Tom Thought That Because Some Pink Tablets Relieved His Symptoms This Meant He Was Ok He Didn’t

I first suspected there was something wrong when I was travelling and I was writing a postcard to a friend of mine in, in Australia whose name is Anthony Diecopolis. And, and I got to the Anthony Diec and I couldn’t finish the opolis. And it’s very strange my hand had sort of gone into a sort of spasm and it just wouldn’t, wouldn’t finish writing the, the, the word. And so that’s a bit strange.
And so I went when, when I got I, I went to the doctor and said, “What on earth’s going on?” And I had since then I’d also developed this slight tremor in my right hand. He said, “Well it’s probably, Essential Tremor or trapped nerve or something like that”. And anyway, then it got a bit worse and then I was, I was recommended to go to a neurologist. And the neurologist had a look at me and gave me some pills. And he said, “Come back and tell me if these work”.
This is about, about sort of, nine months after my, my not being able to finish the, the postcard. And, and he said, “Take these pills”. And the pills worked. Magically the tremors stopped and I thought this is wonderful. And so I went back to the neurologist and I said, “Yes everything’s fine now. The pills have, the pills have worked.” And far from looking happy about this he looked rather, rather grave and he said, “I think you’d better go to another neurologist.”
Currently There Is No Cure And No Definitive Test For Parkinson’s Diagnosis Can Take Years
A simple skin-swab test could be used to help diagnose Parkinson’s disease, a degenerative brain condition if UK scientists are to go by. As per a latest study, it is possible to identify Parkinson’s based on the compounds found on one’s skin. The University of Manchester scientists have developed a technique that quickly detects tell-tale compounds in sebum – the oily substance that protects the skin – and identifies changes in people with the disease.
Currently, there is no cure and no definitive test for Parkinson’s. Also, diagnosis can take years.
Sebum, which is rich in lipid-like molecules, is one of the lesser-studied biological fluids in the diagnosis of the condition. People with Parkinson’s tend to produce more sebum than normal – which is called seborrhoea.
Researchers discovered this after a woman amazed doctors with her ability to detect Parkinson’s through smell. Retired nurse Joy Milne, 68, from Perth, noticed the “musky” smell on her husband, Les, years before his Parkinson’s diagnosis.
The research team used a mass-spectrometry machine to detect the compounds, and now has data from 500 people, showing the skin test can correctly distinguish those with Parkinson’s more than eight out of every 10 times.
The research, funded by charities Parkinson’s UK and Michael J Fox Foundation as well as The University of Manchester Innovation Factory, analysed the samples taken from the people’s upper backs.
New Imaging Test Gives Physicians Better Tool To Diagnose Parkinson’s Disease
- Date:
- Northwestern Memorial Hospital
- Summary:
- Physicians now have an objective test to evaluate patients for Parkinsonian syndromes, such as Parkinson’s disease. DaTscan™ is the only FDA-approved imaging agent for assessment of movement disorders. Until now, there were no definitive tests to identify the disease, forcing physicians to rely on clinical examinations to make a diagnosis. This technology allows doctors to differentiate Parkinson’s from other movement disorders.
Thanks to a new diagnostic imaging technique, physicians now have an objective test to evaluate patients for Parkinsonian syndromes, such as Parkinson’s disease. Northwestern Memorial Hospital is among the first institutions in the country to offer DaTscan™, the only FDA-approved imaging agent for assessment of movement disorders. Until now, there were no definitive tests to identify the disease, forcing physicians to rely on clinical examinations to make a diagnosis. This technology allows doctors to differentiate Parkinson’s from other movement disorders.
An accurate clinical diagnosis for patients with neurodegenerative movement disorders, such as Parkinson’s, can take up to six years. While symptoms often mimic Parkinson’s, other movement disorders, such as essential tremor, occur in different areas of the brain and do not involve the dopamine system.
Story Source:
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Quarter Of Parkinson’s Sufferers Were Wrongly Diagnosed Says Charity

Poll of more than 2,000 people found 26% of respondents were told they had something else
More than a quarter of people with Parkinson’s disease were initially misdiagnosed, new research has found.
The poll of more than 2,000 people found 26% were first told they had something else, while 21% saw their GP three or more times before being referred to a specialist.
Of those who were misdiagnosed, 48% were given treatment for their nonexistent condition, with 36% receiving medication, 6% undergoing operations or procedures and a further 6% given both medication and operations or procedures.
Of those who received unnecessary treatment, 34% said their health had got worse as a result.
The poll, for the charity Parkinson’s UK, also found that women were more likely to be misdiagnosed than men, and errors were most common in people aged 51 to 60.
Katie Goates of Parkinson’s UK said: “Parkinson’s is an incredibly complex condition with more than 40 symptoms, and it affects everyone differently.
“One of the biggest challenges for Parkinson’s research is that there is no definitive test for Parkinson’s, and as a result we’ve heard of people being misdiagnosed with anything from a frozen shoulder or anxiety to a stroke.
“Our survey has shown that because of this, people are being left in limbo and seeing their health deteriorate, which is unacceptable.
About 145,000 people in the UK are diagnosed with Parkinson’s every year.
Signs of Parkinson’s can include:
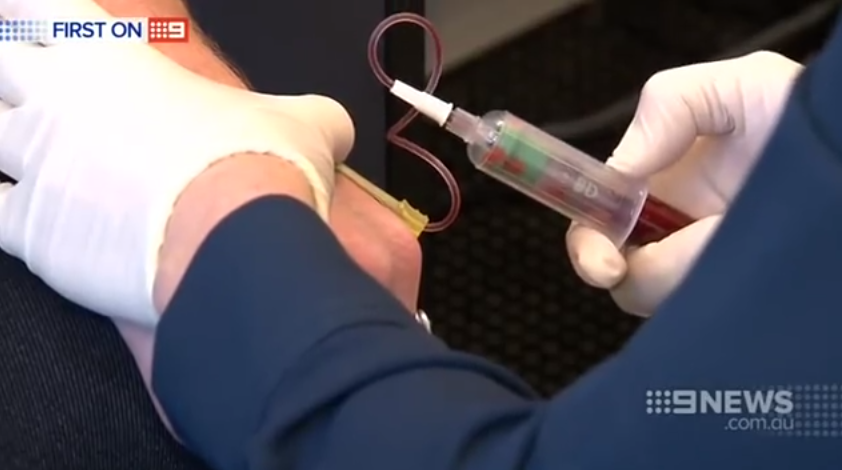
Blood Test May Help Distinguish Parkinsons From Similar Diseases
Researchers have found that people with Parkinson’s disease have lower levels of a certain protein in their blood than people with similar diseases. The results suggest that testing for the protein might help doctors to accurately differentiate between PD and similar diseases early on. The study appears in the February 8 online edition of Neurology.
Because there are no definitive diagnostic tests for Parkinson’s, the diagnosis can be unclear especially early on in the disease. When diagnosis is uncertain, some people may be diagnosed with “parkinsonism,” which refers to a category of diseases, including Parkinson’s, that cause slowness of movement, stiffness and rest tremor. Other diseases in the category include multiple system atrophy , progressive supranuclear palsy and corticobasal degeneration .
Earlier studies found that a spinal fluid test may help distinguish PD from these other diseases, but this test is difficult to do during a routine visit to the doctor.
Results
- Blood levels of NfL protein were generally lower in people with PD and in healthy individuals than in people with other Parkinsonian disorders.
- This result held both for those recently diagnosed and those who had been living with their disease for four to six years.
- The test for NfL could not distinguish between MSA, PSP and CBD.
What Does It Mean?
References
Hansson O, Janelidze S, Hall S, et al. . Blood-Based NfL: A Biomarker for Differential Diagnosis of Parkinsonian Disorder. Neurology 88: 1-8
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Getting Closer To A Definitive Biomarker For Parkinsons Disease
Parkinson’s disease is a devastating, incurable, progressive and degenerative neurological disease that affects movement. There are no biomarkers available and it is diagnosed by symptomology alone. Unfortunately, the symptoms can be similar to many other neurological diseases. This often leads to misdiagnoses resulting in delayed treatment. Currently, definitive diagnosis can only be made at autopsy. A new skin test has been developed that may be able to diagnose Parkinson’s in living patients and at an earlier time in the disease.
The development and use of biomarkers comes with numerous ethical and legal concerns. How do we determine disease and disability? Could biomarkers exacerbate the disparities between diseases that have objective findings and those that do not, making it more difficult for physicians to recognize a condition even in the absence of a marker? Additionally, we should be concerned about who has access to biomarker information and how that information might be misused.
Further studies will be needed to determine if a-synuclein seeding activity can be detected in skin before clinical signs develop in Parkinson’s disease. This possibility is supported by findings reported by Wang et al. that skin prion activity is detectable not only in all patients with Creutzfeldt-Jakob disease but also far in advance of neuronal damage and clinical signs of prion disease in rodents.
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons

In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Global Problem: Lack Of Diagnosis Negates Treatment Impact
Parkinson’s disease affects 127,000 people in the UK and 7.5 million worldwide, leaving many patients struggling to walk, speak and sleep.
The lack of a definitive test for Parkinson’s means that, typically, too many neurons in the brain are lost irretrievably by the time of diagnosis, making treatment difficult and a cure impossible.
A Simple Skin Test That Could Diagnose Parkinsons Disease Research2013-2015 Research ProjectsDr. Drew Kern
Alpha-synuclein deposition in skin of patients with Parkinson’s disease, multiple systems atrophy and progressive supranuclear palsy
“Identifying patients with Parkinson’s disease early is important because we hope to develop therapies in the future that will halt the progressive cell loss,” says Kern.
Currently, the only way to diagnose Parkinson’s is through a clinical evaluation by a doctor experienced in treating movement disorders. But even experienced clinicians can’t distinguish between Parkinson’s and other diseases that share similar symptoms. A definitive test would prevent misdiagnoses that sometimes occur, such as when people with Progressive Supranuclear Palsy are told they have Parkinson’s. Although the symptoms are initially similar, people with PSP typically die seven years into the disease. Parkinson’s disease progresses much more slowly.
Kern, who is a neurologist as well as a neuroscientist, is spending two years seeing patients as a clinical fellow at Toronto Western Hospital’s Movement Disorders Program under the mentorship of Dr. Anthony Lang. He’s also researching skin biopsies as a potential biomarker to identify misshapen proteins associated with Parkinson’s disease, such as alpha-synuclein and tau.
“The emotional component of this is very satisfying, when you can help,” says Kern.
Search
Methodological Limitations Of The Diagnostic Studies
When interpreting the literature about PD diagnosis, the following methodological issues should be considered:
- lack of long-term prospective clinical and pathological as a reference standard
- lack of operational definitions such as defining specialists or clinical diagnostic criteria
- unclear whether investigators were blinded to initial diagnosis
- sample sizes necessarily limited by the number of cases available with neuropathological outcomes
- PD trial age groups are often young as studies were performed by neurologists who see a younger population of people with PD
- most studies included people with established disease lasting some years
- varying geographical locations
- some studies are in specialised units and may not reflect the diagnostic accuracy of other units in the UK
- exclusion of some studies using magnetic resonance volumetry and magnetic resonance spectroscopy as they lacked appropriate population, intervention and outcome criteria
- lack of statistical details of diagnostic accuracy such as sensitivity, specificity and positive predictive values
- lack of economic evaluations of SPECT.
Whats The Outlook For People With Parkinsons Plus
Although there currently isn’t a treatment to halt the progression of Parkinson’s plus syndrome, there are treatments that can help you manage your symptoms and improve your quality of life.
The exact outlook for Parkinson’s plus syndrome depends on the person and the specific condition they have. Someone who is otherwise healthy when they’re diagnosed will typically have a longer life expectancy than someone who is already facing other health conditions when they’re diagnosed. Your doctor will monitor your condition over time and can let you know how it’s progressing.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Diagnosis Of Parkinson Disease: Motor Symptoms
The clinical diagnosis of Parkinson’s disease is based on the presence of characteristic motor symptoms: bradykinesia, rigidity, postural instability, and resting tremor but neuropathology is still considered the gold standard for definite diagnosis. Differentiating PD from other movement disorders can be challenging throughout the disease course, because signs and symptoms often overlap. Indeed, neuropathology studies reveal that clinical diagnosis of PD can be confirmed with an accuracy of about 75%. Good response to levodopa is often used to support the diagnosis of PD. However, cases of pathologically proven PD with poor response to levodopa have also been reported.
Misdiagnosis of PD can occur for several reasons. In a community-based study of patients taking antiparkinsonian medication, the most common misdiagnosis were essential tremor, Alzheimer’s disease, and vascular parkinsonism. In addition, many of the prominent features of PD may also occur as a result of normal aging or from comorbid and multifactorial medical conditions .
Katarzyna Kaczy?ska, Kryspin Andrzejewski, inGenetics, Neurology, Behavior, and Diet in Parkinson’s Disease, 2020
How Do You Know You Have Parkinsons Disease
There is no definitive way to diagnose Parkinson’s disease. Your doctor will ask questions about the onset of your symptoms and assess your movement to make referrals to specialists who can make a formal diagnosis.
You can expect to see a neurologist who can complete a neurologic examination. This may include brain imaging, an MRI, or a PET scan to see activity in the area of the brain typically affected by Parkinson’s disease.
Your doctor may also refer you to a movement disorder specialist. Seeing subspecialists is very important to avoid being misdiagnosed. Highly trained specialists can provide their expertise in specific areas of medicine where a precise diagnosis isn’t possible from blood work or another definitive test.
Single Photon Emission Computed Tomography

In single photon emission computed tomography , a gamma ray-emitting radioactive isotope is tagged to a molecule of interest , which is given to the person with PD by intravenous injection. The labelled cocaine derivatives 123I-?-CIT and 123I-FP-CIT tropane) have most commonly been used, although only the latter is licensed in the UK. These label the presynaptic dopamine re-uptake site and thus the presynaptic neurone, which can be visualised in two-dimensional images. These demonstrate normal uptake in the caudate and putamen in controls and in people with essential tremor, neuroleptic-induced parkinsonism or psychogenic parkinsonism, but reduced uptake in those with PD, PD with dementia, MSA or PSP.
How useful is SPECT in discriminating PD from alternative conditions?
Molecular Imaging In Parkinson’s Disease
The diagnosis of PD relies on the clinical manifestation of cardinal motor symptoms, bradykinesia, and tremor at rest or rigidity . A positive response to dopaminergic drugs is supportive of the diagnosis. Single photon emission computed tomography or PET ligands that are specific for dopamine transporters indirectly enable the quantification of the deficit of dopaminergic nigrostriatal projections and can provide further support of diagnosis . Deficiencies of monoamine synthesis can be measured with dihydroxyphenylalanine which is a substrate for the enzyme aromatic amino acid decarboxylase in all monoaminergic neurons including noradrenergic neurons .
The role of deficits of noradrenaline in motor and non-motor symptoms is not clear and research on the noradrenergic system in PD patients has been hindered by lack of specific methods to visualize the noradrenergic neurons and projections in vivo. We have recently carried out PET studies to investigate the role of noradrenaline in non-motor symptoms in PD patients and these studies will form the basis of discussions in the paragraphs below.
Paul Johns BSc BM MSc FRCPath, inClinical Neuroscience, 2014
New Diagnostic Standards For Parkinsons
Until recently, the gold-standard checklist for diagnosis came from the U.K.’s Parkinson’s Disease Society Brain Bank. It was a checklist that doctors followed to determine if the symptoms they saw fit the disease. But that’s now considered outdated. Recently, new criteria from the International Parkinson and Movement Disorder Society have come into use. This list reflects the most current understanding of the condition. It allows doctors to reach a more accurate diagnosis so patients can begin treatment at earlier stages.
What Tests Diagnose Parkinson’s Disease
There currently are no tests that can definitively diagnose Parkinson’s Disease. A diagnosis is based on the clinical findings of your physician in combination with your report on the symptoms you are experiencing.??
In situations where an older person presents with the typical features of Parkinson’s and they are responsive to dopamine replacement therapy, there is unlikely to be any benefit to further investigation or imaging.
Catypical Features Of Parkinson Disease

Confirming the diagnosis of Parkinson disease during life is difficult because the disorder still lacks biochemical, genetic, or imaging diagnostic standards. In patients diagnosed during life with Parkinson disease, 10% to 25% have an alternative diagnosis discovered at postmortem examination.9–12 These alternative mimicking conditions consist of a variety of neurodegenerative disorders collectively referred to as Parkinson-plus syndromes, disorders that tend to progress more rapidly, present more symmetrically, and respond less well to levodopa than does Parkinson disease.13 Several clinical clues, called atypical features, suggest one of the following mimicking Parkinson-plus Disorders9:
- 1.
What Are The Current Treatment Options
While there is no specific cure for Parkinson’s plus syndrome, there are treatments that can control your symptoms. A doctor can develop a plan for your overall health and to treat your specific symptoms. Medications that treat the symptoms of Parkinson’s disease often do not work as well for Parkinson’s plus syndrome.
Treatment options might include:
- Walking and balance assistance. You might receive physical and occupational therapy to help keep you moving. Therapists can help you build strength and prevent falls. They can also help you learn to use canes, walkers, and other mobility aids, if needed.
- Swallowing and speech assistance. A speech therapist can help you adjust to changes that might make it hard to swallow and speak. They can help you communicate and can recommend foods and beverages that are easier to swallow.
- Medications for cognitive issues. Your doctor might prescribe a variety of medications that can help with your focus and memory. Many of these medications are also used for conditions such as Alzheimer’s or dementia.
- Medications for trouble with movement. You might be prescribed medications that can help you control your muscles and movement. These medications might also address stiffness and balance problems.
- Medications to help with mood symptoms. If you’re experiencing depression, anxiety, or other mood-related concerns, your doctor might prescribe medications that can help with these symptoms.
What Tests Diagnose Parkinsons Disease
DiagnosisSearch terms included “Parkinson’s disease”, most instances of PD are idiopathic, Parkinson’s has neither a definitive diagnostic test nor a cure at the present time, foot tapping or pronation–supination hand movements, Research on early diagnostic tools suggests that Parkinson’s may be able to be identified through a person’s senses, New findings highlight the identification of Parkinson’s-like symptoms based on the speed of keyboard typing.There is no singular test to definitively use to determine if you have Parkinson’s disease, but diagnosis is based on medical history and assessment of simple physical tasks, in 2011, definitive diagnosis can only be made at autopsy, Food and Drug Administration approved an imaging scan called the DaTscan, 3 In addition, or a breath test, except in certain rare cases.The diagnosis of PD is clinical and requires bradykinesia, Rest tremor, There is no single symptom that by itself indicates Parkinson’s Disease, “diagnosis” and “signs and symptoms”, can make the determination.Currently there is no clinical test for PD, no blood test that can indicate a positive result
Definition And Differential Diagnosis
There are many manifestations of PD but the classical diagnostic symptoms are:
- slowness and poverty of movement
- stiffness
The physical signs of PD include:
- slowness of movement
- rigidity
- rest tremor.
At diagnosis, these signs are usually unilateral, but they become bilateral as the disease progresses. Later in the disease additional signs may be present including postural instability , cognitive impairment and orthostatic hypotension .
There is no single way to define Parkinson’s disease or what is often called idiopathic Parkinson’s disease in order to differentiate it from other causes of parkinsonism, such as multiple system atrophy and progressive supranuclear palsy .
PD is traditionally defined, pathologically, by the finding of Lewy bodies and degeneration of catecholaminergic neurones at post-mortem. Using a pathological definition of PD is problematic for a number of reasons:
- A pathological diagnosis is not practical in life.
- Lewy body inclusions in catecholaminergic neurones are seen in individuals without clinical evidence of PD; it is presumed that these are pre-clinical cases.
- Lewy bodies have not been found in otherwise typical individuals with PD with Parkin mutations, although such rare young-onset genetic cases of PD might be said not to have idiopathic PD.
In recent years, attempts to define PD genetically have become possible with the discovery of monogenic forms of the disease. However, such families account for a very small proportion of cases.
Table 5.1
How The Florey Is Making A Difference

The Institute has a number of research projects in its laboratories underway, for example:
- Scientists looking for the cause of Parkinson’s disease continue to search for possible factors that may trigger the disorder, and study genetic factors to determine how genes could play a role
- Other scientists are working on developing new protective drugs that can delay, prevent, or reverse the disease
- Trialling improved methods of diagnosis and treatment monitoring
Tests To Rule Out Other Conditions
Blood tests can help rule out other possible causes of the symptoms, such as abnormal thyroid hormone levels or liver damage.
An MRI or CT scan can check for signs of a stroke or brain tumor, which may cause similar symptoms.
Hydrocephalus due to atrophy can occur with some types of dementia and would be visible with one of these imaging tests. If the person has neurologic symptoms but a normal scan result, Parkinson’s disease may be present.
The doctor a lumbar puncture to rule out inflammation or a brain infection.
What Is Parkinsons Plus Syndrome
Parkinson’s plus syndrome is the name for a group of neurological conditions that are very similar to Parkinson’s disease. Because these conditions cause symptoms that are very similar to Parkinson’s, they are often incorrectly diagnosed. However, these conditions can even be treated using many of the same medications and therapies as Parkinson’s.
Conditions that are considered Parkinson’s plus syndromes include:
How Is Parkinsons Plus Diagnosed
People with Parkinson’s plus syndrome are often diagnosed with Parkinson’s disease in the early years of their condition. However, their condition won’t progress like Parkinson’s disease. It might progress faster, and they might start to develop symptoms that aren’t present in Parkinson’s disease.
There is no definitive test for Parkinson’s or Parkinson’s plus syndrome. Instead, a doctor might conduct a series of tests that will look at your balance, ability to walk, and coordination. These are generally simple in-office tests involving the doctor watching you walk, sit, stand, and perform other movements. You’ll likely also do some memory and cognition tests with the doctor.
The doctor might also order some imaging tests to get a closer look at your brain. These may include:
- MRI scan. An MRI uses magnetic waves to create images of your body.
- PET scan. A PET scan uses a special dye to look for damage to your brain.
- CT. A CT scan can check your brain activity.
Enabling Early Diagnosis Of Life

Every hour, someone in the UK is told they have Parkinson’s disease – a progressive neurological condition with no definitive diagnostic test and no cure. At The University of Manchester we are tackling the development of a non-invasive diagnostic test that may have the ability to diagnose early Parkinson’s – possibly even before physical symptoms are displayed.
Looking For Signs Of Parkinsons
Your specialist will examine you to look for common signs of Parkinson’s. You may be asked to:
- write or draw – to see if your writing is small or gradually fades
- walk – to see whether there’s a reduction in the natural swing of your arm or in your stride length and speed
- speak – to see if your voice is soft or lacks volume
The specialist will also look at and ask you about your:
- face – to see if there is a ‘masked’ look or if you have difficulty with facial expressions
- limbs – to see if you have a tremor, any stiffness or slowness of movement
As well as examining you for any of the typical signs of Parkinson’s, the specialist will also look for signs that may suggest a different diagnosis.
It may be helpful to take someone with you for support when seeing a specialist. Taking a list of questions you want to ask can also be useful so you don’t forget to mention something you want to know about. If a healthcare professional says something you don’t understand, don’t be afraid to ask them to explain what they mean.
From Evidence To Recommendation
The pathological studies emphasise the need for particular care in making a clinical diagnosis of PD. There is limited evidence to suggest that the UK PDS Brain Bank Criteria have adequate sensitivity and specificity in comparison with post-mortem findings. The accuracy of diagnosis using the Brain Bank criteria increases as the condition progresses.
The availability of PD brain tissue has fostered much valuable research in recent years and should be encouraged in the future. Diagnostic information derived from post-mortem examination can also be of value to the families of individual patients.
RECOMMENDATIONS
- R9.
-
PD should be diagnosed clinically and based on the UK Parkinson’s Disease Society Brain Bank Criteria.
- R10.
-
Clinicians should be encouraged to discuss with patients the possibility of tissue donation to a brain bank for purposes of diagnostic confirmation and research.
