What Is The Trend Over Time In The Prevalence And Incidence Of Parkinsonism In Canada
Between 2004?2005 and 2013?2014, the number of Canadians living with diagnosed parkinsonism increased from approximately 61,000 to 84,000, while the number of Canadians newly diagnosed increased from approximately 8,000 to 10,000. However, during the same period, there was no significant change in the age-standardized prevalence proportion, which remained at 0.4%, or the incidence rate, which went from 51.6 per 100,000 to 52.6 per 100,000. The sex differential also remained constant over time for both indicators .
Figure 3: Age-standardized prevalence and incidence of diagnosed parkinsonism, including Parkinson’s disease, among Canadians aged 40 years and older, by sex, 2004?2005 to 2013?2014
| Indicator | |
|---|---|
| 67.8 | 40.3 |
Notes: Age-standardized estimates to the 2011 Canadian population. The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. The 95% confidence intervals of the prevalence estimates are too small to be illustrated.Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
How Many Canadians Live With Parkinsonism And How Many Are Newly Diagnosed Each Year
Based on the latest estimates available , in 2013?2014, approximately 84,000 Canadians aged 40 years and older were living with diagnosed parkinsonism and 10,000 Canadians were newly diagnosed with this condition . The age-standardized prevalence was 1.5Footnote i times higher among males than among females , and similarly the age-standardized incidence was 1.7Footnote i times higher among males than females . The epidemiological burden of parkinsonism increases with age. In 2013?2014, when comparing estimates among Canadians aged 85 years and older vs. those aged 40-44 years, the prevalence of the condition was 169Footnote i times higher in the older age group , while the incidence was 48Footnote i times higher in the older age group .
Figure 1: Prevalence of diagnosed parkinsonism, including Parkinson’s disease, by sex and age group, Canada, 2013?2014
| Age group |
|---|
| 44.7 | 55.1 |
Note: The 95% confidence interval shows an estimated range of values which is likely to include the true value 19 times out of 20. Data source: Public Health Agency of Canada, using Canadian Chronic Disease Surveillance System data files contributed by provinces and territories, July 2017.
Variations In Incidence And Prevalence Of Parkinsons Disease In Taiwan: A Population Yu Sun
1Department of Public Health, College of Medicine, National Cheng Kung University, Tainan 70101, Taiwan
2Department of Public Health, College of Public Health, China Medical University, Taichung 40402, Taiwan
3Department of Health Care Management, National Taipei University of Nursing and Health Sciences, Taipei 11219, Taiwan
4Department of Neurology, En Chu Kong Hospital, Sanxia District, New Taipei City 23702, Taiwan
Abstract
1. Introduction
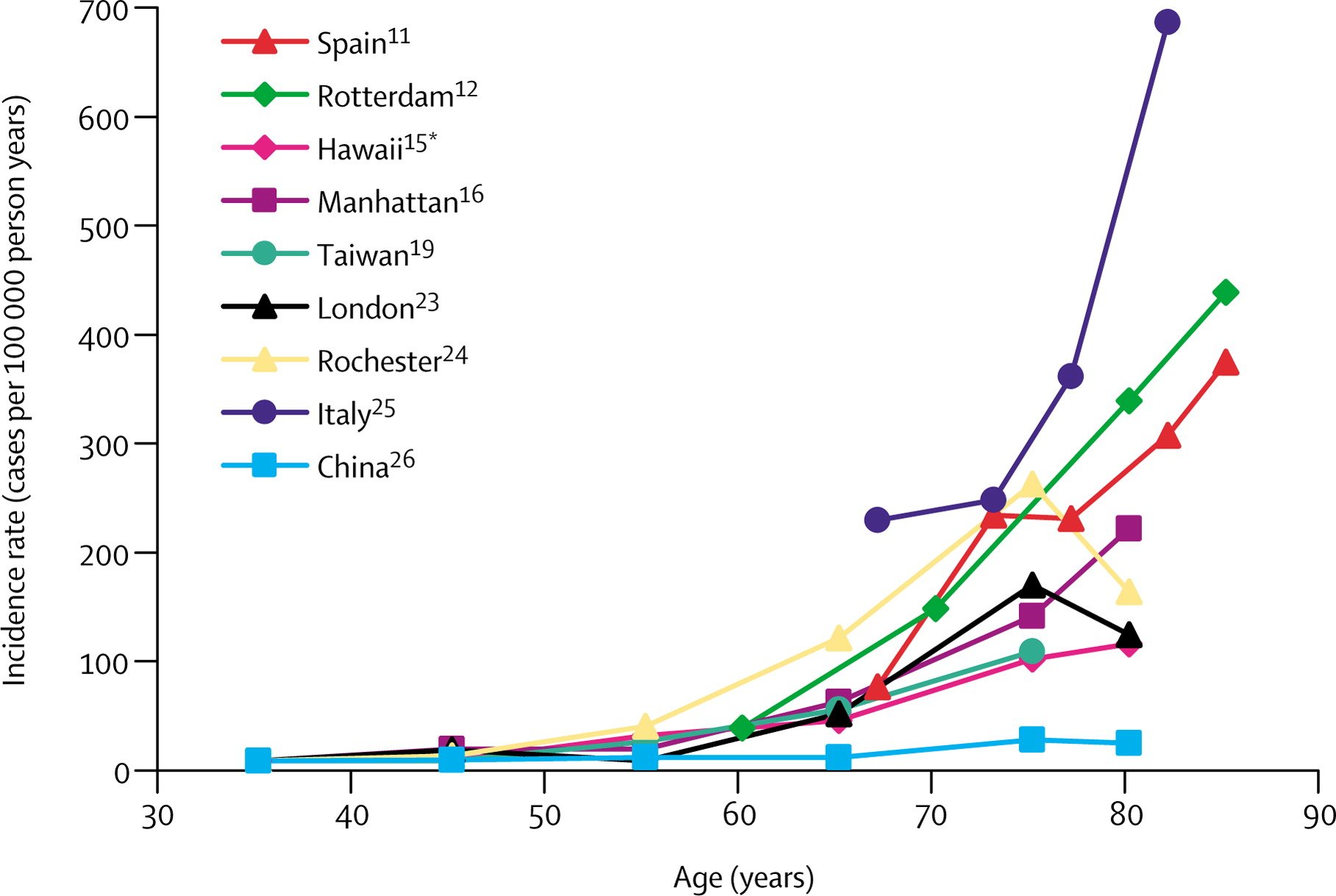
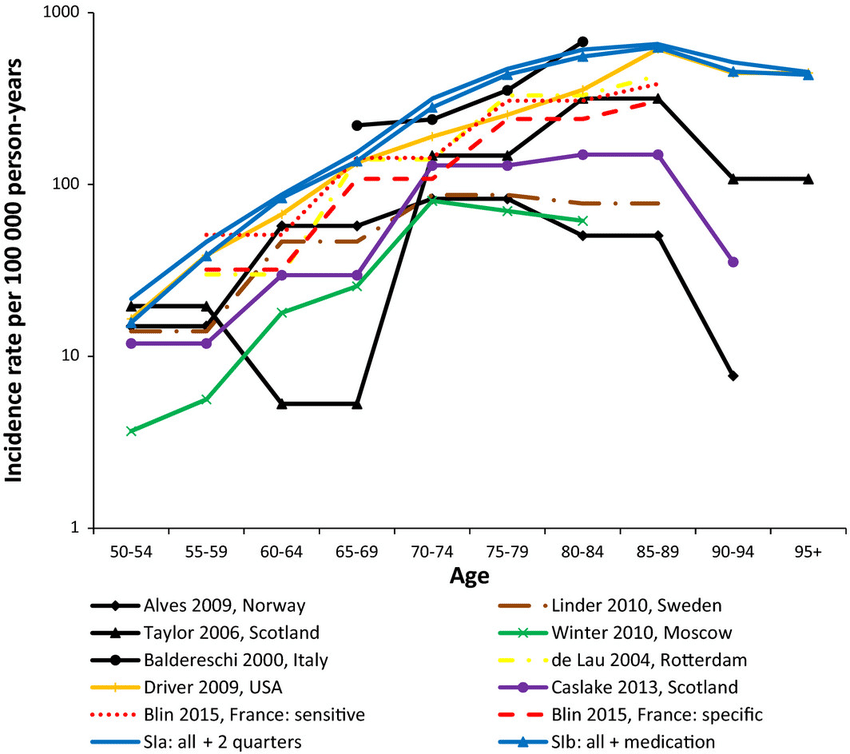
Genetic variants are considered to be the most likely etiological factor for PD incidence in patients <40 years , and certain occupational and environmental factors add additional risk to the incidence of PD . Sufficient evidence shows that age is the strongest risk factor for PD , where the PD incidence starts to increase sharply after 60 years of age . Despite this trend, several studies found that the incidence of PD increases up to a peak in 70–79 years and then declines in very old patients . Such phenomenon may be attributed to the difficulty in distinguishing between normal and PD patients in the most advanced ages whose neurodegeneration may be regarded as “normal” aging-related signs .
2. Research Design and Methods
2.1. Data Source
2.2. Study Subjects
2.3. Demographics, SES, and Urbanization Level
2.4. Validation
2.5. Statistical Analysis
| Variables | Prevalence rate ‡ |
| Calendar year | |
| 299.3 | 87.3 |
| Variables |
4. Discussion
4.1. Main Findings
4.2. Trends of the Incidence and Prevalence of PD
Disclosure
Acknowledgment
What Are The Management Options For Canadians Living With Parkinsonism
There is currently no cure for Parkinson’s disease and most other parkinsonism cases. However, treatment options are available to help mitigate the symptoms and health impacts associated with these conditions. Most often the primary treatment is pharmacological, but it may also include other therapeutic options and, in the case of Parkinson’s disease, surgical interventions. Studies have shown that specially tailored exercise programs, supervised by physiotherapists or other trained professionals, may help affected individuals maintain or improve their physical functionality and general well-being.Footnote 2 Footnote 3 Footnote 4 Footnote 5
Box 1: What’s in the data?
The data used in this publication are from the Canadian Chronic Disease Surveillance System , a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries.
Definition of diagnosed parkinsonism, including Parkinson’s disease, in the CCDSS
Parkinsons Disease Prevalence Age Distribution And Staging In Colombia
https://doi.org/10.4081/ni.2020.8401
- Jorge Luis OrozcoDepartamento de Neurología, Fundación Valle del Lili, Cali; Centro de Investigaciones Clínicas, Fundación Valle del Lili, Cali, Colombia.
- Jaime Andrés Valderrama-ChaparroDepartamento de Neurología, Fundación Valle del Lili, Cali; Centro de Investigaciones Clínicas, Fundación Valle del Lili, Cali, Colombia.
- Gabriel David Pinilla-MonsalveDepartamento de Neurología, Fundación Valle del Lili, Cali; Facultad de Ciencias de la Salud, Universidad Icesi, Cali, Colombia.
- María Isabel Molina-EcheverryFacultad de Ciencias de la Salud, Universidad Icesi, Cali, Colombia.
- Ana Melissa Pérez CastañoPROESA, Universidad Icesi, Cali, Colombia.
- Yoseth Ariza-AraújoFacultad de Ciencias de la Salud, Universidad Icesi, Cali, Colombia.
- Sergio I. PradaCentro de Investigaciones Clínicas, Fundación Valle del Lili, Cali, Colombia.
- Yuri Takeuchi | ytakeuchi@icesi.edu.coDepartamento de Neurología, Fundación Valle del Lili, Cali; Facultad de Ciencias de la Salud, Universidad Icesi, Cali, Colombia.
Highlights From The Canadian Chronic Disease Surveillance System
Parkinsonism, including Parkinson’s disease, can have significant impacts for those affected, their caregivers, and society. With a growing and aging population, it is estimated that the number of Canadians living with parkinsonism will double between 2011 and 2031 and that the incidence will increase by 50%.Footnote 1
The Public Health Agency of Canada , in collaboration with all Canadian provinces and territories, conducts national surveillance of parkinsonism to support the planning and evaluation of related policies, programs, and services. This fact sheet presents an overview of the data on diagnosed parkinsonism, including Parkinson’s disease, from the Canadian Chronic Disease Surveillance System .
Projected Estimates Of Parkinsons Disease With Aging Population
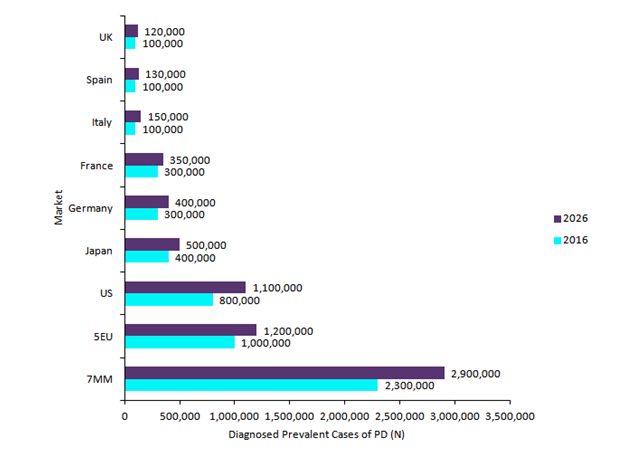
As the life expectancy has increased worldwide, it is expected that the burden of chronic diseases, like PD, will continue to grow. It is estimated that the number of people with PD in 2005 totaled between 4.1 million and 4.6 million and that number will more than double by 2030 to between 8.7 million and 9.3 million.7
Estimation Of The 2020 Global Population Of Parkinsons Disease
N. Maserejian, L. Vinikoor-Imler, A. Dilley
Category:Epidemiology
Objective: To estimate the number of individuals living with PD globally in 2020.
Background: Although previous studies have estimated PD prevalence in many countries, the number of individuals with PD globally in 2020 has not been estimated.
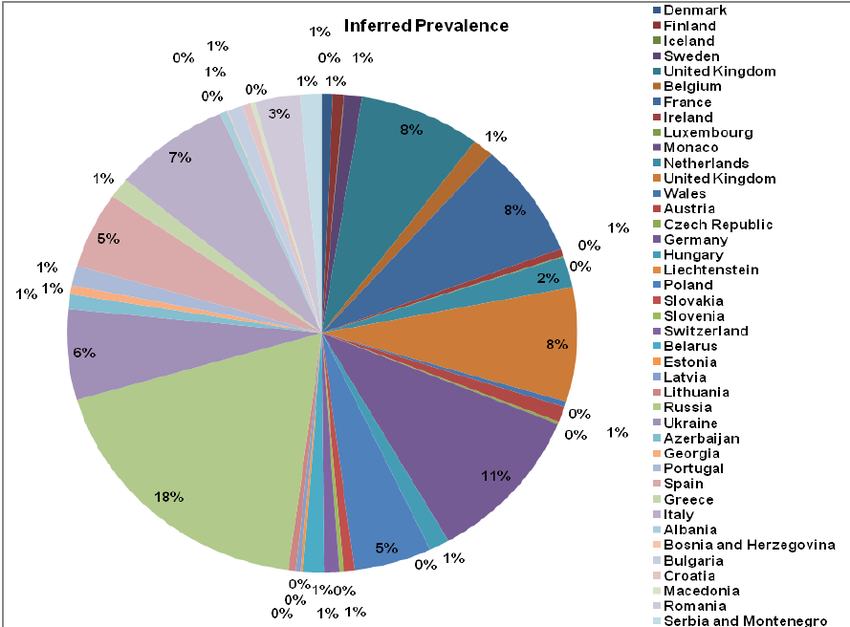
Method: We comprehensively reviewed the literature for recent and reliable prevalence estimates of PD globally. The Global Burden of Disease Study was the only source available that provided an overall global estimate, with 2017 the most recent year available from the published manuscript or online tools . We verified the estimates of the PD prevalence of several countries that comprised the GBD summary estimate, by reviewing the individual publications and comparing them to the GBD estimates. GBD estimates tended to be in the lower range but close to estimates from the individual papers. For all but two countries , we applied the GBD prevalence proportions in 2017. For the US and Canada, we applied more recent prevalence proportions by Marras et al. 2018 . We assessed the worldwide PD population in 2020 by multiplying the most reliable prevalence proportions by the corresponding 2020 population, using CDC data for US, Statistics Canada for Canada, Eurostat for European countries and UN population estimates for the rest of the world.
To cite this abstract in AMA style:
Mov Disord.
Association Between Autonomic Dysfunction And Disease Severity
The presence of autonomic dysfunction was associated with less advanced disease, less disability and greater quality of life. Although the reasons for this are far from clear, it appears that, in our cohort autonomic dysfunction is more common in early stage disease. Indeed, it is remarkable that in untreated patients, over two-thirds at Hoehn and Yahr stage IV or V had no autonomic dysfunction. It has previously been suggested that prominent autonomic features early in the course of the disease are a worrying or atypical feature, favouring multiple system atrophy as the underlying diagnosis . There is evidence that autonomic involvement can occur in the early stages of PD; in one study, 38% of patients with abnormal autonomic function tests were in the first 5 years of their disease .
Previous research has suggested no significant association between autonomic dysfunction and mortality in people with PD . In our largely untreated population, the lack of dysfunction in late stage disease may partly explain this observation.
Characteristics Of The Administrative Data Used For The Study
We conducted an observational study to determine PD prevalence based on administrative de-identified data from two Colombian HMOs using claims from 2015. Access was obtained in the settings of a research agreement with Icesi University . According to national records from 2015, 97.6% of the Colombian population is insured by the National Healthcare System.13 The two HMOs that provided us with claims data have 4,312,928 beneficiaries distributed across different regions of the country, mainly in the southwest. These claims are filled only by physicians certified by the government and other regulatory entities. The information is compiled by the institutions providing health services , and is prepared annually and submitted to the national government for regulatory purposes.
The analyzed data include individual records of all services provided to each affiliate: medical consultation, pharmacy, laboratory, medical props , and surgical procedures. These records are encoded through a complete, expandable and standardized system called CUPS . CUPS are defined by a decision-making group composed by medical scientific societies of the country and are used universally by all HMOs. Since each patient may use the HMO more than once per year or receive more than one service per visit, claims were grouped using a randomly assigned ID number to obtain the total patients per year and period.
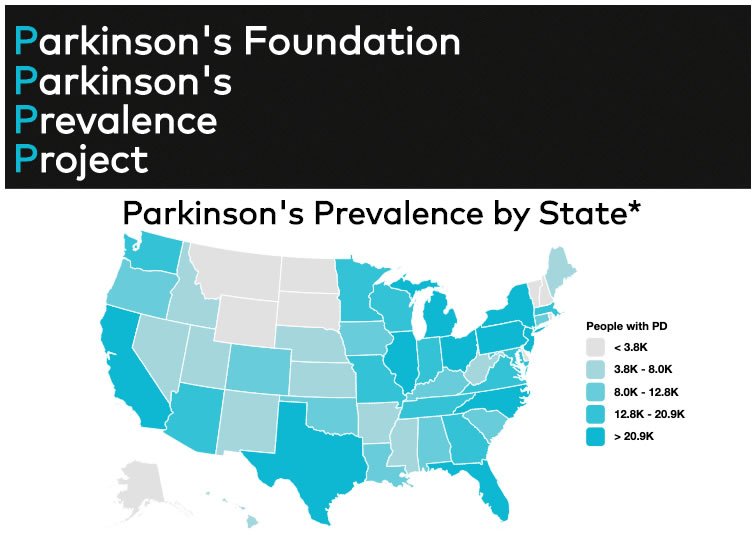
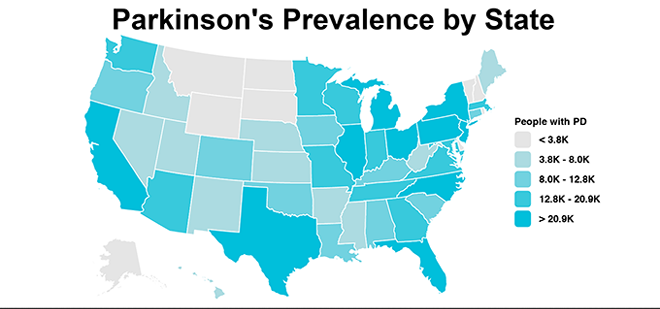
The Importance Of Establishing Parkinsons Prevalence Numbers
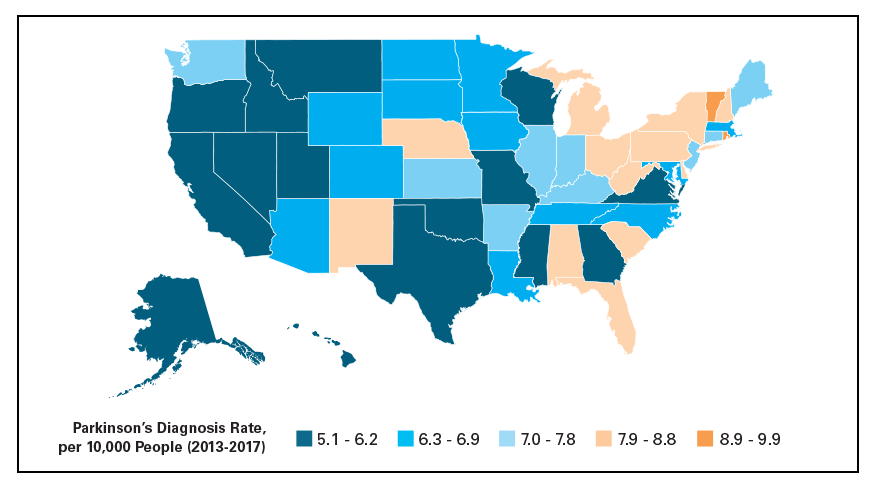
Parkinson’s Prevalence estimates will help the Parkinson’s Foundation attract the attention of federal and state government as well as the pharmaceutical industry to the growing need and urgency in addressing PD. This is an important first step to better understanding who develops PD and why.
The next phase of this study will be to determine the rate of PD diagnosis or incidence, how that has changed over time and what is the rate of mortality among those affected by PD. Determining the prevalence and incidence will allow the PD community to effectively advocate for additional money and resources necessary to support Parkinson’s research.
Parkinson’s Foundation Prevalence Project numbers highlight the growing importance of optimizing expert Parkinson’s care and treatment for people with Parkinson’s, which would help future caregivers and ease the strain on health and elder care systems.
Loading…
Heart Rate Response To Standing: Parasympathetic Function
To record heart rate response to standing, patients were asked to lie down quietly for at least 5 minutes. The patient had the 12 lead ECG machine attached with continuous rhythm strip recording. When the patient stood up a point was marked on the ECG trace and recording continued for a further 30 beats. R-R variability was measured as the ratio of the longest R-R interval compared to the shortest R-R interval . This ratio was then classified as being abnormal if?1.00.
Appropriateness Of The Tests Performed And Limitations
Our figures for autonomic dysfunction are likely to be an under-estimate. Only two of the four tests could be performed satisfactorily on three-quarters of the cohort. If more patients had been able to undergo testing it is likely that our estimate would have been higher. Difficulties in performing autonomic tests have been reported in other centres too, even when conducting tests in a hospital setting. Magerkurth et al documented that 20% of their patients could not satisfactorily perform the Valsalva manoeuvre with cardiovascular monitoring.
Finally, we acknowledge that the small number of patients involved in our study, limits the extent to which conclusions can be drawn regarding their significance. However, in this resource limited setting, where diagnosis is rare, recruiting large numbers of PD patients is difficult. This is reflected in the extremely limited amount of previous data regarding PD in SSA.
Prevalence And Incidence Of Parkinson’s In New Zealand
The ageing population means that more people are likely to be afflicted with age-related neurodegenerative diseases such as Parkinson’s and Alzheimer’s. Medicine has made huge strides in the last few decades in treating and preventing cardiac issues. With our resulting longer lives, concerns about our brain wearing out are beginning to replace fears of our heart stopping.
We have performed research into the numbers of people in New Zealand with Parkinson’s for the period 2006 to 2020. This study was conducted by Drs Toni Pitcher and Daniel Myall using pharmacoepidemiology methods . Citations for the scientific publications of the research are listed at the bottom of the page as well as a link to github where the analysis code can be found.
Estimated Healthcare Costs Related To Pd In The Us
The combined direct and indirect cost of Parkinson’s, including treatment, social security payments and lost income, is estimated to be nearly $52 billion per year in the United States alone.
Medications alone cost an average of $2,500 a year and therapeutic surgery can cost up to $100,000 per person.
The Impact Of Parkinsons Disease On Overall Health
Based on the Blue Cross Blue Shield Health Index, the overall health of those affected by Parkinson’s is significantly lower than the general population. In 2017, the average BCBS Health Index for someone aged 30-64 with Parkinson’s was 57, compared to 88 for the entire commercially insured population in this age range. This translates to an average of 10.7 years of healthy life lost for those with the condition compared to 3.4 years for the 30-64 population as a whole.4
Caring for someone with Parkinson’s Disease
The majority of Parkinson’s patients are cared for by informal caregivers, such as a family member. The physical, mental and emotional work this requires can be significant. The Impact of Caregiving on Mental and Physical Health found that caregivers have 26% poorer health compared to a benchmark population, as measured by the BCBS Health Index. In addition, a national survey conducted by the Blue Cross Blue Shield Association found that 1 in 4 unpaid caregivers are feeling more stress trying to balance work and family due to COVID-19.5
How Many People Does Parkinsons Disease Affect
![[PDF] Parkinson](https://www.parkinsonsinfoclub.com/wp-content/uploads/pdf-parkinsons-disease-prevalence-diagnosis-and.png)
Parkinson’s disease affects 1 in every 500 people in Canada. Over 100,000 Canadians are living with Parkinson’s today and approximately 6,600 new cases of PD are diagnosed each year in Canada . Most are diagnosed over the age of 60; however, at least 10% of the Parkinson’s population develops symptoms before the age of 50. Approximately four million people worldwide are living with the condition.
Bp Response To Hand Grip: Sympathetic Function
BP response to hand grip was measured with a hand-held sphygmomanometer. Patients were given the instruction “to squeeze the machine as tightly as possible” with their dominant hand to determine their maximum possible power, and then to hold it at one third of their maximum total power for as long as possible up to five minutes. During this period, BP was measured three times at one minute intervals and the highest result noted. The mean resting diastolic BP was subtracted from the highest diastolic BP during handgrip and the result recorded. Failure to increase diastolic BP by more than 20 mmHg during the prolonged handgrip was recorded as abnormal.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
Supine And Standing Bp: Sympathetic Function
Baseline systolic and diastolic BP was measured in a supine position after five minutes resting quietly. Three measurements were taken at one-minute intervals and the mean calculated. The patient was then asked to stand up. Three standing BP results were recorded; immediately on standing, after 30 seconds and after one minute standing up. The lowest systolic BP value of the three was recorded. A decrease in systolic BP, from the mean supine BP, of greater than 20 mmHg was recorded as an abnormal result.
What Are The Symptoms Of Parkinsons Disease
The symptoms of Parkinson’s disease develop gradually, as levels of dopamine fall. Early Parkinson’s disease symptoms usually affect one side of the body. The main symptoms of Parkinson’s disease include:
- Tremors: uncontrollable shaking, the symptom most associated with the disease, often beginning in the hands.
- Rigidity: stiffness or tensing of the muscles.
- Bradykinesia: slowness of movement, and loss of spontaneous movement.
- Postural instability: lack of balance and coordination which may lead to falling.
People with Parkinson’s disease may also experience other problems, including tiredness, depression, sleep problems, cognitive impairment and difficulties with handwriting. They can also find their speech and facial expression change and some people have difficulties eating and swallowing.
What Is The Incidence Of Parkinson Disease
Parkinson disease is recognized as one of the most common neurologic disorders, affecting approximately 1% of individuals older than 60 years. The incidence of Parkinson disease has been estimated to be 4.5-21 cases per 100,000 population per year, and estimates of prevalence range from 18 to 328 cases per 100,000 population, with most studies yielding a prevalence of approximately 120 cases per 100,000 population. The wide variation in reported global incidence and prevalence estimates may be the result of a number of factors, including the way data are collected, differences in population structures and patient survival, case ascertainment, and the methodology used to define cases.
Parkinsons Disease : Disease Understanding
American Association of Neurological Surgeons defines Parkinson’s disease as a progressive disorder that is caused by degeneration of nerve cells in the part of the brain called the substantia nigra, which controls movement. These nerve cells die or become impaired, losing the ability to produce an important chemical called dopamine. Normally, dopamine operates in a delicate balance with other neurotransmitters to help coordinate the millions of nerve and muscle cells involved in the movement. Without enough dopamine, this balance is disrupted, resulting in tremor , rigidity , slowness of movement, and impaired balance and coordination are hallmark symptoms of Parkinson’s disease. People with Parkinson’s also lose the nerve endings that produce norepinephrine, the main chemical messenger of the sympathetic nervous system, which controls many automatic functions of the body, such as heart rate and blood pressure. The loss of norepinephrine might help explain some of the non-movement features of Parkinson’s, such as fatigue, irregular blood pressure, decreased movement of food through the digestive tract, and sudden drop in blood pressure when a person stands up from a sitting or lying-down position.
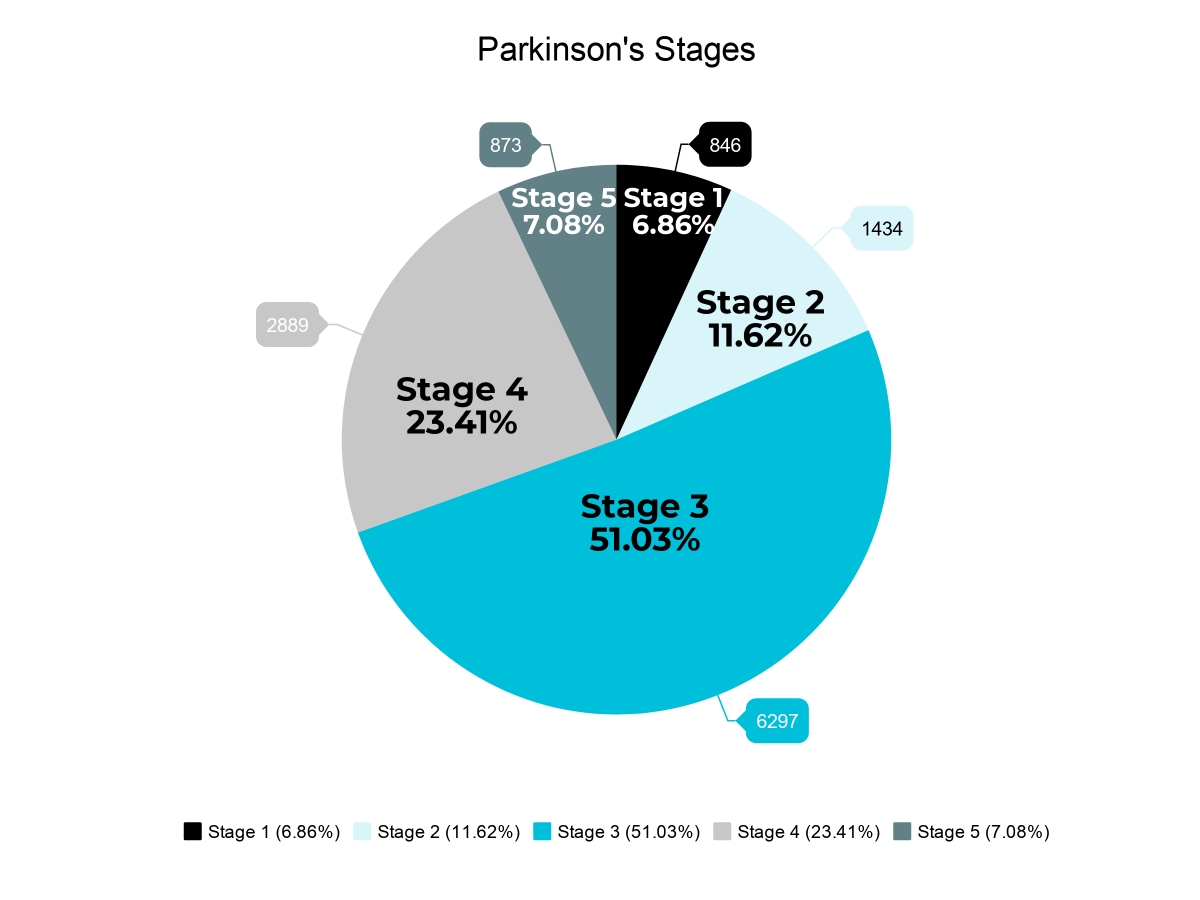
Because Parkinson’s Disease develops over time, various stages help identify how symptoms have progressed and what should be expected next. Generally, there are five stages of Parkinson’s Disease:
- Stage I
- Stage IV
- Stage V
Surgery For People With Parkinsons Disease
Deep brain stimulation surgery is an option to treat Parkinson’s disease symptoms, but it is not suitable for everyone. There are strict criteria and guidelines on who can be a candidate for surgery, and this is something that only your doctor and you can decide. Surgery may be considered early or late in the progression of Parkinson’s. When performing deep-brain stimulation surgery, the surgeon places an electrode in the part of the brain most effected by Parkinson’s disease. Electrical impulses are introduced to the brain, which has the effect of ‘normalising’ the brain’s electrical activity reducing the symptoms of Parkinson’s disease. The electrical impulse is introduced using a pacemaker-like device called a stimulator. Thalamotomy and pallidotomy are operations where the surgeon makes an incision on part of the brain. These surgeries aim to alleviate some forms of tremor or unusual movement, but they are rarely performed now.
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinson’s disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinson’s disease management. But generalist teams are becoming more aware of how to help people with Parkinson’s disease.
Patient Selection And Diagnostic Criteria
We selected all PD patients registered in the RID program during the 6-year study period. The diagnostic criteria for PD established by the NHI in the RID program are similar to the UK PD society brain bank clinical diagnostic criteria, and are as follows: 1) diagnosis of Parkinsonian syndrome : mild or worse bradykinesia and at least one of the following: muscular rigidity, rest tremor, postural instability; 2) the exclusion criteria for PD: history of strokes, head injury, definite encephalitis, drug side effects, and hypoxia; 3) supportive prospective positive criteria for PD: three or more required for diagnosis of definite PD in combination with step one: unilateral onset, rest tremor present, progressive disorder, persistent asymmetry affecting the side of onset most, excellent response to levodopa, severe levodopa-induced chorea, levodopa response for 5?years or more, clinical course of 10?years or more.
The database did not contain any personal identifiers as all identifiable personal information in the database was removed to comply with the privacy rules of the health insurance portability and accountability act. Informed consent was not required for this study as all the data was obtained from medical records. This study was performed based on the ethical principles of the Declaration of Helsinki of the World Medical Association. All procedural and ethical aspects of this study were approved by the Institutional Review Board of Korea University Ansan Hospital .
What Are The Stages Of Parkinsons Disease
Parkinson’s disease is often divided into two parts: early stage and advanced stage disease.
- Early stage: when symptoms appear and start to affect everyday activities, such as washing, getting dressed and walking.
- Advanced stage: when motor complications occur from the long term use of one of the main treatments for Parkinson’s disease, levodopa.
New Parkinsons Disease Prevalence Study
Trying to estimate the number of people living with Parkinson’s disease in North America is extremely important but notoriously difficult. It is critical to know the prevalence of PD because it informs lawmakers who make decisions concerning allocation of research funds about the true impact of the disease, and it also informs public health officials who need to plan for the growing PD population. The difficulties in ascertaining this number however, lie in trying to capture every case of a highly varied disease, on a continent without a centralized medical system and without uniformity in medical care.
A newly published study on the prevalence of PD is the most comprehensive study yet to tackle this question. The study was conducted with the support of Parkinson’s Foundation and consisted of five separate studies to determine the local prevalence — one each in Minnesota, Hawaii, and Ontario, Canada, and two in California. The data from each study was then analyzed together and compared to US Medicare data. According to this strategy, the estimated prevalence of PD in people 45 and older is 572 per 100,000. Using the last available US Census Bureau data from 2010, the overall prevalence of PD across North America in 2010 was calculated to be 680,000. Population projections were then used to extrapolate the prevalence for the year 2020, calculated to be 930,000, and for the year 2030, calculated to be 1,238,000.
Who Is Affected By Parkinsons Disease
Several studies have found that the incidence of PD is much more common in men than women.2,4 One estimate found that PD affects about 50 percent more men than women.2 The reasons for the differences in men and women with PD are unclear, although some suggested explanations are the protective effect of estrogen in women, the higher rate of minor head trauma and exposure to occupational toxins in men, and genetic susceptibility genes on the sex chromosomes.4
People with a close family member with Parkinson’s have a small increased risk of developing the disease. About 15 percent to 25 percent of people with PD have a known relative with the disease.2
It is estimated that about 10 million people worldwide are living with PD. The incidence of the disease is higher in industrialized countries.3,4
The incidence of PD increases with age: while PD affects 1 percent of the population over the age of 60, this increases to 5 percent of the population over the age of 85.1
Approximately 5 percent of people with PD are diagnosed before the age of 60.1
Urban areas have a higher prevalence and incidence of PD.5
No One Definitive Cause Of Parkinsons
There are no biomarkers or objective screening tests that indicate one has Parkinson’s. That said, medical experts have shown that a constellation of factors are linked to it.
Parkinson’s causes are likely a blend of genetics and environmental or other unknown factors. “About 10 to 20 percent of Parkinson’s disease cases are linked to a genetic cause,” says Ted Dawson, M.D., Ph.D., director of the Institute for Cell Engineering at Johns Hopkins. The types are either autosomal dominant or autosomal recessive .
But that leaves the majority of Parkinson’s cases as idiopathic, which means unknown. “We think it’s probably a combination of environmental exposure — to toxins or pesticides — and your genetic makeup,” says Dawson.
Age. The biggest risk factor for developing Parkinson’s is advancing age. The average age of onset is 60.
Gender. Men are more likely to develop Parkinson’s disease than women.
Genetics. Individuals with a parent or sibling who is affected have approximately two times the chance of developing Parkinson’s. “There’s been an enormous amount of new information about genetics and new genes identified over the past 10 or 15 years that have opened up a greater understanding of the disease,” says Dawson.
Parkinson’s Disease Stage Assessment
To determine disease stage , we adapted items from clinical and functional scales and translated them into ICD-10 conditions and ATC drug codes as follows: dementia , tracheostomy , gastrostomy , jejunostomy , falls and fractures and deep brain stimulation . Due to inherent limitations of the used dataset, disease duration and motor complications were not taken into account in the staging classification.
Availability Of Data And Materials
Data is available from the Korea National Health Insurance Sharing Service Institutional Data Access / Ethics Committee for researchers who meet the criteria for access to confidential data. Researchers can apply for the National Health Insurance data sharing service upon approval by the Institutional Review Board of their institution. After a review by the Korea National Health Insurance Sharing Service Institutional Data Access / Ethics Committee, authors are required to pay a data access fee and confirm that other researchers will be able to access the data in the same manner as the authors.
Epidemiology Of Parkinsons Disease Benjamin C.L. Lai, MD, MSc Joseph K.C. Tsui, MD, FRCP, FRCPC
ABSTRACT: The etiology of the majority of cases of Parkinson’s disease remains unknown, with multifactorial theories of genoenvironmental interaction being postulated. The prevalence and incidence of PD increase exponentially with age, and are slightly higher in men than in women. A number of putative risk factors are associated with PD, age being the one most consistently agreed-upon. Exposure to pesticides is one proposed risk factor, while an inverse association between smoking and consumption of coffee and PD has been reported in other studies. The mortality rate for PD increases in older patients. The most common cause of death is pneumonia.
Exposure to pesticides is one proposed risk factor for Parkinson’s disease, while coffee consumption and smoking have been claimed as protective factors, though the mechanism remains unclear.
IntroductionParkinson’s disease is one of the most common age-related neurodegenerative disorders, second in frequency only to Alzheimer’s disease. In the United States, at least half a million people are diagnosed as having PD, and the frequency of PD is predicted to triple over the next 50 years as the average age of the population increases.
Epidemiology of Parkinson’s disease
Prevalence
AcknowledgmentsThe authors thank the Medical Research Council of Canada and the Pacific Parkinson’s Research Institute for their support.
