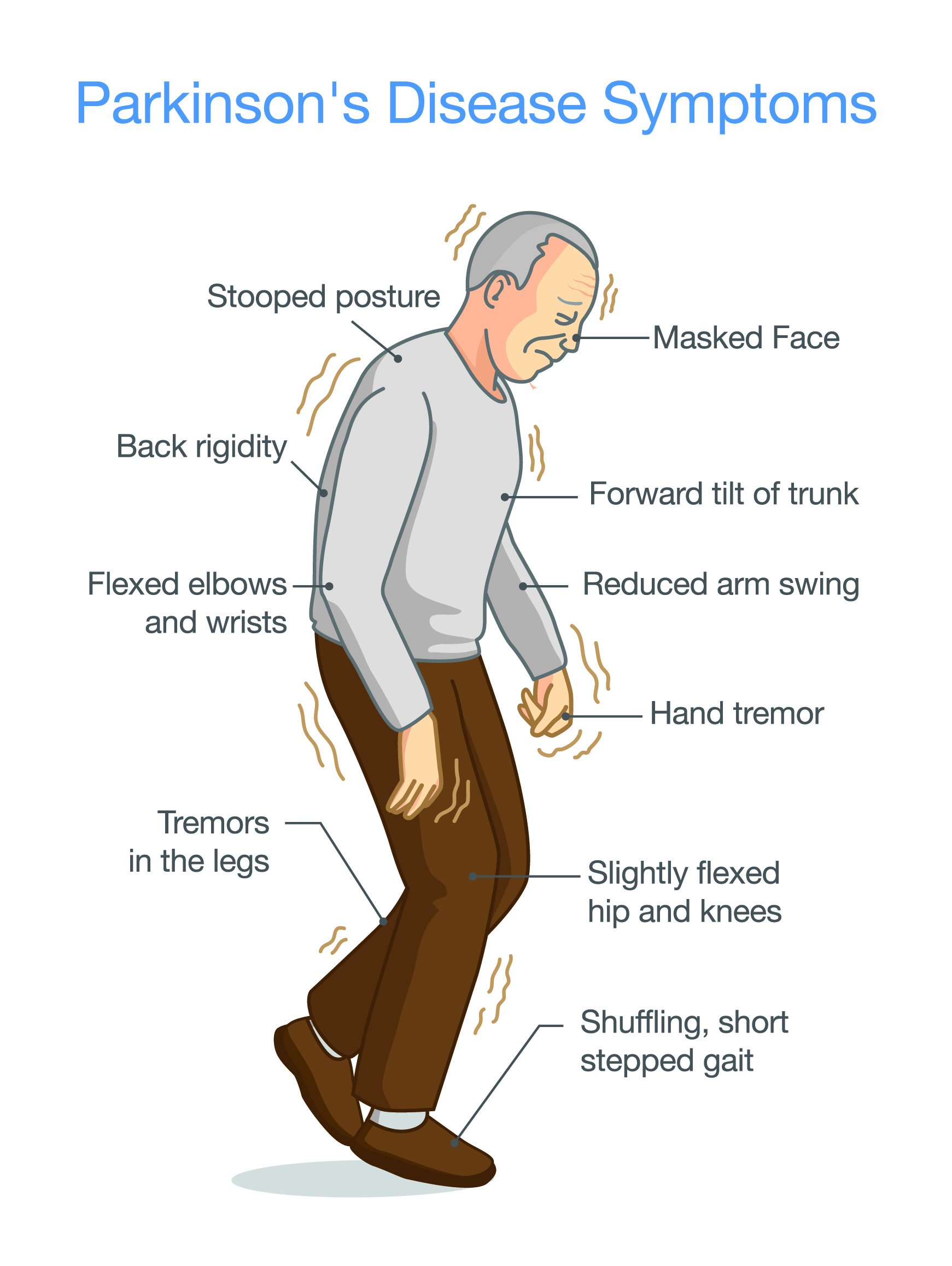
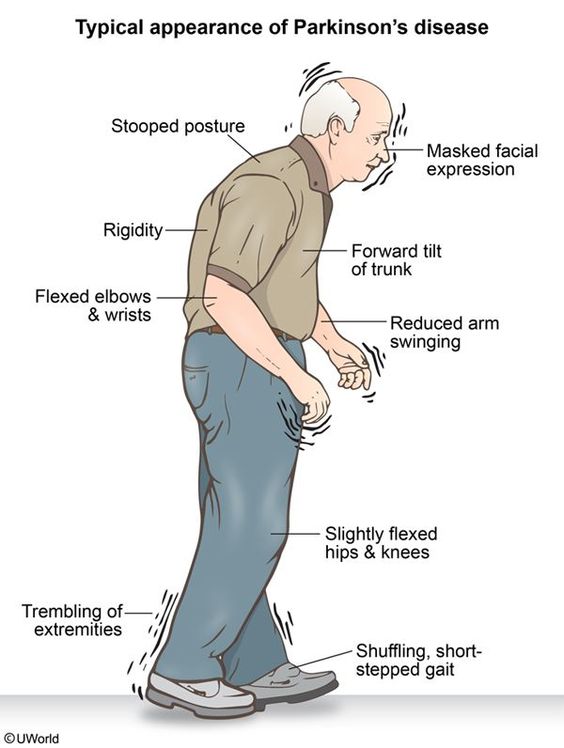
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Sidebar: Ninds Steps Up Pursuit Of Pd Biomarkers
In 2012, the NINDS dramatically accelerated efforts to identify biomarkers by establishing the Parkinson’s Disease Biomarkers Program . This unprecedented program unites a range of stakeholders from basic and clinical researchers to healthcare professionals, the NINDS staff, information technology experts, and people living with PD and their families.
PDBP supports research and builds resources aimed at accelerating the discovery of biomarkers to ultimately slow the progression of PD. For example, the program has established a repository of biological specimens and a Data Management Resource system maintained by the NIH Center for Information Technology. The DMR allows researchers to access clinical, imaging, genetic, and biologic data, while a complementary PDBP-supported project develops statistical tools to analyze vast quantities of data so that patterns can be identified across these diverse sources of information.
How Early Can Parkinson’s Disease Be Diagnosed
A: A true determination of Parkinson’s disease is a clinical diagnosis, which means certain motor symptoms have to be present, but we now know more about some early signs of Parkinson’s disease that, while they don’t always lead to the condition, are connected.
In terms of how early we can detect, we can detect a mutation that is associated with an increased risk of Parkinson’s as early as birth. In the minority of patients who may have a known Parkinson’s-related genetic mutation , that gene could be tested for at any time in life. At the same time, that’s not diagnosing Parkinson’s; it’s just identifying the risk.
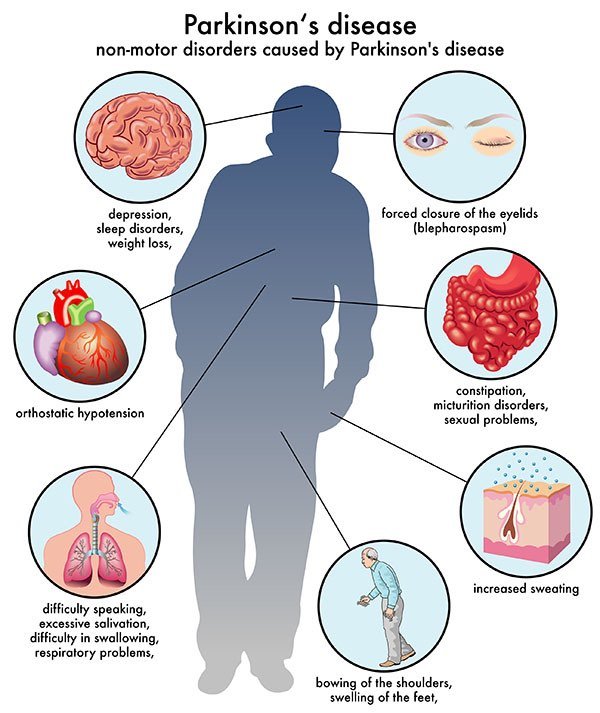
Early warning signs are what we call prodromal, or preclinical, symptoms. Prodromal symptoms are an early warning sign that someone might get Parkinson’s disease. Though some of these symptoms have a very high probability of signaling future Parkinson’s, having one or more of them is still not a 100 percent probability. Some prodromal symptoms are loss of sense of smell, REM behavior disorder, anxiety or depression, and constipation.
What Would Parkinson The Social Reformer Think
Parkinson was a social reformer writing under the nom de plume ‘Old Herbit’ he campaigned for the rights of ‘lunatics’, children, and older people. Age is the strongest risk factor for PD. Worldwide prevalence of PD per 100,000 is 41 at 40–49 years compared to 428 at 60–69 years; and 1,903 in those older than 80 years . 200 Years ago, when Parkinson wrote the Shaking Palsy, average life expectancy at birth in the UK was less than 45 years. For a women born in the UK 2010, this is now 82 years. In recent years life expectancy has also begun to increase in the developing world resulting in an increased burden of chronic disease. Traditionally healthcare systems in the developing world have been focused on managing communicable disease in younger populations. As their populations age the need to manage chronic disease in an ageing population will present an increasing challenge. Dorsey et al. have projected that the number of individuals living with PD will more than double between 2005 and 2030, and that the population of PD patients is set to become increasingly concentrated in the developing world .
Conditions Misdiagnosed As Parkinson’s Disease Neuroscience
Parkinsons disease, especially in its early stages when symptoms are mild, is not an easy disease to diagnose. The non-specific, and easily overlooked nature of the signs of Parkinsons make it difficult to spot, and unlike many illnesses, there is no one laboratory test or radiological exam that will provide a definitive diagnosis of Parkinsons disease.
Patients exhibiting Parkinsons-like symptoms may undergo blood and urine tests, or CT or MRI scans to exclude other conditions, but none of these will provide a diagnosis of Parkinsons disease. The best way to test for Parkinsons disease is to conduct a systemic neurological examination that includes tests to gauge a patients reflexes, muscle strength, coordination, balance, gait, and overall movement. Even so, according to information presented on The Michael J. Fox Foundation for Parkinsons Research, up to 25 percent of Parkinsons disease diagnoses are incorrect.
So, why is there confusion about diagnosing Parkinsons disease? The simple answer is that symptoms of Parkinsons disease are not clear cut, and therefore, it is easy to mistake them for other conditions, or to classify them as parkinsonian when they are not.
Here is a brief overview of the top ten conditions mistaken for Parkinsons disease:
Beyond those top three, there are other conditions that are often confused with Parkinsons disease, including:
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
