Q: My Husband Has Pd With Moderate Symptoms Normally He Is Independent With All His Activities Although He Walks Slowly One Day His Symptoms Worsened Dramatically And He Was Not Able To Walk I Took Him To The Er Where He Tested Positive For Covid
A: In general, people with PD and other brain illnesses often have 1) worsening of their PD symptoms in the face of inter-current illnesses such as COVID-19, and 2) have a slower recovery to their baseline once they have recovered from the inter-current illness. It sounds like both of these have happened to your husband. However, with proper rehab and some perseverance, there is hope that he will slowly return to his baseline.
Q: Once I Am Vaccinated Can I Go Back To Doing Things As I Was Doing Them Before The Pandemic Does The Emergence Of The Delta Variant Change Anything
A: The CDC continually updates its guidelines in response to evolving public health conditions.
- Fully vaccinated people can participate in many of the activities that they did before the pandemic; for some of these activities, they may choose to wear a mask.
- To reduce the risk of becoming infected with the Delta variant and potentially spreading it to others, everyone, including those who are fully vaccinated, should wear a mask in public indoor settings if they are in an area of substantial or high transmission. The CDC constantly updates the map of US counties for which this applies. You will need to refer to your local public health authorities to determine whether your area is one with substantial or high transmission
- Fully vaccinated people might choose to mask regardless of the level of transmission in their area, particularly if they or someone in their household is immunocompromised or at increased risk for severe disease, or if someone in their household is unvaccinated. People who are at increased risk for severe disease include older adults and those who have certain medical conditions, such as diabetes, overweight or obesity, and heart conditions.
If Someone Did Not Have Parkinsons Before Is It Likely That They Will Develop It After Recovering From Covid
Dr. Okun: We do not have the numbers on how common it is to receive a Parkinson’s diagnosis after recovering from COVID-19. There are several intriguing papers on how COVID-19 may affect the brain and how it may possibly contribute to Parkinson’s risk. At this point, we caution the public and researchers not to speculate until we have more data.
I Do My Best To Remain Optimistic And Cling To The Fact That The Parkinsons Diagnosis Is Overturned
Neurologists told me that the three drug components of Stalevo would be out of my system within a few weeks, but my brain only felt clear in February 2016 – four months after I’d stopped taking it. The huge range of motor and non-motor symptoms persists and other new ones have arrived since my body stopped receiving the added, yet unnecessary, dopamine. I do my best to remain optimistic and cling to the fact that the Parkinson’s diagnosis is overturned.
Look out for another article by Joanne in the coming weeks, discussing the issue of misdiagnosis in more depth. Joanne has written about her experiences on her blog here
I Have Parkinsons And Blood Pressure Issues Should I Be Worried About Getting The Vaccine
Dr. Okun: No. You will most likely be sitting when you get the vaccine, so if you get faint or have a change in your blood pressure you should be okay. Stay hydrated; it will help with changes in blood pressure. Take a water bottle and a snack with you. You will likely be asked to sit in a waiting area for 15-20 minutes after each shot to make sure you do not have a reaction. If you can drink a small bottle of water either immediately before or immediately after the shot, we believe this is a good idea, especially if prone to fainting.
What Do People With Parkinsons Need To Bring With Them For Their Vaccine Appointment
Dr. Okun: Take your personal information and medication list. If you are prone to fainting, let the nurse know. For the second shot, bring the card issued to you on the first shot, so that the vaccine administration can be documented. Take a picture of the card once you have both shots so that you always have a copy.
A Decade Of Unnecessary Parkinsons Drugs Is Likely To Have Remodelled My Brain
A key issue is that I no longer have a convenient label for my symptoms. I had pre-existing joint and gastro issues that have worsened immeasurably during the past decade. My ability to concentrate, to function, to move, to ‘be’ all worsened beyond comprehension. I have been told that nearly a decade of unnecessary Parkinson’s drugs is likely to have remodelled my brain, through its innate neuroplasticity, so that it now considers the symptomatic side effects of those drugs ‘normal’ for me. Just as hitting a tennis ball every day for 10 years will build up your ball-hitting skills, so the brain can be driven by drugs and their side effects into behaviours that it then reconfigures and learns as normal.
‘Writhing and contorting’
Actually weaning myself off Stalevo – a Parkinson’s medication used to increase dopamine levels in the brain – which I was taking eight times a day, was pretty terrifying. I was initially advised to drop one daily dose per week. By the second week I was writhing and contorting involuntarily – not something I had ever done before. I was then asked to drop one daily dose per month. I took my last Stalevo dose on 25 October 2015.
Ask Your Doctor If You Can Change The Time At Which You Take Your Meds
Don’t experiment with the timing of your Parkinson’s disease drugs yourself, because this can result in a variety of complications. You can, on the other hand, ask your doctor whether it is possible to take your medications at a different time of day. Meds that induce sleepiness may be better taken before bedtime, for instance, while those drugs that have insomnia as a side effect may be better taken earlier in the day. Your doctor will have had more experience in prescribing the medications you take, and will have helpful tips to share.
In A Sense The Certainty Of Diagnosis Was Good I Belonged Somewhere
Post-misdiagnosis
I still have no confirmed diagnosis. The swathe of neurological symptoms still persist today – some aspects of movement are identified as functional movement disorder, but otherwise it has been a question of ruling in/out alternative causes for some symptoms.
One theory is that an initial brain insult during the 2006 anaesthetic, together with a gastro drug I was taking at the time that has Parkinsonism as a side effect, combined to give me Parkinson’s disease. But now this original brain insult plus nine years of my brain’s neuroplasticity being driven into new behaviours by Parkinson’s drugs, plus issues that arose during Parkinson’s drug withdrawal are the current neurological problems that I have to contend with.
Fortunately, while there is widespread dysfunction, I have been told that there does not appear to be any brain disease processes associated with these symptoms. Again, there are no tests to prove/disprove this and one remains reliant on the expertise of brilliant neuroscientists.
Q: Are There Any Reasons Why A Person With Pd Should Not Get A Covid
A: There are no substantiated scientific concerns to suggest that the vaccines have a different safety profile in people with PD as compared to the general population, so what we know about the vaccines for all-comers would hold true for those with PD. Having PD might lead to a more complicated infection should you contract COVID-19, plus people with PD also tend to be older which further increases the risk for complicated COVID-19 infection. Because of these issues, vaccination for COVID-19 for people with PD is a good idea. Discuss with your doctor any concerns you have about the COVID-19 vaccine.
What Should I Know About Storage And Disposal Of This Medication
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture .
Store cassettes containing levodopa and carbidopa enteral suspension in the refrigerator in their original carton, protected from light. Do not freeze the suspension.
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA’s Safe Disposal of Medicines website for more information if you do not have access to a take-back program.
It is important to keep all medication out of sight and reach of children as many containers are not child-resistant and young children can open them easily. To protect young children from poisoning, always lock safety caps and immediately place the medication in a safe location – one that is up and away and out of their sight and reach. http://www.upandaway.org
Ways To Cope With The Side Effects Of Parkinsons Disease Drugs Drugs & Medications
Prescription drugs are the most powerful tools modern science has available to help you fight your Parkinson’s disease symptoms — but the very medications designed to make your life better can also cause side effects.
These side effects range from unpleasant to downright scary .
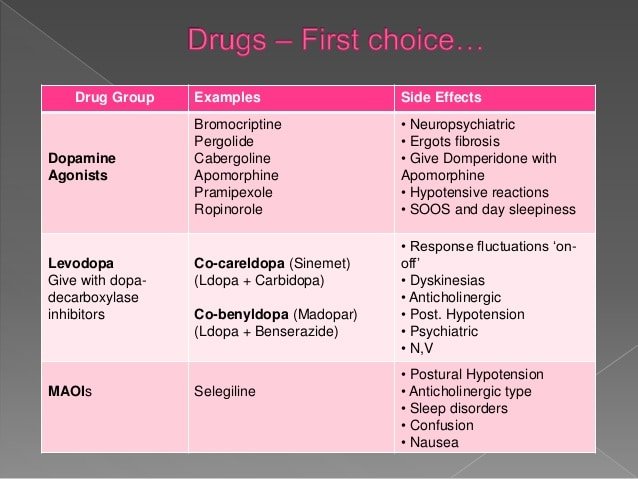
If you have Parkinson’s disease, you will already be familiar with the most frequently prescribed Parkinson’s disease medications:
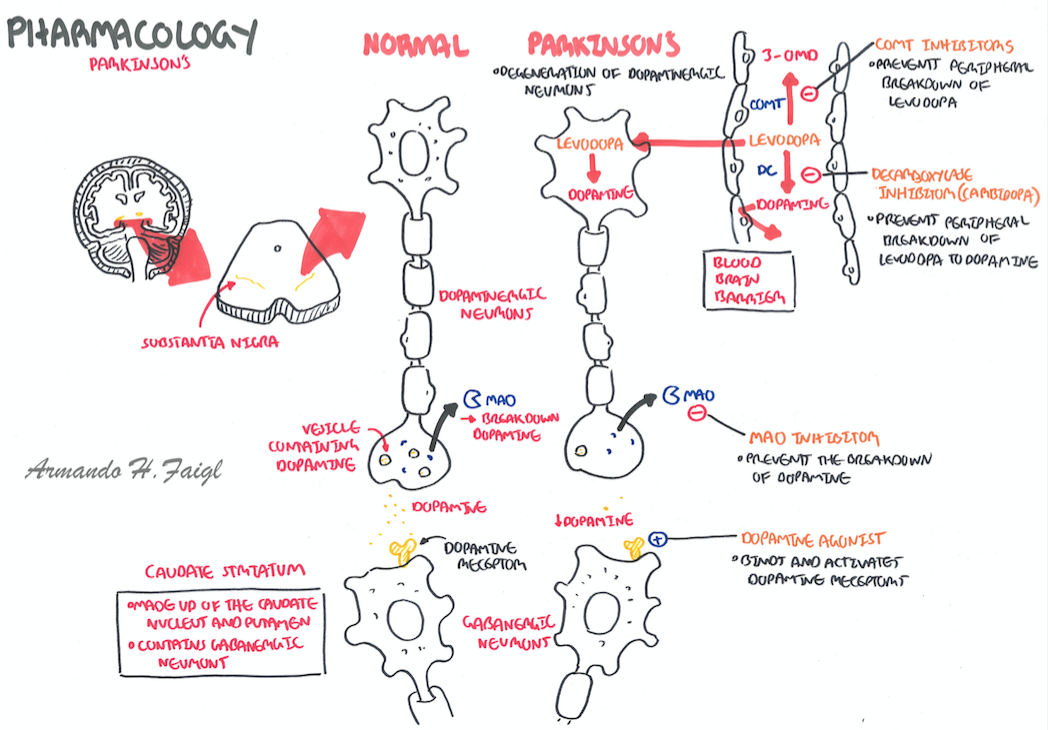
- Levodopa works to boost your dopamine levels indirectly, and is almost always prescribed in combination with carbidopa. Brand names include Sinemet, Rytary, Parcopa, and Stalevo, and they’re powerful weapons in the fight against the motor symptoms of Parkinson’s disease.
- Dopamine agonists — like pramipexole , ropinirole , apomorphine , and Neupro — act similarly to dopamine, thereby reducing your Parkinson’s disease symptoms.
- COMT inhibitors, like entacapone , are prescribed to make levodopa work more effectively.
- MAO-B inhibitors help your brain use the dopamine it does have access to more efficiently, and examples are selegiline and rasagiline .
- Amantadine is both an anti-flu and Parkinson’s drug, and it is particularly useful in combating the involuntary movements levodopa can result in.
- Dyskinesia — involuntary movements, which can strike the arms, legs, torso, and face
- Nausea and vomiting
- Diarrhea, constipation, and urinary difficulties, including discolored urine and finding it hard to pee
- Dizziness or lightheadedness
Q: I Am On Amantadine For My Pd I Know That It Is Also An Anti
A: We do not have evidence that amantadine acts against COVID-19, so you should continue to assume that it is not effective against this coronavirus.
Tips and Takeaways
- Most people who are infected with COVID-19 will recover completely. However, older adults and those with underlying medical issues such as advanced PD are at an increased risk of developing serious outcomes from COVID-19 as compared to those who are younger and healthier.
- Three COVID-19 vaccines have been approved in the US.
- Getting vaccinated reduces your chances of contracting COVID-19, but those who are vaccinated can still contract COVID-19.
- Vaccination is about 90% effective in protecting against severe illness, hospitalization, and death, even for the new Delta variant
- Continue to monitor CDC guidelines for information on COVID-19.
- Talk with your doctor about any concerns you have about COVID-19 or COVID-19 vaccines.
Do you have a question or issue that you would like Dr. Gilbert to explore?
Dr. Rebecca Gilbert
APDA Vice President and Chief Scientific Officer
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
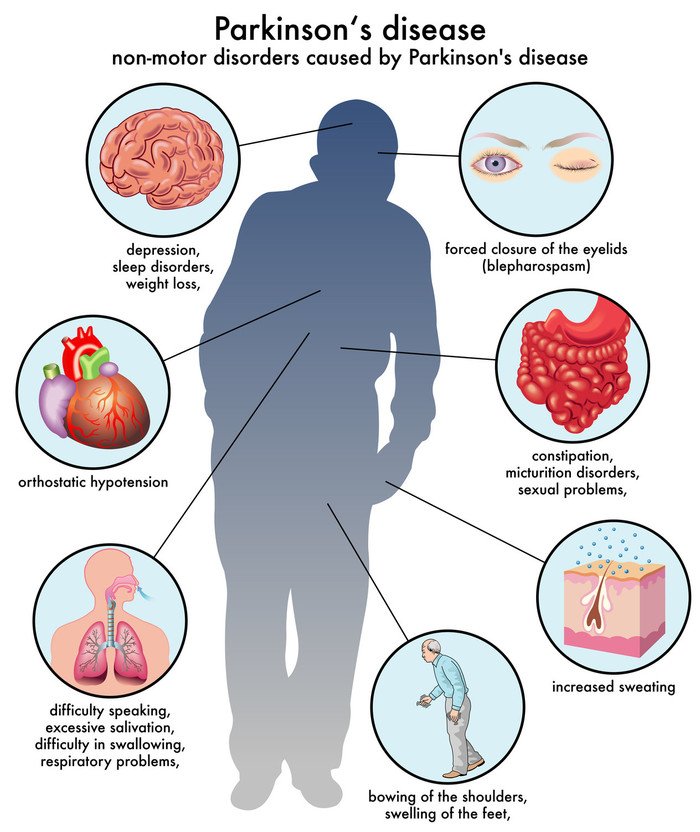
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Learning How To Reduce Side Effects Of Parkinsons Treatment
Patients often develop unwanted side effects of Parkinson’s drugs when on them for a long time. A new study compares an old standby with newer options.
Treatments for Parkinson’s disease can be very effective, but they all produce side effects, leaving patients and their doctors wondering which drug or combination of drugs will work the best.
Now a large study comparing the three leading treatments shows the oldest to be the best—but not by a large margin—which leaves plenty of reasons to keep using the more recently developed alternatives. The results were published in the June 11 online edition of the journal The Lancet.
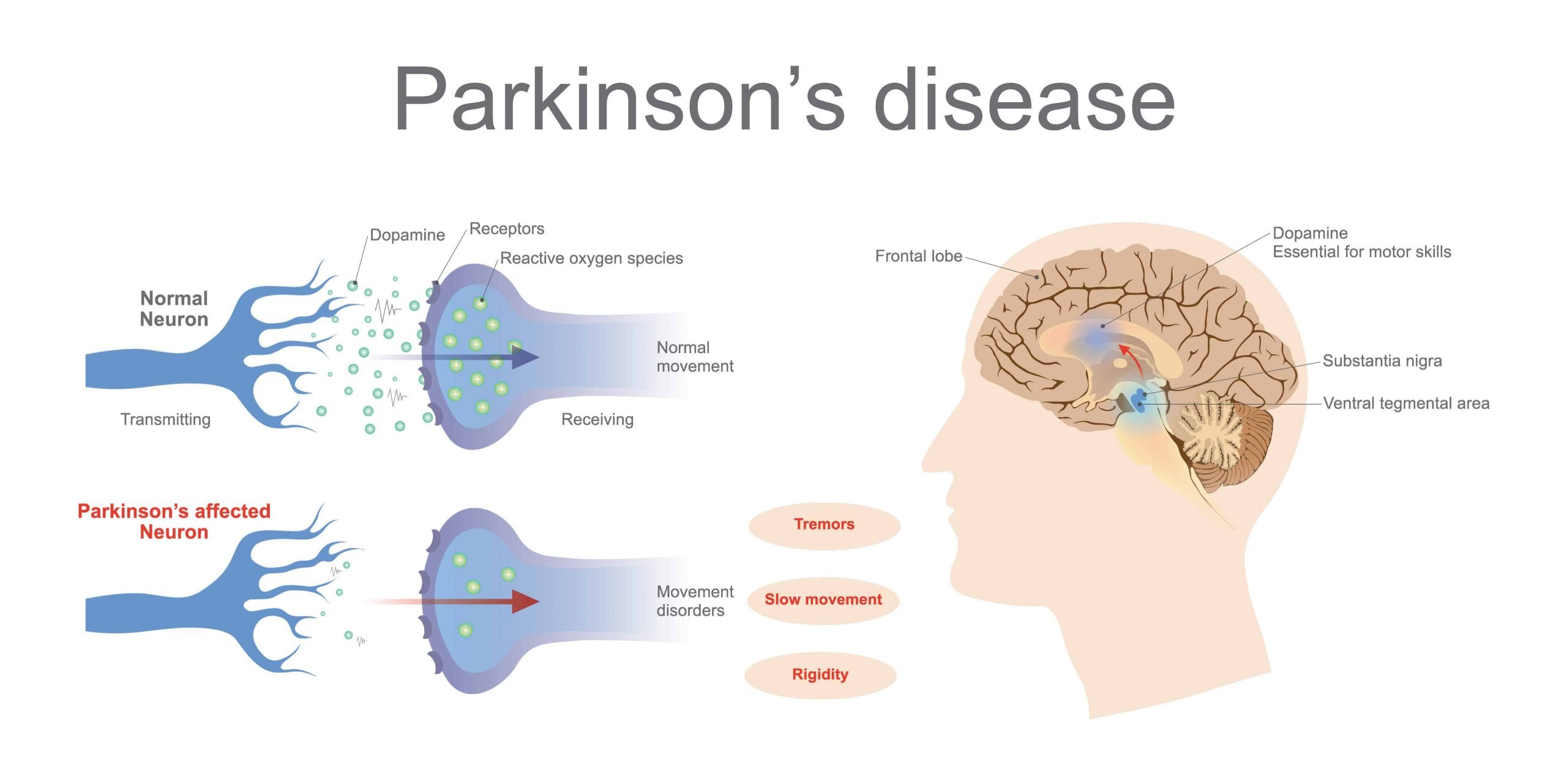
Without treatment, PD eventually becomes disabling. People first develop a slight tremor, usually in a finger or a hand, or twitching in the arms or legs. Then they start to feel as though their feet are stuck to the floor when they try to take a step.
All of these problems result from the death of cells that are located deep within the brain. Those cells produce dopamine, a brain chemical essential for normal muscle movement. When the level of dopamine in the brain drops below a certain level, symptoms emerge and, without treatment, they worsen, making walking and other simple daily activities like drinking a cup of coffee difficult.
Fortunately, since the 1960s, people with PD have been able to take levodopa, which nerve cells in the brain use to make dopamine, and reverse most of the symptoms for a few hours.
iSTOCKPHOTO/MMEEMIL
Do People With Parkinsons Get Priority Access To The Covid
Each state has its own process for rolling out the vaccine to different population groups. If you would like to advocate for people with Parkinson’s to be part of a priority group, we encourage you to contact your elected officials. We have created a letter that you can personalize and send them either by mail or electronically.
Treatment Of Motor Disorder Side Effects Associated With L
This example describes a multicenter, randomized, double-blind, placebo-controlled, dose finding study of oral eltoprazine in Parkinson’s patients with L-DOPA induced dyskinesias, in a levodopa challenge-dose setting in Parkinson’s Disease. A total of 22 patients participated in the study, out of which 18 patients fulfilled the protocol in terms of eligibility, interventions, and outcome assessment.
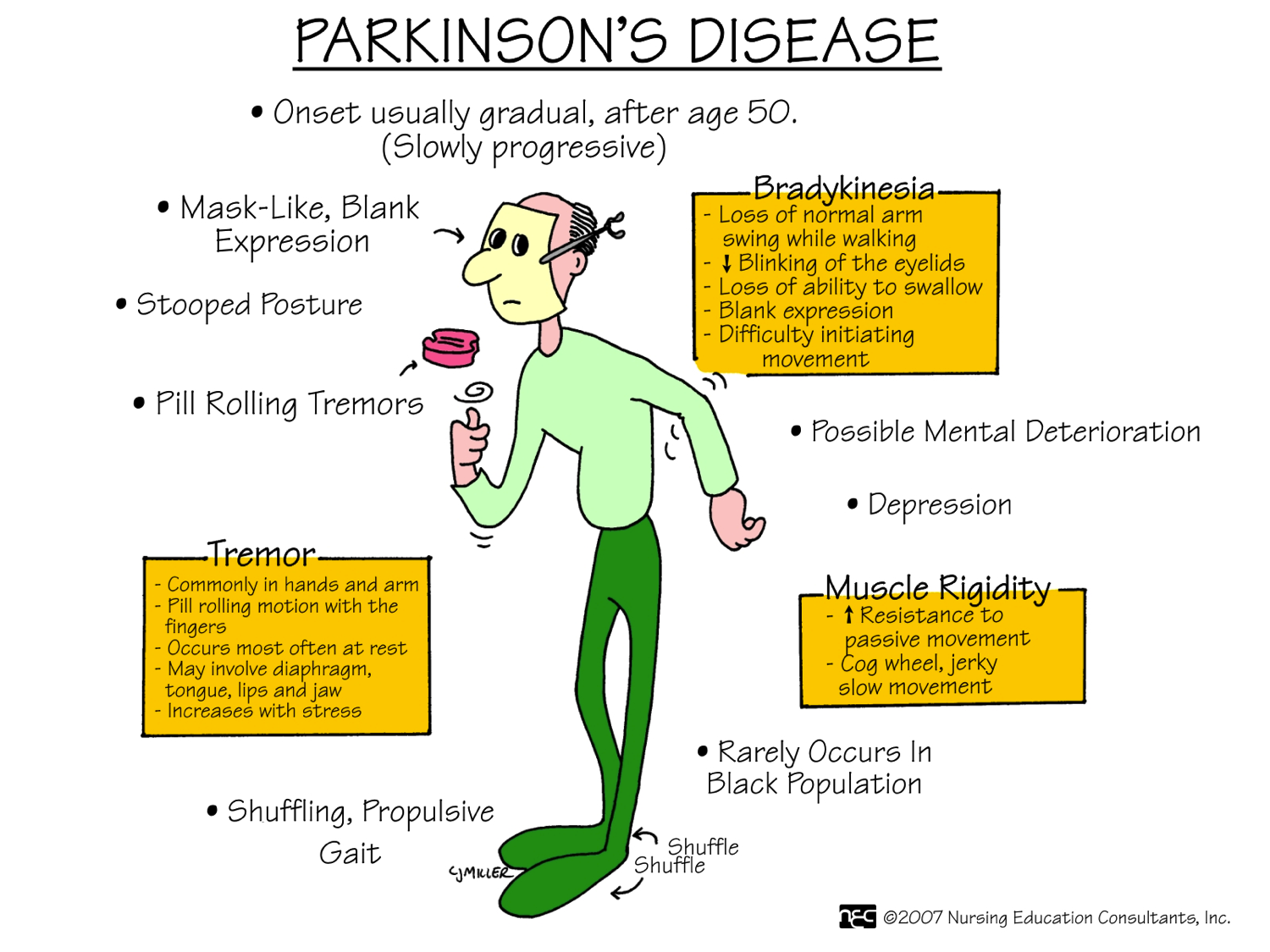
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Read more about Parkinson’s tremors
Rigidity
Bradykinesia
mask-like expression of the face
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
If Levodopa Causes Dyskinesia Then Why Should I Take It

At present, treatment with levodopa is the most effective way to relieve tremor, stiffness, and slow movement associated with Parkinson’s. In the early stage of Parkinson’s, levodopa may not be necessary and there are other medications available to treat this stage of the disease. However, as the disease progresses and symptoms begin to interfere with daily living, your doctor will prescribe levodopa.
- It typically doesn’t develop immediately – It’s important to note that there is usually a time lag of roughly 4 to 10 years from the start of treatment with levodopa to when dyskinesia emerges, and its severity will vary among different individuals.
- Younger people are at a greater risk –People who get Parkinson’s in their later years may not show signs of dyskinesia or may have only mild symptoms within their lifetime. Being diagnosed with Parkinson’s at a younger age is associated with a greater chance of developing dyskinesia.
- As with every aspect of Parkinson’s, there is variability in dyskinesias – Some do not develop dyskinesias at all. For those who do get them, not all experience them the same. Dyskinesia in its milder form may not be bothersome, and the mobility afforded by taking levodopa may be preferable to the immobility associated with not taking levodopa. People with Parkinson’s must weigh the benefits from using levodopa versus the impact of dyskinesia on their quality of life.
Nuplazid Side Effects List For Healthcare Professionals
The following serious adverse reactions are discussed elsewhere in the labeling:
- Increased Mortality in Elderly Patients with Dementia-Related Psychosis
- QT Interval Prolongation
Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
The clinical trial database for Nuplazid consists of over 1200 subjects and patients exposed to one or more doses of Nuplazid.
- Of these, 616 were patients with hallucinations and delusions associated with Parkinson’s disease psychosis .
- In the placebo-controlled setting, the majority of experience in patients comes from studies evaluating once-daily Nuplazid doses of 34 mg compared to placebo for up to 6 weeks.
In the controlled trial setting, the study population was approximately 64% male and 91% Caucasian, and the mean age was about 71 years at study entry.
- Additional clinical trial experience in patients with hallucinations and delusions associated with PDP comes from two open-label, safety extension studies .
- The majority of patients receiving long-term treatment received 34 mg once-daily .
- Over 300 patients have been treated for more than 6 months; over 270 have been treated for at least 12 months; and over 150 have been treated for at least 24 months.
Common Adverse Reactions :
Postmarketing Experience
Ask Whether Your Dosages Or Medications Can Be Changed
Parkinson’s disease patients who experience side effects like dyskinesia may be getting too much levodopa, and can talk to their doctor about the possibility of reducing the dose, or adding in more carbidopa. These small tweaks to your medication regime may reduce your side effects without affecting the efficacy of the drug. You can also inquire about taking long-acting carbidopa/levodopa, which releases the medications into your blood stream at a slower rate and tends to have fewer side effects because of that.
Side Effects Not Requiring Immediate Medical Attention
Some side effects of levodopa may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common
- Discolored sputum or nasal discharge
- falls
- pain in the arms or legs
- skin scraping or tearing
Applies to levodopa: compounding powder, inhalation capsule, oral capsule, oral tablet
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Q: I Have Parkinsons Disease Should I Receive A Covid
A: For information about the COVID-19 vaccines – how they work, safety, and more — please visit our updated COVID-19 information section. In general, your age alone increases your risk of complications from COVID-19 infection. Depending on what PD symptoms you have, PD can also increase the risk of complications from the virus. For these reasons, it would be wise to protect yourself as much as possible from COVID-19, which would include getting vaccinated. As always, speak to your doctor about your individual clinical situation and to find out when and where you will be able to get the vaccine.
Side Effects Of Your Specific Parkinson’s Medication
To check what specific side effects your medication can have, read the information leaflet that comes inside the packet.
We’ve listed some general information about side effects in our information about individual Parkinson’s drugs
If you’re under treatment for coronavirus and are experiencing side effects with your Parkinson’s treatment, please report it on the government’s Yellow Card website.
Im Allergic To Other Vaccines Should I Get The Covid
Dr. Okun: In many cases, people with allergies to vaccines may possibly receive the Moderna or Pfizer vaccines. Side effects including allergies to vaccines are usually caused by the fluid surrounding the vaccine itself. Do not assume you cannot get this vaccine; talk to your doctor. Old fashioned vaccines are manufactured in a completely different fashion as compared to the current COVID-19 vaccinations. It will be rare for someone to not be able to receive the vaccines; we believe most people are eligible.
Q: Are There Any Studies Of The Effects Of The Covid
A: Currently, there is no data that the COVID-19 vaccine has any long-term negative effects on anyone, including those with PD. Some people with PD have reported a worsening of PD symptoms in the short term after vaccination, which then resolve. The Center for Disease Control instituted a vaccine safety monitoring system, called v-safe, which captures side effects of the vaccine. If you have side effects from the vaccine and have PD, you can alert the CDC using this system. This will be an invaluable tool for scientists to discover trends in vaccine side effect profiles.
Q: How Does The Delta Variant Affect Someone With Pd
A: We do not have any specific data yet on how the Delta variant affects people with PD.
The COVID-19 virus, like all viruses, is able to mutate and create variants of itself. Many variants of COVID-19 have been identified around the world. Only a few of these variants have been of concern to public health however, because they have a characteristic that makes the virus either more easily transmissible or more likely to cause significant disease. The Delta variant is currently the variant of concern and has been shown to be more easily transmitted from person to person than prior variants of COVID.
The vaccines approved in the US do offer protection against the Delta variant, but not to the extent that was seen in the original trials. That means that fully vaccinated people are more likely to get infected with the Delta variant of COVID-19 than other variants. However, the major goal of the vaccines is to prevent severe illness, hospitalization, and death from COVID-19 and all the approved vaccines are approximately 90% effective in preventing these consequences of infection. Therefore, vaccination remains extremely valuable.
Does Nuplazid Cause Addiction Or Withdrawal Symptoms
Drug Abuse And Dependence
Nuplazid is not a controlled substance.
Abuse
Nuplazid has not been systematically studied in humans for its potential for abuse, tolerance, or physical dependence.
While short-term, placebo-controlled and long-term, open-label clinical trials did not reveal increases in drug-seeking behavior, the limited experience from the clinical trials do not predict the extent to which a CNS-active drug will be misused, diverted, and/or abused once marketed.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
What Are The Differences Between Available Vaccines
Dr. Okun: Moderna and Pfizer vaccines are distributed in the U.S. and in other countries, with 94 and 95 percent effectiveness. Both require two dosages and need to be stored at incredibly low temperatures — the Pfizer vaccine requiring an even lower storage temperature than the Moderna vaccine — making distribution and storage a challenge. These two vaccines belong to a new treatment approach called messenger RNA vaccines, which create a COVID-19 defense system.
Other vaccines are in development around the world and most work more like a traditional vaccine . They send instructions through DNA, teaching the immune system how to respond to COVID-19. There are several vaccines in early development, but these have the most available information:
- Oxford–AstraZeneca: distributed in the U.K. with ~70 percent effectiveness. It works in two dosages. The major benefit to this vaccine is that it can be stored at refrigerator temperatures. The vaccine may be more effective if a weakened first shot is followed a few weeks later by a standard dose.
- Sinovac and Sinopharm: created in China with ~78-80 percent effectiveness using two dosages. There is limited data on these vaccines. Sinovac is currently in late-stage trials in other countries.
- Sputnik V: distributed in Russia and works using two dosages. Early reports are of ~92 percent effectiveness. However, there is limited data on this vaccine.
