I Do My Best To Remain Optimistic And Cling To The Fact That The Parkinsons Diagnosis Is Overturned
Neurologists told me that the three drug components of Stalevo would be out of my system within a few weeks, but my brain only felt clear in February 2016 – four months after I’d stopped taking it. The huge range of motor and non-motor symptoms persists and other new ones have arrived since my body stopped receiving the added, yet unnecessary, dopamine. I do my best to remain optimistic and cling to the fact that the Parkinson’s diagnosis is overturned.
Look out for another article by Joanne in the coming weeks, discussing the issue of misdiagnosis in more depth. Joanne has written about her experiences on her blog here
Tom Thought That Because Some Pink Tablets Relieved His Symptoms This Meant He Was Ok He Didn’t
I first suspected there was something wrong when I was travelling and I was writing a postcard to a friend of mine in, in Australia whose name is Anthony Diecopolis. And, and I got to the Anthony Diec and I couldn’t finish the opolis. And it’s very strange my hand had sort of gone into a sort of spasm and it just wouldn’t, wouldn’t finish writing the, the, the word. And so that’s a bit strange.
And so I went when, when I got I, I went to the doctor and said, “What on earth’s going on?” And I had since then I’d also developed this slight tremor in my right hand. He said, “Well it’s probably, Essential Tremor or trapped nerve or something like that”. And anyway, then it got a bit worse and then I was, I was recommended to go to a neurologist. And the neurologist had a look at me and gave me some pills. And he said, “Come back and tell me if these work”.
This is about, about sort of, nine months after my, my not being able to finish the, the postcard. And, and he said, “Take these pills”. And the pills worked. Magically the tremors stopped and I thought this is wonderful. And so I went back to the neurologist and I said, “Yes everything’s fine now. The pills have, the pills have worked.” And far from looking happy about this he looked rather, rather grave and he said, “I think you’d better go to another neurologist.”
Comparison Of Patients In Whom A Diagnosis Of Parkinson’s Disease Was Maintained Or Rejected
Patients in whom a diagnosis of Parkinson’s disease was confirmed had more severe disease as measured by the Hoehn and Yahr stage , more often had a tremor at rest or a classical pill rolling tremor , and more often reported a good initial and sustained response to levodopa than those in whom it was rejected.
Patients in whom the diagnosis was changed to non-parkinsonian tremor had no other parkinsonian features such as rigidity, bradykinesia, hypomimia, or monotonous speech. They also reported falls significantly less frequently and had higher mini-mental state scores . Those in whom the diagnosis was changed to atypical parkinsonism had more severe akinesia , rigidity , and postural instability , less commonly reported an initially or currently good response to levodopa , but more often had incontinence and additional features incompatible with Parkinson’s disease. Those in whom the diagnosis was changed to vascular parkinsonism were older than those in whom a diagnosis of Parkinson’s disease was confirmed , had a larger number of smoking years , more often had gait difficulties as their first complaint , and had more severe postural instability ; they never had a rest tremor.
Sensitivity Specificity And Predictive Value Of A Previous Diagnosis Of Parkinson’s Disease
Of 126 patients with a pre-existing clinical diagnosis of probable and possible Parkinson’s disease in the overall sample , 111 were confirmed as having Parkinson’s disease, resulting in a sensitivity of 88.1% ; similarly, it was confirmed that 54 of 74 patients did not have Parkinson’s disease, resulting in a specificity of 73.0% . The positive and negative predictive values of a previous clinical diagnosis of Parkinson’s disease were 84.7% and 78.3% . In other words, in 85% of patients with a previous diagnosis of Parkinson’s disease this diagnosis was confirmed, and 78% of patients with a diagnosis other than Parkinson’s disease did not have the disease .
When this was broken down by a specialist or other doctor diagnosis, the diagnostic validity was as follows. Neurologists and geriatricians had a sensitivity and specificity of 93.5% and 64.5% , respectively, compared with 73.5% and 79.1% for non-specialists. The positive predictive values were greater for specialists than for other doctors , but the negative predictive values were equivalent v non-specialist 79.1% ).
The Diagnostic Process: What Will Your Neurologist Ask You If They Suspect Parkinson’s
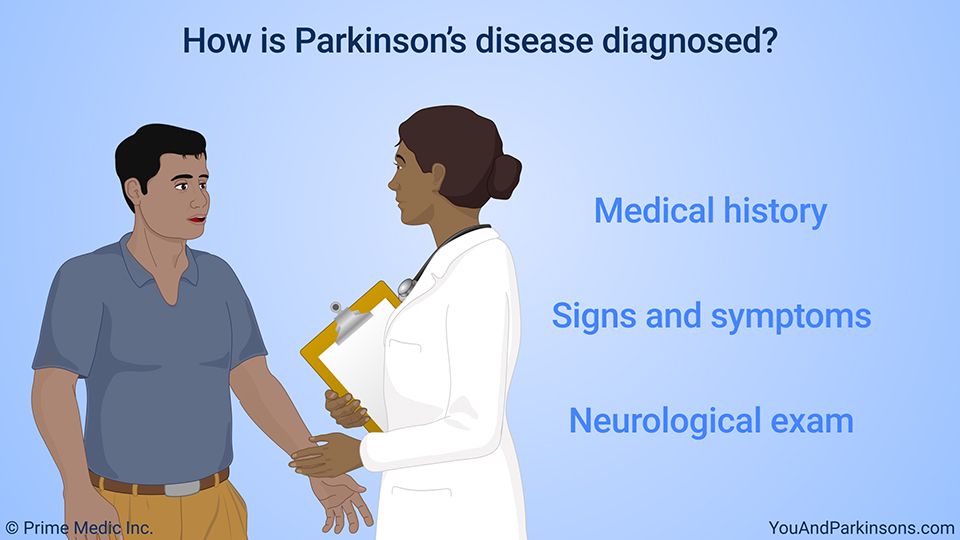
The early symptoms of Parkinson’s disease can be caused by other conditions as well, so your neurologist will seek to rule these in or out. The following differential diagnoses will be considered :
- Bradykinesia: Drug-induced Parkisinson ism, vascular Parkinsonism — Parkinsonism referring to the motor symptoms seen in Parkinson’s disease.
- Tremor: Essential tremor, intention tremor , tremors are the result of side effects of medications you are taking or as the result of alcohol abuse.
If your neurologist uses the Unified Parkinson’s Disease Rating Scale , the most common rating scale, your neurological examination will consists of four distinct parts where your neurologist suspects Parkinson’s disease :
Questions that you and/or a caregiver can answer orally include those relating to your current symptoms:
Patients In Whom A Diagnosis Of Parkinson’s Disease Was Or Was Not Previously Made
Patients in whom a diagnosis of Parkinson’s disease was previously made had a longer disease duration and greater disease severity , with more severe akinesia , postural instability, and rigidity than those in whom the diagnosis was not made before. They were also more likely to be depressed , to have experienced dyskinesias , and to live alone or with their family than in a nursing home .
A Decade Of Unnecessary Parkinsons Drugs Is Likely To Have Remodelled My Brain
A key issue is that I no longer have a convenient label for my symptoms. I had pre-existing joint and gastro issues that have worsened immeasurably during the past decade. My ability to concentrate, to function, to move, to ‘be’ all worsened beyond comprehension. I have been told that nearly a decade of unnecessary Parkinson’s drugs is likely to have remodelled my brain, through its innate neuroplasticity, so that it now considers the symptomatic side effects of those drugs ‘normal’ for me. Just as hitting a tennis ball every day for 10 years will build up your ball-hitting skills, so the brain can be driven by drugs and their side effects into behaviours that it then reconfigures and learns as normal.
‘Writhing and contorting’
Actually weaning myself off Stalevo – a Parkinson’s medication used to increase dopamine levels in the brain – which I was taking eight times a day, was pretty terrifying. I was initially advised to drop one daily dose per week. By the second week I was writhing and contorting involuntarily – not something I had ever done before. I was then asked to drop one daily dose per month. I took my last Stalevo dose on 25 October 2015.
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
In A Sense The Certainty Of Diagnosis Was Good I Belonged Somewhere

Post-misdiagnosis
I still have no confirmed diagnosis. The swathe of neurological symptoms still persist today – some aspects of movement are identified as functional movement disorder, but otherwise it has been a question of ruling in/out alternative causes for some symptoms.
One theory is that an initial brain insult during the 2006 anaesthetic, together with a gastro drug I was taking at the time that has Parkinsonism as a side effect, combined to give me Parkinson’s disease. But now this original brain insult plus nine years of my brain’s neuroplasticity being driven into new behaviours by Parkinson’s drugs, plus issues that arose during Parkinson’s drug withdrawal are the current neurological problems that I have to contend with.
Fortunately, while there is widespread dysfunction, I have been told that there does not appear to be any brain disease processes associated with these symptoms. Again, there are no tests to prove/disprove this and one remains reliant on the expertise of brilliant neuroscientists.
Patients With A Previous Diagnosis Other Than Parkinson’s Disease
Among all patients seen, two were referred for diagnostic purposes without a previous diagnosis, and 69 of 202 patients had a previous diagnosis other than Parkinson’s disease . Among these, 56 patients had been given a diagnosis of non-parkinsonian tremor, two of vascular parkinsonism, one of atypical parkinsonism, and 10 had been prescribed an antiparkinsonian drug for parkinsonian features without a specific diagnosis . Thirteen of the 69 patients with different diagnoses and the two patients referred for diagnostic purposes fulfilled strict clinical criteria for Parkinson’s disease . In two additional patients who had a previous diagnosis of non-parkinsonian tremor, a diagnosis of “possible Parkinson’s disease” was made . If only patients who had at some point in the past seen a specialist were considered, the diagnosis was changed to probable Parkinson’s disease in five and to possible Parkinson’s disease in one .
Sensitivity, specificity, and predictive values for the overall sample* and by type of clinician
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Patients With A Previous Diagnosis Of Parkinson’s Disease
The diagnosis of probable Parkinson’s disease was confirmed in 109 of the 131 patients with this diagnosis , including three in whom atypical features were found but were insufficient to invalidate the diagnosis of Parkinson’s disease . Two additional patients were found to have possible Parkinson’s disease. However, in 20 of the 131 patients the diagnosis of Parkinson’s disease was unequivocally rejected . The alternative diagnoses were non-parkinsonian tremor in four patients , vascular parkinsonism in six , progressive supranuclear palsy in four , and multiple system atrophy in three . Two patients received a diagnosis of idiopathic torsion dystonia, and one of dementia without parkinsonism. When only those patients who had seen a specialist at some point in the past were considered, the diagnosis was changed from Parkinson’s disease to a different diagnosis in 11%.
Patients with an initial diagnosis of Parkinson’s disease
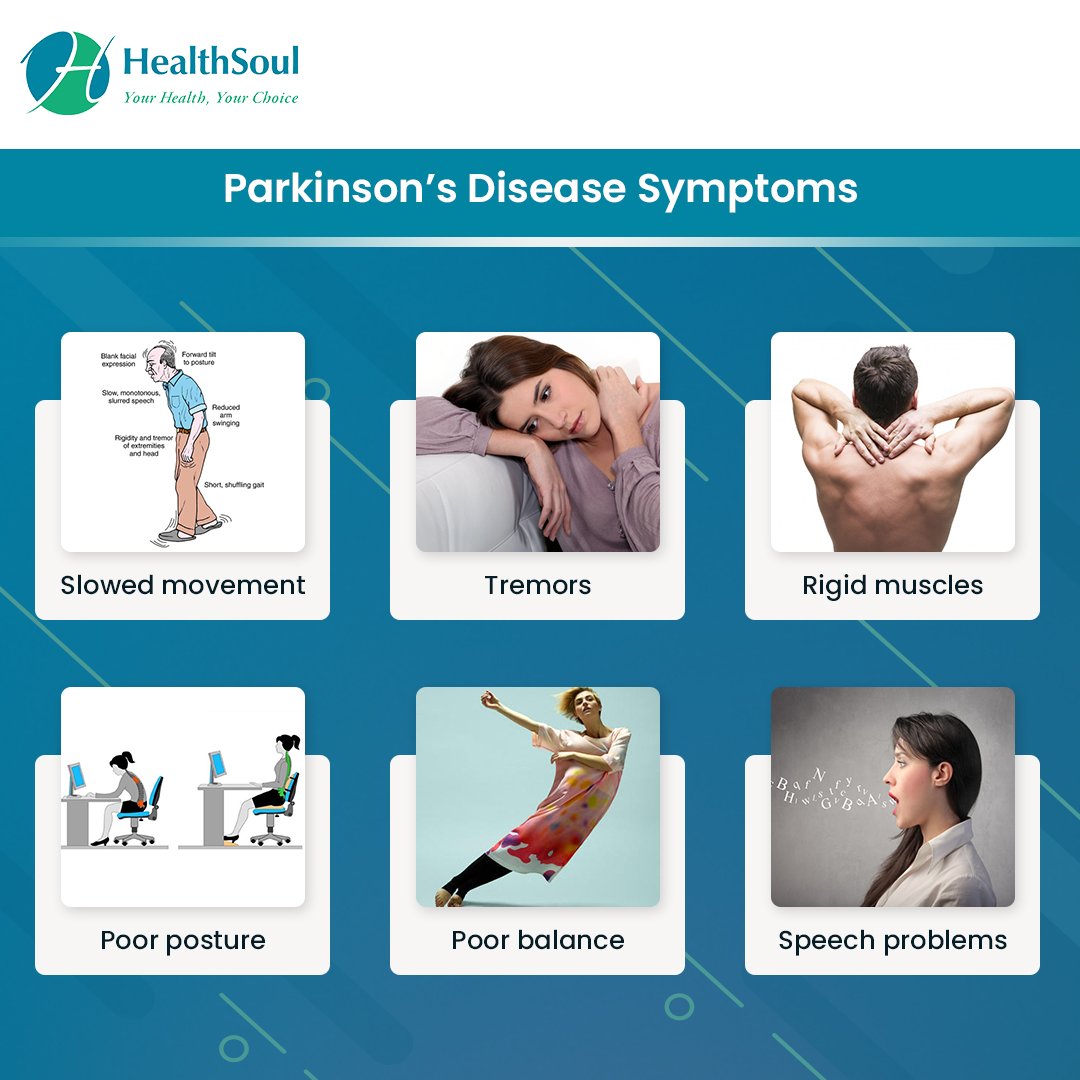
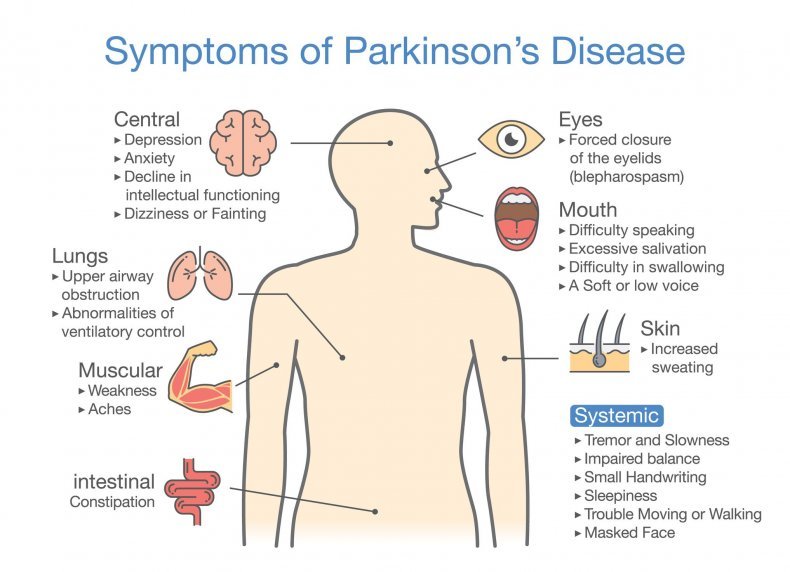
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Read more about Parkinson’s tremors
Rigidity
Bradykinesia
mask-like expression of the face
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
Parkinson’s Patients Do Best If Treated By Neurologist
Study Shows Parkinson’s Patients Cared for by Neurologists Are Less Likely to Be Put in Nursing Homes
Aug. 10, 2011 — People with Parkinson’s disease may live longer if treated by a neurologist, a new study suggests.
The study also found that Parkinson’s patients who see a neurologist are less likely to be placed in a nursing home and less likely to break a hip.
The study is published in Neurology.
“This is a very interesting and unique investigation,” Washington University researcher Allison Wright Willis, MD, tells WebMD. “There are ways that we can help improve the lives of people with Parkinson’s disease beyond discovering a cure and beyond discovering the cause.”
Researchers analyzed the records of nearly 138,000 newly diagnosed Parkinson’s disease patients receiving Medicare seen in outpatient clinics during 2002. Between 2002 and 2005, 58% of them were treated by neurologists.
The fact that more than half of Parkinson’s patients are already seeing a neurologist for treatment is reassuring to James C. Beck, PhD, director of research programs at the Parkinson’s Disease Foundation.
“But that still leaves a large number, over 40%, who are not seeing a neurologist for their care,” Beck tells WebMD. Beck was not involved in the study.
The study revealed that women are 22% less likely than men to see a neurologist, and minorities are 17% less likely than whites to see a neurologist.
What To Look For In A Parkinsons Disease Neurologist
Here is a checklist of basic questions for your prospective neurologist:
- How long have you worked in the field? How many Parkinson’s patients do you see a year?
- Do you have special training in movement disorders? Are you board-certified in neurology?
- Who do I see when you are not available?
- What hospital do you use for treating patients?
It’s important to understand that the online rating systems for doctors are not very accurate. Or they are, in some ways, and it is not the information you are looking for. For example, many of these ratings rank a doctor high if he is always on time and never backed up. If you think about the clinic setting and the inability to really control what happens in a typical day, and the doctor who is always time may be the doctor who never has that extra minute to give you when you need it. These ratings also often include how easy it is to get an appointment.
Of course, the doctor who is exceptional that everyone wants to see ranks poor on this measure, and the doctor who doesn’t have a strong following ranks high. If you do look at these rankings, make sure to read the comments, and realize that one bad comment could simply represent one patient having a bad day after being given a diagnosis he didn’t want.
What Parkinsons Diagnosis Criteria Do Doctors Use
Other Challenges Of Diagnosing Parkinsons Disease
Related: Here’s what’s important to remember if you were just diagnosed with Parkinson’s disease.
Methodological Limitations Of The Diagnostic Studies
When interpreting the literature about PD diagnosis, the following methodological issues should be considered:
- lack of long-term prospective clinical and pathological as a reference standard
- lack of operational definitions such as defining specialists or clinical diagnostic criteria
- unclear whether investigators were blinded to initial diagnosis
- sample sizes necessarily limited by the number of cases available with neuropathological outcomes
- PD trial age groups are often young as studies were performed by neurologists who see a younger population of people with PD
- most studies included people with established disease lasting some years
- varying geographical locations
- some studies are in specialised units and may not reflect the diagnostic accuracy of other units in the UK
- exclusion of some studies using magnetic resonance volumetry and magnetic resonance spectroscopy as they lacked appropriate population, intervention and outcome criteria
- lack of statistical details of diagnostic accuracy such as sensitivity, specificity and positive predictive values
- lack of economic evaluations of SPECT.
Can Parkinsons Disease Be Diagnosed By How You Smell
There’s evidence that people with Parkinson’s disease may emit a specific type of scent, which is related to increased sebum production. However, doctors have not developed a way to use this odor to diagnose the disease. More research is being done to see how the finding can help with diagnosis and treatment.
Likelihood Of Referral According To Final Diagnosis
Overall, 74% of all cases with a diagnosis of Parkinson’s disease had been seen by a specialist. However, when these cases were classified by final diagnosis , it was observed that, paradoxically, fewer cases with atypical disease had been seen by a specialist compared with those with classical Parkinson’s disease ; p = 0.02).
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Cerebellum The Coordinating Center In The Brain

movements and speech are also evaluated. The examiner may ask you to say “mama” or “papa” to test your lips. The examiner may ask you to say “Lulu” to test your tongue. The examiner may ask to say, “Ahh.” This tests your pharynx. The sensory examination includes an evaluation of your ability to perceive a light touch, a pin prick, and your ability to tell whether your thumb or great toe is being moved up or down. Testing for PD requires skill and practice on the part of the examiner.
-
What tests will my nueologist do for parkinsons?
1 month ago
What to expect when meeting a neurologist for parkinsons disease?
1 year ago
How does a neuroligist check for parkinsons?
1 year ago
What do neurologists do for those who have parkinson’s?
1 year ago
What does neurology brings to parkinson’s disease?
2 years ago
How can neurologist help with parkinsons disesae?
2 years ago
How can a neurologists help a pateint with parkinsons disease?
2 years ago
How can neurologists help with parkinsons disease?
2 years ago
Why are people with parkinsons reffered to a neuologist?
2 years ago
How long neurologist check a patient with Parkinson?
2 years ago
How does a nuerologist determine parkinsons?
2 years ago
Do you a nuerologist if you have parkinsons disease?
2 years ago
What to expect when going to a nuerologist to talk about parkinsons?
2 years ago
What does a neurologist do when diagnosing parkinsons?
2 years ago
How long should i wait to see a neurologist for parkinsons?
2 years ago
If Its Not Parkinsons Disease What Could It Be
Here are some possibilities:
Side effects of medication: Certain drugs used for mental illnesses like psychosis or major depression can bring on symptoms like the ones caused by Parkinson’s disease. Anti-nausea drugs can, too, but they typically happen on both sides of your body at the same time. They usually go away a few weeks after you stop taking the medication.
Essential tremor: This is a common movement disorder that causes shaking, most often in your hands or arms. It’s more noticeable when you’re using them, like when you eat or write. Tremors caused by Parkinson’s disease usually happen when you’re not moving.
Progressive supranuclear palsy: People with this rare disease can have problems with balance, which may cause them to fall a lot. They don’t tend to have tremors, but they do have blurry vision and issues with eye movement. These symptoms usually get worse faster than with Parkinson’s disease.
Normal pressure hydrocephalus : This happens when a certain kind of fluid builds up in your brain and causes pressure. People with NPH usually have trouble walking, a loss of bladder control, and dementia.
How Is Parkinsons Disease Tested And Diagnosed
At Banner Health, our neurologists have years of experience in testing and diagnosing Parkinson’s disease. Our team of compassionate experts knows that each patient is different, so we work with you to quickly find the right diagnosis to begin building your treatment plan.
Parkinson’s is not simple to diagnose. No test exists to diagnose Parkinson’s disease. Doctors test and diagnose Parkinson’s based on your medical history, symptoms and neurological and physical exams.
Many times a primary care provider is the first to suspect a Parkinson’s diagnosis. If you’re experiencing symptoms such as tremors, shaking, slow movement, stiffness and/or trouble with balance, talk to your doctor or seek the opinion of a neurologist. Banner Health neurologists are movement disorder specialists, who have experience and specific training to assess and treat Parkinson’s.
Learn More About Parkinsons Disease: Overview
Tests For The Diagnosis Of Parkinsons Disease
There’s no specific single test that allows a direct diagnosis of Parkinson’s disease. This means that it can’t be detected by a blood, urine, or cerebrospinal fluid test, as well as an imaging test.
We hope that, in the future, researchers will be able to detect a biomarker that will facilitate direct diagnosis. However, for the time being, we have to use what’s available.
On the other hand, the MSD Manual points out that when Parkinson’s disease isn’t certain, the doctor may prescribe a drug called levodopa. If the person shows a clear improvement after taking it, then the diagnosis is that they have Parkinson’s.
How Does Alcohol Affect Parkinsons Medication
What Is The Prognosis For Parkinsons Disease
What Is The Prognosis For Parkinsons Disease
The rate at which Parkinson’s progresses varies from patient to patient. Some patients experience its changes over 20 years or more. While others find the disease advances quicker.
Parkinson’s is not a fatal disease. However, secondary complications from symptoms may increase falls, blood clots or pneumonia, which can be life-threatening. These are more common in later stages of Parkinson’s.
In general, the average life expectancy of Parkinson’s patients is similar to people without the disease.
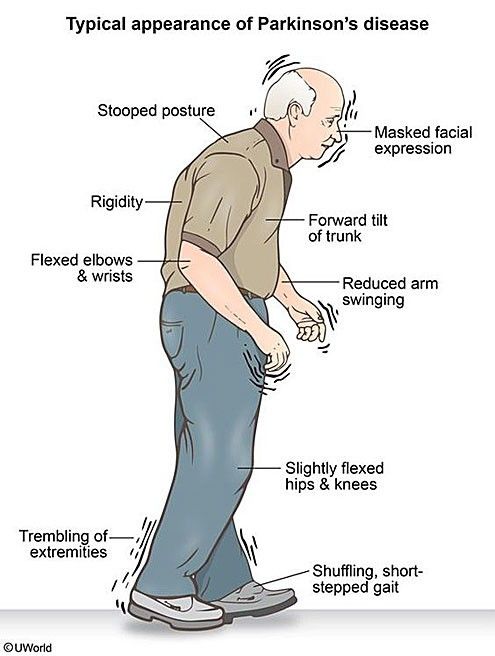
What Are The Symptoms Of Parkinson’s Disease
The main symptoms of Parkinson’s disease are:
- tremor or shaking, often when resting or tired. It usually begins in one arm or hand
- muscle rigidity or stiffness, which can limit movement and may be painful
- slowing of movement, which may lead to periods of freezing and small shuffling steps
- stooped posture and balance problems
The symptoms of Parkinson’s disease vary from person to person as well as over time. Some people also experience:
- loss of unconscious movements, such as blinking and smiling
- difficulties with handwriting
- drop in blood pressure leading to dizziness
- difficulty swallowing
- sweating
Many of the symptoms of Parkinson’s disease could be caused by other conditions. For example, stooped posture could be caused by osteoporosis. But if you are worried by your symptoms, it is a good idea to see your doctor.
Parkinsons Symptoms That Lead To Diagnosis
The biggest clues your doctor will look for involve observing you as you sit and speak during an exam for PD, as well as how you perform movement tasks that your doctor may ask you to do. This will help your doctor determine if you have the hallmark symptoms of PD:
-
Balance and posture problems
-
Stiffness, or rigidity
-
Tremor, or uncontrolled shaking
For example, your doctor will likely look for any signs of tremor as you sit with your hands relaxed in your lap. Such hand tremors normally occur in only one hand, as PD tends to impact one side of your body more than the other. In addition, your doctor will take note of your facial expressions. PD symptoms can affect your facial muscles, and people with PD often smile and blink less often than people who do not have the disease. Other signs that can be picked up during an exam include:
How Does Alcohol Affect Parkinsons Symptoms
In general, alcohol can be harmful to people with chronic conditions. According to the Centers for Disease Control and Prevention , overconsuming alcohol can be a long-term risk factor for a weakened immune system, learning and memory problems, high blood pressure, digestive issues, and various types of cancer. When looking specifically at Parkinson’s symptoms, however, reports differ on how alcohol and PD may be linked.
Surgery For People With Parkinsons Disease
Support For People With Parkinsons Disease
Parkinsons Disease And Alcohol: Your Guide
If you have Parkinson’s disease , you may be wondering whether alcohol consumption affects the development or progression of your condition. Some people may wonder if they should avoid drinking completely. As one MyParkinsonsTeam member asked, “How does alcohol affect Parkinson’s — how much can I drink? Or should I avoid drinking altogether?”
Some studies haven’t found that small amounts of alcohol are associated with a higher PD risk, while others highlight the dangers alcohol can pose for anyone with a chronic condition. In addition, there may be adverse interactions between alcohol and common Parkinson’s medications. Because of conflicting information, people with PD may feel confused about whether or not to drink.
“I’ve been told by more than one doctor that I should not have any alcohol,” one MyParkinsonsTeam member wrote. “And at this point, I don’t remember which doctor or specifically why.”
So, how do you decide what approach to take?
If you have Parkinson’s disease and are trying to decide whether or not to reduce your drinking — or quit alcohol completely — here are some things to consider.
Obtaining A Parkinson’s Disease Diagnosis
New Diagnostic Standards For Parkinsons
Be Honest With Yourself And Your Doctor
“I am not even a big drinker, but miss the odd one,” wrote a MyParkinsonsTeam member. “So, I had an alcohol-free beer, which tasted OK, to be honest.”
