The 2016 Edition Of The Researchers Days Organised By The Fnr Attracted A Large Audience That Took Part In Fascinating Scientific Experiments And Had The Opportunity To Mingle With The Present Researchers The Luxembourg Parkinson Study Was Of Course There Too With A Booth Called What Parkinsons Disease Feels Like We Took A Closer Look

In order to see how Parkinson’s disease feels like, hundreds of visitors tried on a Parkinson suit which simulates the two most representative motor symptoms of Parkinson’s disease: the muscle rigidity and the tremors. At first glance, the suit looks like a race car driver’s outfit. But together with the elbow and knee bands, and the ankle, wrist and chest weights, this suit shows how rigid the muscles and articulations can be, and how difficult it is for Parkinson’s disease patients to move.
If You Live In South Jersey And Have Questions About The Final Stages Of Parkinsons Disease Or Hospice Care For Your Loved One Please Call Samaritan At 229
Samaritan is a member of the National Partnership for Healthcare and Hospice Innovation, a network of not-for-profit hospice and palliative providers across the country. If you know someone outside of our service area who is living with advanced illness and can benefit from hospice or palliative care, please call 1 -GET-NPHI for a referral to a not-for-profit provider in your area.
When I First Began To Suspect Something Was Going On Inside Of Me I Felt Like My Insides Were Shaking All The Time
There is most likely as many people with Parkinson’s who experience external tremors who experience internal tremors. You can have one, both, or neither and still have… Parkinson’s disease. Most people don’t know about external tremors as you can’t see them.
Some other symptoms of PD you will never see are having to deal with cognitive issues: failing memory, anxiety, feelings of apathy, and depression to name a few. Some of these issues don’t occur because we are sad and blue about our predicament, but more than likely they are a symptom of the disease itself, not a reaction of how we are handling it.
Interested In Parkinsons Disease Research Sign Up To Our Forums And Join The Conversation
Don’t give up.
At times, not giving up is easier said than done, especially when you feel alone and abandoned. You may feel your friends and family have abandoned you, but it’s often more a case of them not understanding your new journey. It’s probably best to give those people in your life a free forgiveness pass and move on as you make new friends in the PD community who truly understand what living with PD is like.
Parkinson’s disease causes grief, but we can choose to live joyfully and intentionally in spite of what we feel has been taken from us. It is not a death sentence, and we must learn to readjust to our “new” life. And a new life brings new opportunities. As one person said, never lose hope and keep the faith because God is doing miracles every day and you may be the one He is working through to accomplish just that.
***
How Can Hospice Help Your Loved One In The Final Stages Of Parkinsons Disease

Hospice care is an extra layer of support to help you care for your loved one with end-stage Parkinson’s disease. It is a special kind of care that provides comfort, support, and dignity at the end of life.
The comprehensive program focuses on physical, emotional, and spiritual quality of life through the help of a team of experts. The team includes a board-certified physician, nurse, social worker, certified home health aide , spiritual support counselor, and volunteer.
The nurse will explain the prognosis and what to expect in the upcoming days or weeks. They will also monitor pain and other symptoms. The CHHA helps with personal care needs like bathing and changing bed linens. The social worker helps address social, emotional and practical challenges including complex and inter-related needs. The spiritual support counselor helps explore spiritual concerns.
Most importantly, the hospice team will be there for you during this difficult time, bringing you peace of mind. The team is on call 24 hours a day – even at 2:00 am.
Hospice is about making your final months and weeks as good as possible. This means focusing on what really matters to you.
You Could Have Parkinsons Disease Symptoms In Your 30s Or 40s And Not Know It
Blog post | 11 Apr 2019
You’d be forgiven for thinking that Parkinson’s is only an older person’s disease.
Many people with Parkinson’s, a progressive disease of the nervous system, are indeed at retirement age. So the world was shocked when Back to The Future actor Michael J. Fox revealed he was diagnosed with Parkinson’s disease at only 29 years old.
But Fox’s case isn’t unique. It’s believed that 1 in 10 people with Parkinson’s develop the disease some time before their 40th birthday. About 1 in 5 Australians with Parkinson’s are at ‘working age’ .
And a person can live with symptoms for many years before a diagnosis of Parkinson’s is made.
To mark World Parkinson’s Day, Thursday April 11, here’s what you need to know about the early signs of this insidious neurological disease.
What Is Parkinsons Disease Symptoms Causes Diagnosis Treatment And Prevention
The causes and symptoms of Parkinson’s disease can vary from person to person. While there is no cure, there are medications and treatments to help manage the condition.
Parkinson’s disease is a movement disorder that happens when nerve cells in a certain part of the brain are no longer making the chemical dopamine.
The condition is also sometimes known as paralysis agitans or shaking palsy.
The Parkinson’s Foundation estimates that 60,000 Americans are diagnosed with Parkinson’s every year. However, the true number of people who develop the disease may be much higher.
Difference Between Parkinsons Disease Dementia And Dementia With Lewy Bodies
Technically, the difference between these two conditions lies in how quickly the cognitive difficulties and hallucinations develop in relation to the movement issues. In DLB, the cognitive difficulties and hallucinations develop much sooner in the disease course than in PDD, sometimes even prior to the movement difficulties. Because of the similarities between PD, PDD, and DLB, current thinking in the medical community is that they should be viewed as related diseases which fall along a continuum of Lewy body disorders.
Treatments For Parkinsons Disease Dementia And Dementia With Lewy Bodies
Treatments for DLB are similar to PDD and are aimed at symptom control. The motor symptoms of slowness, stiffness and walking difficulties can be treated with Levodopa. However, Levodopa can cause or exacerbate hallucinations, making it difficult to use it as a treatment for patients who have or are at risk of having hallucinations. Sometimes, clinicians will need to treat the hallucinations more aggressively in order for a patient to tolerate Levodopa given to help the motor symptoms. On the flipside, anti-psychotic medications to control hallucinations can worsen motor symptoms, so treating all the symptoms of LBD simultaneously can be a tricky balancing act.
Some One Who Has Pd Has Likened It To Wearing A Leaded Body Suit
You have the will to get where you’re going or do what you want to do but your body is determined to get you there by the slowest means possible , while exerting the most energy you have. It’s as if your life has switched to slow motion and everything takes so much longer. You expect to look into the mirror and see the likeness of a 70 year old and yet, you’re only 42. Life can be hard.
Learn More About One Of The Most Common Neurological Conditions
As many as one million people live with Parkinson’s disease in the United States and it’s the second most common neurodegenerative disorder. However, there is still much to learn about Parkinson’s disease on many levels, says Tatyana Simuni, MD, director of the Parkinson’s Disease and Movement Disorders Center at Northwestern Memorial Hospital. When it comes to research and breakthroughs, scientists at Northwestern Medicine are consistently paving the way forward with new strategies for side effects and better insight into slowing the progression.
And in the everyday, here are 7 things you may not know about Parkinson’s disease.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
The Overlaps Between Stress And Parkinson’s Disease Part 2
These changes in internal pressure under stress would also explain the feelings of heaviness/being crushed expressed above, since if the internal pressure forces in the body aren’t sufficient to overcome the external force of gravity, it would stand to reason that the body would start to adopt concave shapes, like the classic stooped posture of PD. This is easy to understand with a simple analogy of a balloon. If we pump up the balloon to a high pressure, the balloon would be perfectly round. However, if we then started to deflate it again, decreasing its internal pressure, then the sphere would begin to collapse under gravity: the balloon becomes more rugby ball or american football shaped. This is because the internal pressure pushing outwards is no longer sufficient to completely overcome the external force of gravity. As we keep deflating the balloon , the balloon will continue to flatten out on. Indeed, eventually it will be just be a flat pancake of rubber on the floor, of course.
What Are The Primary Motor Symptoms Of Parkinsons Disease
There are four primary motor symptoms of Parkinson’s disease: tremor, rigidity, bradykinesia and postural instability . Observing two or more of these symptoms is the main way that physicians diagnose Parkinson’s.
It is important to know that not all of these symptoms must be present for a diagnosis of Parkinson’s disease to be considered. In fact, younger people may only notice one or two of these motor symptoms, especially in the early stages of the disease. Not everyone with Parkinson’s disease has a tremor, nor is a tremor proof of Parkinson’s. If you suspect Parkinson’s, see a neurologist or movement disorders specialist.
Tremors
Read more about Parkinson’s tremors
Rigidity
Bradykinesia
mask-like expression of the face
Postural Instability
Walking or Gait Difficulties
Dystonia
Vocal Symptoms
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
What Are The Treatment Options For Parkinsons Psychosis

Because Parkinson’s drugs can cause psychosis, your doctor will likely start by taking you off your medications, one at a time, or adjusting the dose. Changing your medication may make your movement symptoms worse.
Your doctor will keep adjusting your medication. The goal is to get you to a dose that improves your movement without causing hallucinations and delusions.
If changing your medication doesn’t work, the next step is to go on an antipsychotic medication. These drugs prevent psychosis symptoms by altering levels of chemicals in your brain.
Older antipsychotic drugs can make Parkinson’s movement symptoms worse. Newer drugs, called atypical antipsychotics, are less likely to affect your movement. These drugs are off-label, meaning they’re not approved to treat Parkinson’s specifically. They include:
- clozapine
- quetiapine
In 2016, the Food and Drug Administration approved pimavanserin . It’s the first drug designed specifically to treat Parkinson’s disease psychosis. Nuplazid reduces the number of hallucinations and delusions without affecting movement.
Nuplazid and other newer antipsychotic drugs do carry a black box warning. They can increase the risk of death in older people who have psychosis related to dementia. Your doctor will consider this and other risks before prescribing one of these drugs.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Treatment Options For Early Onset Parkinsons Disease
Parkinson’s treatment aims to slow the disease’s progression. Medication treatment options may include the following:
- Levodopa is a chemical that’s converted to dopamine in the brain. People with early onset Parkinson’s may experience more negative side effects, such as involuntary movements.
- MAO-B inhibitors can help reduce the breakdown of dopamine in the brain.
- Catechol-O-methyltransferase inhibitors can help extend Levodopa’s effects on the brain.
- Anticholinergics can help reduce tremors.
- Amantadine may be used to improve muscle control and relieve stiffness.
What Is Parkinsonism Is It Different From Parkinsons
Parkinson’s disease is the most common cause of parkinsonism, a category of neurological diseases that cause slowed movement.
No quick or easy diagnostic tests exist for Parkinson’s disease, so a patient may receive an initial diagnosis of parkinsonism without a more specific condition being confirmed.
Classic Parkinson’s disease — referred to as idiopathic because it has no known cause — is the most common and most treatable parkinsonism.
About 15 percent of people with parkinsonism have atypical variants, which are also known as Parkinson’s plus syndromes.
What Are The Different Stages Of Parkinsons Disease

Each person with Parkinson’s disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinson’s disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinson’s disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Parkinsons Disease And Sex Issues: Libido Sex Drive Emma-Marie Smith
Parkinson’s disease and sex is a complicated topic. No matter your age, gender or relationship status, sex plays a significant part in many people’s lives. Sexual desire does not go away with a diagnosis of Parkinson’s disease, and most people are perfectly able to continue having intimate relationships. However, you may experience changes to your libido or physical ability during sex. As with all Parkinsonian symptoms, it helps to be prepared so that you’re aware of your options. With this in mind, here’s what to expect from Parkinson’s disease and sex.
Tips For Caring For Someone With Parkinsons Disease
Caring for a loved one with early onset Parkinson’s can be difficult. If you’re a caregiver for someone with this condition, it’s important that you remember your own emotional and physical health.
Not only are you dealing with a difficult diagnosis, you’re also managing an increased number of responsibilities. Burnout is common in caregivers, so make sure you’re checking in with your own needs.
The Michael J. Fox Foundation Center for Parkinson’s Research recommends these tips for caregivers:
Research And Statistics: Who Has Parkinsons Disease
According to the Parkinson’s Foundation, nearly 1 million people in the United States are living with the disease. More than 10 million people worldwide have Parkinson’s.
About 4 percent of people with Parkinson’s are diagnosed before age 50.
Men are 1.5 times more likely to develop the disease than women.
What Is Parkinson’s Disease Its A Movement Disorder

Parkinson’s disease is a progressive brain illness that affects the way you move. In more clinical terms, Parkinson’s disease is a neurodegenerative disorder of the central nervous system.
Normally, there are cells in the brain that produce a chemical called dopamine. Dopamine sends signals to the parts of your brain that control movement. When approximately 60-80% of the dopamine-producing brain cells are damaged, symptoms of Parkinson’s disease appear, and you may have trouble moving the way you want.
Parkinson’s disease is a chronic illness and it slowly progresses over time. While there is no therapy or medicine that cures Parkinson’s disease, there are good treatment options available that can help you live a full life.
A Day In The Life Of A Parkinsons Disease Sufferer
A Typical Morning
What is Parkinson’s disease?
Parkinson’s disease is largely thought of as a condition of affecting motor control. James Beck, PhD, vice president of scientific affairs for the Parkinson’s Disease Foundation , says that while every case is different, the four cardinal signs of the disease are tremor, muscle rigidity, bradykinesia or akinesia , and problems with walking and balance. These symptoms occur as cells in a part of the brain known as the substantia nigra begin to die off, for reasons that remain unknown. These cells produce an important chemical neurotransmitter known as dopamine. Without dopamine, the brain is unable to control muscle movement. But dopamine is so much more than that. You may have heard it referred to as the “happiness” neurotransmitter, so it’s no surprise that two of the non-motor symptoms of Parkinson’s disease are depression and apathy. Add to that pain from rigid muscles, blood pressure instability, drooling, sweating, constipation, impaired cognition, and absolutely crushing fatigue, and you’ve got yourself a disease that affects just about every facet of life. “A person with mid-stage Parkinson’s disease walking around may look like they are drunk,” says Dr. Beck. “They commonly have slurred speech, and swallowing is another problem, which can contribute to drooling. This constellation of motor effects looks like drunkenness, but their minds are clear.”
Treatment for Parkinson’s
Getting Help
Is There A Way To Slow The Progress Of Parkinson’s
Parkinson’s disease is a progressive disorder, which means its symptoms worsen slowly over time. There is no cure for Parkinson’s disease yet and no known way to slow its progress.
But there are treatments and medications that can control or reduce the symptoms and help people live productive lives. Some research suggests that regular exercise may slow the progress of Parkinson’s. Physical activity can also alleviate stiffness and other symptoms.
There are other things a person can do to feel better after a diagnosis of Parkinson’s, such as joining social support groups and learning as much as possible about the disease. It’s also important to make the home safer and less cluttered, since a person with Parkinson’s is more likely to fall.
While it’s not always easy, neurologists say a positive mindset can also help.
Tips For A Better Sex Life With Parkinsons Disease
- Communicate: Be open with your partner about your feelings and discuss your physical needs. If the topic of sex causes upset or arguments, it might be worth seeing a sex therapist.
- Consider changing your medication: If your medication is having an impact on your sex life, talk to your doctor about an alternative treatment. Your sex life is important, so it should be given as much attention and care as your general health and wellbeing.
- Be open with your doctor: Don’t be afraid to talk about sex with your doctor – that’s what your healthcare team is there for, and they will have dealt with these types of concerns before.
- Deal with fatigue and depression: Depression and fatigue can negatively impact your sex life, so look at ways of treating these symptoms. A combination of therapy and antidepressant medications may help, so talk to your doctor.
What It’s Like To Have Parkinson’s For 15 Minutes

I’m at a close friend’s wedding, waiting to give a speech. Public speaking always makes me anxious, but today it’s worse than usual: my hand is shaking noticeably and I can’t seem to make it stop. The loss of control is unnerving.
When I try to speak to a neighbour, my voice comes out in a whisper, even though it seems to take more effort. Soon, my upper arm feels tired. I tell myself I just need to relax and snap out of it. I pick up my spoon and fill it with soup, but this only makes the tremors more obvious, as the metal beats against the bowl.
For a moment, I have forgotten that I’m immersed in an interactive installation called Transports, created by Liam Jarvis and his team from the Analogue theatre company.
It aims to simulate the physical and psychological effects of the early stages of Parkinson’s disease by taking inspiration from body illusions, like the rubber hand trick, in which the brain accepts a fake limb as its own.
Exercise Is Vital For Managing Parkinsons Disease
Research shows that people with Parkinson’s disease who exercised a minimum of two and a half hours a week experienced a slower decline in quality of life. Regular exercise helps significantly with maintaining balance, mobility and the ability to accomplish daily tasks. Workouts that focus on flexibility, stretching, aerobic activity and resistance training such as tai chi, Pilates and dance are often the most appropriate.
Parkinsons Disease And Sex: What You Need To Know
There is no reason why you cannot continue to have a healthy sex life with Parkinson’s disease. However, studies suggest that around 70 to 80% of those with PD experience sexual dysfunction. These common sexual problems are believed to result from Parkinson’s medication side-effects and psychological issues.
Men and women experience different issues when it comes to Parkinson’s disease and sex. In men, common problems include erectile dysfunction, lower sex drive, premature ejaculation and inability to orgasm. Women may experience pain during intercourse, as well as lack of sexual arousal, inability to orgasm and reduced lubrication.
In addition, the motor symptoms of Parkinson’s disease can create physical challenges during sex. Many people with PD experience slowed movement and rigidity that makes any movement difficult. Tremors and involuntary movement can also occur during sexual activity.
What Are The Risk Factors For Parkinsons Disease
Risk factors for Parkinson’s disease include:
Genetics
People with a first-degree relative with Parkinson’s are at an increased risk for the disease — possibly as much as 9 percent greater.
Fifteen to 25 percent of people with Parkinson’s have a known relative with the disease, but a condition called familial Parkinson’s, which has a known genetic link, is relatively rare.
Age
The average age of onset is 60 years, and the incidence rises with advancing age. About 10 percent of people have “early-onset” or “young-onset” disease, which begins before age 50.
Gender
Parkinson’s affects about 50 percent more men than women, for unknown reasons.
Pesticide Exposure
Exposure to some pesticides has been shown to raise the risk of developing Parkinson’s.
Problematic chemicals include organochlorine pesticides like DDT, dieldrin, and chlordane. Rotenone and permethrin have also been implicated.
Fungicide and Herbicide Exposure
Exposure to the fungicide maneb or the herbicides 2,4-dichlorophenoxyacetic acid , paraquat, or Agent Orange may raise the risk of Parkinson’s.
The U.S. Veterans Health Administration considers Parkinson’s to be a possible service-related illness if the person was exposed to significant amounts of Agent Orange.
Head Injuries
Head injuries may contribute to the development of Parkinson’s in some people.
Coffee and Smoking
People who drink coffee or smoke tobacco have been found to have a lower risk of Parkinson’s disease, for reasons that remain unclear.
What Are The Types Of Parkinsons Hallucinations

Hallucinations can affect any of the five senses:
- Sight . Seeing something that isn’t there, such as insects crawling on the walls or a deceased relative.
- Hearing . Hearing voices or sounds that aren’t real.
- Smell . Smelling an odor that isn’t there, like cookies baking or a skunk’s spray.
- Feeling . Feeling imaginary things, like bugs crawling on your skin.
- Taste . Having a strange taste in your mouth that isn’t from something you’ve eaten or a medical condition.
Some people sense the presence of a person or an animal nearby. Others see real objects transform into other things — for example, a vase changes into a dog.
It’s more common to have hallucinations at night, when the darkness creates shadows. Hallucinations can last anywhere from a few seconds to a few minutes.
Early in the disease, most people with Parkinson’s psychosis have insight, which means they understand that what they’re experiencing isn’t real. Later in the disease, often people lose insight and believe that what they see, hear, or feel is real.
Early Symptoms Of Parkinson’s Can Be Overlooked
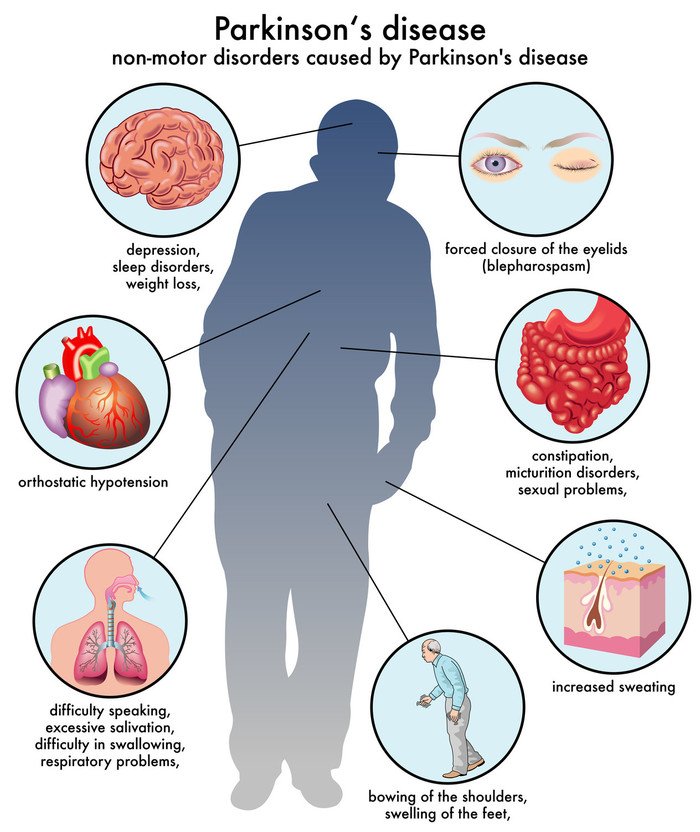
Symptoms of Parkinson’s disease are divided into 2 groups: motor symptoms and non-motor symptoms.
Early non-motor symptoms can be subtle and it’s possible to overlook them as signs of Parkinson’s: for example, anxiety and depression, fatigue, loss of smell, speech problems, difficulty sleeping, erectile dysfunction, incontinence and constipation. Another sign of Parkinson’s is handwriting that becomes smaller.
Motor symptoms of Parkinson’s can include tremor , slowness of movement , muscle rigidity and instability .
It’s possible for non-motor symptoms to start occurring up to a decade before any motor symptoms emerge. Years can pass before symptoms are obvious enough to make a person to go to the doctor.
There’s no ‘one size fits all’ when it comes to Parkinson’s disease — different people will experience different symptoms, and of varying severity. One in 3 people, for example, won’t experience tremor.
On average, 37 people are diagnosed with Parkinson’s every day in Australia. —Parkinson’s Australia
