Sleep Disturbances Common In Parkinson’s Disease Can Be Early Indicator Of Disease Onset
- Date:
- IOS Press BV
- Summary:
- Up to 70% of Parkinson’s disease patients experience sleep problems that negatively impact their quality of life. Some patients have disturbed sleep/wake patterns such as difficulty falling asleep or staying asleep, while other patients may be subject to sudden and involuntary daytime sleep “attacks.” A new article discusses the underlying causes of sleep problems in PD, as well as medications, disease pathology, and comorbidities, and describes the most appropriate diagnostic tools and treatment options.
Up to 70% of Parkinson’s disease patients experience sleep problems that negatively impact their quality of life. Some patients have disturbed sleep/wake patterns such as difficulty falling asleep or staying asleep, while other patients may be subject to sudden and involuntary daytime sleep “attacks.” In the extreme, PD patients may exhibit REM-sleep behavior disorder , characterized by vivid, violent dreams or dream re-enactment, even before motor symptoms appear. A review in the Journal of Parkinson’s Disease discusses the underlying causes of sleep problems in PD, as well as medications, disease pathology, and comorbidities, and describes the most appropriate diagnostic tools and treatment options.
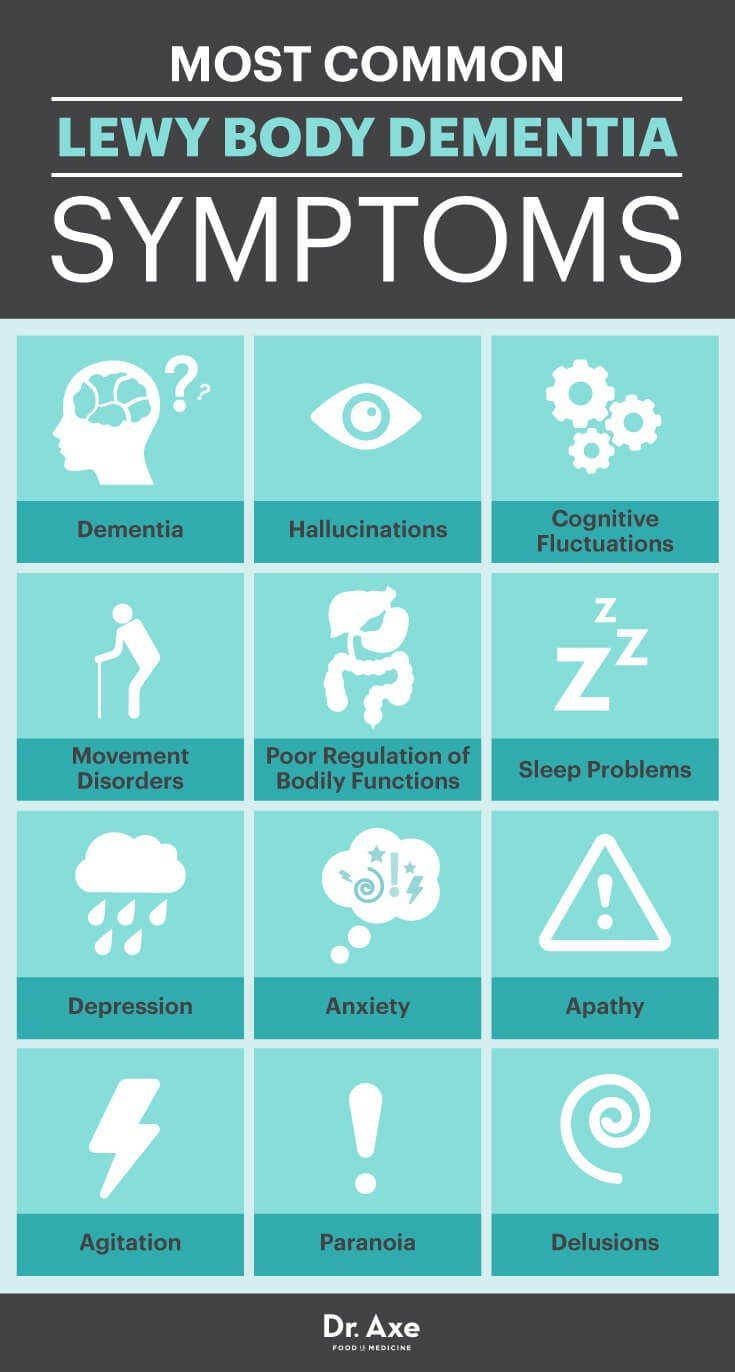
The presence of other conditions common in PD patients such as depression, dementia, hallucinations, and psychosis may interfere with sleep. Unfortunately, some antidepressants can also impair sleep.
Story Source:
Parkinson’s Disease Is A Nightmare Full Of Nightmares And One Women Is Waking Up
Through unfailing commitment — and a little luck — Helen Garvy stumbled upon a possible solution buried in a particular strain of cannabis. In doing so, she very well may have found an end to the living nightmares.
This article by Lex Pelger originally appeared on Van Winkles, the publication about sleep.
most important results are to be found in the mental sphere; as, for instance, in Senile Insomnia with wandering. An elderly person , is fidgety at night, goes to bed, gets up, thinks he has some appointment to keep, that he must dress and go out. Day, with its stimuli and real occupations, finds him quite rational again. Nothing can compare in utility to a moderate dose of Indian hemp at bedtime.
— Dr. John Russell Reynolds , leading neurologist and the personal physician to Queen Victoria
Imagine acting out a nightmare. You’re in the woods. You’re with your family. A wild animal appears — a wolf or a bear or a monster — and springs for you. Desperate and terrified, you’re forced to defend yourself and your loved ones with a furious violence. You fight tooth and nail and in one lucky maneuver you’re somehow able to position your hands around the beast’s throat. Then, you begin to wake up, groggy and confused, to find your hands clasped not around a wild dog but the throat of the person in bed with you.
Research Shows Bad Dreams Could Predict Future Memory And Thinking Problems
Researchers in Portugal have discovered that the content of dreams, particularly those with negative emotions, may predict long-term cognitive decline in people with Parkinson’s.
Results published in the Journal of Sleep Research have identified a link between dream content and future performance in cognitive tests – designed to test thinking, planning and memory – after 4 years.
Previous studies have shown that the dreams of people with Parkinson’s can include more aggressive content, being overall more vivid and nightmarish, than those of people without the condition.
Now researchers have reported that these kinds of bad dreams are significantly associated with future cognitive decline.
Rem Sleep Behavior Disorder With Parkinsons Disease Can Be A Nightmare J. Andrew Berkowski, M.D.
Acting out dreams could indicate REM sleep behavior disorder. What you should know about the symptoms, diagnosis and treatment.
Certain sleep disorders are common in people with Parkinson’s disease.
One of them — REM sleep behavior disorder — is a condition characterized by the acting out of dreams that are vivid, intense and violent. People have been known to yell or talk while asleep, carry on conversations or hit themselves or their bed partner. Even if physical damage does not occur, the condition can be frightening for the bed partner to witness.
REM behavior disorder does not necessarily disrupt the quality or quantity of sleep itself. But it is potentially harmful because of the physical movements involved.
What Types Of Sleep Problems Do People With Parkinsons Disease Have

Parkinson’s disease affects every person differently. It also impacts sleep in different ways. People with Parkinson’s may have:
- Insomnia, finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
How Are Sleep Problems Diagnosed In People With Parkinsons Disease
If you’re having problems sleeping, sit down with your healthcare provider to discuss the issue in detail. Your provider will ask you questions to better understand your symptoms.
Be prepared to explain when sleep disruptions happen and how they affect your life. Keeping a sleep journal for a few weeks can help you remember the details.
If your provider suspects you may have a sleep disorder, they may recommend you have a sleep study. This overnight test uses electrodes attached to your skin to track how your body functions when you’re sleeping.
What Is The Prognosis And Life Expectancy For Parkinson’s Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
How Are Sleep Problems Treated In People With Parkinsons Disease
Your provider will recommend treatments that address what’s causing your sleeping challenges. Your provider may:
- Change your medication: If a medication could be causing your sleep issues, your provider may decide to adjust your treatment plan. Reducing the dose or switching medicines may solve the problem.
- Prescribe a new medication or therapy: If you have a sleep disorder, your provider will discuss your options. In some cases, your provider may recommend a new medication. If you have sleep apnea, wearing a special oral appliance can help. The device enables you to get a steady flow of oxygen, so your body doesn’t gasp for air.
- Suggest lifestyle changes: Your daily habits and sleeping environment can help or hurt your sleep efforts. Setting regular sleep and wake times, keeping the room dark and avoiding electronic screens at bedtime may improve how well you sleep. If you have REM sleep disorder, your provider will discuss options for how best to protect you while you sleep.
Parkinsons Disease Linked To Sleep Disorders Sleep Disturbances

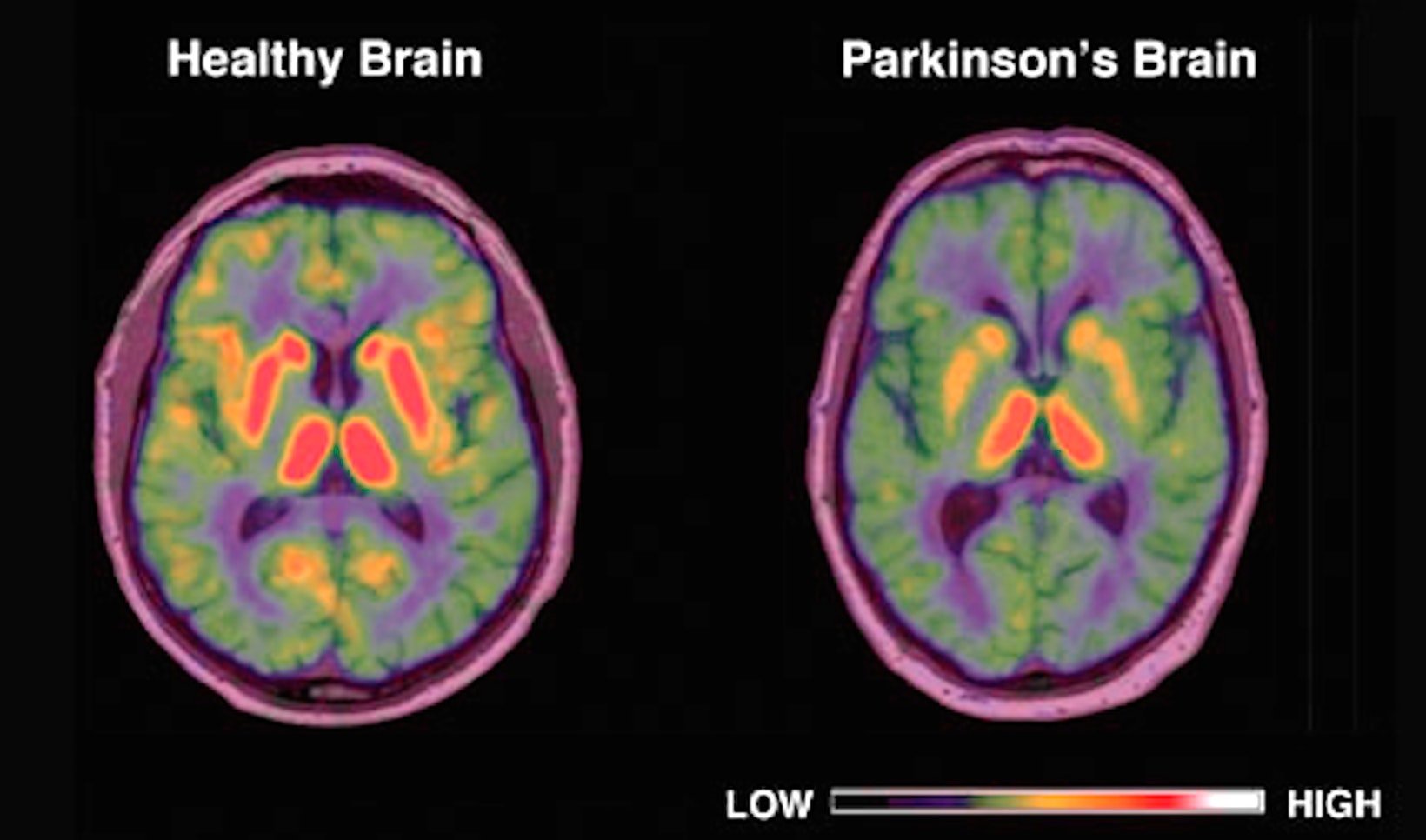
Parkinson’s disease has been linked to sleep disorders and sleep disturbances. Parkinson’s disease is characterized by the loss of brain cells that control movement. Symptoms of Parkinson’s disease can include tremors, stiffness, slowness of movements, as well as balance and coordination problems. Memory problems, depression, and sleep problems can all occur in Parkinson’s disease, too.
Sleep problems and sleep disorders may occur as an early sign of Parkinson’s disease, even before motor symptoms have started. Common sleep disorders experienced in Parkinson’s disease include insomnia, excessive daytime sleepiness, nightmares, sleep attacks, REM sleep behavior disorder , periodic leg movement disorder, restless leg syndrome, sleep apnea, and nocturia, which is frequent nighttime urination.
Rem Behavior Disorder Strongly Linked To Other Brain Disorders
It sounds too strange to be true, but it is actually possible for people to begin to act their dreams out. This can manifest in bizarre and astonishing ways. Though typically episodic, when dream enactment occurs it can cause serious harm to the afflicted person or a bed partner. These behaviors are most commonly associated with REM behavior disorder . Interestingly, these unusual episodes may predict the later development of other neurodegenerative conditions such as dementia and even Parkinson’s disease. Learn about the relationship between acting out dreams and the incidence of these subsequent neurodegenerative conditions.
Acting Out Dreams Is Often Early Sign Of Parkinson’s Disease
13 April 2015
A rare sleep disorder that makes people act out their dreams may be an early warning of a deadly neurological illness, a new review of previous research suggests.
About half of people who have a condition known as rapid eye movement sleep behavior disorder will develop Parkinson’s disease or a related disorder within a decade of being diagnosed with RBD.
Eventually, nearly everyone with RBD will ultimately develop a neurological disorder, the study found.
“If you get this disorder and live long enough, you will almost certainly get Parkinson’s disease or a condition similar to it — it’s an early warning sign,” said Dr. Michael Howell, a professor of neurology at the University of Minnesota in Minneapolis and co-author of the study, published today in the journal JAMA Neurology.
The main symptom of RBD is moving around during the rapid eye movement period of sleep, when most dreaming occurs and the muscles are usually paralyzed by the brain stem. People with RBD are thought to have a brain-stem malfunction that allows them to move during REM sleep, and thus act out their dreams, according to the study.
To find out whether RBD was, in fact, an early sign of Parkinson’s disease and similar brain disorders, Howell and his colleagues sifted through more than 500 studies on the subject published between 1986 and 2014.
The findings could help doctors find a way to treat Parkinson’s while it’s still in its early stages, Howell said.
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy “sleep hygiene” habits may also promote more restful sleep.
Do:
- Get outside during the day. Bright light tells your body it’s time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Don’t:
- Take long naps during the day.
- Use stimulants, such as caffeine, within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
Your Dreams Could Be An Early Clue To Parkinson’s Disease
![[Video] Parkinson’s Disease Psychosis with Dr. Christopher ...](https://www.parkinsonsinfoclub.com/wp-content/uploads/video-parkinsonatms-disease-psychosis-with-dr-christopher.png)
Breaking down Parkinson’s disease05:25
Actor Alan Alda revealed that he has Parkinson’s disease — and in an interview Tuesday on “CBS This Morning,” the award-winning actor said an unusual dream helped lead to his diagnosis.
Alda, best known for his portrayal of Army Capt. “Hawkeye” Pierce in the TV series “M*A*S*H, was diagnosed three and a half years ago after experiencing a lesser-known early sign of Parkinson’s. He said he asked his doctor to test him for the disease after reading an article about how physically acting out your dreams can be one of the earliest precursors of the neurological disorder.
“I asked for a scan because I thought I might have it,” Alda said. “I read an article by Jane Brody in The New York Times that indicated that if you have — if you act out your dreams, there’s a good chance that might be a very early symptom, where nothing else shows.” He recognized that it had happened to him.
“By acting out your dreams, I mean I was having a dream where someone was attacking me and I threw a sack of potatoes at them, and what I was really doing was throwing a pillow at my wife,” Alda explained.
At that point, he had no other sign of illness. “The doctor said, ‘Why do you want a scan? You don’t have any symptoms,'” Alda recalled. “And I said, I want to know if there’s anything I can do — I want to do it.”
Sleep Disorders In Parkinson’s Disease By Amer G Aboukasm
Although the daytime clinical manifestation of Parkinson’s disease have been well recognized for almost two centuries, the nocturnal symptoms, which occur in as many as 75% of patients and the associated sleep disorders were not studied until the 1960s. A variety of psychological and physiological processes can lead to disruption of the normal rhythm of the sleep-wake cycle in patients with Parkinsonism. First, the degenerative process in Parkinson’s disease affects the neurophysiological and neurochemical systems responsible for sleep organization, thus results in disruption of sleep. Second, the motor, respiratory and behavioral phenomena accompanying the disease may produce nocturnal symptoms. Third, the medication used in its treatment may induce new symptoms, such as nightmares or nocturnal movements. All these effects on sleep have implications for treatment planning.
How To Talk To Someone With Hallucinations Or Delusions
- It is usually not helpful to argue with someone who is experiencing a hallucination or delusion. Avoid trying to reason. Keep calm and be reassuring.
- You can say you do not see what your loved one is seeing, but some people find it more calming to acknowledge what the person is seeing to reduce stress. For example, if the person sees a cat in the room, it may be best to say, “I will take the cat out” rather than argue that there is no cat.
Page reviewed by Dr. Chauncey Spears, Movement Disorders Fellow at the University of Florida, a Parkinson’s Foundation Center of Excellence.
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication you’re taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldn’t be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Medications To Help Treat Parkinsons Disease Psychosis

Your doctor might consider prescribing an antipsychotic drug if reducing your PD medication doesn’t help manage this side effect.
Antipsychotic drugs should be used with extreme caution in people with PD. They may cause serious side effects and can even make hallucinations and delusions worse.
Common antipsychotic drugs like olanzapine might improve hallucinations, but they often result in worsening PD motor symptoms.
Clozapine and quetiapine are two other antipsychotic drugs that doctors often prescribe at low doses to treat PD psychosis. However, there are concerns about their safety and effectiveness.
In 2016, the approved the first medication specifically for use in PD psychosis: pimavanserin .
In clinical studies , pimavanserin was shown to decrease the frequency and severity of hallucinations and delusions without worsening the primary motor symptoms of PD.
The medication shouldn’t be used in people with dementia-related psychosis due to an increased risk of death.
Psychosis symptoms caused by delirium may improve once the underlying condition is treated.
There are several reasons someone with PD might experience delusions or hallucinations.
The Relationship Between Parkinsons Disease And Sleep
It’s unclear whether poor sleep causes parkinsonian symptoms to worsen or whether worsening parkinsonian symptoms cause poor sleep. In many cases it’s likely a case of bidirectionality, with each one exacerbating the other.
Fragmented sleep and sleep deprivation appear to leave the brain more vulnerable to oxidative stress, which has been tied to the development of Parkinson’s disease. Parkinson’s disease is not usually diagnosed until individuals have developed sufficient motor symptoms, by which time a significant portion of brain cells have already been damaged. If poor sleep quality or having sleep disorders foreshadows the development of parkinsonian symptoms, these could be useful in early diagnosis of the disease.
More research is needed to clarify the multifaceted relationship between Parkinson’s disease and sleep. A better understanding of this connection may offer medical experts the unique opportunity to screen at-risk individuals and perhaps delay the onset of the disease.
Parkinsons Should Be Treated Through A Team Approach
The Parkinson’s Foundation recommends people diagnosed with PD seek out a movement disorders specialist. These specialists are more likely to include other healthcare professionals who can help tackle day-to-day PD challenges in a care team, such as physical therapists, occupational therapists, speech therapists or nutritionists.
? Keep reading:Importance of Expert Care
Whats The Relationship Between Parkinsons And Sleep
Parkinson’s disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinson’s disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinson’s disease. These signs may include things like thrashing while you’re asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinson’s disease, a restful night’s sleep can be hard to find.
People With Parkinsons Can Have A Good Quality Life
There is no one-size-fits-all treatment approach when it comes to PD. While medication is the most common treatment, surgical therapy and lifestyle modifications, like rest and exercise, help manage the disease. Shop around until you find what works best. Find your ideal support group, therapist, exercise class and complementary therapy.
? Keep reading: Find resources in your area.
Parkinsons Sleep Problems: Diagnosis And Treatment
Parkinson’s disease is chronic and progressive, meaning it tends to get worse over time. However, there are treatment options that can help manage symptoms and allow patients to get more restful sleep.
The simplest way to start sleeping better with Parkinson’s disease is by adopting healthy sleep habits. Sleep hygiene tips for Parkinson’s disease sufferers include:
- Sticking to regular bedtimes
- Following a consistent bedtime routine with soothing activities such as listening to music or reading a calming book
- Getting regular exercise, preferably early in the day
- Getting adequate exposure to light, whether outdoors or through light therapy
- Avoiding long naps and naps late in the day
- Creating a cool, dark, and comfortable sleeping environment
- Restricting bedtime activities to sex and sleep only
- Turning off screens an hour before bedtime
- Reducing liquid intake before bedtime
- Avoiding caffeine, alcohol, and tobacco
- Eating a healthy diet and avoiding large meals at night
Light therapy, exercise, and deep brain stimulation have been successfully used to improve overall sleep quality and to treat specific conditions, such as REM sleep behavior disorder, in patients with Parkinson’s disease. Cognitive behavioral therapy for insomnia has proven effective at reducing insomnia in healthy adults, although further research is needed on the effects of CBT in patients with Parkinson’s disease.
- Was this article helpful?
Evaluation Of Sleep Hygiene Program: Sleep Diary
Monitoring the effectiveness of behavior changes is best done by keeping a diary. The table below depicts a sample diary that could be kept by the bedside and filled out upon arising by the patient or caregiver. If daytime sleepiness and napping are problems, items can be added to record the number, time, and duration of napping episode. The diary can be carried with the patient.
How Does Parkinsons Disease Cause Sleep Problems
Researchers have yet to uncover every nuance of the Parkinson’s and sleep connection. So far, medical experts believe several causes may contribute:
- Chemical changes in the brain: Ongoing research shows that Parkinson’s disease may disrupt sleep-wake cycles. Changes to certain brain chemicals may cause people with Parkinson’s to get less sleep.
- Medication: Some drugs that treat Parkinson’s disease may make it harder to fall or stay asleep. A medication may also disrupt your sleep patterns by making you drowsy during the day .
- Mental health challenges: People with Parkinson’s commonly deal with mood disorders, such as anxiety or depression. Any mood disorder may keep you up at night or make you sleep less soundly.
- Parkinson’s symptoms: Pain, waking up at night to pee or other Parkinson’s symptoms can make restful sleep harder to come by. Sleep apnea can also disrupt sleep.
Why Do Parkinsons Patients Have Trouble Sleeping

Despite having daytime tremors, Parkinson’s patients do not shake in their sleep. However, both Parkinson’s disease itself and the medications used to treat it can give rise to a number of sleep problems that lead to insomnia and excessive daytime sleepiness.
Patients with motor symptoms may have trouble adjusting sleeping positions to get comfortable. Others may experience distressing nocturnal hallucinations when trying to fall asleep. These may be a result of medications or cognitive impairment.
In turn, excessive daytime sleepiness may occur as a consequence of sleeping poorly at night. It may also be triggered by medications. Parkinson’s patients who suffer from EDS may be at a higher risk of accidents and unable to safely carry out activities such as operating a motor vehicle.
Since insomnia frequently goes hand-in-hand with anxiety and depression, it may be a contributing factor to sleep problems in people with Parkinson’s disease. For that reason, doctors often look for mental health disorders in people with Parkinson’s disease who have sleep problems.
The Development Of Other Degenerative Conditions
The behaviors associated with RBD can occur decades prior to the onset of other neurodegenerative changes. In fact, it seems that the majority of those afflicted with RBD will go on to develop other conditions. In particular, Parkinson’s disease, Lewy body dementia, and multiple system atrophy seem to be associated with RBD. It may take years — sometimes even decades — before these other conditions develop. In some individuals, the other disorders may never fully manifest as death occurs due to other causes.
Though not all go on to develop the other associated conditions, it occurs with a high frequency. More than 80% of people with RBD go on to develop Parkinson’s symptoms, for example. Though also commonly seen early in the other two conditions, far fewer will go on to develop these disorders.
It is important to obtain an accurate diagnosis of the behaviors. Other parasomnias may also manifest with movements during sleep. Certain medications, including antidepressants and anticholinergics, may provoke sleep behaviors. In addition, there are other medical disorders such as multiple sclerosis, narcolepsy, and stroke that might result in RBD.
Nighttime Hallucinations Psychosis & Confusion
Nighttime hallucinations and confusion may result from any combination of cognitive impairment, dopaminergic medications, age and PD-related vision changes and lack of sleep. Psychosis may first appear after infection, trauma, surgery or prolonged hospitalization. Symptoms may range from a sensation that someone or something is standing at the side of or behind the person, to very detailed and often frightening visions. Delusions may occur as well.
Treating Parkinson’s Psychosis
The first-line approach to treatment of PD psychosis involves simplification of the anti-PD medication regimen and adjusting dose timing , treating other sleep disturbances, providing a consistent and familiar sleep environment , and in more severe cases, the use of atypical antipsychotic drugs.
Most of the available anti-psychotics are always avoided in PD psychosis because they block dopamine receptors and can cause significant problems with movement. However, two anti-psychotic medications, quetiapine and clozapine, are sometimes used as they have less of an ability to worsen motor symptoms. However, data for the use of quetiapine is limited and clozapine requires the patient to undergo frequent blood draws to monitor blood counts. A newer medication pimavanserin, was approved by the FDA to treat PD psychosis. It has a different mechanism of action, and does not block the dopamine system, but rather the serotonin system, and therefore does not increase motor symptoms.
Phenomenology Of Dreams In Parkinson’s Disease
NeuroHealth Parkinson’s Disease and Movement Disorders Center, Warwick, Rhode Island, USA
Department of Psychiatry and Human Behavior, Brown Medical School, Providence, Rhode Island, USA
Department of Psychiatry and Human Behavior, Brown Medical School, Providence, Rhode Island, USA
Butler Hospital, Providence, Rhode Island, USA
NeuroHealth Parkinson’s Disease and Movement Disorders Center, Warwick, Rhode Island, USA
Department of Clinical Neurosciences, Brown Medical School, Providence, Rhode Island, USA
NeuroHealth Parkinson’s Disease and Movement Disorders Center, Warwick, Rhode Island, USA
Department of Psychiatry and Human Behavior, Brown Medical School, Providence, Rhode Island, USA
Department of Psychiatry and Human Behavior, Brown Medical School, Providence, Rhode Island, USA
Butler Hospital, Providence, Rhode Island, USA
NeuroHealth Parkinson’s Disease and Movement Disorders Center, Warwick, Rhode Island, USA
Department of Clinical Neurosciences, Brown Medical School, Providence, Rhode Island, USA
What Is The Treatment For Parkinson’s Disease

There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with carbidopa , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, constipation, dizziness, hallucinations, and nausea.
How Might Parkinson’s Affect Bladder Problems
Bladder difficulties can be common in Parkinson’s, particularly in the later stages of the condition. The loss of dopamine and the resulting interruption of signals from the brain can mean that messages telling the bladder to retain or expel urine are disrupted.
However, it is important to stress that bladder problems are not inevitable in Parkinson’s. If difficulties do arise, especially in older people, they may be caused by factors totally unrelated to the condition, so a thorough medical evaluation should be carried out with any appropriate tests.
Bladder problems associated with Parkinson’s include:
How Common Is Parkinson’s Disease Psychosis
Between 20-40% of people with Parkinson’s report the experience of hallucinations or delusions. When followed as the disease progresses over the years, this number increases. The increase does not mean that the hallucinations are persistent across the majority of patients. However, it is important to note that these statistics sometimes include “delirium,” in which the symptoms are temporary due to medication that needs to be adjusted or infection that needs to be treated, and “isolated minor symptoms” or “minor hallucinations,” including illusions, where instead of seeing things that are not there , people misinterpret things that are really there. These are the most common types of psychosis in people with PD, with different studies placing the occurrence between 25-70% of people with Parkinson’s. Typically, if the person with PD only has these minor hallucinations, their doctor will not prescribe an antipsychotic medication, though more significant psychosis that requires medication may develop over time. In one study, 10% of those with minor hallucinations had their symptoms resolved within a few years, while 52% saw their symptoms remain the same and 38% saw their psychosis symptoms get worse.
We recommend that people with Parkinson’s not use a single percentage to represent the prevalence of hallucinations and PDP. Parkinson’s is a complex disease and as it progresses the percentages and risk of symptoms will change.
Increased Feelings Of Anxiety Or Depression
Anxiety and depression have been linked to Parkinson’s. In addition to movement problems, the disease can also have an impact on your mental health. It’s possible that changes in your emotional well-being can be a sign of changing physical health as well.
If you are more anxious than usual, have lost interest in things, or feel a sense of hopelessness, talk to your doctor.
Sleep Disturbances In Parkinson’s Disease

In general, research seems to indicate that people with Parkinson’s disease have more sleep disruptions than similarly aged people without the disease. The most commonly reported sleep-related problems are the inability to sleep through the night and difficulty returning to sleep after awakening, generally referred to as maintenance insomnia. Unlike many older adults, patients with Parkinson’s disease often find that they have no trouble initiating sleep, but often wake up within a few hours and find sleeping through the rest of the night to be difficult. People with Parkinson’s disease also report daytime sleepiness, nightmares, vivid dreams, nighttime vocalizations, leg movements/jerking while asleep, restless legs syndrome, inability to or difficulty turning over in bed, and awakenings to go to the bathroom.
Although all the reasons for these sleep changes are unknown, potential explanations include reactions to/side effects of medications and awakening due to symptoms such as pain, stiffness, urinary frequency, tremor, dyskinesia, depression and/or disease effects on the internal clock.
When Should I Call My Healthcare Provider
Reach out to your provider if trouble sleeping harms your quality of life. Always call your healthcare provider if you experience symptoms that worry you, especially if they could put you or those around you in danger.
Sometimes, a sleep disturbance could be a sign of depression related to Parkinson’s disease. If you’ve lost interest in activities you once loved or feel numb to what’s going on in your life, reach out to a provider you trust. Some people feel better after starting a new medication or talking to someone about what they’re feeling. You don’t have to feel like this.
A note from Cleveland Clinic
Researchers continue to study the sleep-Parkinson’s disease relationship. Understanding more about how Parkinson’s affects sleep may lead to earlier detection of Parkinson’s disease and more effective treatments. Even now, you have plenty of options to treat sleep problems. Be open with your provider about any sleep issues you’re having. Together, you can find a plan that improves your sleep as well as any other challenges Parkinson’s disease may create in your life.
