Do You Or Did You Suffer From A Sleep Disorder How Has Having Parksinons Impacted Your Ability To Get Quality Rest Ask Questions And Share Your Knowledge Of Pd In Our Forums

More serious sleeping disorders may also occur such as sleep apnea or REM sleep behavioral disorder. Around 40 percent of people living with Parkinson’s disease will experience sleep apnea when breathing becomes obstructed while asleep. The common symptoms of this are loud snoring, pauses in breathing, restless sleep, and feeling very tired during the day. Sleep apnea can be controlled using breathing equipment — continuous positive airway pressure — throughout the night.
REM sleep behavioral disorder is where the muscles don’t fully relax while dreaming, therefore the person is likely to act out their dreams. This can include hitting, kicking, grinding teeth, and shouting. Around half of those living with Parkinson’s experience this but in most cases it can be improved with medication.
MORE: How Parkinson’s disease affects your body.
Parkinson’s News Today is strictly a news and information website about the disease. It does not provide medical advice, diagnosis or treatment. This content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or another qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read on this website.
Directing Glance On Dopaminergic System Physiology: Can The Dopamine Be A Reliable Bridge Between Rls/wed And Pd
Dopamine is the most common catecholamine in the central nervous system that can modulate different functions, like movement, cognition, reward and motivation . DA derived from the conversion of 2,3-dihydroxyphenylalanine by the enzyme DOPA decarboxylase . Tyrosine hydroxylase is the enzyme responsible for converting the amino acid tyrosine to DOPA, monitoring the DA amount.
It is known that there are three groups of dopaminergic cells that give rise to three different axonal pathways with different functions: nigrostriatal, mesocorticolimbic, and tuberoinfundibular system. The latter is the smallest in terms of brain DA content and controls the pituitary system. Nigrostriatal DA pathway controls voluntary movement, and dysfunction in this pathway has been implicated in movement disorder like PD. Mesocorticolimbic systems DA modulate various cognitive/emotive functions, and their degeneration may lead to some psychiatric disorders. Several studies have pointed out that mesocorticolimbic system can also modulate thalamocortical arousal state . Studies from the effect of psychomotor stimulant with a molecular structure similar to DA, like amphetamine, , has demonstrated that endogenous DA is involved in promoting wakefulness .
Take into consideration his contribution to sleep-wake state in addition to other waking behaviors like movement, DA has been considered the “bridge” that underlying PD and RLS/WED .
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Having RLS in 2002 and/or 2008 was associated with a higher risk of constipation in 2012, compared with controls. Only individuals who had RLS in both 2002 and 2008 showed higher odds of having possible RBD alone, and both constipation and possible RBD in 2012, “indicating a potential association between continuous/recurrent RLS and ,” according to the researchers.
They cautioned that constipation is a relatively non-specific Parkinson’s symptom and may not indicate a direct link between RLS and Parkinson’s.
No differences were found between olfactory scores of men with or without RLS. However, the team noted that olfactory scores were only available from a subset of participants. Additionally, the timing of the smell sense analysis may also have influenced this result, since a loss of sense of smell has been reported as a relatively late symptom in the early stages of Parkinson’s compared with RBD and constipation, they said.
“We assessed the association between RLS and prodromal signs, but not between RLS and incidence. However, our focus was on identifying whether RLS is an early indicator of the underlying common disease process in ,” the authors wrote.
The findings warrant future studies for RLS and Parkinson’s incidence in the long-term, they said.
Among the study’s limitations, the authors mentioned that the link between Parkinson’s and RLS may differ by gender, since women, although they have a reduced risk for Parkinson’s, are more susceptible to RLS.
Early Multiple Sclerosis Symptoms: Restless Leg Syndrome Numbness And Weakness
Sensory problems, including restless leg syndrome , numbness and weakness, are the first sign of multiple sclerosis . Sensory problems can occur in 20 to 50 percent of individuals with multiple sclerosis with a condition known as paresthesia. The condition can be caused by prolonged sitting or standing or remaining in a certain position for a long period of time.
Restless leg syndrome is a condition that makes the legs feel tingling when they are at rest and creates an overwhelming sensation to move them. Studies have shown that individuals with MS are three times more likely to experience restless leg syndrome compared to the general population. Cervical cord damage plays a large role in the development of RLS and can occur more in those with multiple sclerosis.
Feelings and sensations of restless leg syndrome include crawling underneath the skin, tingling, burning or creeping. Symptoms may be relieved with movement of the legs, but this relief is temporary. Furthermore, it’s impossible to keep your legs moving constantly, which makes the hours during sleep the most difficult. Many individuals suffer from sleep deprivation when they have RLS.
Weakness in multiple sclerosis can be caused two different ways: It can result from spasms or fatigue or it can result from damaged nerves. The first cause of weakness can result in loss of strength or loss of control of extremities. Due to the second cause of weakness signals may become disrupted and not reach the extremities.
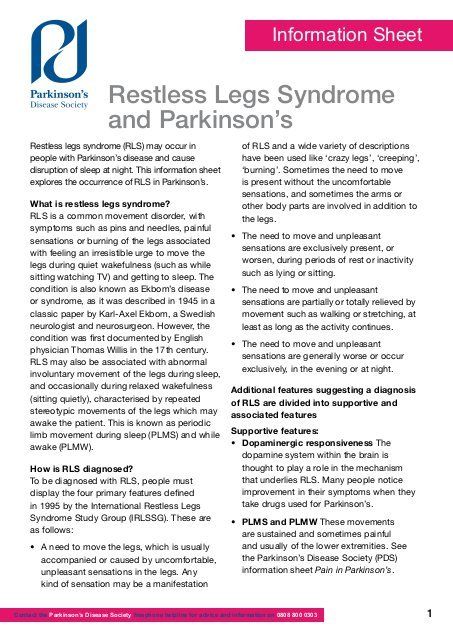
Is It Difficult To Diagnose Restless Legs Syndrome In People With Parkinson’s
Because there isn’t a specific test for restless legs syndrome, it can be difficult to diagnose the condition. Sometimes symptoms only happen briefly or from time to time.
Also, the condition can cause discomfort at night-time and this can be mistaken for arthritis in people with Parkinson’s.
Another reason why a person with Parkinson’s may experience disturbed sleep is due to dyskinesia. Dyskinesia is involuntary movements sometimes seen in people with Parkinson’s. If you’re concerned about this, speak to your GP, specialist or Parkinson’s nurse.
Your treatment will depend on how severe your symptoms are and what may be causing them.
Restless Legs Syndrome Insomnia And Brain Chemistry: A Tangled Mystery Solved
Johns Hopkins researchers believe they may have discovered an explanation for the sleepless nights associated with restless legs syndrome , a symptom that persists even when the disruptive, overwhelming nocturnal urge to move the legs is treated successfully with medication.
Neurologists have long believed RLS is related to a dysfunction in the way the brain uses the neurotransmitter dopamine, a chemical used by brain cells to communicate and produce smooth, purposeful muscle activity and movement. Disruption of these neurochemical signals, characteristic of Parkinson’s disease, frequently results in involuntary movements. Drugs that increase dopamine levels are mainstay treatments for RLS, but studies have shown they don’t significantly improve sleep. An estimated 5 percent of the U.S. population has RLS.
The small new study, headed by Richard P. Allen, Ph.D., an associate professor of neurology at the Johns Hopkins University School of Medicine, used MRI to image the brain and found glutamate — a neurotransmitter involved in arousal — in abnormally high levels in people with RLS. The more glutamate the researchers found in the brains of those with RLS, the worse their sleep.
Allen says there are already drugs on the market, such as the anticonvulsive gabapentin enacarbil, that can reduce glutamate levels in the brain, but they have not been given as a first-line treatment for RLS patients.
For more information:
Restless Legs Syndrome And Leg Motor Restlessness In Parkinsons Disease Keisuke Suzuki
1Department of Neurology, Dokkyo Medical University, 880 Kitakobayashi, Mibu, Shimotsuga, Tochigi 321-0293, Japan
2School of Nursing, Dokkyo Medical University, Tochigi, Japan
3Department of Neurology, Dokkyo Medical University Koshigaya Hospital, Saitama, Japan
Academic Editor:
Abstract
1. Introduction
2. The Diagnosis of RLS
IRLSSG Consensus Diagnostic Criteria for Restless Legs Syndrome/Willis-Ekbom Disease
Essential Diagnostic Criteria . Consider the following:An urge to move the legs is usually but not always accompanied by, or felt to be caused by, uncomfortable and unpleasant sensations in the legs.The urge to move the legs and any accompanying unpleasant sensations begin or worsen during periods of rest or inactivity such as lying down or sitting.The urge to move the legs and any accompanying unpleasant sensations are partially or totally relieved by movement, such as walking or stretching, at least as long as the activity continues.The urge to move the legs and any accompanying unpleasant sensations during rest or inactivity only occur or are worse in the evening or night than during the day.The occurrence of the above features is not solely accounted for as symptoms primary to another medical or a behavioral condition .
3. The Pathophysiology of RLS
4. Imaging in RLS
5. RLS and PD
6. RLS Mimics in PD
7. Variants of RLS in PD
8. Leg Motor Restlessness in PD
9. Treatment of RLS and LMR in PD
10. Conclusion
Conflict of Interests
References
Copyright
Restless Legs Syndrome A Condition That Is Often Difficult To Pinpoint
2021-03-22T16:53:20.896Z
Restless legs syndrome is a very common nervous disorder, affecting mostly women, and sometimes difficult to diagnose. On Europe 1, Nathalie Patte-Karsenti, neurologist in the Parkinson’s unit at the Rothschild Foundation hospital in Paris, explains how to treat it.
Restless legs syndrome is a very common nervous disorder, affecting mostly women, and sometimes difficult to diagnose.
On Europe 1, Nathalie Patte-Karsenti, neurologist in the Parkinson’s unit at the Rothschild Foundation hospital in Paris, explains how to treat it.
Legs that are tingling, itching or burning … Restless legs syndrome is a neurological pathology that is not serious, but particularly disabling.
It is often difficult for the patient to stay still, and in some cases a train or car trip, as well as watching a movie or a show, is simply unthinkable.
RLS concerns nearly 10% of the French population, and 2.5% of those affected suffer from it on a daily basis.
And this disease mainly affects women.
RLS is characterized by an overwhelming urge to move one’s legs, an urge more or less associated with unpleasant sensations, of varying intensity, from tingling, discomfort, feeling of heat, to pain.
“These symptoms appear at rest, generally in the evening, and are relieved by movement”, indicates at the microphone of
Sans Rendez-vous
, the health program of Europe 1, Nathalie Patte-Karsenti, neurologist in the Parkinson’s unit of the Rothschild Foundation hospital in Paris.
>>
What Natural Interventions May Be Beneficial For Restless Leg Syndrome
- Iron. Iron deficiency or altered brain iron metabolism have been linked to RLS; supplementation is often recommended for RLS patients who have been tested and shown to be deficient. Iron supplementation has been shown to significantly improve symptoms in iron-deficient RLS patients.
- Folate. Low levels of folate may play a role in RLS, especially in pregnant women. Pregnant women with lower folate levels were more likely to develop RLS than women who took vitamins during pregnancy.
- Magnesium. Low magnesium levels can cause excitability of neurons; magnesium supplements are often used to prevent abnormal activity in the nervous system. A case study indicated magnesium may improve symptoms and sleep problems associated with RLS.
- Diosmin. Diosmin is a natural flavone derivative often used for supporting venous function. Since venous disorders have been linked with RLS, diosmin is a promising possible treatment.
- Green coffee extract. Diabetes and pre-diabetes are known risk factors for RLS. Green coffee extract may help maintain healthy glucose levels.
- Valerian root. Valerian, an herbal sedative, is often used as a sleep aid. In a clinical trial, supplementation with valerian resulted in improvements in RLS symptoms and less daytime sleepiness.
- Other natural interventions that may help relieve RLS symptoms include D-ribose and vitaminsC and E.
Is There A Link Between Restless Leg Syndrome And Parkinson’s Disease
Previous studies have suggested that there is a link between RLS and PD due to both conditions sharing the common feature of dysfunction in the part of the brain that produces dopamine. Another commonality between these two conditions is that they have been shown to run in the family. About half of the cases are in patients that have relatives with the disorder. Another argument for the medical linkage of these neurological disorders is that they share the same treatments – no other common disorder is treated with the same dopamine agents.
Even though earlier studies have shown a significant prevalence of RLS in patients with Parkinson’s, researchers have not been able to find a common patient demographic or Parkinson’s treatment to reliably predict the development of restless leg syndrome. Also through studies, they have found that though both conditions present dysfunction in the dopamine-producing neurons in the brain, the actual mechanisms, or how the neurons are affected, are not identical.
Earlier studies involved patients with advanced cases of Parkinson’s disease that have been taking dopamine drugs for years, which may account for the significance of RLS. The use of dopamine drugs makes it much harder to correctly diagnose restless leg syndrome. The dopamine can cause restlessness that may be confused with RLS.
Parkinsons & Restless Leg Syndrome: Using Dopaminergic Medication
Because RLS is well-treated by medications that also treat PD, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in PD, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that DaTscan results are not abnormal in RLS.
Using dopaminergic medications to treat RLS however can be tricky. In some people they can lead to a phenomenon known as augmentation, in which long term use of dopaminergic medications can worsen the symptoms – making them appear earlier in the day or migrating to the upper body in addition to the legs.
How Can I Get A Good Night’s Sleep Despite Restless Legs Syndrome
Experts agree that simply changing your behavior can often help you sleep if you have restless legs syndrome. For people with mild to moderate RLS, these steps can reduce or prevent symptoms:
- Cut down on caffeine.
- Stop smoking, or at least cut back.
- Go to bed and get up at the same time each day, including weekends.
- Exercise regularly, but moderately .
- Apply heat or ice, or soak in a hot bath.
Restless Legs Syndrome: Detection And Management In Primary Care

NATIONAL HEART, LUNG, AND BLOOD INSTITUTE WORKING GROUP ON RESTLESS LEGS SYNDROME, National Institutes of Health, Bethesda, Maryland
Am Fam Physician. 2000 Jul 1;62:108-114.
Restless legs syndrome is a neurologic movement disorder that is often associated with a sleep complaint. Patients with RLS have an irresistible urge to move their legs, which is usually due to disagreeable sensations that are worse during periods of inactivity and often interfere with sleep. It is estimated that between 2 and 15 percent of the population may experience symptoms of RLS. Primary RLS likely has a genetic origin. Secondary causes of RLS include iron deficiency, neurologic lesions, pregnancy and uremia. RLS also may occur secondarily to the use of certain medications. The diagnosis of RLS is based primarily on the patient’s history. A list of questions that may be used as a basis to assess the likelihood of RLS is included in this article. Pharmacologic treatment of RLS includes dopaminergic agents, opioids, benzodiazepines and anticonvulsants. The primary care physician plays a central role in the diagnosis and management of RLS.
Chronic Dopaminergic Therapy Can Cause Augmentation Of Symptoms
Augmentation is a common consequence of chronic use of levodopa in restless legs syndrome, and can also occur with dopamine agonists. Augmentation typically involves daytime symptoms becoming more frequent or intense than they were before treatment began, or shifting to an earlier time in the day.9
Refer patients experiencing augmentation to a specialist. Most cases can be reversed with a change in dosing frequency, by lowering the dose, by switching drugs or by stopping dopaminergic therapy.3
Controlled trials of pramipexole have been too short to establish how often augmentation occurs or how to manage it.6 In a retrospective case-series analysis, over an average of 2 years of pramipexole treatment, one-third of patients developed augmentation, on average 9 months after starting treatment.19
Can Restless Legs Syndrome Develop Into Something More Serious
Most people with restless legs syndrome have the “idiopathic” form, meaning there’s no known cause. For them, there is no risk of RLS developing into something more serious, like Parkinson’s disease.
Restless legs syndrome can get worse in people with other medical conditions if they don’t get those conditions treated.
Restless Legs Syndrome Is An Idiopathic Sensorimotor Disorder
Restless legs syndrome consists of a pattern of symptoms involving an urge to move the legs because of unpleasant sensations. Symptoms are worse or only present at rest, worse or only present in the evening or night-time, and are relieved by movement . The diagnosis covers a spectrum from mild and harmless to severe and distressing. As the pathology is unknown and no objective test exists, diagnosis is based on patient report of symptoms, according to consensus criteria.
What Is The Pooled Prevalence Of Rls/wed And Its Mimics In Pd

In view of these contrasting results, what is the overall prevalence of the sum of true, secondary and mimics of RLS/WED in PD? A recently-published meta-analysis4343. Yang X, Liu B, Shen H, Li S, Zhao Q, An R et al. Prevalence of restless legs syndrome in Parkinson’s disease: a systematic review and metaanalysis of observational studies. Sleep Med. 2018 Mar;43:40-6. https://doi.org/10.1016/j.sleep.2017.11.1146https://doi.org/10.1016/j.sleep.2017.11…. tried to answer this question comparing 28 clinical studies. The pooled prevalence among diverse populations was 14%, being higher among those who had previously received dopaminergic treatment than among drug-naïve patients . Differences were also marginal for gender prevalence, favoring women . In their discussion, the authors were careful enough to acknowledge the intrinsic limitations of these studies, including a variety of biases.
Pramipexole Is Not Recommended In Pregnancy Or Breastfeeding
There is a lack of clinical data in pregnancy, along with evidence that pramipexole impairs implantation and disrupts early pregnancy in rats .6 Pramipexole is expected to inhibit lactation because of its effects on prolactin. It may be excreted into breast milk and should not be used during breastfeeding.6
Pathological Evidence Of Dopamine Dysfunction In Pd And Rls
Post-mortem studies in PD demonstrate loss of nigral neurons resulting in striatal dopamine deficiency, with differing morphological lesion patterns according to the clinical subtypes of PD. Cell loss in the ventrolateral part of the substantia nigra pars compacta projecting to the dorsal putamen is more prominent in the akinetic-rigid type, whereas tremor-dominant PD shows predominantly medial SNPC cell loss . Variability in lesion patterning might explain why some patients with PD may develop RLS. In addition, loss of dopamine 2 receptors has been documented in advanced PD .
At autopsy of 8 patients with primary RLS, there was a significant decrease in dopamine 2 receptors in the putamen compared to a neurologically normal control group. The decrease in the D2 receptors correlated to the severity of the RLS . This evidence that the nigrostriatal dopaminergic system is affected in both RLS and PD might provide a stronger argument for an etiologic link between the two. Moreover, there were significant increases in tyrosine hydroxylase in the substantia nigra, but not in the putamen of the RLS group. Phosphorylated tyrosine hydroxylase was found to be increased in both the substantia nigra and putamen. These findings are consistent with data from animal iron deficiency models demonstrating increased presynaptic dopaminergic activity .
Pramipexole May Be Useful For Severe Restless Legs Syndrome
If the patient reports significant distress from restless legs syndrome that cannot be managed by non-drug measures , consider drug treatment in the context of a full discussion about the potential symptomatic benefit and possibility of adverse effects.
Australian guidelines recommend a non-ergot-derived dopamine agonist for pharmacotherapy of restless legs syndrome when symptoms are frequent .3 Indirect and unpublished data, together with experience with other dopamine agonists, suggest that pramipexole is less likely than levodopa preparations to worsen symptoms with long-term use , but that levodopa preparations are better tolerated.4,5 Refer to a specialist if initial treatment is not effective.3
The safety and efficacy of pramipexole have not been evaluated in children and adolescents under 18 years old.6 Children and adolescents with restless legs syndrome that cannot be managed by non-drug measures should be assessed by a specialist.
Guidelines recommend levodopa with either carbidopa or benserazide for occasional use in intermittent restless legs syndrome3, but augmentation limits levodopa’s usefulness for treating daily symptoms.
Restless Legs Syndrome And Periodic Limb Movement Disorder
Most people who have RLS also have a condition called periodic limb movement disorder . PLMD involves repetitive flexing or twitching of the limbs while asleep at night. It is different from RLS in that these movements are not accompanied by uncomfortable sensations and because they occur during sleep, patients are often not aware of them. However, PLMD-associated movements can cause a person to wake up and therefore can compound sleep issues in patients who also have RLS.
Although most people with RLS have PLMD, many with PLMD do not have RLS.
Your Dreams Could Be An Early Clue To Parkinson’s Disease
Breaking down Parkinson’s disease05:25
Actor Alan Alda revealed that he has Parkinson’s disease — and in an interview Tuesday on “CBS This Morning,” the award-winning actor said an unusual dream helped lead to his diagnosis.
Alda, best known for his portrayal of Army Capt. “Hawkeye” Pierce in the TV series “M*A*S*H, was diagnosed three and a half years ago after experiencing a lesser-known early sign of Parkinson’s. He said he asked his doctor to test him for the disease after reading an article about how physically acting out your dreams can be one of the earliest precursors of the neurological disorder.
“I asked for a scan because I thought I might have it,” Alda said. “I read an article by Jane Brody in The New York Times that indicated that if you have — if you act out your dreams, there’s a good chance that might be a very early symptom, where nothing else shows.” He recognized that it had happened to him.
“By acting out your dreams, I mean I was having a dream where someone was attacking me and I threw a sack of potatoes at them, and what I was really doing was throwing a pillow at my wife,” Alda explained.
At that point, he had no other sign of illness. “The doctor said, ‘Why do you want a scan? You don’t have any symptoms,'” Alda recalled. “And I said, I want to know if there’s anything I can do — I want to do it.”
Restless Legs Syndrome: A Common Underdiagnosed Disorder
Edward M. DeSimone II, RPh, PhD, FAPhAProfessor of Pharmacy SciencesSchool of Pharmacy and Health ProfessionsCreighton University
School of Pharmacy and Health ProfessionsCreighton UniversityOmaha, Nebraska
US Pharm.
Restless legs syndrome is a common sensorimotor disorder of the central nervous system. It is characterized by an irresistible urge or need to move the limbs that occurs as a result of uncomfortable limb sensations. Although RLS usually starts in the legs, it can spread to other parts of the body, such as the arms or torso. RLS sufferers often describe the disorder as feeling like water flowing inside the legs, “bugs in the bones,” or electricity in the legs. These symptoms may be present all day, but usually worsen during periods of inactivity and in the evening. People with RLS usually must move their limbs for complete or partial relief of the uncomfortable sensations. At night, RLS often is associated with periodic limb movements , which can cause sleep problems and also make it difficult to perform sedentary activities such as sitting comfortably in a car or on an airplane for extended periods.
When Should I See A Doctor About Restless Legs Syndrome
You should see a doctor to confirm the diagnosis of RLS and to exclude other conditions that may resemble RLS. The doctor can treat associated problems like iron deficiency.
If you have RLS, you should also see a doctor if you are:
- Feeling depressed or anxious
- Having trouble concentrating
You don’t have to wait until one of these things happens. If you just want to feel better, see your doctor.
Restless Leg Syndrome And Multiple Sclerosis Connection

Cases of restless leg syndrome in multiple sclerosis patients greatly vary from 13.3 percent to 65.1 percent. These numbers are still larger than rates of restless leg syndrome in the general population. Multiple sclerosis patients with RLS rate higher on the Expanded Disability Status Scale compared to MS patients without RLS. RLS can negatively impact a person’s sleep and cause further complications such as worsened fatigue and greater inflammation, which can contribute to pain. Further research will be conducted to better understand the connection between RLS and MS and provide more effective treatment.
Other Conditions Associated With Restless Legs Syndrome
The following medical conditions are also associated with RLS, although the relationships are not clear. In some cases, these conditions may contribute to RLS. Others may have a common cause, or they may coexist due to other risk factors:
- Osteoarthritis . About three-quarters of patients with RLS also have osteoarthritis, a common condition affecting older adults.
- Varicose veins. Varicose veins occur in about 1 in 7 patients with RLS.
- Obesity.
- Diabetes. People with type 2 diabetes may have higher rates of secondary RLS. Nerve pain related to their diabetes cannot fully explain the higher rate of RLS.
- Hypertension .
- Chronic obstructive pulmonary disease .
- Chronic alcoholism.
- Sleep apnea and snoring.
- Chronic headaches.
- Brain or spinal injuries.
- Many muscle and nerve disorders. Of particular interest is hereditary ataxia, a group of genetic diseases that affects the central nervous system and causes loss of motor control. Researchers believe that hereditary ataxia may supply clues to the genetic causes of RLS.
- Attention-deficit hyperactivity disorder .
- Psychiatric disorders, such as depression.
The Link Between Rls And Parkinsons: Dopamine Agonists
Although the cause of RLS remains unknown, we know that RLS runs in families in about one-half of the cases, and that some families have an abnormality on chromosome 12. Because RLS is well treated by medications that also treat Parkinson’s disease, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in Parkinson’s disease, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that there is no major deficit on PET or other imaging studies of the brain, as is there is in PD. The spinal fluid is normal in RLS, but shows low dopamine in PD.
Lastly, RLS does not progress to cause other major symptoms such as tremor, gait disorder, or loss of taste or smell, and does not progress to PD. In fact, one of the leading possibilities as the cause of RLS and for which there is good scientific evidence and much research is a form of iron-transport abnormality in the brain. In effect, RLS patients may have low levels of iron in brain nerve cells—just the opposite of some portions of the brain in PD.
Dr. Poceta is a Consultant in Neurology and Sleep Disorders in the Division of Neurology, Scripps Clinic, La Jolla, and the Scripps Clinic Sleep Center. His current interests include organized medicine and Internet medicine.
Is Restless Leg Syndrome A Precursor To Other Ailments
One of the more interesting and somewhat unusual behaviors that can affect residents of Mount Vernon and elsewhere is Restless Legs Syndrome. It affects about 10 percent of the U.S. population, including some receiving hospice care, and ranges from occasional twitches to full motion throughout the day.
It’s also a condition that the team at Above and Beyond Home Health Care has experience with. Some of our clients have it or have had Restless Legs Syndrome and we also are happy to educate people who may have recently been diagnosed with it. In some cases, it may be accompanied by other health conditions, or sometimes it may indicate a higher risk of other conditions in the future. It also can be scary and confusing when someone is diagnosed.
According to the National Institutes of Health’s National Library of Medicine, science has been officially tracking Restless Legs Syndrome as its own behavior since the mid-1990s. Prior to this, it may have been observed but thought of more as a symptom of various types of health conditions.
Since then, research has continued into how Restless Legs Syndrome behaves and different methods or medications that may be able to reduce its strength and duration. As with any health topic, some knowledge has changed as more cases are observed or as medical professionals learn more about possible interactions with Restless Legs Syndrome and other conditions.
Restless Leg Syndrome As A Symptom For Other Diseases

Aside from multiple sclerosis, restless leg syndrome can be a symptom of other diseases as well. A recent study revealed that restless leg syndrome can be a symptom of heart problems, kidney problems and stroke.
For the study 3,700 veterans with RLS were observed along with 3,700 healthy participants as controls. Both groups were followed for eight years. Researchers were specifically looking for outcomes of stroke and heart and kidney problems.
Related Reading:
Restless leg syndrome is symptom for stroke, heart and kidney disease: Study
Restless leg syndrome has been found to increase the risk of stroke, heart disease and kidney disease. Restless leg syndrome is a condition that causes a person to feel an overwhelming urge to move their legs when in an inclined position . Tingling, aching and itching sensations may occur as well. Continue reading…
New research from the University of Vermont suggests that in mice models, salt intake may increase the risk of developing multiple sclerosis . With the use of three genetically different groups of mice, researchers conducted their study. Continue reading…
