Have You Ever Thought How Challenging Drinking A Glass Of Water Can Be For Someone Suffering From Parkinsons Disease
On World Health Day, you’ll likely read about how healthy habits like exercising or drinking more water, can improve your health. While these are helpful tips and important topics to cover, we decided to take things a step further. What if you couldn’t drink that glass of water by yourself? It can be daunting to consider, but this scenario can become all-too-real for a person suffering from Parkinson’s disease. There are 10 million people in the world suffering from this disorder; which is why, today, we decided to share with you how Parkinson’s Disease can affect mobility and balance, and what can be done when the disorder is detected in its early stages. That is why raising awareness for this degenerative disease is important, and, while there is still much research to be done, we have high hopes that researchers will find a way to reduce the symptoms of Parkinson’s disease, and eventually find a cure. This is becoming more and more urgent, given the fact that life expectancy is rising and the number of individuals with Parkinson’s disease will only increase in the future. But is there another solution in sight?
Request Brochure
Production Of Dopamine Neurons From Stem Cells: Could We Be One Step Closer To The Cure
As the disease progresses, people may experience reduced quality of life, if normal functions such as swallowing, start to be affected. Currently, there is no known cure for Parkinson’s disease. Once Parkinson’s is diagnosed, the symptoms can often be treated with medications and therapies, especially in the early stages. However, the scientific community is making every effort to find a way to cure or at the very least find more effective ways to lessen the symptoms of this physically impairing disease.
As we mentioned before, the disease primarily affects dopamine-producing brain cells or neurons. The good news is, scientists in Sweden have identified some insights and a set of markers that should help control the quality of stem cells engineered for clinical use to treat Parkinson’s disease. As the disease progresses and dopamine-producing brain cells malfunction and die, it leads to lower levels of dopamine, which is a chemical messenger essential for controlling movement. These findings should help fine-tune stem cell engineering to produce pure populations of high-quality dopamine neurons. Then, a pool of progenitor cells can be transplanted into the brains of patients, so they can make new supplies of dopamine cells.
But while this exciting new research is still in the lab, what else can we hope for to delay the symptoms of Parkinson’s and improve the quality of life of those suffering from the disease?
Identifying Newly Diagnosed Pd Patients And Matched Controls For Each Pd Patient
The study population comprised newly diagnosed patients with PD and their matched controls. First, we identified PD patients using the registration code for PD in the program for rare, intractable disease from January 1, 2004, to December 31, 2006, and we defined the index date as the date of the earliest claim with the V124 code. To remove any prevalent cases, we excluded patients who had PD diagnostic codes or PD registration codes before January 1, 2004. As the V124 registration criteria did not exclude atypical Parkinsonian syndromes, we excluded patients diagnosed with atypical parkinsonism during the entire study period, from 2002 to 2017. Moreover, we excluded patients under 40 years of age. Lastly, we excluded patients whose total number of days of antiparkinsonian medications was less than 180 days. The list of the antiparkinsonian medications used in this study is given in Supplementary Table .
Then, we selected up to four controls for each PD patient matched by sex and age at the index date. Previous studies reported that matching 4 controls to 1 patient can minimize the bias in measuring treatment effect in the maximum number of matched controls,. Individuals who had the registration code for rare, intractable disease for PD , had any diagnostic code for Parkinsonism , or had been prescribed an antiparkinsonian drug during the study period were not recruited as controls.
Research Is Underway To Further Understand The Cardiac Effects Of Parkinsons
It is possible to image the sympathetic nervous system of the human heart by injecting a radioactive tracer, meta-iodo-benzyl-guanidine, . Development of this technique, known as MIBG cardiac imaging, holds much promise as a test to confirm the diagnosis of PD , to identify those who are at risk of developing PD in the future, and to distinguish PD from related disorders. MIBG cardiac imaging is still considered an experimental procedure for detection of PD and is not yet in use as a clinical tool for this purpose.
A recent research study was conducted in monkeys in which the destruction of the sympathetic nerves of the heart was chemically induced to mimic the changes that are seen in PD. The cardiac system was then imaged using a number of new-generation radioactive tracers, which bind to markers of inflammation and oxidative stress. This model system may help to shed light on the molecular changes that accompany the loss of the sympathetic nerves of the heart and can also be used to track the response of the cardiac system to therapeutic agents.
Breathing Problems In Parkinsons Disease: A Common Problem Rarely Diagnosed

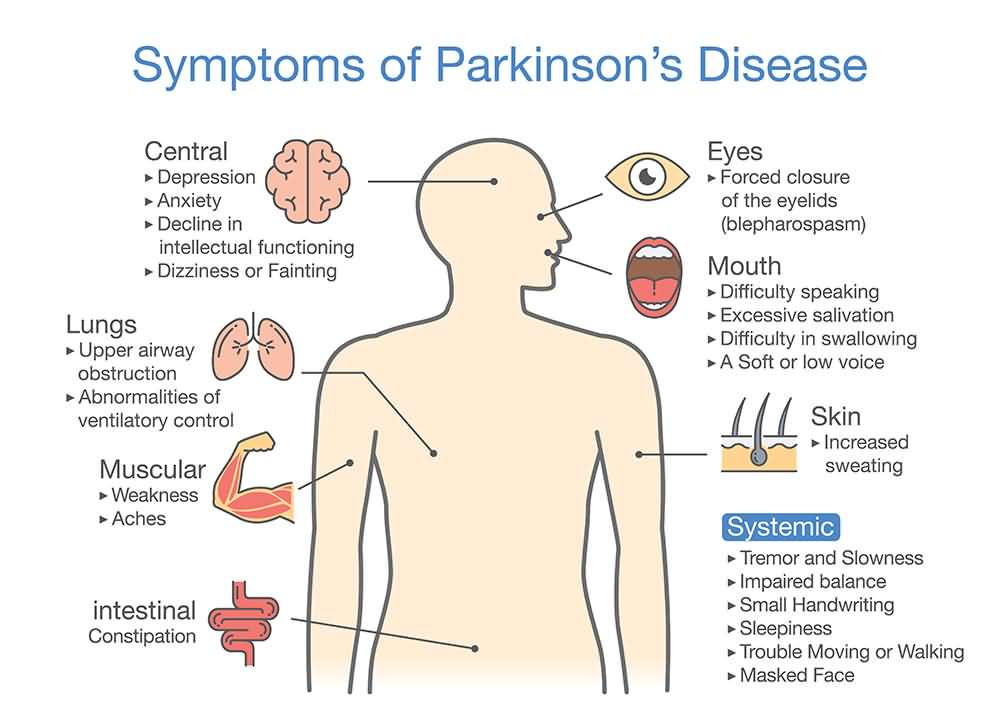
Parkinson’s disease is the second most common neurodegenerative disorder after Alzheimer’s disease. It is characterized by bradykinesia tremor, rigidity, and postural instability. Potential non-motor manifestations of PD include depression, anxiety, constipation, overactive bladder symptoms, dementia, and sleep disturbances.
Although James Parkinson, in 1817, described breathing abnormalities in his “Essay on the shaking palsy”, there has been limited research on this important non-motor symptom.
People living with Parkinson’s may present with a wide variety of respiratory symptoms, ranging from shortness of breath at rest to acute stridor. Shortness of breath can be very distressing for patients and clinicians alike. Multiple investigations may be undertaken, looking for infection, blood clots and heart problems. Although these potential causes of breathing abnormalities need to be excluded, clinicians must remember that PD itself and its medications can cause SOB; and that normal investigations should not automatically lead to a diagnosis of anxiety, depression or lead to inappropriate treatment plans.
Several different patterns of breathing abnormality may be found in PD:
KM Torsney, D Forsyth
How Parkinsons Disease Affects The Autonomic Nervous System And The Heart
In PD, there are two major reasons why the automatic control of the cardiac system is impaired. First, areas of the brain that control this system often contain Lewy bodies and have undergone neurodegeneration. In addition, the autonomic nervous system itself is directly affected by Lewy body-like accumulations and neurodegeneration. This means, when the baroreceptors in the heart and carotid artery sense a drop in blood pressure and try to generate a signal to the heart and blood vessels to increase the blood pressure, the message may not get through. This results in neurogenic orthostatic hypotension , or drops in blood pressure upon standing due to autonomic nervous system dysfunction. There are no medications that can cure nOH by restoring the autonomic nervous system in PD. nOH however, can be treated. Read more about nOH and its treatments here.
Structural problems of the heart such as coronary artery disease or cardiomyopathy are not thought to be part of the pathology of PD, although of course, could co-exist with PD.
How Can We Reduce Mobility Constraints In People With Parkinsons Disease
Over the last few decades, neuroscience has been providing us with exciting new findings regarding the effects of physical exercise on neuroplasticity , neuroprotection and slowing of neural degeneration. In fact, it has been proven that physical exercise can improve brain function in people with neurological disorders.
Aerobic exercise, such as treadmill training and walking programs, have been tested on individuals with Parkinson’s Disease and has been shown to improve gait and quality of life in general. However, the type of exercise chosen should take into account a specific program provided by a specialist. The exercise shouldn’t, by any means, put the patient’s physical integrity at risk, especially if the patient is a senior. In order to address complex mobility issues in people with Parkinson’s Disease, a therapist could incorporate tasks such as balance training into the patient’s rehabilitation. These are exercises that challenge sensorimotor control of dynamic balance and gait to improve mobility.
According to a study by Dr. Ergun Y. Uc, of the University of Iowa, the results suggest that
“walking may provide a safe and easily accessible way of improving the symptoms of Parkinson’s disease and quality of life.”
The Heart Of The Matter: Cardiovascular Effects Of Parkinsons Disease
It has long been understood that Parkinson’s disease does not just cause movement symptoms, but also causes a litany of non-motor symptoms with effects throughout the body. One of the organ systems that is affected is the cardiac system, encompassing the heart, as well as the major and minor blood vessels. I received this topic as a suggestion from a blog reader and we will be discussing this important issue today. Please feel free to .
Symptoms That May Be Related To Pd But That Few People Know About
People with PD and care partners may suspect that a particular symptom is related to PD, but they can’t find information about it, so they are not sure. Two symptoms that pop up in this category are runny nose and breathing problems, which we’ll focus on today. Of course, if these are new symptoms for you, they could be indicative of a new problem, including infection with COVID-19, so make sure to get yourself checked out by your doctor. However, if all else is ruled out, PD could be to blame. Excessive sweating and specific skin disorders are in this category as well and have been addressed previously.
How Can Parkinsons Disease Affect Mobility And Sense Of Balance
The neurophysiology of Parkinson’s Disease proves that it affects balance, gait, movement and can actually cause constraints on mobility. But what do we mean by mobility?
Mobility is a person’s ability to move safely in a variety of environments in order to accomplish functional tasks.
Functional tasks like drinking a glass of water or eating can become a problem. And if we think about it, mobility is something we take for granted most of the time. We don’t expect to lose it, and we don’t expect to get a degenerative disease, such as Parkinson’s. Therefore, being able to maintain good mobility is something of utmost importance as we age, and we must take preventive measures to delay mobility impairment as much as possible.
Mobility requires dynamic neural control, a sense of balance, and enough agility to be able to adapt to postural transitions as quickly as possible. What also concerns us today is the several types of mobility deficits caused by the progression of Parkinson’s Disease. We need to understand what preventive exercises and preventative measures can be taken to minimize the risk of falls and injury.
Parkinson’s Disease and fall prevention
While Parkinson’s is not life-threatening, people may experience life-threatening complications, such as choking on food or falling over. We must help our elderly loved ones prevent falls at any cost so that suggested exercise programs can work effectively in combatting the effects of Parkinson’s Disease.
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
How Are Mental Health Problems Treated In Parkinsons Disease
Mental health problems in Parkinson’s disease can be treated with a combination of medication, talking therapy and lifestyle changes. Your doctor may also suggest joining a Parkinson’s support group so that you can share your challenges with other PD patients.
Other ways to care for your mental health if you have Parkinson’s include:
Parkinson’s disease and mental health problems are not easily cured. However, there are a variety of treatment options and lifestyle changes that can boost your mental wellbeing and improve your overall quality of life.
Standard Protocol Approval Registration And Patient Consent

The study protocol was assessed and determined to be exempt from review by the Institutional Review Board of Seoul National University Hospital . Furthermore, the NHIS approved the use of its database and provided data after excluding all possible patient identification information . The requirement for informed consent was waived by the Institutional Review Board of the Seoul National University, because the database was anonymized. All methods were carried out in accordance with relevant guidelines and regulations.
Understanding The Neurologic Control Of The Cardiac System
Before we explore this issue, let’s first learn a bit about the autonomic nervous system and about the cardiac system’s place within it. The ANS is part of the peripheral nervous system, a network of nerves throughout the body. The ANS exerts control over functions that are not under conscious direction such as respiration, heart function, blood pressure, digestion, urination, sexual function, pupillary response, and much more. The ANS is further subdivided into the parasympathetic nervous system and the sympathetic nervous system. Both the parasympathetic and sympathetic nervous systems regulate most major organs. Often, they have opposite effects, with the sympathetic nervous system activating a system and the parasympathetic system calming it down.
One of the systems controlled by the ANS is cardiac regulation. Blood pressure sensors, known as baroreceptors, reside in the heart as well as in the carotid artery, the major artery in the neck. If the baroreceptors sense a change in the blood pressure, a signal is sent to particular areas in the brain. From there, the autonomic nervous system sends signals to the heart to control heart rate and cardiac output. Signals are also sent to the blood vessels to change the size of their diameter, thereby regulating blood pressure.
The Preponderance Of Injury In The Past Of People With Pd
Neck issues or damage can be caused by injuries, but the injury site doesn’t have to be local to the neck itself, since it is an integral part of the kinetic chain of the human body – problems anywhere else which affect posture can, in turn, profoundly affect how we tense our necks and cause strains on it by the way we are holding up the head. I’ve frequently asked people with Parkinson’s Disease to think carefully about any pains and injuries which they might have incurred either before or concurrent with their PD diagnosis. I’ve found that the overwhelming majority of us have suffered a prior accident or physical trauma. Injuries to jaw, neck, shoulders, back, hips, knees or feet predominate. All these severely affect posture and hence the kinetic chain and are liable to make our necks prone to permanent strains and stiffness. So in my view, even if chemical “cures” were invented tomorrow, people with PD would still present with the postural problems, still suffer from the old injuries which have been masked by the narratives of neurology, and would probably quickly decline into pain and problems again, unless these past injuries are properly attended to.
Other Symptoms To Spot For Potential Early Warning Signs
A telltale sign you have Parkinson’s is slight shaking or tremor in your thumb, finger, hand or chin, the health site says.
It adds: “A tremor while at rest is a common early sign of Parkinson’s disease.”
It is worth noting that a person with Parkinson’s disease can also experience a wide range of other physical and psychological symptoms.
According to the NHS, these include depression and anxiety, balance problems , loss of sense of smell , problems sleeping and memory problems.”
Parkinson’s Can Cause An Unusual Type Of Breathing Issue
- Dr. keith Roach
Dear Dr. Roach • My husband has Parkinson’s disease. He also has a stent in his heart. We have been to many doctors to address a breathing problem: fast breathing. He experiences this daily, and we are told that it is anxiety. It is difficult to watch him go through this. It sometimes happens before he is due for his Sinemet, but other times right after taking it.
He has been prescribed Xanax, clonidine, cannabidiol-infused gummies and a few others. One doctor says it is from Parkinson’s, but the rest say it is anxiety. — E.W.
Answer • Shortness of breath can have many causes, but someone with Parkinson’s disease has an unusual possibility, called “respiratory dyskinesia.” This is an involuntary rapid breathing that causes distress, and it usually happens an hour after taking a medication like Sinemet. Changing the dose can help with diagnosis, and working with a neurologist to adjust the dose of the Sinemet can solve the problem. I would start with an expert on Parkinson’s. Keeping a diary of when he takes his medication and when the breathing trouble starts and stops will be helpful, as would a video of what it looks like when happening.
Having Parkinson’s doesn’t make someone less likely to have other causes of shortness of breath, and anyone with a stent in the heart is at risk of developing further blockages. Poor blood flow to the heart is another potential cause. Get the Parkinson’s evaluation first.
.
What Happens When The Lungs Arent Working At Their Best
When the muscles and joints that work our breathing mechanisms become weak or stiff, the lungs become less efficient. This means a person may be short of breath and more easily tired when carrying out everyday tasks. Some people find it hard to cough strongly enough to clear phlegm, which can develop into a chest infection.
It might sound scary, but exercising the lungs is critically important for people with Parkinson’s. Pneumonia is the main reason people with the condition are admitted to hospital in an emergency, and respiratory complications, such as a chest infection or pneumonia, can be life-threatening.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinson’s disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable – reducing symptoms during “on” periods and no longer controlling symptoms during “off” periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they can’t. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinson’s disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare team’s efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinson’s disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein – glial cell-line derived neurotrophic factor, GDNF – to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
What Are The Causes And Symptoms Of Parkinsons Disease

As a neurodegenerative disorder, Parkinson’s Disease leads to the progressive deterioration of motor function due to loss of dopamine-producing brain cells. While the cause of Parkinson’s Disease is unknown, researchers speculate that both genetic and environmental factors are involved. Studies also show that men are 50% more likely to develop the disorder than women.
Primary symptoms of Parkinson’s Disease:
- tremor
- dementia
Clinical Evaluation To Assess Breathing Abnormalities
A physician should evaluate shortness of breath and any other breathing abnormalities. Potential causes of breathing difficulty include heart and lung conditions, which should be ruled out. People with PD often see general practitioners for medical care in addition to neurologists. It is important for such providers to be aware that PD and associated medications can cause shortness of breath.3
What Medications Are Used To Treat Parkinsons Disease
Medications are the main treatment method for patients with Parkinson’s disease. Your doctor will work closely with you to develop a treatment plan best suited for you based on the severity of your disease at the time of diagnosis, side effects of the drug class and success or failure of symptom control of the medications you try.
Medications combat Parkinson’s disease by:
- Helping nerve cells in the brain make dopamine.
- Mimicking the effects of dopamine in the brain.
- Blocking an enzyme that breaks down dopamine in the brain.
- Reducing some specific symptoms of Parkinson’s disease.
Levodopa: Levodopa is a main treatment for the slowness of movement, tremor, and stiffness symptoms of Parkinson’s disease. Nerve cells use levodopa to make dopamine, which replenishes the low amount found in the brain of persons with Parkinson’s disease. Levodopa is usually taken with carbidopa to allow more levodopa to reach the brain and to prevent or reduce the nausea and vomiting, low blood pressure and other side effects of levodopa. Sinemet® is available in an immediate release formula and a long-acting, controlled release formula. Rytary® is a newer version of levodopa/carbidopa that is a longer-acting capsule. The newest addition is Inbrija®, which is inhaled levodopa. It is used by people already taking regular carbidopa/levodopa for when they have off episodes .
Blood Sampling And Assessment Of Inflammatory Markers
All the patients underwent blood sampling by venipuncture of forearm veins.
Assessment of inflammatory markers
The serum concentrations of TBARS and thiol were measured in all the patients in order to detect lipid peroxidation and determine anti-oxidative defense capability, respectively . In addition, the level of EPCs was measured by flow cytometry based on a previous report . First, mononuclear cells were incubated for 30 min at 4 °C in a dark room with monoclonal antibodies against kinase insert domain-conjugating receptor and fluorescein isothiocyanate-conjugated CD34 and CD133, by which the EPC surface markers of CD133/CD34 and KDR/CD34 were determined. The control ligand was then added. Quantitative two-color flow cytometric analysis was performed using an Epics XL flow cytometer . In these arrays, each analysis included 10,000 cells per sample and was performed in duplicate, with mean level reported.
Assessment of serum adhesion molecules
To assess serum sICAM-1, sE-selectin, and sP-selectin levels, commercially available enzyme-linked immunosorbent assays were used . The dual wavelength absorbance, from which the degree of enzymatic turnover of the substrate was estimated, was measured at 450 and 620 nm. Absorbance was directly proportional to the concentration of antigens present. To determine the antigen concentrations of the unknowns, a standard curve of absorbance of standard antigen versus the given antigen concentration was plotted.
Parkinsons Disease And Mental Health: Whats The Link
The relationship between Parkinson’s disease and mental health is not straightforward. This is because, when it comes to the brain, no one is entirely sure what causes either Parkinson’s disease or mental illness. However, there is no evidence to suggest that a pre-existing mental health condition increases your risk of developing Parkinson’s disease . On the other hand, a diagnosis of Parkinson’s disease does make you more susceptible to developing mental health conditions.
Anxiety and depression are the most common mental health symptoms in people with Parkinson’s. Signs to look out for include:
- Changes in appetite, either eating too much or too little
- Excessive tiredness
- Lack of interest in hobbies and activities
- Feeling hopeless or “down” most days
- Feeling fearful or constantly worried
The mental health symptoms of Parkinson’s disease can also affect your physical symptoms and vice versa. For example, some people find that their anxiety increases when they have OFF episodes where their medication doesn’t work as well. Others report feeling depressed as a result of worsening symptoms.
If you’re struggling with the mental or emotional effects of Parkinson’s disease, you should talk to your doctor. He or she may suggest changing or adjusting your medication.
Effects Of Dopaminergic Therapy: Risk Or Protection
Studies have provided controversial results about the therapeutic effects of dopaminergic stimulation, and the role of drugs commonly used in the treatment of PD is still debated, strictly depending both on disease stage and administration modality.
Most papers strengthen the role of anti-Parkinsonian drugs as a protective factor against the development of respiratory failure. Levodopa increases inspiratory muscle function in anaesthetised dogs , and dopamine improves diaphragm function during acute respiratory failure in patients with COPD . In early stages, the levodopa equivalent daily dose does not correlate with pulmonary functional testing; as the disease progresses, anti-Parkinsonian medications may be responsible for the maintenance of the maximal inspiratory mouth pressure and sniff nasal inspiratory pressure . Accordingly, bedtime controlled-release levodopa is associated with less severe obstructive sleep apnoea in PD . Because dopamine is not known to increase muscle strength, it may ameliorate respiratory function by improving muscle coordination by a central activity .
Many authors have investigated the effect of dopaminergic therapy on aforementioned respiratory dysfunction, especially on obstructive and restrictive patterns .
Main findings of major studies we considered about the effects of dopaminergic drugs on respiratory parameters and respiratory dysfunctions
Abnormal Lung Function Found In Patients With Early
Results of a study on patients with early-stage Parkinson disease add to the evidence showing an association between PD and pulmonary function and point to the potential use of respiratory center drive to identify early PD.
Results of a study on patients with early-stage Parkinson disease add to the evidence showing an association between PD and pulmonary function and point to the potential use of respiratory center drive to identify early PD.
Prior research has shown that impaired pulmonary function is a nonmotor symptom of PD that increases disability in patients with PD, and respiratory complications are associated with greater mortality. However, most of the studies involved patients with advanced-stage PD. The researchers of the current study set out to investigate the link between pulmonary function and early-stage idiopathic PD, as well as the role of respiratory center drive, which is measured by airway occlusion pressure and is associated with the level of muscular activity when breathing in.
The study, published in Frontiers in Neurology, enrolled 43 patients with idiopathic PD and 41 healthy controls from the hospital at Tianjin Medical University in China. The patients had a mean disease duration of 1.67 years, and their mean total levodopa equivalent dose was 313.18 mg. The control participants were matched to the patients on age, sex, and body mass index.
Reference
The Gastrointestinal Effects Of Parkinson’s Disease
Surveys show that between 20% and 40% of people with Parkinson’s disease suffer from serious constipation . Larger numbers of people with PD have related gastrointestinal issues such as bloating, a feeling of fullness and nausea.?? As the disease progresses, all of these GI problems become more common. In rare cases, serious complications—such as megacolon and perforation or tearing of the colon—may arise from these GI problems.
The connection between the two may seem odd on the surface, but research shines some light on these unpleasant consequences of the disease.
A large survey of healthy people who were followed over several years revealed that men who reported having less than one bowel movement daily had a 2 to 7 times higher risk of developing PD than that of men who had daily bowel movements; their risk was four times higher than that of men who had two or more bowel movements a day.??
What Can Be Done About These Unpleasant Gi Problems
Unfortunately, research studies on GI problems related to PD have been few and far between, so doctors do not have any tried and true methods to deal with them. Some of the drugs to treat GI problems in people without PD cannot be used for those with PD because these drugs negatively impact dopamine systems in the brain.
If you have PD and experience constipation, it makes sense to try to use safe and simple methods to address this issue before you add new drugs to your daily regimen. Increasing dietary fiber and drinking lots of water and other fluids is a reasonable first step in treatment. If your doctor approves it, you might also consider taking fiber supplements, such as psyllium or methylcellulose. If these simple methods don’t work, your doctor might consider giving you a stool softener or a laxative.
