When People Talk About Parkinsons They May Mention The Effects It Has On The Substantia Nigra But Did You Know That There Are Other Areas Of The Brain That Are Affected By The Condition
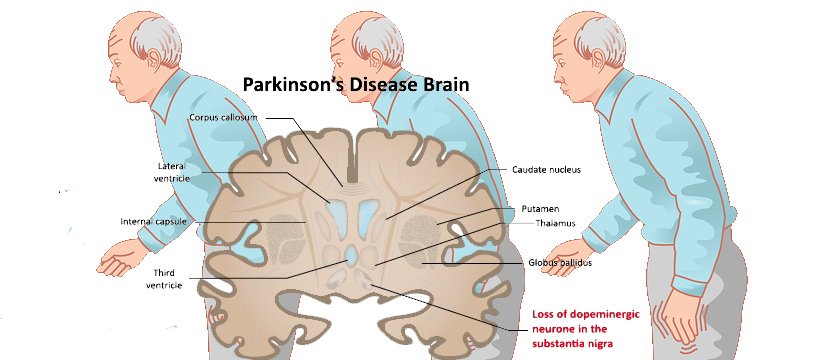
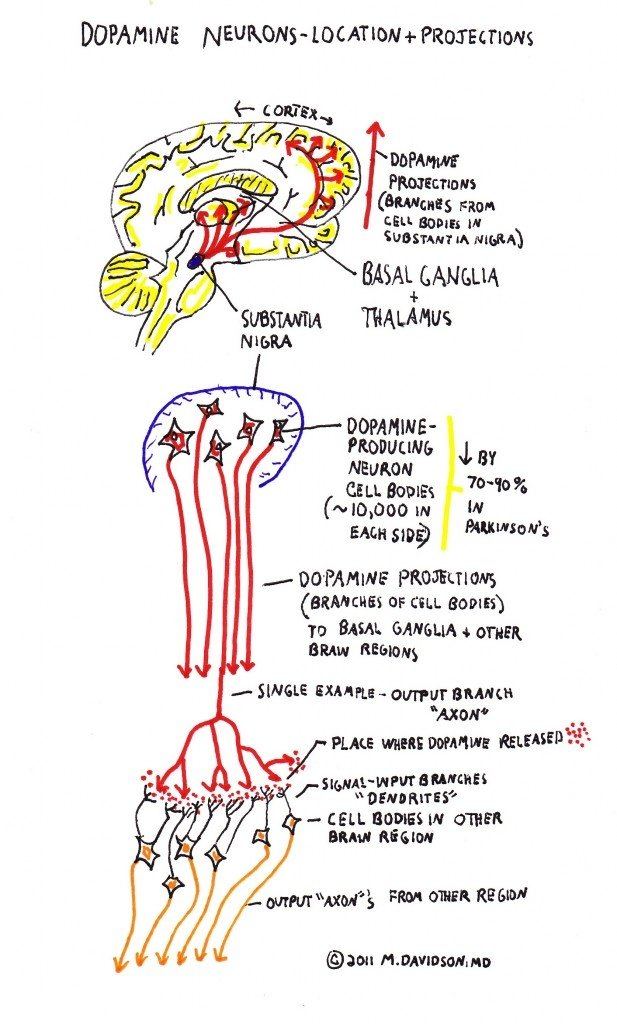
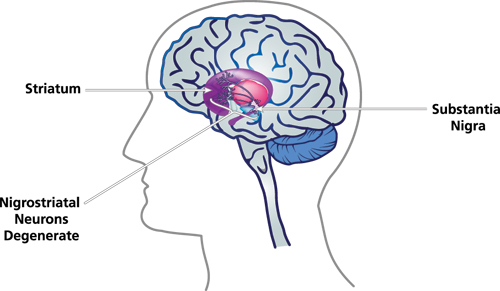
Parkinson’s is a condition that causes the gradual loss of the dopamine-producing brain cells of the substantia nigra — an area of the brain located just above where the spinal cord meets the midbrain. It is these cells that produce and release the neurotransmitter dopamine, which has a key role in turning thought about movement into action.
While this definition of the condition is useful to briefly explain Parkinson’s, the whole story is somewhat more complex. Over the last 30 years, it has become accepted that Parkinson’s also causes a number of non-motor symptoms, such as changes in sleep, smell and even the way we think, which likely involve other areas of the brain.
Now scientists are looking at the broader effects of the condition on the brain in an attempt to better understand why people experience different symptoms. The finding could lead us to new treatments that tackle more than just the motor symptoms of the condition.
Reviewperipheral Nervous System Involvement In Parkinson’s Disease: Evidence And Controversies C.Comiaclicense
A variable degree of peripheral nervous system dysfunction is frequent in Parkinson’s disease patients.
- •
-
One line of evidence supports a direct damage to small nerve fibers, probably triggered by alpha synuclein deposition.
- •
-
A role of prolonged exposition to levodopa and vitamin B deficiency was also documented by independent research groups.
- •
-
In this review we provide an update on the different standpoints and discuss future directions.
Role Of The Peripheral Nervous System In Pd Pathology Diagnosis And Treatment
- 1Department of Neurology, Affiliated Hospital of Nantong University, Nantong, China
- 2Research Center of Clinical Medicine, Affiliated Hospital of Nantong University, Nantong, China
- 3Department of Neurology, Affiliated Hospital of Nantong University, Nantong, China
Studies on Parkinson disease have mostly focused on the central nervous system—specifically, on the loss of mesencephalic dopaminergic neurons and associated motor dysfunction. However, the peripheral nervous system is gaining prominence in PD research, with increasing clinical attention being paid to non-motor symptoms. Researchers found abnormal deposition of ?-synuclein and neuroinflammation in the PNS. Attempts have been made to use these pathological changes during the clinical diagnosis of PD. Animal studies demonstrated that combined transplantation of autologous peripheral nerves and cells with tyrosine hydroxylase activity can reduce dopaminergic neuronal damage, and similar effects were observed in some clinical trials. In this review, we will systematically explain PNS performance in PD pathology and its clinical diagnostic research, describe PNS experimental results and the results of clinical trials, and discuss future directions. The mechanism by which SCs produce such a therapeutic effect and the safety of transplantation therapy are briefly described.
Research Is Underway To Further Understand The Cardiac Effects Of Parkinsons
It is possible to image the sympathetic nervous system of the human heart by injecting a radioactive tracer, meta-iodo-benzyl-guanidine, . Development of this technique, known as MIBG cardiac imaging, holds much promise as a test to confirm the diagnosis of PD , to identify those who are at risk of developing PD in the future, and to distinguish PD from related disorders. MIBG cardiac imaging is still considered an experimental procedure for detection of PD and is not yet in use as a clinical tool for this purpose.
A recent research study was conducted in monkeys in which the destruction of the sympathetic nerves of the heart was chemically induced to mimic the changes that are seen in PD. The cardiac system was then imaged using a number of new-generation radioactive tracers, which bind to markers of inflammation and oxidative stress. This model system may help to shed light on the molecular changes that accompany the loss of the sympathetic nerves of the heart and can also be used to track the response of the cardiac system to therapeutic agents.
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
Study Finds Widespread Sympathetic Nerve Damage In Parkinson’s Disease
- Date:
- NIH/National Institute Of Neurological Disorders And Stroke
- Summary:
- For years, researchers have known that the symptoms of Parkinson’s disease result from damage to a specific region of the brain. A new study shows that the disease also causes widespread damage to the sympathetic nervous system, which controls blood pressure, pulse rate, perspiration, and many other automatic responses to stress. The findings help explain the blood pressure regulation problems commonly found in PD and may lead to new treatments for the disease.
Many people with PD develop a problem called orthostatic hypotension , in which blood pressure falls suddenly when a person stands up. This condition can lead to dizziness, lightheadedness, and fainting. OH increases the risk of falls and other types of accidents, which can be disabling or even life-threatening. Patients with PD frequently have other symptoms of sympathetic nervous system failure, including intolerance to heat or cold and sexual dysfunction. However, the underlying cause of these problems has been unclear.
The NINDS is a component of the National Institutes of Health in Bethesda, Maryland, and is the nation’s primary supporter of biomedical research on the brain and nervous system.
Story Source:
The Heart Of The Matter: Cardiovascular Effects Of Parkinsons Disease
It has long been understood that Parkinson’s disease does not just cause movement symptoms, but also causes a litany of non-motor symptoms with effects throughout the body. One of the organ systems that is affected is the cardiac system, encompassing the heart, as well as the major and minor blood vessels. I received this topic as a suggestion from a blog reader and we will be discussing this important issue today. Please feel free to .
Gene Therapy : A Method Of Manipulating Cells At The Molecular Level
of preventing or altering rare genetic disease states. Viruses have the natural ability to deliver genetic material to cells, which makes them excellent vectors for gene delivery . Lentivirus, Herpes Simplex Virus, Adenovirus and Adeno-Associated viruses are among the most prominently used vectors for gene delivery to the therapeutic target.While, gene therapy is a promising treatment option for a range of diseases, there are still a number of unwarranted
The Use Of Nano Structured Neural Scaffolds For Neural Regeneration
Topical ReviewUse of nano-structured neural scaffolds for neural regeneration in case of Parkinson’s DiseaseABSTRACTParkinson’s Disease affects a large percentage of people all over the world. Currently, an effective strategy for regeneration of neurons that are lost in PD does not exist; however, nanotechnology has offered new avenues in the field of neural tissue regeneration. Nanostructured scaffolds have been shown to have the ability to promote neuronal growth and their excellent biomimetic
Rebuilding The Nervous System And Regenerating Neural Connections
Now for the very good news. Since we now understand that PD is principally a problem with the Nervous System, it is entirely possible that we can pro-actively prevent further degeneration, and even regain what we’ve already lost, because Vagal Tone can always be improved, neurons regenerated, neural pathways re-written, and senses retrained.
I would go much further than this, as in pursuing these solution strategies, I can honestly say I am now, in many ways, better than I ever was before PD. Indeed, when I am the “on” state, I can actually move in ways I never could before, I am much more flexible and fluid, and have increased ranges of motion. I also have much better awareness of my own body and extremities and balance sense , much better understanding of what my body is telling me , much better eyesight, including peripherial vision and appreciation for color, much better listening skills, including a profoundly increased appreciation for the nuances in music, and so forth.
Below are just a few things we can all do to help ourselves.
Start stimulating the Smart VN and Cranial Nerves on a daily basis, in order to re-strenthen Vagal Tone. I am collating simple and quick methods for doing this here: THE VAGUS NERVE AND PARKINSON’S DISEASE and THE CRANIAL NERVES AND PARKINSON’S DISEASE.
Use vibration therapies to mindfully stimulate the hands and feet, in order to rebuild awareness and sense of the extremities.
Practice making eye contact with other people.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Parkinson’s Disease Brain Vs Normal Brain: What’s Different
It’s not yet possible to spot the difference between a brain with Parkinson’s and a normal, “healthy” brain on an MRI scan. However, since Lewy bodies were first found in the substantia nigra in 1927, doctors have known they are a feature of Parkinson’s disease. The presence of these Lewy bodies is thought to be what separates people with Parkinson’s disease from the general population. However, Lewy bodies can only be diagnosed with certainty during a brain autopsy after death.
Understanding The Neurologic Control Of The Cardiac System
Before we explore this issue, let’s first learn a bit about the autonomic nervous system and about the cardiac system’s place within it. The ANS is part of the peripheral nervous system, a network of nerves throughout the body. The ANS exerts control over functions that are not under conscious direction such as respiration, heart function, blood pressure, digestion, urination, sexual function, pupillary response, and much more. The ANS is further subdivided into the parasympathetic nervous system and the sympathetic nervous system. Both the parasympathetic and sympathetic nervous systems regulate most major organs. Often, they have opposite effects, with the sympathetic nervous system activating a system and the parasympathetic system calming it down.
One of the systems controlled by the ANS is cardiac regulation. Blood pressure sensors, known as baroreceptors, reside in the heart as well as in the carotid artery, the major artery in the neck. If the baroreceptors sense a change in the blood pressure, a signal is sent to particular areas in the brain. From there, the autonomic nervous system sends signals to the heart to control heart rate and cardiac output. Signals are also sent to the blood vessels to change the size of their diameter, thereby regulating blood pressure.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
How Does Neuron Dysfunction Affect Parkinsons Patients
Parkinson’s disease is a disorder that affects the brain and the nervous system of its sufferers.
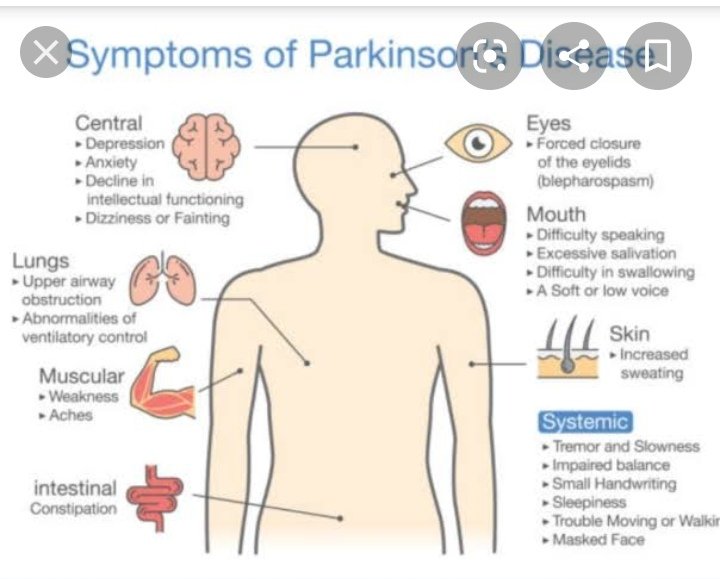
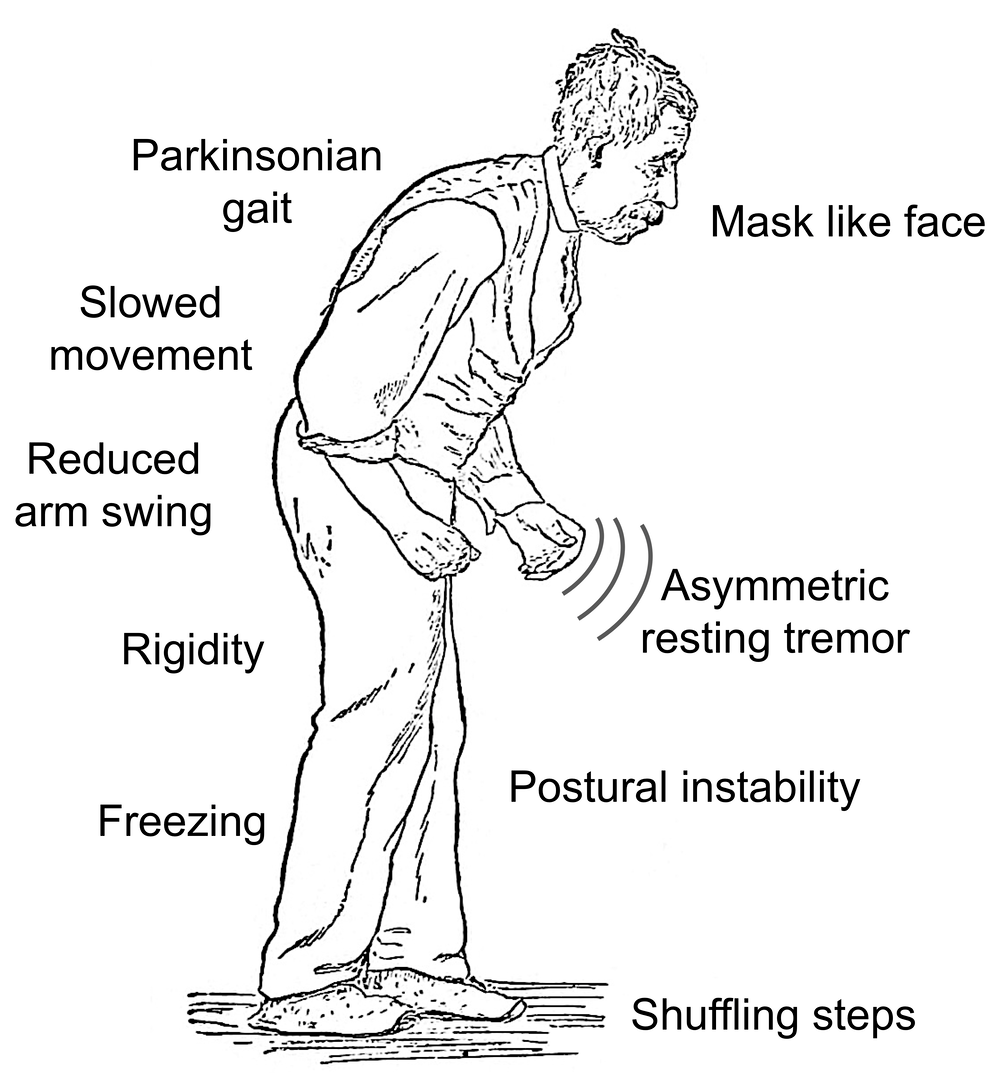
Over time, neurons in the regions of the brain that control movement degenerate, leading to a loss of motor control and a host of primary and secondary symptoms. People with Parkinson’s disease often experience tremors and shaking, a slow, shuffling walk, and an occasional sensation of being frozen in place, incapable of voluntary movement. Parkinson’s sufferers also routinely experience other, more subtle, motor symptoms, such as very small, cramped handwriting, a rigid, mask-like facial expression, and difficulty controlling the tone and volume of their voice.
These symptoms are caused by dysfunction in the neurons that control movement. These densely packed nerve endings in the brain and throughout the body send and receive chemical signals relating to movement. In Parkinson’s, these neurons lose their ability to produce dopamine, a chemical messenger essential to transmitting these signals. This leads to random firing of the neurons and compromised movement. Eventually, Parkinson’s often effects other body systems, causing digestive, urinary, skin, and psychiatric problems.
Edison Home Health Care is happy to advise and assist you or any loved one seeking a home attendant for Parkinson’s related issues. Give us a call at 888-311-1142, or fill out a contact form and we will respond shortly.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Evidence For Sc Involvement In Pd From Animal Models
Although the relationship between pathologic changes and PD progression is not fully understood, the therapeutic potential of SCs for PD has been widely investigated in animal experiments based on their neuroregenerative capacity in the PNS . In the 1980s, Aguayo and colleagues demonstrated that PNS grafts could support CNS neuron survival following injury and guide axonal regeneration in mice. Transplanted dopaminergic neurons survived and extended fibers into a peripheral nerve bridge formed by homotopic sciatic nerve covering the skull that connected the midbrain tissue graft over the superior colliculus and the caudate-putamen nucleus .
Table 2. Application of PNS in animal experiments.
Schizophreni Symptoms And Devastating Mental Disease
the two Greek words “skhizo” and “phren” . The term was first coined in 1908 by a Swiss psychiatrist Eugen Bleuler. Schizophrenia is probably the most tragic, enigmatic and devastating mental disease that physiatric APN treat in their practices. Schizophrenia is a mental disease that is diagnosed in the early years of the patient that is inflicted by it. One of the many puzzling characteristics of schizophrenia is that men generally suffer from the mental illness more severely than
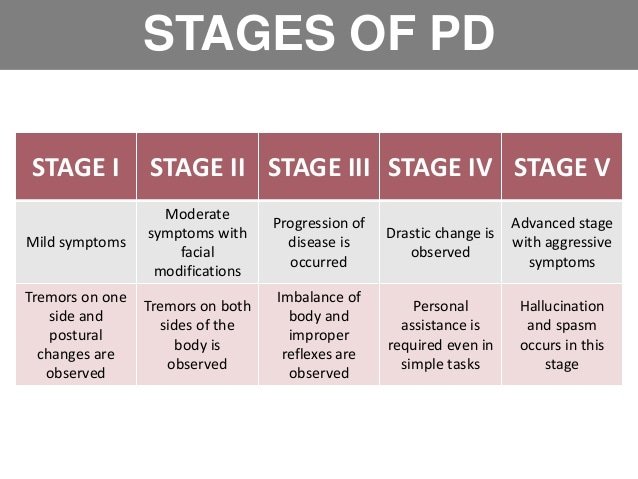
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Sc Mechanisms For Neuronal Repair And Regeneration
Schwann cells are a type of peripheral glial cell originating from the neural crest that initially differentiate into SC precursor cells, then immature SCs, and finally into myelinating and non-myelinating cells that retain the ability to dedifferentiate to an immature SC state . SCs secrete a basal lamina composed of growth-promoting laminin, type IV collagen, and heparin sulfate proteoglycans , which are critical for the SC myelinating function. More importantly, SCs proliferating after nerve injury may form a channel that promotes axonal regeneration along residual SC structures known as Büngner bands . In contrast, oligodendrocytes in the CNS do not secrete basal lamina, so the healthy CNS is free of these basal lamina components except at the pial surface and sites of contact between astrocytes and blood vessels . SC maturation is accompanied by the establishment of autocrine circuits involving platelet-derived growth factor, insulin-like growth factor-1, and neurotrophin-3 that allow SCs to survive after nerve injury and promote peripheral nerve regeneration . Up to 30 or 40% of oligodendrocytes may be lost following CNS injury, and those that survive may be unable to support neuroregeneration . SC autocrine and cytokine secretion functions are not limited to the PNS, as demonstrated in animal models and clinical trials of SC transplantation into the brain.
Vagus Nerve Branch Competition And Contradiction
The concept of competition between Sympathetic and Para-Sympathetic Nervous Systems is well known, as is the VN’s ability to inhibit Sympathetic influences, allowing us to discharge from excited or stressed states.
However, there may also be a different type of competition, in which the two Vagal branches convey contradictory information to the target organs. Both branches of the VN are capable of regulating heart beat rate, for example, via signals they send to specialized muscle tissue in the heart.
This competition between the two branches readily explains many medical issues when the Smart VN becomes very weak . Its regulation of the heart may then be easily inhibited, resulting in sudden loss of control. If there is a surge of Vegetative VN activity in response to this withdrawal of the Smart VN, the consequence is a rapid slowing of the heart rate, from which it might not be able to recover, and the heart and brain being starved of oxygen. Examples of this occurring include massive bradycardia in hypoxic babies and sudden death of athletes following exercise.
Similarly, the breathing rate in people with a weak Smart VN system may be overly prone to the influences of the Vegetative VN, and sudden changes from Smart to Vegetative VN control can cause asthma attacks.
The Complete Explanation For Parkinson’s Disease
Notwithstanding the types of sudden onset PD caused by blows to the head or acute chemical poisoning, we now have a complete, simple and elegant framework of understanding of “Ideopathic” Parkinson’s Disease, which is readily explained as follows.
With the weakening of the Smart VN and associated Cranial Nerves, go all their functions outlined previously, leading, precisely, to all the well known major non-motor symptoms of Parkinson’s Disease. Facial expressiveness is lost and the face becomes a blank mask. Use of the larynx and muscles in the throat are lost, causing the problems with speech and vocalizations, swallowing, chewing and saliva control. The ability to rotate and tilt the head is lost and the neck becomes extremely stiff and painful. The ability to raise the arms is lost and shoulders become painful and frozen. The sense of balance provided by the ear is lost, causing falls. The ability to experience positive emotional states, and to read these in the faces of others, is lost and anti-socialness increases, leading to feelings of isolation.
As the Freeze response of the Vegetative VN becomes more easily excited, its other role in regulating rest and digest function is inhibited, resulting in the appearance of the gastric problems associated with PD , together with imbalances in the gut microbiome.
If these negative feedback cycles are not interrupted, these vicious circles lead to the apparently degenerative nature of Parkinson’s Disease.
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Forgetfulness
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. It’s clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
The Use Of Levodopa And Peripheral Neuropathy
There are reports in the literature that levodopa use may increase the risk of peripheral neuropathy, although other studies suggest that this is not the case. There are studies that demonstrate for example, that cumulative Levodopa exposure correlates to prevalence of PN in people with PD. Other studies however, demonstrate no difference in the prevalence of PN whether the person was treated with Levodopa or not, suggesting that Levodopa treatment does not play a role in development of PN.
Another area of research that emerges from the literature is the potential role of Vitamin B12 deficiency in the development of PN in those with PD. Some studies suggest that Vitamin B12 deficiency is a more common cause of PN among those with PD than those with PN who do not have PD.
There is also research that suggests that levodopa treatment may contribute to PN through impairment of Vitamin B12 metabolism, leading to Vitamin B12 deficiency. Taking COMT inhibitors such as Entacapone may protect against this complication.
Regardless, if PN is diagnosed in anyone, whether they have PD or not, and whether they take Levodopa or not, Vitamin B12 and various other markers of Vitamin B12 metabolism should be tested. If Vitamin B12 levels are low or even low-normal, a person should take Vitamin B12 supplementation, which may help with the symptoms of PN. Other causes of PN, many of which can be checked with various blood tests, should be investigated as well.
How Does Parkinson Affect The Nervous System What Is Parkinson’s?Parkinson’s Effect On The Nervous System And Dopamine.The Two Types Of Parkinson’s Related To The Nervous Systemdistinct subtypesAutonomic Nervous System And Parkinson’s
Autonomic dysfunctionHow To Keep Your Nervous System Healthy?healthyHere are some important recommendations:
What Are The Symptoms Of Parkinson’s Disease
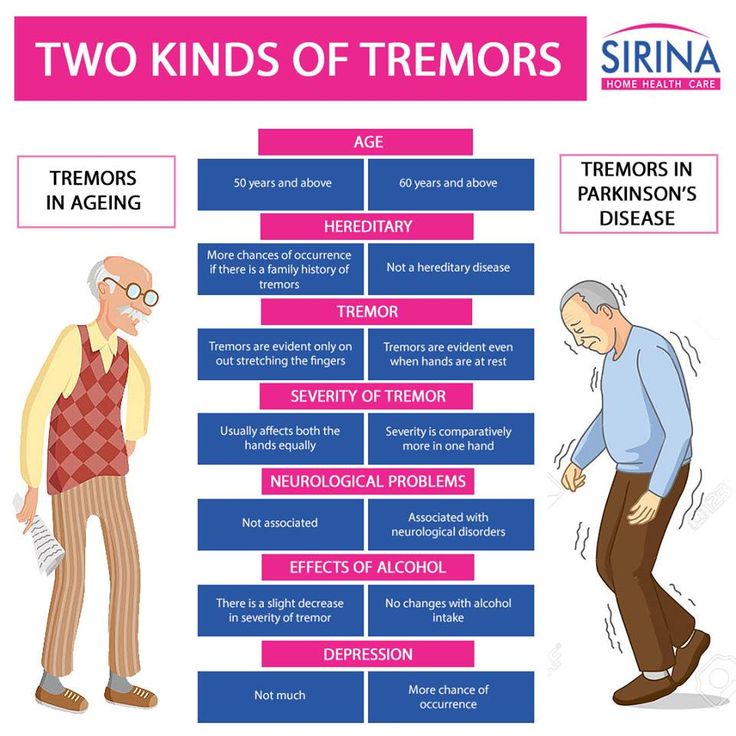
The symptoms of Parkinson’s disease include tremors or trembling ; difficulty maintaining balance and coordination; trouble standing or walking; stiffness; and general slowness.
Over time, a person with Parkinson’s may have trouble smiling, talking, or swallowing. Their faces may appear flat and without expression, but people with Parkinson’s continue to have feelings — even though their faces don’t always show it. Sometimes people with the disease can have trouble with thinking and remembering too.
Because of problems with balance, some people with Parkinson’s fall down a lot, which can result in broken bones. Some people with Parkinson’s may also feel sad or depressed and lose interest in the things they used to do.
The symptoms of Parkinson’s disease appear gradually and get worse over time. But because Parkinson’s disease usually develops slowly, most people who have it can live a long and relatively healthy life.
Peripheral Neuropathy And Parkinsons Disease
A number of studies have tried to determine if PN is more common among people with PD as opposed to people without PD. PN is a relatively common condition in the general population, which makes it difficult to ascertain whether or not it is even more common among people with PD.
The available studies have varying results and are difficult to compare with each other as they:
- Include different types of populations of people with PD
- Assess peripheral neuropathy differently
- Assess for causes of peripheral neuropathy differently
A recent review looked at all the available data and determined that large fiber neuropathy was present in 16% of patients with PD, about double the prevalence of this condition in the general population. Skin biopsy-proven small fiber neuropathy was present in over 50% of people with PD, although this result was based on a small sample of patients.
