Understanding How This Dementia Differs From Alzheimer’s Can Help Patients Know What To Expect And Feel Less Fearful
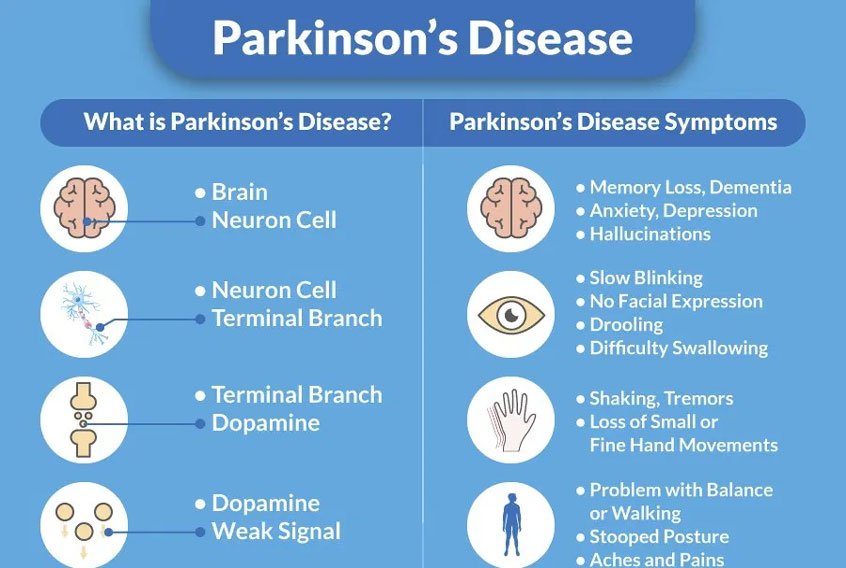
En español | Many symptoms of Parkinson’s disease — shuffling gait, quivering hands, stooped posture — are easy to spot. But this disease can also cause problems that are far less visible but no less distressing. Perhaps the most worrisome is cognitive decline, which affects about 50 percent of patients.
“This is a scary, confusing and concerning topic for a lot of people,” says neurologist Rachel Dolhun, M.D., senior vice president of medical communications at the Michael J. Fox Foundation. While these feelings are natural, common misconceptions can exacerbate patients’ fears.
For starters, cognitive decline doesn’t necessarily equal full-blown dementia, and many people with Parkinson’s develop only mild impairment. Another misconception is that even slight memory slippage signals that rapid deterioration is imminent — but that’s far more common with Alzheimer’s disease than it is with Parkinson’s, says Tsao-Wei Liang, M.D., chief of the movement disorders division at Jefferson Health. “It’s not always relentlessly progressive, and more often than not, symptoms can be managed with medication, caregiver support and basic organizational strategies,” he says.
It’s also important to know that many Parkinson’s patients with some cognitive impairments are able to form new short-term memories, even if they struggle with attention and multitasking. “People with Parkinson’s will often remember if you give a clue or prompt them,” Dolhun says.
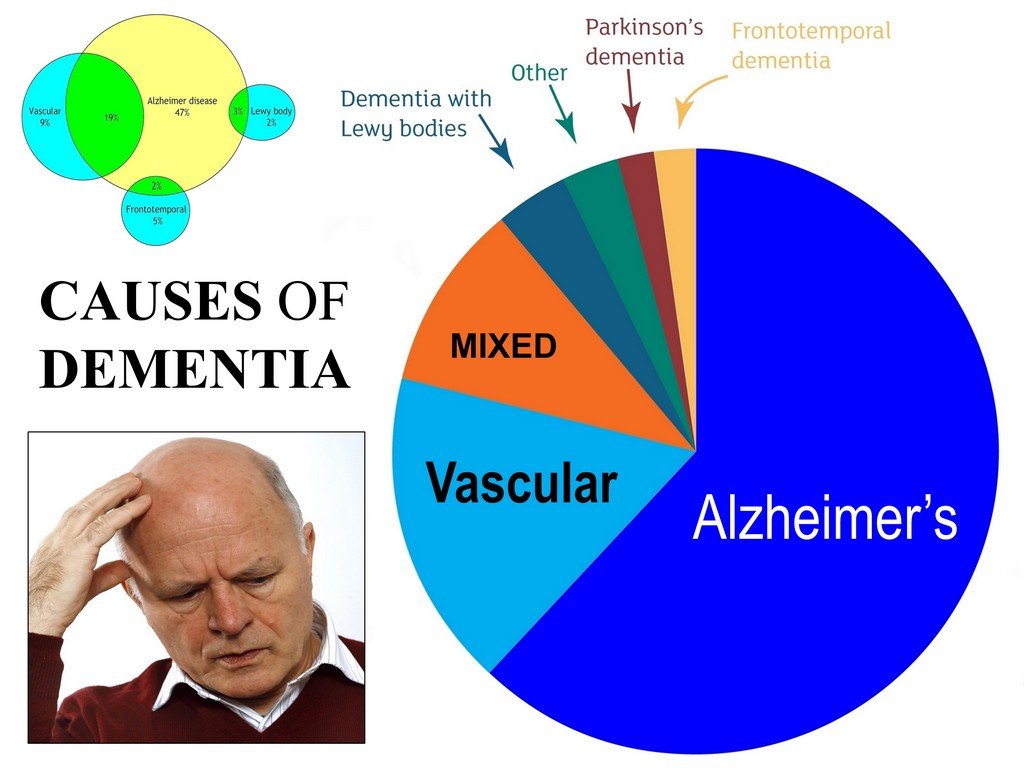
Whats The Difference Between Lewy Body Dementia Parkinsons Disease And Alzheimers Disease
Lewy body dementia is an umbrella term for two related clinical diagnoses: “dementia with Lewy bodies” and “Parkinson’s disease dementia.” These disorders share the same underlying changes in the brain and very similar symptoms, but the symptoms appear in a different order depending on where the Lewy bodies first form.
Dementia with Lewy bodies is a type of dementia that causes problems with memory and thinking abilities that are severe enough to interfere with everyday activities. It specifically affects a person’s ability to plan and solve problems, called executive function, and their ability to understand visual information. Dementia always appears first in DLB. The motor symptoms of Parkinson’s such as tremor, slowness, stiffness and walking/balance/gait problems usually become more evident as the disease progresses. Visual hallucinations, REM sleep behavior disorder, fluctuating levels of alertness and attention, mood changes and autonomic dysfunction are also characteristic of DLB.
Finally, Alzheimer’s is characterized by different abnormal clumps called amyloid plaques, and jumbled fiber bundles called tau tangles. These microscopic structural changes in the brain were discovered by Dr. Alois Alzheimer in 1906. These plaques and tangles, together with loss of connections between nerve cells, contribute to loss of coherence and memory, as well as a progressive impairment in conducting normal activities of daily living.
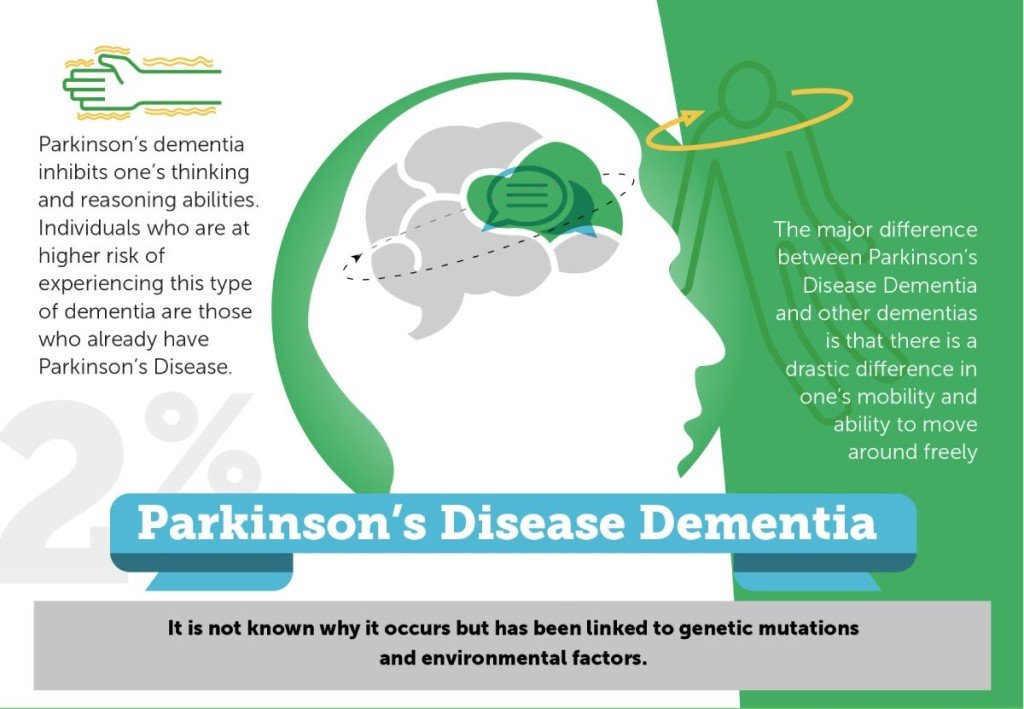
Difference Between Parkinsons Disease Dementia And Dementia With Lewy Bodies
Technically, the difference between these two conditions lies in how quickly the cognitive difficulties and hallucinations develop in relation to the movement issues. In DLB, the cognitive difficulties and hallucinations develop much sooner in the disease course than in PDD, sometimes even prior to the movement difficulties. Because of the similarities between PD, PDD, and DLB, current thinking in the medical community is that they should be viewed as related diseases which fall along a continuum of Lewy body disorders.
Dementia Can Be Treated Through Medication But Its Progression Will Continue
Some of the problems caused by dementia are treatable, but there are no medications that slow the progression of this problem, just as there are no treatments that slow the progression of the rest of the Parkinson’s Disease syndrome. We often use the same medications that are used in Alzheimer’s disease to improve concentration and memory, although only one, rivastigmine, has been approved by the Food and Drug Administration for dementia in PD. Most experts believe that each of the Alzheimer drugs are about as useful in dementia in Parkinson’s Disease as they are in Alzheimer’s, which, unfortunately, is not great. As with all medications used in PD, whether for slowness, stiffness, tremor, depression or sleep disorders, if the medication is not helpful, one should either try a higher dose or stop it. Since the drugs used to treat dementia take several weeks to work, and the dose often requires increases, the family needs to allow a reasonable time period, usually around two months, to decide if it is helpful or not. Obviously this needs to be discussed with the prescribing doctor.
There is a lot of research being done to better understand and better treat dementia in PD.
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
What Are Parkinson’s Disease Dementia Medical Treatment And Medications
There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa; medications known as dopamine agonists that act on the dopamine receptor; and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with Alzheimer’s disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
Things You Should Know About The Link Between Parkinsons And Dementia
Both Parkinson’s disease and dementia were ravaging the brain and behavior of actor Robin Williams before his death, but at the time, he didn’t realize he had the latter.
Despite the fact that the signs of this combination can be confusing, the double diagnosis of Parkinson’s and dementia impacts a large number of people. Of the one million people who have Parkinson’s in the U.S., 50 to 80 percent may have dementia—either as a result of Parkinson’s pathology, or separately.
Robin Williams’ widow, Susan, wrote an editorial published in Neurology that was addressed to neurologists after his death. In it, she shared what it was like seeing her husband experience both Parkinson’s disease and Lewy body dementia firsthand.
“My hope is that it will help you understand your patients along with their spouses and caregivers a little more,” Susan wrote.
Williams was first diagnosed with Parkinson’s disease, which at first seemed to provide some answers for his out-of-character symptoms.
But it wasn’t until after his death that an autopsy revealed he had been in the later stages of Lewy body dementia—a common form of dementia characterized by deposits of Lewy body proteins in the brain, which can impact physical movement, mood, memory and behavior.
“I will never know the true depth of his suffering, nor just how hard he was fighting,” Susan wrote. “But from where I stood, I saw the bravest man in the world playing the hardest role of his life.”
The Pathologies Are Different But Many Of The Symptoms Can Be Similar
“We do know that the pathology is quite different” between Parkinson’s and dementia, said Dr. Odinachi Oguh, a neurologist at the Cleveland Clinic Lou Ruvo Center for Brain Health. “But the processes in which memory is impacted in both diseases is about the same.”
“From the pathology standpoint, both diseases are characterized by a neurodegenerative process,” Oguh said. “The neurodegeneration results in abnormal accumulation of protein, which builds up and becomes toxic to the brain.”
Alzheimer’s, for example, affects memory areas of the brain, which include the temporal lobes, as well as the memory center, or hippocampus. Parkinson’s, meanwhile, starts in the basal ganglia part of the brain, and as the disease progresses, it can also affect the memory center, resulting in forgetfulness, an early sign of Alzheimer’s or other forms of dementia.
How Is Parkinsons Disease Dementia Different From Alzheimers Disease
Parkinson’s disease Dementia must not be confused with Alzheimer’s disease. Dementia is a hallmark feature of Alzheimer’s whereas a patient may not necessarily contract Dementia if he happens to contract Parkinson’s. Having mentioned that, Dementia does have a greater social and occupational impact on the functioning of people when it affects someone with Parkinson’s as compared to Alzheimer’s.
This is due to the combination of motor and cognitive impairments. Parkinson’s directly affects problem-solving functions in a person, besides other aspects such as the speed of thinking, memory, and mood. Parkinson’s Dementia Aggression can also be related to Lewy bodies, where sticky clumps of protein are found in the nerve cells of people diagnosed with Parkinson’s.
Finally, it must be known to all those associated with Parkinson’s in any capacity, whether be it a patient or a caregiver, that majority of people with Parkinson’s may experience some of the other forms of cognitive impairment over time. Though cases vary from person to person, the development of Dementia in those diagnosed with Parkinson’s cannot be predicted. To put it in numbers, 30 percent of people with Parkinson’s never develop dementia as a part of their progression.
How Parkinsons And Alzheimers Affect The Body And Brain Differently
Alzheimer’s and Parkinson’s are both neurological illnesses. Both diseases are caused by damaged brain cells. Both conditions can involve dementia, as well as depression, anxiety, and sleep disturbances. Both conditions can lead to psychotic symptoms such as delusions and hallucinations.
While Alzheimer’s and Parkinson’s share certain causes and effects, the two diseases are different. They impact the brain and progress in different ways. Both disorders affect people differently, manifest themselves differently, and progress at different rates.
I had a father with Parkinson’s and a mother with dementia. My experience was that the Parkinson’s progressed at a slower rate and was more motor-related than mental.
My father experienced tremors, as well as changes in his walking and facial expressions. But his cognitive ability was relatively intact up to the very last stages of the disease. My mother’s dementia made her feeble and uncertain on her feet, but she remained active and mobile, even as her cognitive ability declined.
Fauci Flu Shots Massively Accelerate Progression Of Prion Diseases
Under normal circumstances without a vaccine, the progression of prion diseases, which is demarcated by the abnormal folding of certain proteins, takes many years. After a Fauci Flu shot, however, that process greatly accelerates – you might say at “warp speed.”
Classen believes that Chinese Virus injections could be piggybacking on mild prion disease that is already in motion in some people, while in others the shots could be actively prompting the misfolding of essential RNA and DNA binding proteins called TDP-43 and FUS, thus catalyzing a toxic “chain reaction” process.
It is probably a little bit different in every person’s body depending on their unique biology, but the end result is still the same: neurodegeneration. For some it happens quickly and in others more slowly, but the common denominator is that it happens.
Classen also says that the vaccine spike proteins could be causing other protein, “including proteins already in cells,” to form what he describes as abnormal clumps called Lewy bodies that can lead to “relatively rapid cell death.”
Research has shown that the development of Lewy bodies in monkeys exposed to the Chinese Virus resulted in “some or all of the motor symptoms of Parkinson’s disease.”
All this pain and suffering to maybe avoid a case of the sniffles? Tragic and idiotic.
As injected people continue to fall ill and die from Chinese Virus injections, we will keep you informed about it at ChemicalViolence.com.
Covid Vaccines Confirmed To Cause Parkinsons Dementia Symptoms
Former National Institutes of Health contract scientist and Classen Immunotherapies proprietor J. Bart Classen has published a paper warning that there is strong potential for Wuhan coronavirus mRNA “vaccines” to trigger Parkinson’s, dementia and a variety of other prion and chronic diseases.
Alzheimer’s, amyotrophic lateral sclerosis , and multiple system atrophy , and mad cow disease are all on the table as possible “side effects” of Chinese Virus injections, Classen says, this based on an extensive analysis of the RNA poisons contained in the Pfizer shot.
This latest paper is Classen’s second look at the prion disease risks associated with Fauci Flu shots, drawing from actual adverse event data from the United Kingdom. Far from theoretical, the risk of neurodegenerative disease stemming from Chinese Disease shots is both real and probable.
AstraZeneca’s vector-based injection for the Wuhan Flu, which is not an mRNA jab, is also linked to causing prion disease. It would appear as though all of the jabs created for the Chinese Communist Party virus are linked to this buffet of neurodegenerative illnesses.
After looking at roughly six months’ worth of data ending around mid-June, Classen found that both the genetically engineered adenovirus injections and the lipid-encapsulated synthetic mRNA injections produce deadly spike proteins that can trigger serious and irreversible “nervous disorders.”
Treatment Of Behavior And Mood Problems In Lewy Body Dementia
Behavioral and mood problems in people with LBD can arise from hallucinations, delusions, pain, illness, stress, or anxiety. They may also be the result of frustration, fear, or feeling overwhelmed. The person may resist care or lash out verbally or physically.
Medications are appropriate if the behavior interferes with the person’s care or the safety of the person or others. If medication is used, then the lowest possible dose for the shortest period of time is recommended.
The first step is to visit a doctor to see if a medical condition unrelated to LBD is causing the problem. Injuries, fever, urinary tract or pulmonary infections, pressure ulcers , and constipation can worsen behavioral problems and increase confusion.
Certain medications, such as anticholinergics and antihistamines may also cause behavioral problems. For example, some medications for sleep problems, pain, bladder control, and LBD-related movement symptoms can cause confusion, agitation, hallucinations, and delusions. Similarly, some anti-anxiety medicines can actually increase anxiety in people with LBD. Review your medications with your doctor to determine if any changes are needed.
Antidepressants can be used to treat depression and anxiety, which are common in LBD. Many of them are often well tolerated by people with LBD.
How Is Parkinsons Dementia Different From Alzheimers Disease
The advanced cognitive changes that impact daily living in Alzheimer’s and Parkinson’s disease are both types of dementia.
Parkinson’s disease dementia can occur as Parkinson’s advances, after several years of motor symptoms. Dementia with Lewy Bodies is diagnosed when cognitive decline happens first, or when Parkinson’s motor symptoms and cognitive decline occur and progress closely together. Cognitive impairments in PDD, combined with the movement symptoms of the disease, produce a greater impact on social and occupational functioning than Alzheimer’s.
Alzheimer’s, a fatal brain disease, causes declines in memory, thinking and reasoning skills. Physicians can diagnose Alzheimer’s. Visit the Alzheimer’s Association to learn the 10 signs Alzheimer’s disease.
Fortunately for people with PD, Parkinson’s disease dementia is less disabling than Alzheimer’s disease. People with Alzheimer’s have language difficulties earlier than people with Parkinson’s, and no new memories are formed. People with PD also have more ability to compensate and adjust based on cues.
Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
There’s no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
Dementia Progresses At Different Rates For Different People
Dementia is, unfortunately, progressive but, like the motor features of MD, progresses at very different rates in different people. It not only causes poor memory and thinking, but also is frequently associated with depression, sleep disorders, loss of motivation, loss of interest and pleasure in activities that had previously enriched or even defined their life. Patients with dementia are often apathetic, showing reduced happiness and unhappiness. They are more likely to develop problems with sleeping too much or developing challenging sleep habits brings with it an increased sensitivity to the side effects of all the drugs used in treating Parkinson’s Disease itself. People with dementia are more likely to develop hallucinations or confusion. Therefore the motor problems of Parkinson’s Disease cannot be treated as aggressively in a patient with dementia as compared to the patient without dementia.
Dementia does not kill people. It is not a death sentence. It is true that dementia is associated with a reduced life expectancy, but this is likely due to the greater difficulty involved in treating the motor problems of PD. As noted above, this is because of the increased likelihood of drug side effects in patients with dementia. Unfortunately, more bad things happen to people with dementia. They may forget to use their cane or walker, increasing the risk of falls. They may take their medications unreliably or incorrectly or ignore warning signs of other medical problems.
Theres No Cure For The Diseases But Some Therapies May Help
Certain drugs, like cholinesterase inhibitors and antipsychotic medications, are prescribed as treatment for people with Parkinson’s and dementia. And lifestyle changes—from improved diet, sleep, exercise and socializing—have been shown to have beneficial effects on patients with these diseases.
Oguh noted she hopes that improved treatments that will help some of the emotional and behavioral problems in these patients will be on the horizon soon.
“I’m hoping that with the new advances in medication, we’ll be able to control better,” Oguh said. “I believe there will be better medication to improve cognition in patients, and that that will be seen in the next five to 10 years.”
What Is Needed For A Parkinson’s Disease Dementia Diagnosis
There is no definitive medical test that confirms cognitive decline or dementia in Parkinson’s disease. The most accurate way to measure cognitive decline is through neuropsychological testing.
- The testing involves answering questions and performing tasks that have been carefully designed for this purpose. It is carried out by a specialist in this kind of testing.
- Neuropsychological testing addresses the individual’s appearance, mood, anxiety level, and experience of delusions or hallucinations.
- It assesses cognitive abilities such as memory, attention, orientation to time and place, use of language, and abilities to carry out various tasks and follow instructions.
- Reasoning, abstract thinking, and problem solving are tested.
- Neuropsychological testing gives a more accurate diagnosis of the problems and thus can help in treatment planning.
- The tests are repeated periodically to see how well treatment is working and check for new problems.
Imaging studies: Generally, brain scans such as CT scan and MRI are of little use in diagnosing dementia in people with Parkinson’s disease. Positron emission tomographic scan may help distinguish dementia from depression and similar conditions in Parkinson’s disease.
What Is The Best Way To Communicate With A Person With Pdd
PD-related mood and motor changes can impact communication; cognitive changes and Parkinson’s disease dementia can further these difficulties.
- It is not usually helpful to try to reason or argue with someone experiencing a hallucination or delusion. Stay calm and be patient. If the person is frightened by the hallucination or delusion, try to redirect their attention to something else.
- You may find acknowledging what the person is seeing, even if you do not see it, can reduce stress.
- Speak slowly and at eye level. Communicate in simple sentences.
- Ask one question at a time and wait for an answer.
- Limit distractions. Turn off the TV or radio before asking a person with PDD to do something.
- Consider causes behind disruptive behavior: the person may be hungry, thirsty, tired, in pain, frustrated, lonely or bored.
- If the person is stuck on an idea, try agreeing with them, then changing the subject.
- It’s OK to use humor to diffuse stressful situations but avoid negative humor or sarcasm ? these can be misunderstood.
Page reviewed by Dr. Jori Fleisher, MSCE, Assistant Professor, Department of Neurological Sciences at Rush University Medical Center, a Parkinson’s Foundation Center of Excellence.
What Is Lewy Body Dementia Causes Symptoms And Treatments
On this page:
Lewy body dementia is a disease associated with abnormal deposits of a protein called alpha-synuclein in the brain. These deposits, called Lewy bodies, affect chemicals in the brain whose changes, in turn, can lead to problems with thinking, movement, behavior, and mood. Lewy body dementia is one of the most common causes of dementia.
LBD affects more than 1 million individuals in the United States. People typically show symptoms at age 50 or older, although sometimes younger people have LBD. LBD appears to affect slightly more men than women.
Diagnosing LBD can be challenging. Early LBD symptoms are often confused with similar symptoms found in other brain diseases or in psychiatric disorders. Lewy body dementia can occur alone or along with other brain disorders.
It is a progressive disease, meaning symptoms start slowly and worsen over time. The disease lasts an average of five to eight years from the time of diagnosis to death, but can range from two to 20 years for some people. How quickly symptoms develop and change varies greatly from person to person, depending on overall health, age, and severity of symptoms.
In the early stages of LBD, symptoms can be mild, and people can function fairly normally. As the disease advances, people with LBD require more help due to a decline in thinking and movement abilities. In the later stages of the disease, they often depend entirely on others for assistance and care.
See A Doctor If Youre Noticing Symptoms Beyond Parkinsons

Sometimes the mood or memory changes a person experiences cannot entirely be explained just by Parkinson’s. If this is the case, “the caregiver should explore other diagnoses, because if something cannot be explained by Parkinson’s, there’s certainly a risk of it being dementia,” Oguh said.
She added that some signs to look for include increased memory and behavioral problems, like mood swings, anxiety or depression. Psychiatric behaviors, like hallucinations, delusions or paranoia, cannot just be explained by Parkinson’s, and are more likely to be caused by a form of dementia like Lewy body dementia.
Oguh urged caregivers to be aware of changing symptoms like these.
“I think sometimes family members are able to realize sooner than the patient,” Oguh said. “Often the patient might lack insight as to what is happening. I would encourage family members to seek expert opinion and treatment options.”
Dementia With Lewy Bodies And Parkinson Disease Dementia
, MD, PhD, Department of Neurology, University of Mississippi Medical Center
Dementia with Lewy bodiesParkinson disease dementia
Dementia is chronic, global, usually irreversible deterioration of cognition.
Dementia with Lewy bodies is the 3rd most common dementia. Age of onset is typically > 60.
Lewy bodies are spherical, eosinophilic, neuronal cytoplasmic inclusions composed of aggregates of alpha-synuclein, a synaptic protein. They occur in the cortex of some patients who have dementia with Lewy bodies. Neurotransmitter levels and neuronal pathways between the striatum and the neocortex are abnormal.
Lewy bodies also occur in the substantia nigra of patients with Parkinson disease, and dementia may develop late in the disease. About 40% of patients with Parkinson disease develop Parkinson disease dementia, usually after age 70 and about 10 to 15 years after Parkinson disease has been diagnosed.
Because Lewy bodies occur in dementia with Lewy bodies and in Parkinson disease dementia, some experts think that the two disorders may be part of a more generalized synucleinopathy affecting the central and peripheral nervous systems. Lewy bodies sometimes occur in patients with Alzheimer disease, and patients with dementia with Lewy bodies may have neuritic plaques and neurofibrillary tangles. Dementia with Lewy bodies, Parkinson disease, and Alzheimer disease overlap considerably. Further research is needed to clarify the relationships among them.
Lewy Body Dementia: A Common Yet Underdiagnosed Dementia
While it’s not a household word yet, Lewy body dementia is not a rare disease. It affects an estimated 1.4 million individuals and their families in the United States. Because LBD symptoms can closely resemble other more commonly known disorders like Alzheimer’s disease and Parkinson’s, it is often underdiagnosed or misdiagnosed. In fact, many doctors or other medical professionals still are not familiar with LBD.
Is The Dementia Caused By Parkinsons Or Something Else
Indications that dementia may be caused by something other than Parkinson’s disease include agitation, delusions , and language difficulties. If the onset of cognitive symptoms is sudden, they’re more likely due to something other than Parkinson’s disease—even reversible causes such as infection, a vitamin B12 deficiency, or an underactive thyroid gland.
Depression can mimic dementia by causing similar symptoms such as apathy, memory problems, and concentration difficulties. Since depression is very common in Parkinson’s patients, it’s important to recognize the signs and symptoms of depression in older adults.
Parkinson’s disease dementia vs. other dementias
Other types of dementia that can be commonly mistaken for Parkinson’s disease dementia include:
Lewy Body Dementia is characterized by fluctuations in alertness and attention, recurrent visual hallucinations, and Parkinsonian motor symptoms like rigidity and the loss of spontaneous movement. In this disorder, cognitive problems such as hallucinations tend to occur much earlier in the course of the disease and often precede difficulties with walking and motor control.
Alzheimer’s disease and Parkinson’s disease are both common in the elderly, especially in those over 85. Patients with Parkinson’s who develop dementia may even develop Alzheimer’s dementia as well. Therefore, it’s important to be aware of the and how it’s treated.
Ways To Decrease The Risk Of Parkinsons And Alzheimers
There is currently no “cure” for either disease. Parkinson’s is considered a more treatable condition, however, especially in the early stages of the disease. Treatments include medication, physical therapy, and lifestyle modifications such as dietary changes. Research continues to suggest that a brain-healthy lifestyle can help prevent both Alzheimer’s and Parkinson’s. Here are some basic guidelines:
What Are The Symptoms Of Parkinson’s Disease Dementia
Cognitive impairment in Parkinson’s disease may range from a single isolated symptom to severe dementia.
- The appearance of a single cognitive symptom does not mean that dementia will develop.
- Cognitive symptoms in Parkinson’s disease usually appear years after physical symptoms are noted.
- Cognitive symptoms early in the disease suggest dementia with Parkinsonian features, a somewhat different condition.
Cognitive symptoms in Parkinson’s disease include the following:
- Loss of decision-making ability
- Loss of short- and long-term memory
- Difficulty putting a sequence of events in correct order
- Problems using complex language and comprehending others’ complex language
Persons with Parkinson’s disease, with or without dementia, may often respond slowly to questions and requests. They may become dependent, fearful, indecisive, and passive. As the disease progresses, many people with Parkinson’s disease may become increasingly dependent on spouses or caregivers.
Major mental disorders are common in Parkinson’s disease. Two or more of these may appear together in the same person.
The combination of depression, dementia, and Parkinson’s disease usually means a faster cognitive decline and more severe disability. Hallucinations, delusions, agitation, and manic states can occur as adverse effects of drug treatment of Parkinson’s disease, this might complicate the diagnosis of Parkinson’s dementia.
ADHD Symptoms in Children?
Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy; there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
