Tom Thought That Because Some Pink Tablets Relieved His Symptoms This Meant He Was Ok He Didn’t
I first suspected there was something wrong when I was travelling and I was writing a postcard to a friend of mine in, in Australia whose name is Anthony Diecopolis. And, and I got to the Anthony Diec and I couldn’t finish the opolis. And it’s very strange my hand had sort of gone into a sort of spasm and it just wouldn’t, wouldn’t finish writing the, the, the word. And so that’s a bit strange.
And so I went when, when I got I, I went to the doctor and said, “What on earth’s going on?” And I had since then I’d also developed this slight tremor in my right hand. He said, “Well it’s probably, Essential Tremor or trapped nerve or something like that”. And anyway, then it got a bit worse and then I was, I was recommended to go to a neurologist. And the neurologist had a look at me and gave me some pills. And he said, “Come back and tell me if these work”.
This is about, about sort of, nine months after my, my not being able to finish the, the postcard. And, and he said, “Take these pills”. And the pills worked. Magically the tremors stopped and I thought this is wonderful. And so I went back to the neurologist and I said, “Yes everything’s fine now. The pills have, the pills have worked.” And far from looking happy about this he looked rather, rather grave and he said, “I think you’d better go to another neurologist.”
Parkinsons Is Easily Identified By A Pathologist But Is Difficult To Diagnose For A Clinician
When I state that Parkinson’s Disease is “well defined,” I mean that the pathologist, looking at slides of the brain under a microscope, can say, knowing nothing about the patient, that the person had PD. Parkinson’s Disease causes certain, easy to detect changes that are seen under the microscope. This, of course, requires that the person is dead, which isn’t much use to that particular person or his family. The absence of a reliable test, in life, means then that there is room for mistakes. And, in fact, we make a fair number of mistakes, and I’ll discuss below the types of cases in which we are most likely to make mistakes. Unfortunately, we are never in the position of being 100% certain that we’ve diagnosed someone correctly, until the autopsy.
Comparison Of Patients In Whom A Diagnosis Of Parkinson’s Disease Was Maintained Or Rejected
Patients in whom a diagnosis of Parkinson’s disease was confirmed had more severe disease as measured by the Hoehn and Yahr stage , more often had a tremor at rest or a classical pill rolling tremor , and more often reported a good initial and sustained response to levodopa than those in whom it was rejected.
Patients in whom the diagnosis was changed to non-parkinsonian tremor had no other parkinsonian features such as rigidity, bradykinesia, hypomimia, or monotonous speech. They also reported falls significantly less frequently and had higher mini-mental state scores . Those in whom the diagnosis was changed to atypical parkinsonism had more severe akinesia , rigidity , and postural instability , less commonly reported an initially or currently good response to levodopa , but more often had incontinence and additional features incompatible with Parkinson’s disease. Those in whom the diagnosis was changed to vascular parkinsonism were older than those in whom a diagnosis of Parkinson’s disease was confirmed , had a larger number of smoking years , more often had gait difficulties as their first complaint , and had more severe postural instability ; they never had a rest tremor.
Sensitivity Specificity And Predictive Value Of A Previous Diagnosis Of Parkinson’s Disease
Of 126 patients with a pre-existing clinical diagnosis of probable and possible Parkinson’s disease in the overall sample , 111 were confirmed as having Parkinson’s disease, resulting in a sensitivity of 88.1% ; similarly, it was confirmed that 54 of 74 patients did not have Parkinson’s disease, resulting in a specificity of 73.0% . The positive and negative predictive values of a previous clinical diagnosis of Parkinson’s disease were 84.7% and 78.3% . In other words, in 85% of patients with a previous diagnosis of Parkinson’s disease this diagnosis was confirmed, and 78% of patients with a diagnosis other than Parkinson’s disease did not have the disease .
When this was broken down by a specialist or other doctor diagnosis, the diagnostic validity was as follows. Neurologists and geriatricians had a sensitivity and specificity of 93.5% and 64.5% , respectively, compared with 73.5% and 79.1% for non-specialists. The positive predictive values were greater for specialists than for other doctors , but the negative predictive values were equivalent v non-specialist 79.1% ).
Patients In Whom A Diagnosis Of Parkinson’s Disease Was Or Was Not Previously Made
Patients in whom a diagnosis of Parkinson’s disease was previously made had a longer disease duration and greater disease severity , with more severe akinesia , postural instability, and rigidity than those in whom the diagnosis was not made before. They were also more likely to be depressed , to have experienced dyskinesias , and to live alone or with their family than in a nursing home .
Next Steps And Considerations After Learning You May Have This Movement Disorder
Parkinson’s is a disease of the nervous system that affects movement. Tremor, stiffness, balance issues and slow movement are some of the common symptoms. More than 1 million people in the United States are currently living with Parkinson’s disease, and about 60,000 Americans are newly diagnosed each year, according to the Parkinson’s Foundation.
“A lot of times I’m asked if Parkinson’s is becoming more common,” said David Charles, M.D., vice-chair of neurology and neurologist in the Movement Disorders Clinic at Vanderbilt University Medical Center. “But the prevalence of Parkinson’s increases with age. And so that leads to the illusion that Parkinson’s disease is happening more often. But actually what’s happening is our population is aging.”
If you or a loved one is among the newly diagnosed, you may be wondering what to expect or what steps to take next. We asked Charles to offer guidance and insight.
What Is Essential Tremor And How Is It Different To A Parkinsons Tremor
A tremor is a rhythmical, involuntary movement that affects a part of the body, such as the hand.
Essential tremor is the most common type of tremor. It’s most noticeable when your hands are doing something and it usually affects both the right and left sides of the body equally. Essential tremors often lessen when your body is resting.
Unlike an essential tremor, a Parkinson’s tremor is most obvious when the affected body part is resting and tends to be less noticeable with movement. It usually starts on one side of the body and may progress to the other side as Parkinson’s develops.
The time it takes to get a diagnosis can vary from person to person. Some people may receive a diagnosis of Parkinson’s quite quickly, but for others it may be a long process. This can be due to a number of things, including your medical history, your age and what symptoms you have.
Your specialist may wish to rule out other causes of your symptoms first and see how you respond to treatment. This may take some time, and, as already mentioned, there is currently no definitive test for Parkinson’s.
How you respond to treatment may help your specialist make a diagnosis. Keeping a diary or record of your symptoms will give the specialist more information to guide their decision.
Because the symptoms of Parkinson’s are sometimes similar to other forms of parkinsonism, people can sometimes be misdiagnosed.
Patients With A Previous Diagnosis Other Than Parkinson’s Disease
Among all patients seen, two were referred for diagnostic purposes without a previous diagnosis, and 69 of 202 patients had a previous diagnosis other than Parkinson’s disease . Among these, 56 patients had been given a diagnosis of non-parkinsonian tremor, two of vascular parkinsonism, one of atypical parkinsonism, and 10 had been prescribed an antiparkinsonian drug for parkinsonian features without a specific diagnosis . Thirteen of the 69 patients with different diagnoses and the two patients referred for diagnostic purposes fulfilled strict clinical criteria for Parkinson’s disease . In two additional patients who had a previous diagnosis of non-parkinsonian tremor, a diagnosis of “possible Parkinson’s disease” was made . If only patients who had at some point in the past seen a specialist were considered, the diagnosis was changed to probable Parkinson’s disease in five and to possible Parkinson’s disease in one .
Sensitivity, specificity, and predictive values for the overall sample* and by type of clinician
Understanding Parkinsons Disease: Getting A Parkinsons Diagnosis

Once you start noticing some changes in your body that impact your daily life or are just simply bothersome, you should begin the process of figuring out if you have Parkinson’s disease. It may seem like a daunting undertaking, but don’t let fear stop you. Once you are diagnosed, you can start treating your symptoms and learning strategies that will help you feel better.
Determining Diagnosis Through Response To Parkinsons Medication
If a person’s symptoms and neurologic examination are only suggestive of Parkinson’s disease or if the diagnosis is otherwise in doubt, the physician may, nevertheless, prescribe a medication intended for Parkinson’s disease to provide additional information. In the case of idiopathic Parkinson’s, there is typically a positive, predictable response to Parkinson’s disease medication; in the case of some related Parkinsonian syndromes, the response to medication may not be particularly robust, or it may be absent entirely.
Unfortunately, there are no standard biological tests for the disease, such as a blood test. However, researchers are actively trying to find biomarkers in blood and other bodily fluids that could help confirm the diagnosis.
Parkinsons Q&a: How Do I Find Information After A New Diagnosis
Navigating Parkinson’s disease can feel like a never-ending learning curve. PD Conversations is a place to ask your Parkinson’s questions and connect with others living with the disease. In this blog series, we highlight a high-interest question answered by the Parkinson’s Foundation Helpline on PD Conversations.
Question:My husband is newly diagnosed with Parkinson’s disease but didn’t tell me much about his diagnosis. What should I know about Parkinson’s, and what resources could be helpful for us?
It sometimes takes time for people who are newly diagnosed to share much about their diagnosis and symptoms. It is difficult news to hear and difficult to digest. Giving him time to reveal what he wants to at the right time might be helpful.
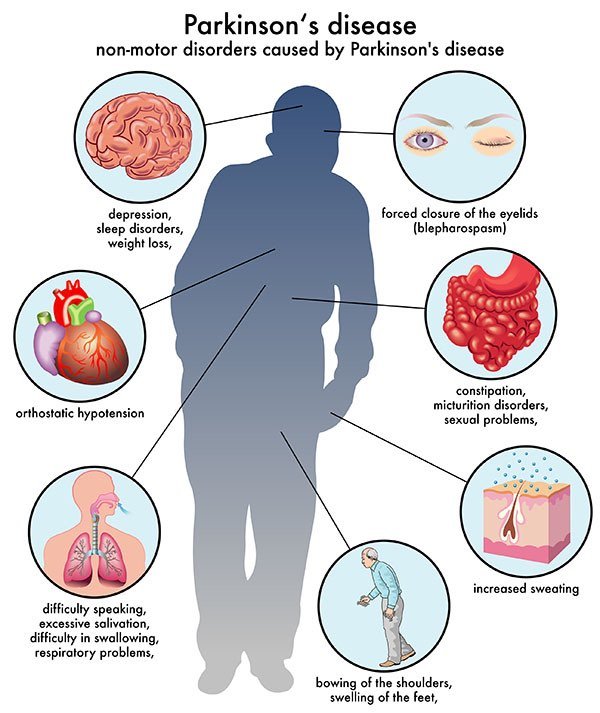
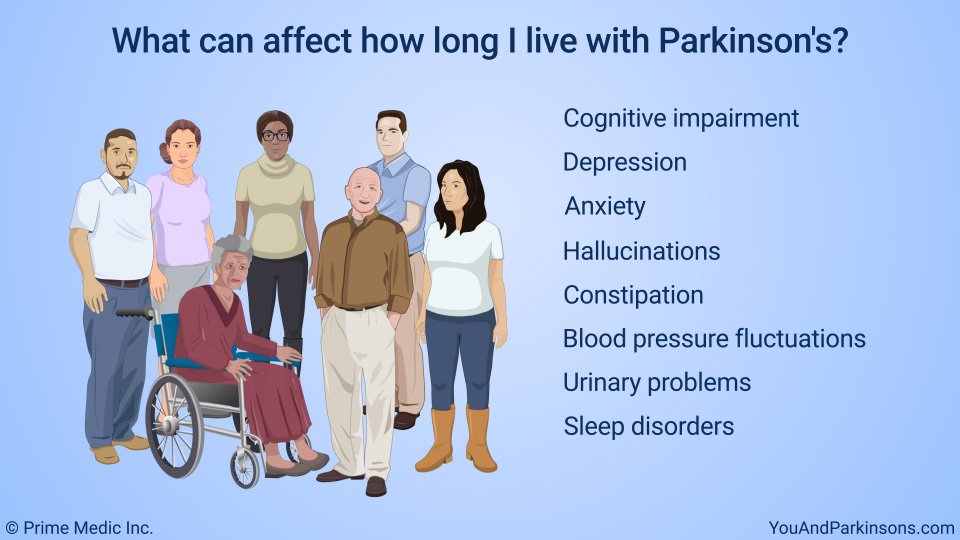
We have no way of knowing the rate of progression or symptoms people may develop. For the most part, he may have some movement symptoms like tremor, slowness of movement, and stiffness or rigidity in his muscles in the beginning. This may worsen over time. He may also have some non-movement symptoms like anxiety, low blood pressure, decreased facial expression, or hoarse voice. However, no one can predict if he will develop any of these symptoms as Parkinson’s is different for every person.
Treatments such as medications and exercise may help manage symptoms, while seeking expert care — through building a care team — improves the quality of life and lowers the risk of complications.
We’re here for you.
Brain Imaging And Other Tools To Aid Diagnosis Of Parkinsons
In addition to taking a history and performing a detailed neurologic examination, physicians sometimes use brain imaging to help support a particular diagnosis. However, these studies have their limitations in the diagnosis of Parkinson’s disease and are typically used only in select patients. Brain imaging is not routinely performed by neurologists or movement disorder specialists when they are considering a diagnosis, especially if the person’s symptoms strongly suggest to the physician that idiopathic Parkinson’s disease is the correct diagnosis.
Helping diagnose Parkinson’s with DaTscan and other tests
Rather, use of imaging is most helpful when the diagnosis is uncertain, or when physicians are looking for changes in the brain that are more typical of one of several Parkinsonian syndromes and other conditions that can mimic Parkinson’s. Imaging studies to evaluate Parkinson’s disease and Parkinsonian syndromes include magnetic resonance imaging , which examines the structure of the brain, and DaTscan, an imaging test approved by the Food and Drug Administration to detect the dopamine function in the brain. A DaTscan may help differentiate idiopathic Parkinson’s disease from certain other neurologic disorders. Most physicians’ offices will have access to MRI; however, DaTscan imaging may only be available at larger hospitals or medical centers.
Patients With A Previous Diagnosis Of Parkinson’s Disease

The diagnosis of probable Parkinson’s disease was confirmed in 109 of the 131 patients with this diagnosis , including three in whom atypical features were found but were insufficient to invalidate the diagnosis of Parkinson’s disease . Two additional patients were found to have possible Parkinson’s disease. However, in 20 of the 131 patients the diagnosis of Parkinson’s disease was unequivocally rejected . The alternative diagnoses were non-parkinsonian tremor in four patients , vascular parkinsonism in six , progressive supranuclear palsy in four , and multiple system atrophy in three . Two patients received a diagnosis of idiopathic torsion dystonia, and one of dementia without parkinsonism. When only those patients who had seen a specialist at some point in the past were considered, the diagnosis was changed from Parkinson’s disease to a different diagnosis in 11%.
Patients with an initial diagnosis of Parkinson’s disease
A Second Opinion After Your Parkinsons Disease Diagnosis
Getting a second opinion after an initial diagnosis can be helpful. “The first time someone’s told they have Parkinson’s can be very upsetting — and of course, understandably so,” Charles said. “Seeking a second opinion is always entirely reasonable.” Parkinson’s is a slowly progressive disease, he added, so there’s no harm in taking additional time to get a second opinion.
Conditions That May Be Mistaken For Parkinsons Disease
There are a few conditions that may be confused with Parkinson’s disease. These conditions can cause similar symptoms, and because there is no definitive test that proves you have Parkinson’s disease or any of these “similar” conditions. As you might imagine, this can make it challenging at times for doctors to figure out which condition you have. A few of the most common conditions that might look like Parkinson’s are:
Pd Diagnosis Disease Severity And Disease Progression
The diagnosis of PD is essentially clinical , and we believe that the clinical evaluation of patients will not be replaced by modern imaging techniques. Nevertheless, as pointed out earlier, misdiagnosis can approach 20% of cases . Recently, in line with the European Union, the U.S. FDA approved DAT scan as a diagnostic tool to help differentiate between PD and Essential Tremor. This is the only current FDA-approved subsidiary examination to aid in PD diagnosis.
The role of magnetic resonance imaging in the diagnosis of PD is still not fully established. Traditionally, it has been seen as a means to potentially exclude alternate diagnoses such as vascular parkinsonism, or more importantly , atypical forms of degenerative parkinsonism such as MSA or progressive supranuclear palsy . Traditional structural MRI findings of these latter diagnoses such as increased pallidal iron, rim of putaminal hyperintensity, “hot cross bun” sign and/or cerebellar atrophy in MSA or the hummingbird or penguin sign in PSP may not be reliable, particularly in early disease.
Figure 5. Multimodal MRI in PD. Differences are noted between patients with PD and controls through voxel-based analysis of R2?, mean diffusivity, and fractional anisotropy maps.
- •
-
Low dopamine transporter uptake in basal ganglia demonstrated by SPECT or PET imaging.*
RONALD F. PFEIFFER, inAnimal Models of Movement Disorders, 2005
Methodological Limitations Of The Diagnostic Studies

When interpreting the literature about PD diagnosis, the following methodological issues should be considered:
- lack of long-term prospective clinical and pathological as a reference standard
- lack of operational definitions such as defining specialists or clinical diagnostic criteria
- unclear whether investigators were blinded to initial diagnosis
- sample sizes necessarily limited by the number of cases available with neuropathological outcomes
- PD trial age groups are often young as studies were performed by neurologists who see a younger population of people with PD
- most studies included people with established disease lasting some years
- varying geographical locations
- some studies are in specialised units and may not reflect the diagnostic accuracy of other units in the UK
- exclusion of some studies using magnetic resonance volumetry and magnetic resonance spectroscopy as they lacked appropriate population, intervention and outcome criteria
- lack of statistical details of diagnostic accuracy such as sensitivity, specificity and positive predictive values
- lack of economic evaluations of SPECT.
Expect To Understand Only Part Of What You Are Told
After the sudden announcement of a Parkinson’s diagnosis, you will likely be unable to absorb all the information that health care professionals will give you.
You should not look for more information in the first few weeks following your diagnosis because this may increase your anxiety level instead of reassure you.
How Will I Manage The Changes Caused By The Disease
You likely had plans, dream vacations or other things you wanted to accomplish in your future. You must now incorporate your condition into these projects. Although Parkinson’s is a progressive disease, it progresses slowly and differently from person to person.
Take advantage of everyday that passes and continue the hobbies and activities you enjoyed. For some, the diagnosis can be the opportunity to strengthen character and discover passions and qualities they would not have found otherwise.
Turn your fear into curiosity and learn all you can about the disease. Parkinson Québec has many resources to help you better understand the disease and live with it on a daily basis. Ask your loved ones for help or reach out to available resources for support.
The Right Care Provider To Treat Parkinsons Disease
You can also take your time finding the right neurologist to treat your Parkinson’s and help guide you on your journey. Charles said it’s best to find someone close by whom you can see easily when you need to.
“For people who are able to receive their care at Vanderbilt,” he added, “we have a large division of movement disorders, with faculty specialized in the care of people with Parkinson’s disease. And not only is it a large division, it’s also one of the most highly respected in the nation.”
Likelihood Of Referral According To Final Diagnosis
Overall, 74% of all cases with a diagnosis of Parkinson’s disease had been seen by a specialist. However, when these cases were classified by final diagnosis , it was observed that, paradoxically, fewer cases with atypical disease had been seen by a specialist compared with those with classical Parkinson’s disease ; p = 0.02).
What Parkinsons Diagnosis Criteria Do Doctors Use
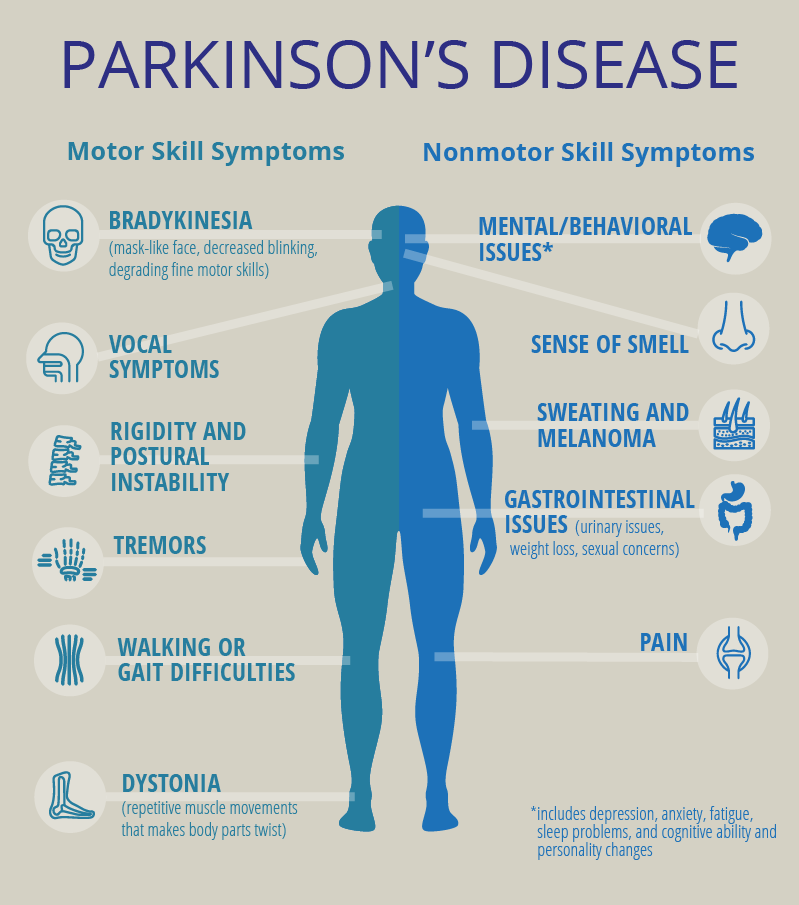
Until the 1980s, there was no formal diagnostic criteria for Parkinson’s disease. Beginning with James Parkinson’s 1817 article, “An Essay on the Shaking Palsy,” and Margaret Hoehn and Melvin Yahr’s description of the five stages of motor progression in 1967, scientists focused on the unique ways Parkinson’s disease affects movement. A few scientists also noted non-motor symptoms like issues with automatic body functions, such as heart rate and blood pressure.
With the discovery in the 1950s of levodopa, a drug that gets turned into dopamine in your brain and thus replaces some of the dopamine that is lost due to PD, and the discovery of how dramatically levodopa improves motor symptoms, the medical community continued to focus more of their efforts on defining and treating Parkinson’s as a motor condition.7
Other Challenges Of Diagnosing Parkinsons Disease
Parkinson’s disease progresses slowly, often with non-motor symptoms appearing months or years before motor symptoms. This can make it challenging for doctors to diagnose you in the early stages, especially since the diagnostic criteria is based mostly on motor symptoms. You may have to wait until your symptoms progress for you and your doctor to confirm your diagnosis.14
Age and gender can be another issue. Since Parkinson’s is associated more with older men, doctors may not think their younger or female patients have Parkinson’s.5 On the other hand, since the disease is associated with aging, your symptoms may be blamed on “getting older.”
Remember that movement disorder specialists are extremely knowledgeable about Parkinson’s disease and can help put the pieces together where other more generalized doctors may not. Never hesitate to fight for the care you deserve.
Related: Here’s what’s important to remember if you were just diagnosed with Parkinson’s disease.
What Doctors Look For When Diagnosing Parkinsons
Certain physical signs and symptoms — noticed by the patient or his or her loved ones — are usually what prompt a person to see the doctor. These are the symptoms most often noticed by patients or their families:
-
Shaking or tremor: Called resting tremor, a trembling of a hand or foot that happens when the patient is at rest and typically stops when he or she is active or moving
-
Bradykinesia: Slowness of movement in the limbs, face, walking or overall body
-
Rigidity: Stiffness in the arms, legs or trunk
-
Posture instability: Trouble with balance and possible falls
Once the patient is at the doctor’s office, the physician:
-
Takes a medical history and does a physical examination.
-
Asks about current and past medications. Some medications may cause symptoms that mimic Parkinson’s disease.
-
Performs a neurological examination, testing agility, muscle tone, gait and balance.
Clinicopathological Types Of Parkinson’s Disease
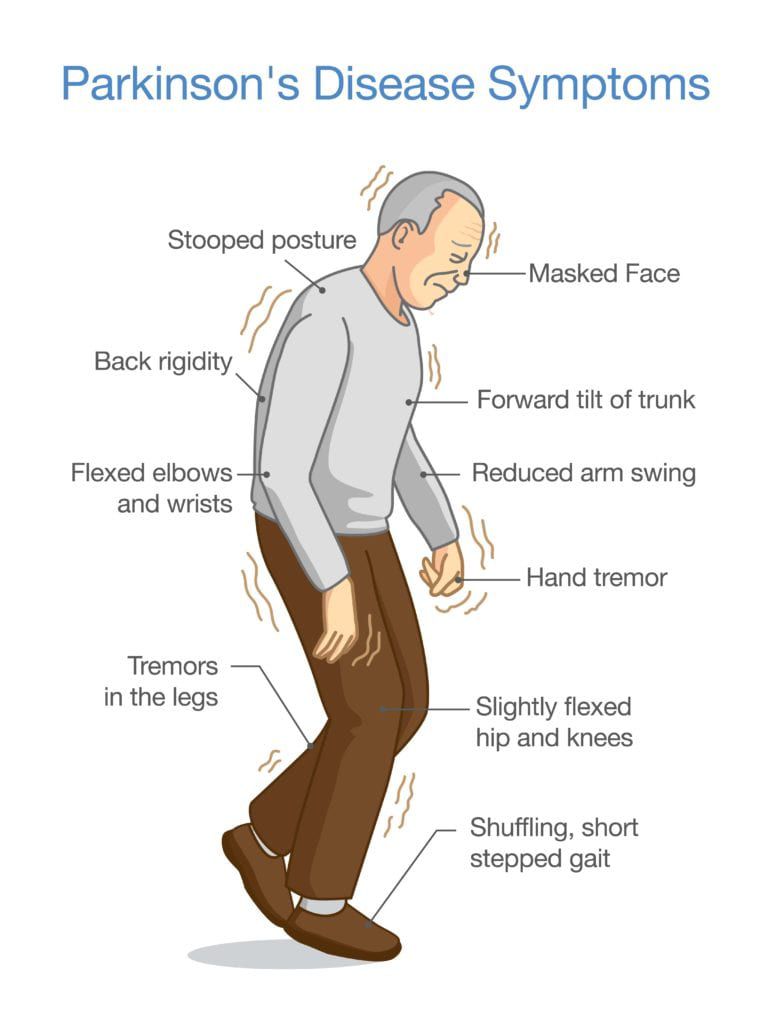
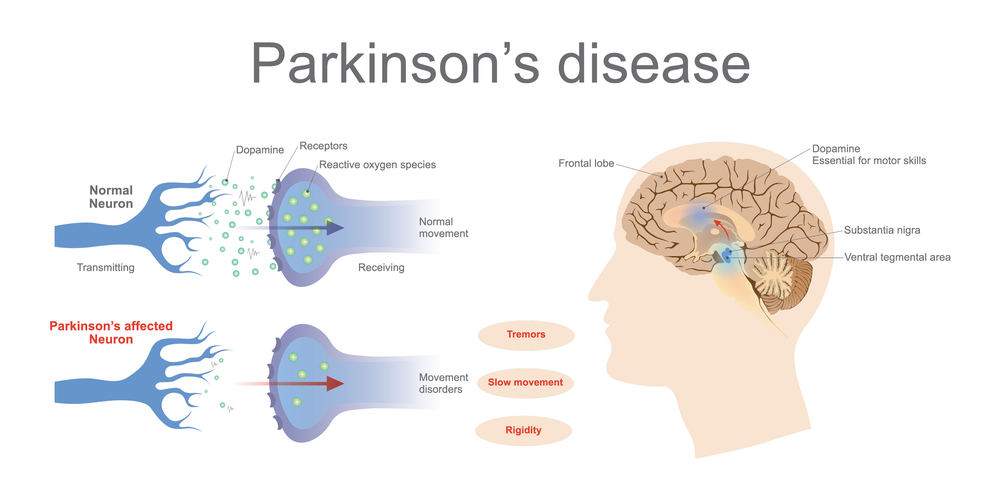
As stated previously, the pathological diagnosis of PD requires Lewy bodies , depigmentation, and cell loss in the substantia nigra . These features define the most common form, or idiopathic PD. The clinical course for idiopathic PD is long and slow, and most often there is very lengthy disease duration. The cardinal clinical features are bradykinesia, muscular rigidity, resting tremor, and postural instability, with greater certainty for this diagnosis when symptom onset is asymmetrical and there is a good response to levodopa therapy.12 In addition to the predominant motor symptoms, PD patients can have a range of nonmotor symptoms, including autonomic dysfunction, olfactory dysfunction, depression, sleep disturbances, hallucinations, cognitive impairment and dementia.12,13 Broader neuropathology in brainstem and cortical regions is associated with these nonmotor features.14 The prevalence of this common form of PD is estimated at 0.3% of the entire population in industrialized countries, increasing to 1% in individuals older than 60 years, and 4% in individuals older than 85 years.15
What Are The Stages To Coping With My Condition
Parkinson’s disease causes recurring bouts of grief. Your life will change and you will no longer be able to continue all your activities.
These are the stages most individuals go through before accepting their diagnosis and developing new life skills. A psychologist specializing in neurodegenerative diseases can help you go through these stages more easily.
There Is No Test To Diagnose Parkinsons Disease
Although Parkinson’s disease is a specific, well defined disease that can be reliably diagnosed at autopsy, it is defined in life by clinical criteria. This means that the diagnosis rests entirely on the information that the patient provides plus the physical examination. There is no test to diagnose PD. When a doctor orders a test when evaluating a patient who he thinks has PD, the test is really being obtained to make sure that there isn’t some other disorder that might look like PD. When I am convinced that a patient has Parkinson’s Disease I order no tests at all. No CAT scan, no MRI, no EEG, no spinal tap, no blood tests. Nothing. The reason is that if any of these tests was to show an abnormality, it would mean to me that the patient had Parkinson’s Disease plus some other disorder that has nothing to do with why the patient was seeing me in the first place. Generally I’d rather not know.
If Its Not Parkinsons Disease What Could It Be
Here are some possibilities:
Side effects of medication: Certain drugs used for mental illnesses like psychosis or major depression can bring on symptoms like the ones caused by Parkinson’s disease. Anti-nausea drugs can, too, but they typically happen on both sides of your body at the same time. They usually go away a few weeks after you stop taking the medication.
Essential tremor: This is a common movement disorder that causes shaking, most often in your hands or arms. It’s more noticeable when you’re using them, like when you eat or write. Tremors caused by Parkinson’s disease usually happen when you’re not moving.
Progressive supranuclear palsy: People with this rare disease can have problems with balance, which may cause them to fall a lot. They don’t tend to have tremors, but they do have blurry vision and issues with eye movement. These symptoms usually get worse faster than with Parkinson’s disease.
Normal pressure hydrocephalus : This happens when a certain kind of fluid builds up in your brain and causes pressure. People with NPH usually have trouble walking, a loss of bladder control, and dementia.
Conditions Misdiagnosed As Parkinson’s Disease
Parkinsons disease, especially in its early stages when symptoms are mild, is not an easy disease to diagnose. The non-specific, and easily overlooked nature of the signs of Parkinsons make it difficult to spot, and unlike many illnesses, there is no one laboratory test or radiological exam that will provide a definitive diagnosis of Parkinsons disease.
Patients exhibiting Parkinsons-like symptoms may undergo blood and urine tests, or CT or MRI scans to exclude other conditions, but none of these will provide a diagnosis of Parkinsons disease. The best way to test for Parkinsons disease is to conduct a systemic neurological examination that includes tests to gauge a patients reflexes, muscle strength, coordination, balance, gait, and overall movement. Even so, according to information presented on The Michael J. Fox Foundation for Parkinsons Research, up to 25 percent of Parkinsons disease diagnoses are incorrect.
So, why is there confusion about diagnosing Parkinsons disease? The simple answer is that symptoms of Parkinsons disease are not clear cut, and therefore, it is easy to mistake them for other conditions, or to classify them as parkinsonian when they are not.
Here is a brief overview of the top ten conditions mistaken for Parkinsons disease:
Beyond those top three, there are other conditions that are often confused with Parkinsons disease, including:
Diagnosis And Management Of Parkinsons Disease
There are no diagnostic tests for Parkinson’s. X-rays, scans and blood tests may be used to rule out other conditions. For this reason, getting a diagnosis of Parkinson’s may take some time.
No two people with Parkinson’s disease will have exactly the same symptoms or treatment. Your doctor or neurologist can help you decide which treatments to use.
People can manage their Parkinson’s disease symptoms through:
- seeing a Doctor who specialises in Parkinson’s
- medication
- multidisciplinary therapy provided for example, by nurses, allied health professionals and counsellors
- deep brain stimulation surgery .
Medications For People With Parkinsons Disease
Symptoms of Parkinson’s disease result from the progressive degeneration of nerve cells in the brain and other organs such as the gut, which produce a neurotransmitter called dopamine. This causes a deficiency in the availability of dopamine, which is necessary for smooth and controlled movements. Medication therapy focuses on maximising the availability of dopamine in the brain. Medication regimes are individually tailored to your specific need. Parkinson’s medications fit into one of the following broad categories:
- levodopa – dopamine replacement therapy
- dopamine agonists – mimic the action of dopamine
- COMT inhibitors – used along with levodopa. This medication blocks an enzyme known as COMT to prevent levodopa breaking down in the intestine, allowing more of it to reach the brain
- anticholinergics – block the effect of another brain chemical to rebalance its levels with dopamine
- amantadine – has anticholinergic properties and improves dopamine transmission
- MAO type B inhibitors – prevent the metabolism of dopamine within the brain.
Diagnosis Of Parkinson Disease: Motor Symptoms
The clinical diagnosis of Parkinson’s disease is based on the presence of characteristic motor symptoms: bradykinesia, rigidity, postural instability, and resting tremor but neuropathology is still considered the gold standard for definite diagnosis. Differentiating PD from other movement disorders can be challenging throughout the disease course, because signs and symptoms often overlap. Indeed, neuropathology studies reveal that clinical diagnosis of PD can be confirmed with an accuracy of about 75%. Good response to levodopa is often used to support the diagnosis of PD. However, cases of pathologically proven PD with poor response to levodopa have also been reported.
Misdiagnosis of PD can occur for several reasons. In a community-based study of patients taking antiparkinsonian medication, the most common misdiagnosis were essential tremor, Alzheimer’s disease, and vascular parkinsonism. In addition, many of the prominent features of PD may also occur as a result of normal aging or from comorbid and multifactorial medical conditions .
Katarzyna Kaczy?ska, Kryspin Andrzejewski, inGenetics, Neurology, Behavior, and Diet in Parkinson’s Disease, 2020
Learn More About Parkinsons Disease: Overview