If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229

Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
Can A Patients Ability To Make Decisions In The Last Days Of Life Be Impaired And How Is This Managed
In a North American study of 47 carers of idiopathic PD patients in the last months of life most described the goal of care as comfort, and almost half “of the patients were described as unable to make any decisions in the last month of life.” 10
When presenting, the patient may already be unable to communicate their symptoms and care preferences due to cognitive impairment and confusion. Also, there might be a physical difficulty in communication from severe rigidity. Care should be taken in considering the presence and consequent treatment of an intercurrent illness, and whether dopaminergic medication is exacerbating confusion due to hallucinations and/or psychosis.27
Continued attempts at verbal and non-verbal communication should be made throughout given the often fluctuating symptoms associated with PD and possible improvement in the intercurrent illness. In the absence of a next of kin or other person who is able to inform the clinical team, decisions should be made on a best interest basis as recommended in end of life care guidance.30
Stage Four: Symptoms Are Severe And Disabling And You Often Need Assistance To Walk Stand And Move
Stage Four Parkinson’s disease is often called advanced Parkinson’s disease. People in this stage experience severe and debilitating symptoms. Motor symptoms, such as rigidity and bradykinesia, are visible and difficult to overcome. Most people in Stage Four aren’t able to live alone. They need the assistance of a caregiver or home health aide to perform normal tasks.
Stage Three: Symptoms Are More Pronounced But You Can Still Function Without Assistance
The third stage is considered moderate Parkinson’s disease. In this stage, you’ll experience obvious difficulty with walking, standing, and other physical movements. The symptoms can interfere with daily life. You’re more likely to fall, and your physical movements become much more difficult. However, most patients at this stage are still able to maintain independence and need little outside assistance.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Can I Support Someone With Parkinson’s At The Advanced Or Palliative Stage
In the advanced stages of Parkinson’s, your patient’s care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the ‘whole person’ to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinson’s may be supported by a number of professionals, including a Parkinson’s nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinson’s should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the person’s wishes and preferences are for their care in the future. They may include decisions on any treatments the person doesn’t want to have in the future – this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease
Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinson’s disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day – even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
How Can Parkinson’s Affect Someone At The Advanced Or Palliative Stage
Parkinson’s progresses in stages: diagnosis, maintenance, advanced and palliative. Professionals should have talk to people with Parkinson’s about advance care planning in the earlier stages of the disease. This can allow them to express their wishes and preferences for their care in the later stages of the disease and make plans for the future.
Although the condition progresses differently and at a different speed for each person, the advanced stage can potentially cover a long period of time.
Problems that affect someone with advanced Parkinson’s may include:
- medicines being less effective at managing symptoms than before
- having to take lots of medicines to manage symptoms and side effects
- more ‘off’ periods – when the effects of medication are reduced, and people experience movement fluctuations and involuntary movements
- increased mobility problems and falls
- swallowing difficulties
- less control of their Parkinson’s symptoms, which become less predictable
- pain.
Some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection, such as pneumonia. People with Parkinson’s most often die because of an infection or another condition, usually caused by Parkinson’s.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a “last in, first out approach.” 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patient’s medication history should be considered.29
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patient’s handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
Myth 4: Aside From Medication There Isnt Much You Can Do
Fact: This “it is what it is; there’s nothing I can do to help myself” myth is counterproductive. There is a lot you can do — chiefly, keeping as active as you can. A recent study found that patients with Parkinson’s who took part in weekly, hourlong exercise sessions were able to do more in their daily lives than those who did not.
Complications Related To Parkinson’s Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Parkinson’s is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinson’s disease in the United States. During the six-year period, 64% of the participants with Parkinson’s disease passed away.
The risk of death of those with Parkinson’s was then compared to Medicare beneficiaries who did not have Parkinson’s or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinson’s was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinson’s disease was similar to those with hip fracture, Alzheimer’s dementia, or a recent heart attack—although it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
Myth 6: Deep Brain Stimulation Is Experimental Therapy
Fact: Deep brain stimulation, or DBS, is a procedure in which doctors place electrodes in the brain at the point when medications are less effective in masking motor symptoms, such as tremor, stiffness and slowness of movement.
While it may sound frightening and futuristic, it’s been around and successfully used for decades. DBS works very similarly to a pacemaker, except the wire is in the brain, not in the heart. It’s been a standard procedure for the past two decades.
Stage One: Symptoms Affect Only One Side Of Your Body
The initial phase of Parkinson’s disease typically presents with mild symptoms. Some patients will not even detect their symptoms in the earliest phases of this stage. Typical motor symptoms experienced in Stage One include tremors and shaking limbs. Family members and friends may begin to notice other symptoms including tremor, poor posture, and mask face or loss of facial expression.
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Forgetfulness
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. It’s clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
Caring For Your Health With Parkinson’s Disease
In addition to caring for your Parkinson’s health, it is also important to care for your overall health. This means visiting your primary care physician periodically for preventive care like the annual flu shot and cancer screenings—for example, a mammogram for breast cancer screening and a colonoscopy for colon cancer screening.
A primary care physician can also evaluate for risk factors related to heart attacks and strokes, and provide counseling on exercise, smoking, alcohol use, depression, or other mental health concerns. Regular visits to your primary care physician or neurologist will also allow them to catch bacterial infections like urinary tract infections before they get serious.
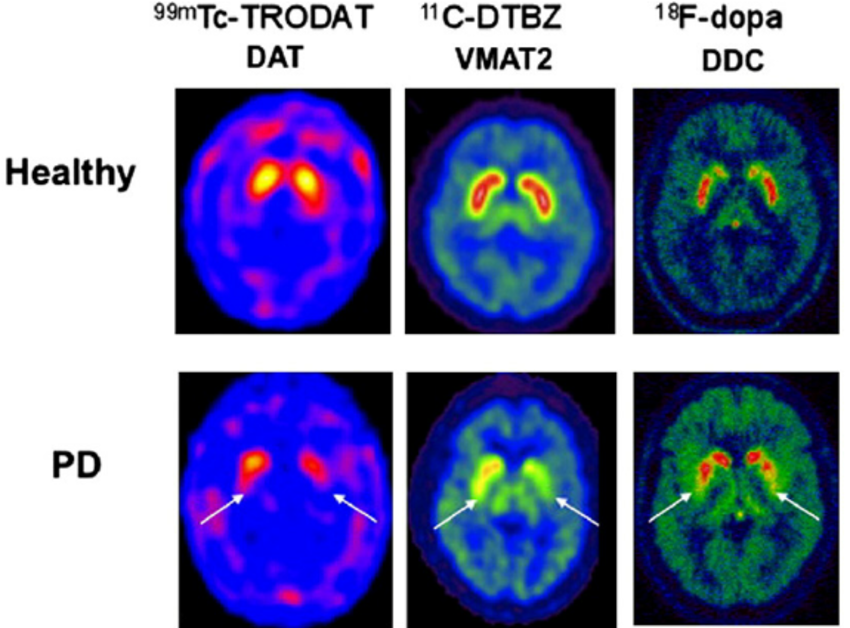
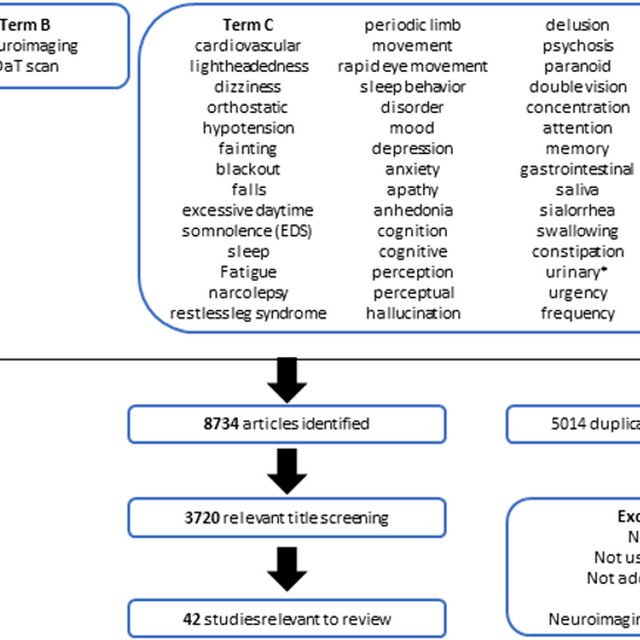
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
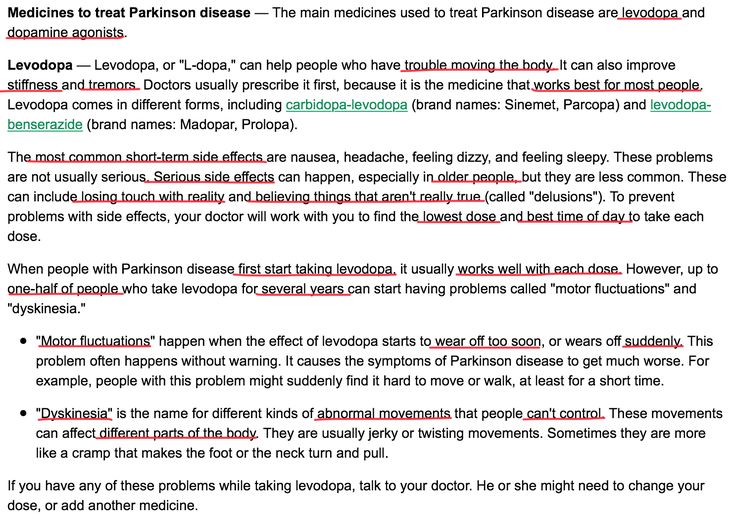
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
How Is Psp Different From Parkinson’s Disease
PSP is often misdiagnosed as Parkinson’s disease, especially early in the disorder, as they share many symptoms, including stiffness, movement difficulties, clumsiness, bradykinesia , and rigidity of muscles. The onset of both diseases is in late middle age. However, PSP progresses more rapidly than Parkinson’s disease.
- People with PSP usually stand exceptionally straight or occasionally tilt their heads backward . This is termed “axial rigidity.” Those with Parkinson’s disease usually bend forward.
- Problems with speech and swallowing are much more common and severe in PSP than in Parkinson’s disease and tend to show up earlier in the disease.
- Eye movements are abnormal in PSP but close to normal in Parkinson’s disease.
- Tremor is rare in PSP but very common in individuals with Parkinson’s disease.
Although individuals with Parkinson’s disease markedly benefit from the drug levodopa, people with PSP respond minimally and only briefly to this drug.
People with PSP show accumulation of the protein tau in affected brain cells, whereas people with Parkinson’s disease show accumulation of a different protein called alpha-synuclein.
Myth 2: Parkinsons Medications Cause Symptoms
Fact: Even though the myth that Parkinson’s disease medicines are toxic and make the condition progress faster was completely debunked, it persists. Levodopa is the main drug therapy for Parkinson’s disease. It’s a potent drug that helps patients with motor symptoms. But many people got the idea that over time, it makes the disease progress faster. The myth was that levodopa is somehow toxic and is somehow making the Parkinson’s progression faster, hurting patients.
This misconception was debunked decades ago with a large clinical trial, where it was found that people exposed to levodopa versus a placebo weren’t worse. In fact, they were better at the end of the study.
It’s true that levodopa isn’t a cure — as yet, there is no cure for Parkinson’s disease — but it’s not toxic.
Parkinsons Disease Is A Progressive Disorder
Parkinson’s Disease is a slowly progressive neurodegenerative disorder that primarily affects movement and, in some cases, cognition. Individuals with PD may have a slightly shorter life span compared to healthy individuals of the same age group. According to the Michael J. Fox Foundation for Parkinson’s Research, patients usually begin developing Parkinson’s symptoms around age 60. Many people with PD live between 10 and 20 years after being diagnosed. However, a patient’s age and general health status factor into the accuracy of this estimate.
While there is no cure for Parkinson’s disease, many patients are only mildly affected and need no treatment for several years after their initial diagnosis. However, PD is both chronic, meaning it persists over a long period of time, and progressive, meaning its symptoms grow worse over time. This progression occurs more quickly in some people than in others.
Pharmaceutical and surgical interventions can help manage some of the symptoms, like bradykinesia , rigidity or tremor , but not much can be done to slow the overall progression of the disease. Over time, shaking, which affects most PD patients, may begin to interfere with daily activities and one’s quality of life.
What Symptoms Can Be Expected In Advanced Pd
- Pain – 86%
- Shortness of breath – 54%
- Problems in swallowing – 40%14
In an analysis of 339 death certificates and medical notes in the UK, pneumonia was found to be a “terminal event in 45%”.13
Caregiver distress with choking and the risk of “choking to death” is also mentioned in a separate study in to experiences regarding all stages of PD.4
In a survey of symptoms and their association with quality of life, in those patients with advanced disease, uncontrolled pain, anxiety and hallucinations were significantly associated with poor quality of life.9
Seizures are also noted in a description of the last phase of Parkinsonian syndromes,15 and in retrospective studies of PD patients’ overall.16,17
These above symptoms often occur on the background of weight loss, pain, and cognitive impairment. It is important therefore to note which medications given at the end of life may exacerbate these symptoms, and which should be considered in anticipation of them.
Myth 1: Parkinsons Is Only A Motor Condition
Fact: While it’s true that Parkinson’s disease symptoms include shaking and tremor, rigid muscles, slowness of movement, and a frozen or “flat” expression, it’s a lot more than that.
Nonmotor symptoms deserve — and are getting — more attention from doctors and researchers. These symptoms include cognitive impairment or dementia , anxiety and depression, fatigue, sleep problems and more.
For some patients, nonmotor symptoms are more disabling than motor symptoms, which are the focus of treatment. Be sure to talk to your doctor about other issues so you can get all of your symptoms addressed.
The Last Year Of Life In Parkinson’s Disease
The study also examined nearly 45,000 hospitalizations in people with terminal Parkinson’s, meaning their end-of-life period.
Of those with terminal PD, the most common reasons for being in the hospital were:
- Infection
- Heart disease
- Lung disease that was not from an infection
Less common causes for hospitalization were problems related to the stomach or intestines, muscles, nervous system, or endocrine system .
It is not surprising that infection was the most common hospitalization before death, as people with Parkinson’s are vulnerable to developing a number of infections as a result of their disease. For example, bladder dysfunction in Parkinson’s increases a person’s risk of developing urinary tract infections, which can become life-threatening if not detected and treated promptly.
In addition, research suggests that aspiration pneumonia is 3.8 times more common in people with Parkinson’s as compared to the general population. It has also been consistently reported to be the main cause of death in people with Parkinson’s.
Aspiration pneumonia results from underlying swallowing difficulties, which leads to stomach contents being inhaled into the lungs. Immobilization and rigidity, which can impair phlegm removal, also contribute to the development of pneumonia in people with Parkinson’s.
Theory Of Pd Progression: Braaks Hypothesis
The current theory is that the earliest signs of Parkinson’s are found in the enteric nervous system, the medulla and the olfactory bulb, which controls sense of smell. Under this theory, Parkinson’s only progresses to the substantia nigra and cortex over time.
This theory is increasingly borne out by evidence that non-motor symptoms, such as a loss of sense of smell , sleep disorders and constipation may precede the motor features of the disease by several years. For this reason, researchers are increasingly focused on these non-motor symptoms to detect PD as early as possible and to look for ways to stop its progression.
Page reviewed by Dr. Ryan Barmore, Movement Disorders Fellow at the University of Florida, a Parkinson’s Foundation Center of Excellence.
*Please note that not all content is available in both languages. If you are interested in receiving Spanish communications, we recommend selecting “both” to stay best informed on the Foundation’s work and the latest in PD news.
Hospice Eligibility For Parkinsons Disease
Due to the progressive nature of Parkinson’s disease, it can be challenging for families to know when their loved one is eligible for the support of hospice care. If a loved one has been diagnosed with six months or less to live or if they have experienced a decline in their ability to move, speak, or participate in the activities of daily living without caregiver assistance, it is time to speak with a hospice professional about next steps.
What Are The Symptoms Of Parkinson Disease
Parkinson disease symptoms usually start out mild, and then progressively get much worse. The first signs are often so subtle that many people don’t seek medical attention at first. These are common symptoms of Parkinson disease:
- Tremors that affect the face and jaw, legs, arms, and hands
- Slow, stiff walking
Surgery For People With Parkinsons Disease
Deep brain stimulation surgery is an option to treat Parkinson’s disease symptoms, but it is not suitable for everyone. There are strict criteria and guidelines on who can be a candidate for surgery, and this is something that only your doctor and you can decide. Surgery may be considered early or late in the progression of Parkinson’s. When performing deep-brain stimulation surgery, the surgeon places an electrode in the part of the brain most effected by Parkinson’s disease. Electrical impulses are introduced to the brain, which has the effect of ‘normalising’ the brain’s electrical activity reducing the symptoms of Parkinson’s disease. The electrical impulse is introduced using a pacemaker-like device called a stimulator. Thalamotomy and pallidotomy are operations where the surgeon makes an incision on part of the brain. These surgeries aim to alleviate some forms of tremor or unusual movement, but they are rarely performed now.
Support For People With Parkinsons Disease
Early access to a multidisciplinary support team is important. These teams may include doctors, physiotherapists, occupational therapists, speech therapists, dietitians, social workers and specialist nurses. Members of the team assess the person with Parkinson’s disease and identify potential difficulties and possible solutions.There are a limited number of multidisciplinary teams in Victoria that specialise in Parkinson’s disease management. But generalist teams are becoming more aware of how to help people with Parkinson’s disease.
How To Manage Symptoms At The End Of Life
At the end of life, good practice is to plan for any potential symptoms that may arise. The most common symptoms anticipated are pain, dyspnoea, nausea and vomiting, agitation, anxiety, delirium and noisy respiratory secretions.18 For patients with PD particular considerations should be given to the more commonly used medicines, specifically anticholinergics and antidopaminergics. These are usually prescribed for treatment of respiratory secretions and nausea and vomiting. Alternatives are available for respiratory secretions, and include glycopyrronium, in preference to hyoscine hydrobromide. Although this is an anticholinergic, only a small proportion crosses the blood brain barrier.
For nausea and vomiting, ondansetron,19 cyclizine, domperidone have all been suggested in PD.20 However, ondansetron has been shown to be inferior to domperidone in the pre-treatment of apomorphine.21 Cyclizine has anticholinergic properties and may exacerbate confusion, especially when comorbid psychosis or cognitive impairment are present. Levomepromazine, although it has antidopaminergic effects, has been shown to be effective for nausea with rotigotine in a case report.22
Agitation, dyspnoea and pain can all be managed with the same anticipatory medications as recommended.20 Specifically relating to PD, several case reports have supported the intraoperative use of midazolam, during sedation, for tremor and dyskinesias,23,24 as well as for agitation at the end of life.20
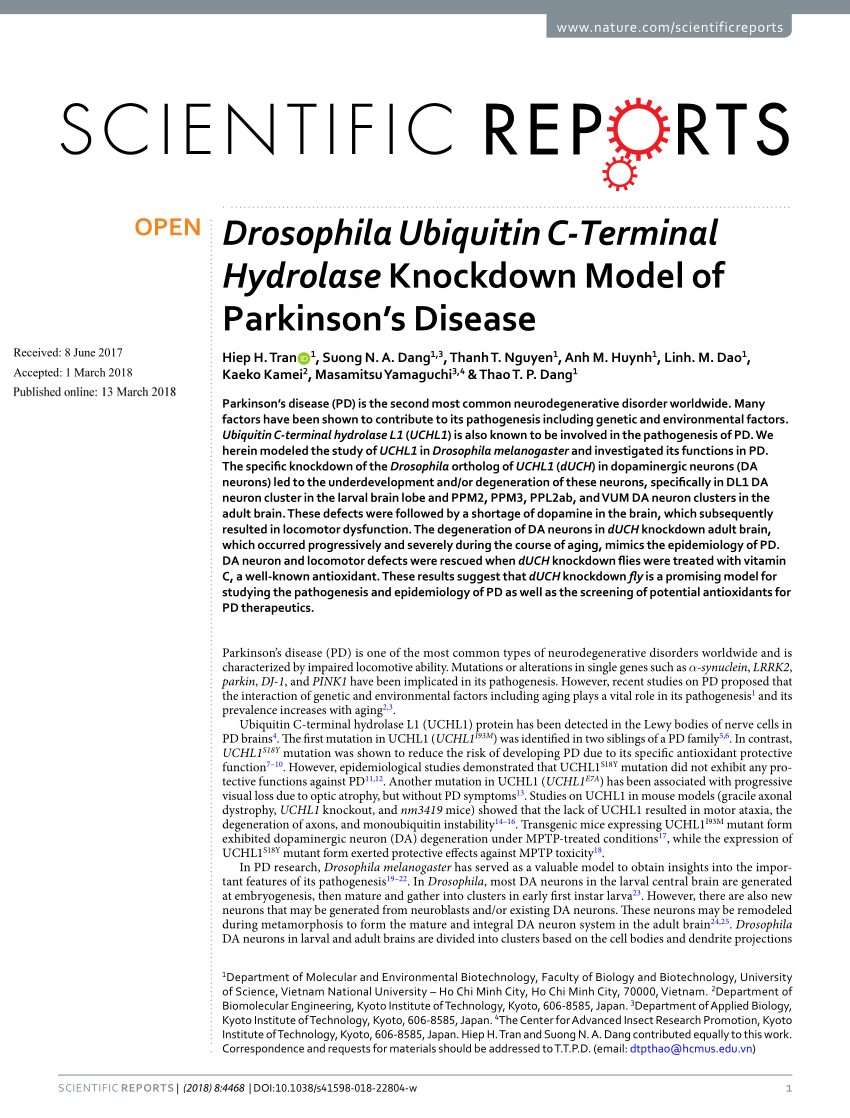
Dysfunctional Protein Clearance Systems
There are two central protein clearance systems within cells responsible for the removal of dysfunctional proteins: the ubiquitin-proteasome system and the autophagy-lysosome pathway. The UPS is primarily responsible for breaking down abnormal proteins, and it does so by “tagging” them with ubiquitin and transporting them to the proteasome for degradation. The autophagy-lysosome pathway is divided into three constituents: macroautophagy, microautophagy, and chaperone-mediated autophagy . Briefly, in macroautophagy, intracellular components, including cytosolic proteins, are engulfed by the autophagosome, which then fuses with the lysosome, leading to the breakdown of its contents. On the other hand, in microautophagy, the lysosome alone engulfs and destroys cytoplasmic components. CMA is a more selective process, whereby molecular chaperones target specific proteins and transport them to the lysosome for degradation . Monomeric ?-synuclein is generally cleared by both the UPS and the autophagy-lysosome pathway , and damage in either of their machineries is implicated in the pathogenesis of PD by contributing to the accumulation of defective proteins, in particular soluble misfolded ?-synuclein .
Unified Parkinsons Disease Rating Scale
The UPDRS contains four parts. The first part assesses intellectual function, mood, and behavior. The second one assesses activities of daily living. The third part assesses one motor function, and the fourth assesses motor complications.
Each part includes scores that altogether rate the severity of the disease. The maximum score is 199, reflecting total disability, whereas a score of zero means no disability.
