Join The Parkinsons Forums: An Online Community For People With Parkinsons Disease And Their Caregivers
Chronic pain between the two groups was assessed using the Brief Pain Inventory , which measures pain severity , pain interference and pain frequency. A qualitative description of pain was also conducted.
Patients described pain as “exhausting,”“tiring,”“penetrating,”“miserable” and “unbearable” significantly more often than controls.
Among patients, those with depressive symptoms — as evidenced by a score of eight or higher in the Hospital Anxiety and Depression Scale — reported pain as tender more frequently than those without depression. Controls with depressive symptoms were more likely to report pain as stabbing, tender and tiring compared to those without evidence of depression.
“These descriptions indicate a significant impact of pain on the psychological well-being of the patient,” the researchers wrote.
Subsequent analysis showed that patients overall scored higher than controls in “worst pain felt since last week” and in global pain severity. Among all participants with depressive symptoms, those with Parkinson’s had higher scores of worst pain felt and average pain felt since last week, as well as higher reported pain levels at the time of assessment and global pain severity than those in the control group.
Symptoms of depression led to similar differences – plus an additional higher impact on social relations – between patients and controls. Of note, depression was associated with greater difficulties in walking in the group without Parkinson’s.
| 44.7 | 55.1 |
What’s Hot In Pd When Should You Start Medication Therapy For Parkinsons Disease
One of the most common questions that we receive on both on the Parkinson’s Foundation Ask the Doctor forum, and on the1-800-4PD-INFO Helpline is “when should I start medications for my Parkinson’s disease.” This months What’s Hot in PD column will focus on this simple, but critically important question.
The most important factor in initiating medications for an individual patient is whether Parkinson’s symptoms are affecting quality of life, or alternatively whether symptoms are affecting work performance. Bothersome Parkinson’s symptoms commonly include motor issues , and/or non-motor issues . Most experts agree that there is no benefit to delaying medication therapy if bothersome symptoms appear, and there may be risks in delaying treatment, especially if a treatment delay results in unsteadiness, falls, and fractures.
Over the last 10-20 years the thinking has evolved on when and how to initiate medication therapy for early Parkinson’s disease. Most experts agree that the medication dosage and the timing of the medication dosage should be carefully monitored in order to maximize the control of potentially responsive Parkinson related symptoms. The recommendation that patients should be started on dopamine agonist instead of levodopa has faded over the last decade, especially with the emergence of impulse control disorders and other dopamine agonist associated side effects.
What Are The Management Options For Canadians Living With Parkinsonism
There is currently no cure for Parkinson’s disease and most other parkinsonism cases. However, treatment options are available to help mitigate the symptoms and health impacts associated with these conditions. Most often the primary treatment is pharmacological, but it may also include other therapeutic options and, in the case of Parkinson’s disease, surgical interventions. Studies have shown that specially tailored exercise programs, supervised by physiotherapists or other trained professionals, may help affected individuals maintain or improve their physical functionality and general well-being.Footnote 2 Footnote 3 Footnote 4 Footnote 5
Box 1: What’s in the data?
The data used in this publication are from the Canadian Chronic Disease Surveillance System , a collaborative network of provincial and territorial chronic disease surveillance systems, led by the Public Health Agency of Canada . The CCDSS identifies chronic disease cases from provincial and territorial administrative health databases, including physician billing claims and hospital discharge abstract records, linked to provincial and territorial health insurance registry records using a unique personal identifier. Data on all residents eligible for provincial or territorial health insurance are captured in the health insurance registries.
Definition of diagnosed parkinsonism, including Parkinson’s disease, in the CCDSS
Parkinsons & Restless Leg Syndrome: Using Dopaminergic Medication
Treating Parkinsons Early With Levodopa Doesnt Affect Progression
No difference in disease progression was found whether levodopa, the most commonly prescribed drug to control symptoms in Parkinson’s disease, was initiated at the time of diagnosis or delayed, according to a study published online in the New England Journal of Medicine on January 24.
Is Early Treatment with Levodopa Safe?
Recently, doctors and researchers have been concerned that early use of levodopa could accelerate disease progression or increase long-term complications, such as involuntary movements and fluctuations of motor control, as well as the wearing-off of the drug’s effect or a delay in its effect.
In 2004, a clinical trial called Earlier versus Later Levodopa Therapy in Parkinson Disease , studied levodopa’s effect on the rate of progression and speculated that the drug either slowed progression or potentially delayed the appearance of symptoms.
Brain imaging data also revealed that levodopa either accelerates the death of dopamine-producing neurons or renders the protein responsible for transporting dopamine to brain nerve cells less effective by slowing down dopamine production. These results were inconclusive in determining whether levodopa affects the progression of Parkinson’s disease beyond helping to control motor symptoms.
Comparing Early versus Delayed Use of Levodopa
Early Levodopa Treatment Is Neither Protective nor Harmful
Future Trials Are Needed
What Should I Know About Storage And Disposal Of This Medication
Keep this medication in the container it came in, tightly closed, and out of reach of children. Store it at room temperature and away from excess heat and moisture .
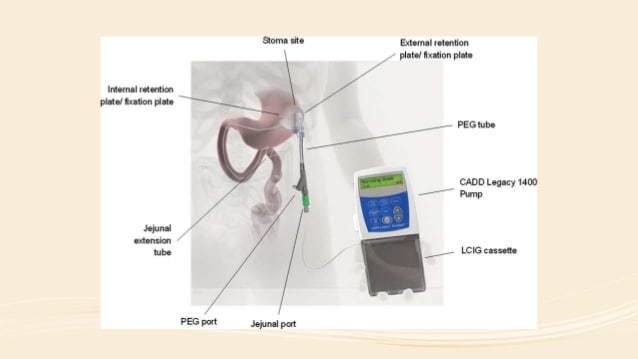
Store cassettes containing levodopa and carbidopa enteral suspension in the refrigerator in their original carton, protected from light. Do not freeze the suspension.
Unneeded medications should be disposed of in special ways to ensure that pets, children, and other people cannot consume them. However, you should not flush this medication down the toilet. Instead, the best way to dispose of your medication is through a medicine take-back program. Talk to your pharmacist or contact your local garbage/recycling department to learn about take-back programs in your community. See the FDA’s Safe Disposal of Medicines website for more information if you do not have access to a take-back program.
It is important to keep all medication out of sight and reach of children as many containers are not child-resistant and young children can open them easily. To protect young children from poisoning, always lock safety caps and immediately place the medication in a safe location – one that is up and away and out of their sight and reach. http://www.upandaway.org
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Tremors
Parkinsons Disease Therapy When To Start And What To Choose http://doi.org/10.17925/ENR.2008.03.02.34Article Information
Article:
Timing of Treatment
Treatment Choices
Levodopa
Dopamine Agonists
Non-ergot-derived dopamine agonists such as pramipexole, ropinirole, rotigotine patch and apomorphine injections are used widely as monotherapy and adjuvants to levodopa in PD. The older drug bromocriptine and other ergot-derived agonists such as pergolide and cabergoline are now rarely used due to an increased risk of fibrotic valvular heart and lung disease.18–20 A recent study by Moller et al. suggests a possible antidepressant action of pramipexole and beneficial effect on tremor when used as an adjuvant therapy to levodopa compared with placebo in advanced PD.21
Monoamine Oxidase-B Inhibitors
Anticholinergics/Catechol O-Methyltransferase Inhibitors/Amantadine
Levodopa versus Dopamine Agonists
Summary
Article Information:
Levodopa Treatment In Parkinsons Disease: Earlier Or Later Correspondence to:ti.gpinu@ittenrap.alliculCopyrightRandomized Delayed-Start Trial of Levodopa in Parkinson’s Disease.N Engl J Medcited by
The main limitation of the LEAP trial is represented by the high percentage of patients on placebo needing levodopa and the number of patients on levodopa who were shifted to the open-label treatment with the same levodopa dose during the phase I, making the results less powerful and more difficult to interpret.
When Should Levodopa Therapy Started In Parkinsons Disease
When should levodopa therapy be started in the treatment of Parkinsons Disease?
The mainstay in the treatment of Parkinsons Disease is the replacement of dopamine.
This therapy was introduced in the 1960s. Instead of using dopamine, which does not cross the blood–brain barrier, the current approach consists of combining levodopa and carbidopa.
Levodopa is transformed into dopamine, and carbidopa is a peripheral inhibitor of the enzyme dopa-decarboxylase.
The inhibition of this enzyme in the periphery, but not in the brain, decreases substantially the required levodopa dosage and the occurrence of gastrointestinal side effects .
In Europe and other countries, benserazide is available as an inhibitor of dopa-decarboxylase.
The effectiveness of levodopa may be limited by early motor fluctuations and dyskinesia attributed to nonphysiological stimulation of dopamine receptors by multiple and higher cumulative levodopa doses.
This effect is believed to occur more in younger Parkinsons Disease patients. A rational strategy is to start levodopa when the parkinsonian symptoms begin to impair activities of daily living or to interfere with social and occupational functioning.
A typical starting dose for carbidopa/levodopa is 25/100 mg tab, 1-2 tabs or 3 times/day.
Maintenance doses of 200 to 600 mg/day of levodopa may be needed in patients with moderately advanced PD.
Dosing Strategies With Conventional Levodopa Formulations
Because of the impracticality and considerable expense of enteral levodopa infusion, physicians generally rely on strategies designed to improve the delivery of oral levodopa to prevent motor complications. The standard approach is to alter the dosing regimen of conventional levodopa formulations, either by increasing the size of each levodopa dose or by “fractionating” the total daily levodopa dose into smaller, more frequent doses. While these modification strategies may be effective in the short term, they fail to address the issue of the short half-life of conventional levodopa in the long-term, and thus repeated modifications to the dosing strategy are often required.
Increasing the amount of levodopa administered at each dose does not eliminate troughs in plasma levels and may lead to an increased incidence and severity of dyskinesia . Levodopa dose fractionating is similarly ineffective at reducing troughs in plasma levels and is often associated with intermittent re-emergence of symptoms due to suboptimal levodopa exposure .
Vacuuming Parkinsons Disease And Chronic Lower Back Pain
When it comes to reinforcing the lower back, concentrating on your transverse abdominals which are twisted around the midline of your body is one of the very best means to do it. These muscular tissues are actually type in supporting your spine and lower back. While people frequently towards problems for their transverse abs, people can inadvertently throw out their lower back if their core isn’t solid sufficient.
Just how to do it: In a standing placement, take a deep breath and also attract your tummy switch in towards your spinal column, contracting as well as engaging your ab muscular tissues as you do so. Think of if someone was mosting likely to show up and punch you in the tummy as well as you want your intestine to be tough and also able to take it; that’s what it needs to feel like. Hold it, and also release gradually. Repeat a few even more times.
Resilience Is About How You Recharge Not How You Endure
really spoke to me about my own background in this context, about my pre-diagnosis lifestyle which I do believe contributed to my chronic illness, that perhaps led to my body saying no. Hence this may serve as an example of what we’ve discussed above. Indeed, I know many people with Idiopathic Parkinson’s Disease will also identify with life-long coping styles such as “thriving on stress”, not being able to sit still, never being able to just rest and relax for long periods.
What Are The Surgical Treatments For Parkinsons Disease
Levodopa Gold Standard Therapy For Parkinsons Disease
The choice of pharmacotherapy for PD has increased dramatically over the last 25 years as the understanding of the pathogenesis of PD has improved. Until the 1960s, drug treatment for PD was limited to anticholinergics, which had low efficacy and a high incidence of associated gastrointestinal and neuropsychiatric side effects . The introduction of levodopa had a dramatic impact, significantly reducing disability and mortality and increasing patient quality of life . Despite the emergence of a host of new dopaminergic therapies for PD, including dopamine agonists, dopamine reuptake inhibitors, and MAO-B inhibitors, levodopa remains the gold standard treatment for PD 40 years on.
When Is It Best To Start The Parkinsons Drug Levodopa

Earlier treatment with levodopa provides symptomatic relief to those with symptoms but does not appear to slow Parkinson’s disease from progressing. Therefore, timing is best determined by symptoms.
The treatment of Parkinson’s disease is complex. Levodopa is the main drug used to reduce tremors and muscle stiffness. Whether it modifies the course of the disease or becomes less effective over time is debated, and it can have side effects, so patients and clinicians sometimes prefer to delay starting treatment.
This Dutch trial involved 445 participants with a recent diagnosis of Parkinson’s disease, enrolled over five years. About half took levodopa for 80 weeks, and half placebo for the first 40 weeks and levodopa for the last 40 weeks. There was no difference in symptoms between the groups at the end of the study.
This evidence supports current guidance to start levodopa when symptoms begin to affect the quality of life and confirm that it has insufficient impact on disease progression to justify earlier treatment.
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
What Is Parkinson’s Disease Its A Movement Disorder
Learning How To Manage Daily Living With Parkinsons
Early stage
Mid stage
>>> Click Here For Effective Lower Back Pain Relief
Preliminary therapy in your home may include warm application as well as avoiding reinjury and heavy lifting. Prescription medicines that are sometimes utilized for severe lower back pain include non-steroidal anti-inflammatory medications, by shot or by mouth, muscular tissue relaxants,Long periods of inactivity in bed are no more recommended, as this therapy might actually reduce healing. Spinal adjustment for durations of up to one month has actually been discovered to be helpful in some clients who do not have indicators of nerve irritability.
Future injury is stayed clear of by utilizing back-protection strategies throughout activities and support devices as needed in your home or job.
Muscle Mass Strain and Ligament StrainA lower back sprain or pressure can happen all of a sudden, or can develop slowly with time from repetitive motions. Parkinson’s Disease And Chronic Lower Back Pain
Stress occur when a muscle is extended as well far and tears, harming the muscle itself.
Strains take place when over-stretching and tearing affects tendons, which connect the bones together.
For practical functions, it does not matter whether the muscle mass or tendon is damaged, as the symptoms as well as treatment coincide.
Usual causes of sprain as well as stress consist of:
While strains as well as stress do not appear major and do not typically trigger long-lasting pain, the acute pain can be fairly severe.
Does Having Rls Increase The Risk Of Developing Pd
When To Start Levodopa In Parkinson’s Disease
Dopamine is a neurotransmitter secreted from the substantia nigra, a small region in the brainstem that withers away in Parkinson’s disease. As natural dopamine levels in the brain begin to fall, signs of Parkinson’s disease appear. If dopamine is replaced, many of the symptoms improve.
One would think, then, that dopamine should be given as soon as possible. There are other options, though. In addition to given dopamine directly , Parkinson’s disease patients may benefit from a class of drugs called dopamine agonists. These are drugs that aren’t dopamine but have similar effects on the nervous system. Some physicians have argued that dopamine agonists should be used earlier in the disease’s course and that only elderly patients with at least moderate disability should receive levodopa.
When To Start Levodopa For Parkinsons Disease
![Pharmacology [CNS] 3](https://www.parkinsonsinfoclub.com/wp-content/uploads/pharmacology-cns-3-parkinsons-disease-treatment-part.jpeg)
Bottom Line: Treat symptoms early…or is it better to wait?
Sign up to be a Bottom Line Insider today!
Get The Latest Health, Life & Money Trends
Levodopa is the most effective medicine used to treat Parkinson’s disease. In fact, nearly everyone who has the disease will need it eventually. But there has long been a debate over whether it’s better to start the drug as soon as symptoms start—or hold out as long as possible to put off dealing with the risks associated with taking levodopa. New research now has the answer…
But first, some background…Parkinson’s disease is a progressive brain disease in which nerve cells in the brain that produce the chemical dopamine, a neurotransmitter needed to send signals between cells, gradually die. As the brain cells die, symptoms such as body tremors and slowed movement begin to interfere with daily activities. There is no cure for PD. Instead, symptoms are managed, typically with levodopa, a drug that converts to dopamine in the brain. Some research has found that starting levodopa soon after diagnosis—before symptoms curtail lifestyle—may slow progression of the disease. But other research has found that starting levodopa early actually may speed the loss of dopamine-producing brain cells…that the brain starts to depend more on drug-dopamine than on naturally produced dopamine. The resulting irregular brain levels of dopamine increase risk for dyskinesia, uncontrolled, jerky or writhing movement.
New Risk Factor for Parkinson’s
What Does Current Guidance Say On This Issue
The NICE guideline recommends levodopa as a first-line treatment in the early stages of Parkinson’s to control problems with movement if symptoms are affecting the quality of life. It does not discuss delayed treatment with levodopa.
If motor symptoms are not affecting the quality of life, the guideline recommends considering other drugs such as dopamine or monoamine oxidase inhibitors based on individual circumstances and preferences.
What Is The Treatment For Parkinsons Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
What Are The Symptoms Of Parkinson’s Disease
The main symptoms of Parkinson’s disease are:
Side Effects Of Taking Carbidopa/levodopa
I am newly diagnosed with Parkinson’s disease and just started on carbidopa/levodopa. However, I feel that the medication is making me feel worse than my original symptoms. Can carbidopa/levodopa make PD worse?
Carbidopa/levodopa can definitively have an array of side effects such as nausea, fatigue and dizziness. Your neurologist will try to find a dose that helps your PD symptoms, but does not cause side effects. Carbidopa/levodopa is probably not making your PD worse per se, but it sounds like overall, you are feeling worse on this dose than you did on no medication. You should discuss this problem with your neurologist who may consider changing your medication dosage.
My husband has had PD for about 10 years. Lately he has been having significant body, arm and finger movements after a dose of levodopa which improve just before the next dose. Is there any treatment for these abnormal movements?
I was advised to take my carbidopa/levodopa at least 30 minutes after a meal. However, this caused a lot of nausea and stomach upset for me, so I now take the medication with meals which is much better for me. Is this OK to do?
I noticed that I have increased trouble with my symptoms when I eat a meal containing protein. How do I adjust my diet to accommodate this?
Dietary protein can interfere with carbidopa/levodopa absorption in some people. This is known as the “protein effect.” The two ways to adjust your diet is to:
Symptomatic And Neuroprotective Therapy
Pharmacologic treatment of Parkinson disease can be divided into symptomatic and neuroprotective therapy. At this time, there is no proven neuroprotective or disease-modifying therapy.
Levodopa, coupled with carbidopa, a peripheral decarboxylase inhibitor , remains the gold standard of symptomatic treatment for Parkinson disease. Carbidopa inhibits the decarboxylation of levodopa to dopamine in the systemic circulation, allowing for greater levodopa distribution into the central nervous system. Levodopa provides the greatest antiparkinsonian benefit for motor signs and symptoms, with the fewest adverse effects in the short term; however, its long-term use is associated with the development of motor fluctuations and dyskinesias. Once fluctuations and dyskinesias become problematic, they are difficult to resolve.
Monoamine oxidase -B inhibitors can be considered for initial treatment of early disease. These drugs provide mild symptomatic benefit, have excellent adverse effect profiles, and, according to a Cochrane review, have improved long-term outcomes in quality-of-life indicators by 20-25%.
Neuroprotective therapy aims to slow, block, or reverse disease progression; such therapies are defined as those that slow underlying loss of dopamine neurons. Although no therapy has been proven to be neuroprotective, there remains interest in the long-term effects of MAO-B inhibitors. Other agents currently under investigation include creatine and isradipine.
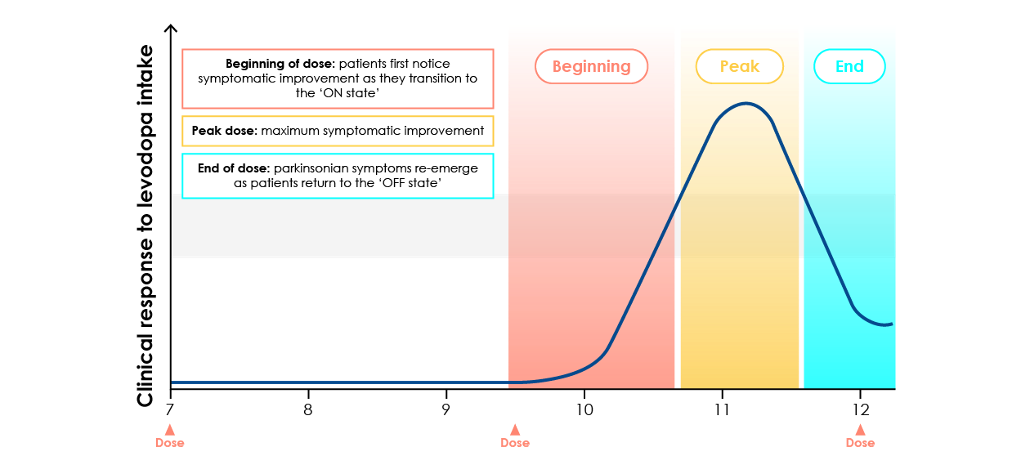
Fear Of Levodopa: Does It Stop Working
Short answer: All patients require increasing doses of levodopa over time and some develop on-off fluctuations, but this is not because the drug stops working.
Longer answer: The two major problems with levodopa are that, over time, many patients start to experience dyskinesia and on-off fluctuations, in which the drug does a relatively good job of controlling symptoms during certain times, but seems to stop working at other times, frequently near the end of the interval between doses. The transitions between the “on” and “off” states can be dramatic and sometimes very rapid, and clearly have a very negative impact on quality of life. For this reason, many patients, sometimes based on advice from their doctors, choose to delay the use of levodopa as long as possible, to try to “save” its use until it is really needed and delay the onset of on-off fluctuations.
This makes intuitive sense: If, for example, a patient started taking levodopa 8 years ago, and now she takes 5 times as much and has on-off fluctuations, the drug stopped working. Right?
Multiple clinical trials have addressed this question, and there is little evidence supporting the concept that levodopa loses effectiveness, simply as a result of prolonged use. To the contrary, the PD-MED clinical trial, which involved 1600 patients over many years , concluded:
Common Drugs For Parkinson’s Disease
Levodopa and carbidopa . Levodopa is the most commonly prescribed medicine for Parkinson’s. It’s also the best at controlling the symptoms of the condition, particularly slow movements and stiff, rigid body parts.
Levodopa works when your brain cells change it into dopamine. That’s a chemical the brain uses to send signals that help you move your body. People with Parkinson’s don’t have enough dopamine in their brains to control their movements.
Sinemet is a mix of levodopa and another drug called carbidopa. Carbidopa makes the levodopa work better, so you can take less of it. That prevents many common side effects of levodopa, such as nausea, vomiting, and irregular heart rhythms.
Sinemet has the fewest short-term side effects, compared with other Parkinson’s medications. But it does raise your odds for some long-term problems, such as involuntary movements. An inhalable powder form of levodopa and the tablet istradefylline have been approved for those experiencing OFF periods, OFF periods can happen when Parkinson’s symptoms return during periods between scheduled doses of levodopa/carbidopa.
People who take levodopa for 3-5 years may eventually have restlessness, confusion, or unusual movements within a few hours of taking the medicine. Changes in the amount or timing of your dose will usually prevent these side effects.
Dopamine agonists. These drugs act like dopamine in the brain. They include pramipexole , rotigotine , and ropinirole , .
What Other Information Should I Know
Keep all appointments with your doctor and the laboratory. Your doctor will order certain lab tests to check your response to levodopa and carbidopa.
Before having any laboratory test, tell your doctor and the laboratory personnel that you are taking levodopa and carbidopa.
Levodopa and carbidopa can lose its effect completely over time or only at certain times during the day. Call your doctor if your Parkinson’s disease symptoms worsen or vary in severity.
As your condition improves and it is easier for you to move, be careful not to overdo physical activities. Increase your activity gradually to avoid falls and injuries.
Levodopa and carbidopa can cause false results in urine tests for sugar and ketones .
Do not let anyone else take your medication. Ask your pharmacist any questions you have about refilling your prescription
It is important for you to keep a written list of all of the prescription and nonprescription medicines you are taking, as well as any products such as vitamins, minerals, or other dietary supplements. You should bring this list with you each time you visit a doctor or if you are admitted to a hospital. It is also important information to carry with you in case of emergencies.
What Should I Do If I Forget A Dose
Take the missed dose of the regular tablet, orally disintegrating tablet, extended-release tablet, or extended-release capsule as soon as you remember it. However, if it is almost time for the next dose, skip the missed dose and continue your regular dosing schedule. Do not take a double dose to make up for a missed one.
If you are using levodopa and carbidopa enteral infusion and will be disconnecting the infusion pump for a short time , other than the normal nightly disconnection, ask your doctor if you should use an extra dose before you disconnect the pump. If the infusion pump will be disconnected for longer than 2 hours, call your doctor; you probably will be advised to take levodopa and carbidopa by mouth while you are not using the suspension.
Data Extraction And Data Synthesis
For each included study, information about study type, patient characteristics, levodopa medication, nutritional intervention, results, and RoB was systematically extracted . To determine the role of dietary interventions in optimizing levodopa treatment, we strictly focused on outcome measures that are clearly related to levodopa treatment. The quality of studies is considered when weighing evidence and inferring conclusions. The latter is primarily based on studies with high or moderate quality.
