Parkinsons Disease And The Perfect Golf Swing: Reflections On My Dad

The earliest memories I have of my dad are of him practicing his golf swing in front of a mirror. It was a beautiful golf swing, perfected through hours upon hours of repetition. He loved the game. He was very physically fit, as a U.S. Marine. He would routinely do 100 push-ups and then run around the neighborhood in his black Marine Corps boots to assure he kept his callouses for reserve weekends. It was the late 1960’s.
He must be a great player, I thought. It took me a few years to realize that my dad did not play golf.
My dad was the oldest son of Irish immigrants. At the age of 18, two weeks into his freshman year at Iona College, my dad received the news that he had a new sibling, a brother. This brother, his youngest, was born with Downs Syndrome. This news would impact my dad’s life in ways he couldn’t have imagined.
Dad completed his graduate studies, began his career in public education and bought his first house. He changed the oil in his old Volkswagens and tuned up the lawnmower to save money. As he pushed the mower past the picture window at the front of our house, he would stop and practice his golf swing in the reflection, so he would be ready for the day when he had the time and resources to play.
Learn How And When To Offer Help
Caregiving begins with the recognition that your loved one needs help and the acceptance that they may not want help yet. Wiener said adult children often call the helpline because they’re worried about their mother, who’s doing all the caregiving for their father. In those cases, Wiener suggests framing the suggestion of extra help as good for the father’s well-being, too. “You can ask, ‘if something happens to you, who will take care of him?’” Sometimes, though, “you have to wait for the crisis” and be ready to help when it becomes clear to your parents that they need more assistance.
Immobility Doesnt Mean Limitation
Your parent may find that their mobility issues start to become more pronounced as their Parkinson’s progresses. The pressure on their partner to care for them can become a burden they may not be able to carry by themself.
Buying mobility aids and equipment to help your parent remain in their own home for longer as well as hiring carers to help with day-to-day tasks can keep your parent independent and relieve the caring responsibilities from their partner.
No Time To Smell The Roses
Over the next 30 years, my dad would rise to become the Superintendent of Schools in a prestigious town in New Jersey. My siblings and I all went off to college and began our own careers. Throughout this time, my dad was an invaluable resource to his mom, dad and brothers in guiding the management of his youngest brother, helping to navigate social services, education and eventually work programs with the objective of socializing and mainstreaming his brother’s experience. My dad led the creation of a group home established by the State of New Jersey and the families of other developmentally disabled adults to form a public-private partnership to allow these adults to be in their community. Later in life, my mom and dad became heavily invested in the transitions of my grandparents, as well. Caregiving was a constant in their lives.
When my dad retired from the NJ Public School System, he had planned to play a lot more golf. He joined the club in his community and would bring his children and grandchildren out to play. Within six months of his retirement, my dad was diagnosed with Parkinson’s disease. He was 60. He played as much golf as he could, but slowly lost his coordination and the swing – perfected in the mirror throughout his decades of self-sacrifice – began to drift away.
There’s Something Unsettling About Someone Standing When You Feel Like They Should Be Sitting

“Dad, you want to just sit here for a minute while I get us a drink?”
On that, he plopped down and I positioned our bags so they’d be in his sight and reach.
“A muffin would be good, too,” he added.
“OK. I’ll see if they have muffins.”
I turned and headed back to the concession stand. I couldn’t have walked more than five or six steps before I glanced back over my shoulder at him. He was still sitting there. I don’t know what I expected to see — like he was going to erupt in flames the moment he was out of my sight or something.
I got in line, and as I waited my turn, I kept looking back.
“Watch him like a hawk.”
We hadn’t come this far to have him fall down and break his wrist or have our bags stolen from under his nose.
In That Moment I Got A Glimpse Of My Dad The Real One
The one who raised three kids and taught us how to throw a football, how to use a hammer, how to treat people. The one who, in another world, would have been leading me through the airport, reciting Civil War trivia as we walked. The one who, to an outsider, would have been just a guy.
The one who, to those who knew him, was far from just a guy.
Volunteer To Help Out
Everyday responsibilities like shopping, cooking, and cleaning become much more difficult when you have a movement disorder. Sometimes people with Parkinson’s need help with these and other tasks, but they may be too proud or embarrassed to ask for it. Step in and offer to run errands, prepare meals, drive to medical appointments, pick up medications at the drug store, and help with any other day-to-day tasks they have difficulty with on their own.
What Makes Pd Hard To Predict
Parkinson’s comes with two main buckets of possible symptoms. One affects your ability to move and leads to motor issues like tremors and rigid muscles. The other bucket has non-motor symptoms, like , loss of smell, and .
You may not get all the symptoms. And you can’t predict how bad they’ll be, or how fast they’ll get worse. One person may have slight tremors but severe dementia. Another might have major tremors but no issues with thinking or memory. And someone else may have severe symptoms all around.
On top of that, the that treat Parkinson’s work better for some people than others. All that adds up to a disease that’s very hard to predict.
My Father Received Poor Treatment For Parkinson’s Here’s What I Did
His care left me horrified – but it spurred me on in my medical career to make sure others didn’t face the same ordeal
As tremors go, it wouldn’t have rated much on the Richter scale but, back in 1990, the shake in my father’s right hand had a seismic impact on him, and our family.
Dad was in his late 50s, a research chemist, and was hoping to retire in a few years. I was a nerdy 16-year-old Belfast schoolboy, with aspirations of medical school. I can still recall the day he came back from the hospital appointment that confirmed all our fears – it was Parkinson’s.
For the first few years, things seemed to be OK. Dad was taking medication that was working – he was able to get about, do what he wanted and his intellect and wit still shone through. It was only when I started working as a junior doctor that things got more difficult.
There was no eye contact with the doctor, no empathy and our concerns about my father’s deterioration were brushed aside
Dad’s response to his treatment had become increasingly unpredictable. He would be stuck to the spot like a mannequin, waiting what felt like hours for his medication to kick in. Once it did, he was great again, but the tablets would wear off far more quickly. Our days became ruled by the clock – hoping he would make it through to his next dose without the last one completely wearing off.
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinson’s report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include “delirium,” in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and “isolated minor symptoms” or “minor hallucinations,” including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinson’s. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinson’s not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinson’s is a complex disease and as it progresses the percentages and risk of symptoms will change.
What Are Hallucinations
Hallucinations are when someone sees, hears or feels something that is not actually there. They are best described as deceptions or tricks played by the brain that involve the body’s senses. Hallucinations are not dreams or nightmares. They happen when the person is awake and can occur at any time of day or night.
But What Stood Out About This Man To Me Was That He Didn’t Have Any Food Stains On His Clothes
He didn’t have elastic shoelaces or drawstring pants. He didn’t have hearing aids. He didn’t have anyone with him to help him get on the plane without getting lost.
I started to hate him because I thought, this is who my dad was supposed to be.
My call finally ended and I hung up. At this point, I had seen enough of the muffin massacre and was ready to go get us a plate, some napkins, something. But I remembered I hadn’t gotten us a preboarding pass yet and we’d be boarding any minute. My dad — not surprisingly — doesn’t do well with people nipping at his heels, squeezing around him, crowding him, hurrying him. We needed to board before the rest of the passengers. It was one of the last obstacles between us and home.
At the ticketing desk, I kept glancing back as I talked to the agent.
“I’m traveling with my father who is, uh, he has… He’s handicapped.”
I never know how to describe it.
Lessons From Being The Child Of A Parent With Parkinsons
For those with the responsibility of having to care for someone diagnosed with Parkinson’s Disease, we all know that it’s far from easy. It is not a one-man job and it is important to reach out for help whether it be from a family member or a caretaker.
My mother was diagnosed with Parkinson’s in 2006 at the age of 46. She underwent DBS surgery in 2009, cervical realignment in 2016, and completed a promising cancer drug clinical trial at Georgetown Hospital conducted by Dr. Fernando Pagan and Dr. Charbel Moussa. My mother also participates in frequent physical and speech therapy and follows an intense medication regime. After almost 15 years since my mother’s diagnosis, I have grown up learning a lot about what it takes to effectively help someone struggling with Parkinson’s and improve their quality of life.
A Positive Mental Attitude
Focusing on the positive ways you can help your parent instead of worrying about how to prevent their Parkinson’s from worsening can help to remove stress and anxiety from the situation.
While there are many treatments to ease your parent’s symptoms they’ll benefit enormously from having their family and friends around them, supporting them as they face such a degenerative disease. Love, acceptance and friendship go a long way when caring for a parent with Parkinson’s.
Listen To The Podcast
“He said: ‘Have you got a big mortgage? How many kids have you got? Sorry to say you’ve got Parkinson’s’.
“That was a lousy way of telling it, as if he thought he was God.”
Dave was devastated by the diagnosis, but determined to deal with it differently to his father and not keep it a secret.
“I walked away from the specialist, across Wimbledon Common, and tears were running down my cheeks. But the sun was shining and I thought, the sun’s going to shine for a bit longer yet.”
He allowed himself 24 hours to feel down about the news, although admits the first three months were hard to get through.
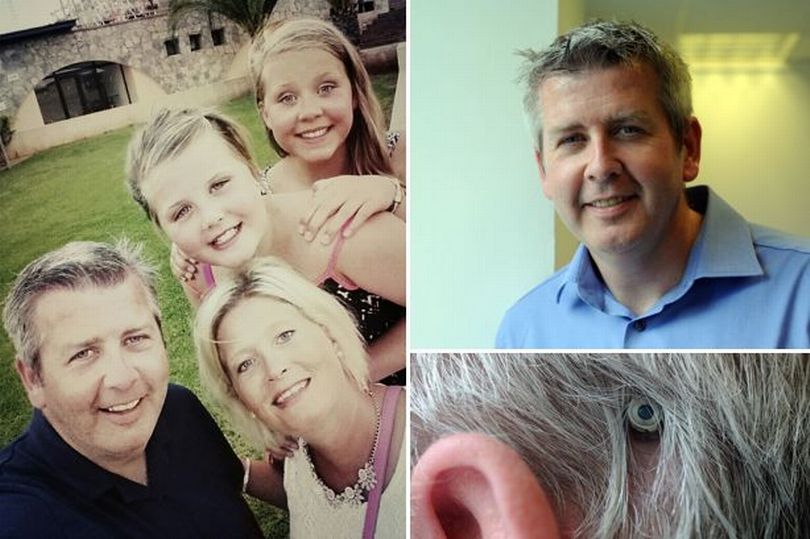
Dave and his wife Carolyn, a clinical psychologist decided to tell their sons, then aged seven and four, that their dad had the neurological condition as soon as questions arose, to make it a normal part of family life. Carolyn has since helped to write a guide on talking to children about Parkinson’s.
“We’ve been very open with the kids from day one because, again, just what happened with my dad, just keeping a secret. And I think it’s important that they knew about it.
“They know I’m getting worse and they know it’s very serious, but I’m just ‘Dad’.”
He says the way his children have accepted it makes him feel guilty about the way he viewed his own father when he turned up unannounced to his football games.
“I didn’t like to see him hunched up and looking shaky on the side of the pitch and I’m embarrassed by that reaction now.
Dave’s tips for living with Parkinson’s
My Dad Wont Help Himself With His Parkinsons
My dad was diagnosed with Parkinson’s about six years ago. My parents are still young . My mom cares for my dad but he won’t help himself and is running my mom ragged. He doesn’t follow any of his doctors advice apart from medication. He doesn’t do the physio exercises, he doesn’t do what the psychiatrist recommends, my sister and I have provided all the research and info we can find for him to read, but he doesn’t. My sister offered to take him to a Parkinson’s support group but he won’t go because he doesn’t want to listen to other people’s problems. He’s allowed this disease to take him over.
The observations I’ve made is that he’s learned to manipulate situations. If there’s something he doesn’t want to do or talk about, all of a sudden he doesn’t feel well. For example, I bought him a day timer to schedule his days and work activities into it so he’s not so dependent on my mom . He got upset, said he wasn’t feeling well and we never did discuss it again. Or, my parents have a cabin at a nearby lake. If there’s work that needs to be done , he doesn’t feel well and my mom has to do it on her own or find someone to help her. However, if she suggestsgoing fishing on the lake, he can last all day without issue.
My sister lives in the same town as them but has two young children and I live 2.5 hours away. My mom can’t take much more and I don’t know how to help.
Try To Preserve Your Relationship With Your Loved One
One big piece of advice Wiener shared is to focus on your first relationship role with your loved one, whether that’s adult child, sibling or spouse. “If there are funds, you can hire people to do the care tasks that come with caregiving. That frees you up to enjoy the time you have with your loved one, doing things that you would normally do.”
Confronting The Unspoken Truth Of My Father’s Life With Parkinson’s
Now that I have seen and treated many people faced with chronic illness, like living with Parkinson’s, I truly feel it is better not to go through it alone.
I first noticed my father’s when I came home for vacation during my first year of medical school. While we were driving back to the house from the airport, I saw something moving in the periphery of my vision. My father was sitting in the passenger seat, his left hand shaking. He saw me glancing at it and explained that the tremor had started a few weeks ago. As a physician himself, he came up with some fancy explanations for the cause. None of them included .
As the years went by, I noticed subtle changes in him. Every few months when I came home from school, he seemed a little different. His gait deteriorated, becoming more slowed and shuffled, and his posture more stooped. It was obvious that his sleeping patterns had become disrupted: I would find him napping throughout the day; at night, he would often wake up from vivid nightmares.
Even his face began to change—it seemed less expressive and animated. His speech grew softer, he mumbled, and he had to repeat himself often. In a matter of a few years, my father had transformed into a different person, a man with textbook PD symptoms. On the outside, he no longer resembled the tall, strong, bold man I knew to be my dad. But inside, his mind and his heart remained the same.
‘my Father Kept Parkinson’s A Secret I Haven’t’
When sports broadcaster Dave Clark was diagnosed with Parkinson’s at the same age as his father – 44 – he knew he couldn’t keep it a secret. His dad, Alan, had been so worried about the stigma around it at the time that he didn’t tell anyone and eventually took his own life.
Alan Clark, was a sales rep in Bradford when he was diagnosed with Parkinson’s, a neurological disorder that attacks the area of the brain which controls movement. It was the 1980s and he was worried he would lose his job if he disclosed he had the disease.
He continued to work full-time to provide for his wife and two sons. Even when he turned up to meetings with hands that shook so much he was accused of being drunk, he still refused to reveal what was going on.
Alan’s son, Dave, a Sky Sports presenter, says: “He went to the doctors by himself, didn’t eat with the family because he was worried about his shakes. He didn’t tell anyone he had Parkinson’s, including me.
“It didn’t end well for my dad. He died when he was 52, took his own life.”
Unknown to Alan, his son had discovered this closely guarded secret as a teenager. Dave happened to watch a documentary, which explained the condition, while he was off sick from school.
It said Parkinson’s causes symptoms such as shaking and slowness of movement due to a reduction of dopamine-producing nerve cells in the brain. Dopamine helps transmit signals between nerve cells.
But decades after his father’s death, he started to suspect something may be up.
Challenges You As A Caregiver Are Likely To Face
There are challenges that a person with Parkinson’s disease confronts. First, the disease can vary from day to day. There will be times when they can function almost normally and then other times when they will be very dependent. This is a natural part of the disease. But it can make a caregiver feel that the person is being unnecessarily demanding or manipulative. Keep in mind that Parkinson’s is unpredictable and each day can pose new challenges for you and your loved one.
Also, keep in mind that Parkinson’s is a progressive disorder. While medications and surgery can provide significant relief of symptoms, they do not stop the progression of the disease.
Depression is also very much a part of the disease. It is important to recognize the signs and symptoms of depression so you can help your loved one seek treatment promptly. And, if you are feeling depressed and having trouble coping, it’s just as important to get care for yourself.
Parents And Parkinsons Disease

My advice to anyone whose parent has recently been diagnosed with PD or has been struggling for years with the disease would be to embrace every moment as a gift and a miracle. I know it sounds cliche, but right now is all we truly have. Try not to be discouraged by the way the disease robs your loved one of their physical strength and independence. Focus instead on what you love about your parent, and help them to see that you love them for who they are. Spend time talking with them. Do what they love to do, and help them to find outlets that bring joy to their souls. Yes, it is truly heartbreaking to watch someone you love become physically less than what they were, but the person you love is still there. They need you – be there for them.
Keenly Observe The Signs And Symptoms
Parkinson’s affects everyone differently. The signs of Parkinson’s described in my father’s story may not necessarily repeat in your loved ones. So be a keen observer. Usually it starts with slight involuntary tremors, sudden or gradual drop in weight, drop in Blood pressure, Tiredness, pain either in joints or throughout the body, various bladder concerns including constipation, accumulation and drooling of saliva and thereby difficulty in swallowing food or drinking water, Emotional changes like depression, sometimes hallucinations and difficulty in memorising and reduction in the capability to think. My father experienced difficulty to maintain a proper posture and developed a hunchback. He hardly sat rather he always maintained a slanting posture. Make note of these symptoms with respect to their time of occurrence in a day. For example: Do they experience tremors in the morning, or does it reduce later? Do they have the drooling saliva problem in the morning or does it vanish off as the day progresses, the consequence of taking a medicine and so on.
Celebrating Rare Disease Day
This year, we’ll be celebrating Rare Disease Day on Feb. 28 to pay homage to unique struggles like my dad’s. While Parkinson’s isn’t a rare disease, I know that my dad struggles with symptoms that are pretty uncommon. And I want to honor that struggle.
Rare Disease Day was created to raise awareness and grab the attention of both policymakers and the general public. According to the International Federation of Pharmaceutical Manufacturers & Associations, about one in 15 people worldwide suffer from a rare disease, and there are between 5,000 and 8,000 known rare diseases. These conditions cause much grief and pain on a daily basis.
My dad is optimistic that scientists may be close to finding a cure for Parkinson’s. And I can only imagine that those who struggle with rare diseases hope for the same. Maybe scientists can at least develop treatments to alleviate symptoms and help those in pain. On days like Rare Disease Day, we can shout a little louder to get the attention of those who can do something about the suffering.
Parkinson’s disease brings a tremendous amount of strife to our lives, never ceasing to take away my dad’s abilities. But it has also brought silver linings: We spend more time with one another, knowing that we won’t live forever. I make it home a little more frequently to ensure I’m not missing all of the important moments. And we’ve begun to talk about our feelings — something our family has never been very good at doing.
