Directing Glance On Dopaminergic System Physiology: Can The Dopamine Be A Reliable Bridge Between Rls/wed And Pd

Dopamine is the most common catecholamine in the central nervous system that can modulate different functions, like movement, cognition, reward and motivation . DA derived from the conversion of 2,3-dihydroxyphenylalanine by the enzyme DOPA decarboxylase . Tyrosine hydroxylase is the enzyme responsible for converting the amino acid tyrosine to DOPA, monitoring the DA amount.
It is known that there are three groups of dopaminergic cells that give rise to three different axonal pathways with different functions: nigrostriatal, mesocorticolimbic, and tuberoinfundibular system. The latter is the smallest in terms of brain DA content and controls the pituitary system. Nigrostriatal DA pathway controls voluntary movement, and dysfunction in this pathway has been implicated in movement disorder like PD. Mesocorticolimbic systems DA modulate various cognitive/emotive functions, and their degeneration may lead to some psychiatric disorders. Several studies have pointed out that mesocorticolimbic system can also modulate thalamocortical arousal state . Studies from the effect of psychomotor stimulant with a molecular structure similar to DA, like amphetamine, , has demonstrated that endogenous DA is involved in promoting wakefulness .
Take into consideration his contribution to sleep-wake state in addition to other waking behaviors like movement, DA has been considered the “bridge” that underlying PD and RLS/WED .
Want To Learn More About The Latest Research In Parkinsons Disease Ask Your Questions In Our Research Forum
Having RLS in 2002 and/or 2008 was associated with a higher risk of constipation in 2012, compared with controls. Only individuals who had RLS in both 2002 and 2008 showed higher odds of having possible RBD alone, and both constipation and possible RBD in 2012, “indicating a potential association between continuous/recurrent RLS and ,” according to the researchers.
They cautioned that constipation is a relatively non-specific Parkinson’s symptom and may not indicate a direct link between RLS and Parkinson’s.
No differences were found between olfactory scores of men with or without RLS. However, the team noted that olfactory scores were only available from a subset of participants. Additionally, the timing of the smell sense analysis may also have influenced this result, since a loss of sense of smell has been reported as a relatively late symptom in the early stages of Parkinson’s compared with RBD and constipation, they said.
“We assessed the association between RLS and prodromal signs, but not between RLS and incidence. However, our focus was on identifying whether RLS is an early indicator of the underlying common disease process in ,” the authors wrote.
The findings warrant future studies for RLS and Parkinson’s incidence in the long-term, they said.
Among the study’s limitations, the authors mentioned that the link between Parkinson’s and RLS may differ by gender, since women, although they have a reduced risk for Parkinson’s, are more susceptible to RLS.
Interrupted Sleep: Exploring Links Between Parkinsons Disease And Restless Leg Syndrome
Restless Legs Syndrome and Parkinson’s disease have interesting dopamine connections. Some Parkinson’s pain may actually be restless legs or arms. Could changes in RLS treatment over the past few years be relevant to getting a good night’s sleep with PD?
To those unfamiliar with the condition, the terminology “Restless Legs” makes it difficult to accept as the serious condition that it is. Whenever I hear the term Restless Legs Syndrome, my brain thinks “ants in my pants”. I picture myself back in elementary school, being forced to sit at a desk, when I’d rather be running around outside. That is far from being an accurate description of this medical condition.
The USA National Institutes of Health describes RLS as follows:
I know the feeling all too well. Sitting anywhere for more than an hour or so where I can’t stretch/straighten out my legs leads to extreme pain that can usually be walked off with just a few minutes of movement. Gymnasium bleachers are the worst for me. I used to prefer bulkhead rows on airplanes, but now they can be painful because I cannot stretch my legs into the space under the seat in front of me. Movie theaters generally aren’t a problem, as the old theaters have been replaced by megaplexes that are focused more on comfy recliner seats. By contrast, traditional theatre can be torture…although an aisle seat usually provides me with enough wiggle room to endure until intermission.
What causes RLS?
According to the NIH:
Suggested further reading:
Is It Difficult To Diagnose Restless Legs Syndrome In People With Parkinson’s
Because there isn’t a specific test for restless legs syndrome, it can be difficult to diagnose the condition. Sometimes symptoms only happen briefly or from time to time.
Also, the condition can cause discomfort at night-time and this can be mistaken for arthritis in people with Parkinson’s.
Another reason why a person with Parkinson’s may experience disturbed sleep is due to dyskinesia. Dyskinesia is involuntary movements sometimes seen in people with Parkinson’s. If you’re concerned about this, speak to your GP, specialist or Parkinson’s nurse.
Your treatment will depend on how severe your symptoms are and what may be causing them.
Restless Legs Syndrome And Leg Motor Restlessness In Parkinsons Disease
Keisuke Suzuki
1Department of Neurology, Dokkyo Medical University, 880 Kitakobayashi, Mibu, Shimotsuga, Tochigi 321-0293, Japan
2School of Nursing, Dokkyo Medical University, Tochigi, Japan
3Department of Neurology, Dokkyo Medical University Koshigaya Hospital, Saitama, Japan
Academic Editor:
Abstract
1. Introduction
2. The Diagnosis of RLS
IRLSSG Consensus Diagnostic Criteria for Restless Legs Syndrome/Willis-Ekbom Disease
Essential Diagnostic Criteria . Consider the following:An urge to move the legs is usually but not always accompanied by, or felt to be caused by, uncomfortable and unpleasant sensations in the legs.The urge to move the legs and any accompanying unpleasant sensations begin or worsen during periods of rest or inactivity such as lying down or sitting.The urge to move the legs and any accompanying unpleasant sensations are partially or totally relieved by movement, such as walking or stretching, at least as long as the activity continues.The urge to move the legs and any accompanying unpleasant sensations during rest or inactivity only occur or are worse in the evening or night than during the day.The occurrence of the above features is not solely accounted for as symptoms primary to another medical or a behavioral condition .
3. The Pathophysiology of RLS
4. Imaging in RLS
5. RLS and PD
6. RLS Mimics in PD
7. Variants of RLS in PD
8. Leg Motor Restlessness in PD
9. Treatment of RLS and LMR in PD
10. Conclusion
Conflict of Interests
References
Copyright
Check Out David Wimbles Site Http://wwwrlcurecom/ For More Info On Rls
The current study assessed the prevalence and the clinical characteristics of RLS in a cohort of AD patients.
It concluded that RLS prevalence in AD cohort was estimated to be about 4%. RLS appeared to be associated with neuropsychiatric symptoms such as apathy. RLS and apathy might share a common pathophysiological basis represented by a dysfunction of the central dopaminergic system.
Methods: Three hundred and thirty-nine subjects with a diagnosis of AD were recruited. Cognitive, functional, and neuropsychiatric measures were collected at baseline and six-monthly for a 2-years follow-up
Results: Fourteen subjects met the RLS criteria. RLS subjects were more frequently male and younger than AD subject without RLS . MMSE, ADL and IADL were not significantly different. NPI total scores did not differ significantly, however, AD patients with RLS were found to be more apathetic than AD subjects without RLS.TALARICO, G., CANEVELLI, M., TOSTO, G., VANACORE, N., LETTERI, F., PRASTARO, M., TROILI, F., GASPARINI, M., LENZI, G. L., BRUNO, G. AMERICAN JOURNAL OF ALZHEIMER’S DISEASE AND OTHER DEMENTIAS28:165-170, 20131533-3175
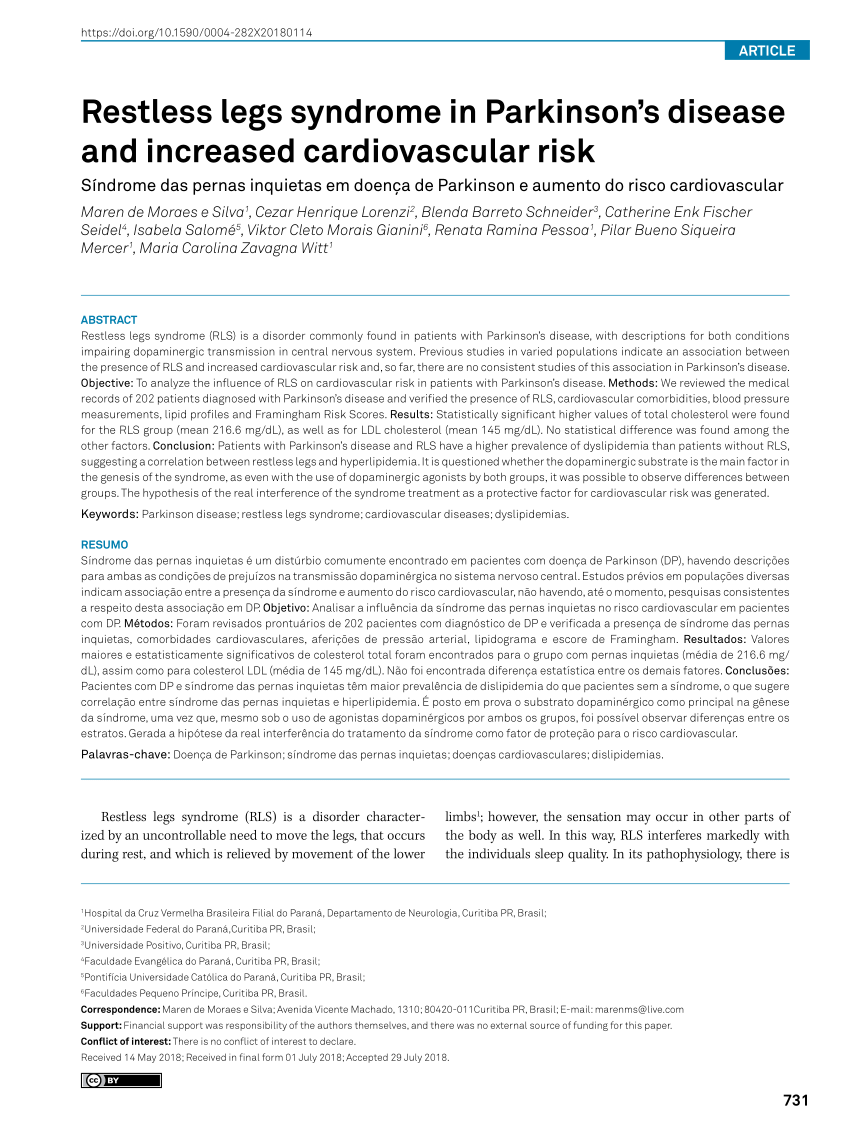
Restless legs syndrome and Parkinson’s disease
Tasneem Peeraully and Eng-King Tan. Department of Neurology, Singapore General Hospital, Outram Road, Singapore 169608, Republic of Singapore
Keywords:Parkinson’s disease; Restless-legs syndrome; Pathophysiology; Dopaminergic dysfunction.
————
Connie’s Comments
Detections Of The Levels Of Iron And Related Proteins In Csf And Serum
The levels of iron and related proteins, including ferritin, transferrin and lactoferrin in CSF and serum from PD patients were detected by Enzyme Linked Immunosorbent Assay. Ab83366 kit for iron, Ab108837 kit for ferritin and Ab108911 kit for transferrin were from Abcam Company . E01L0224 kit for lactoferrin was from Shanghai Lanji Biological Limited Company .
Is There A Link Between Restless Leg Syndrome And Parkinson’s Disease
Previous studies have suggested that there is a link between RLS and PD due to both conditions sharing the common feature of dysfunction in the part of the brain that produces dopamine. Another commonality between these two conditions is that they have been shown to run in the family. About half of the cases are in patients that have relatives with the disorder. Another argument for the medical linkage of these neurological disorders is that they share the same treatments – no other common disorder is treated with the same dopamine agents.
Even though earlier studies have shown a significant prevalence of RLS in patients with Parkinson’s, researchers have not been able to find a common patient demographic or Parkinson’s treatment to reliably predict the development of restless leg syndrome. Also through studies, they have found that though both conditions present dysfunction in the dopamine-producing neurons in the brain, the actual mechanisms, or how the neurons are affected, are not identical.
Earlier studies involved patients with advanced cases of Parkinson’s disease that have been taking dopamine drugs for years, which may account for the significance of RLS. The use of dopamine drugs makes it much harder to correctly diagnose restless leg syndrome. The dopamine can cause restlessness that may be confused with RLS.
Parkinsons & Restless Leg Syndrome: Using Dopaminergic Medication
Because RLS is well-treated by medications that also treat PD, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in PD, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that DaTscan results are not abnormal in RLS.
Using dopaminergic medications to treat RLS however can be tricky. In some people they can lead to a phenomenon known as augmentation, in which long term use of dopaminergic medications can worsen the symptoms – making them appear earlier in the day or migrating to the upper body in addition to the legs.
How Can I Get A Good Night’s Sleep Despite Restless Legs Syndrome
Experts agree that simply changing your behavior can often help you sleep if you have restless legs syndrome. For people with mild to moderate RLS, these steps can reduce or prevent symptoms:
- Cut down on caffeine.
- Stop smoking, or at least cut back.
- Go to bed and get up at the same time each day, including weekends.
- Exercise regularly, but moderately .
- Apply heat or ice, or soak in a hot bath.
Can Restless Legs Syndrome Develop Into Something More Serious
Most people with restless legs syndrome have the “idiopathic” form, meaning there’s no known cause. For them, there is no risk of RLS developing into something more serious, like Parkinson’s disease.
Restless legs syndrome can get worse in people with other medical conditions if they don’t get those conditions treated.
Detections Of The Levels Of Neurotransmitters In Csf And Serum
The levels of neurotransmitters, including DA, 5-HT, Ach and NE in CSF and serum from PD patients, were measured by high-performance liquid chromatography. Phenomenex 150?×?2?mm, 150?×?3?mm chromatographic column, and liquid chromatography tandem mass spectrometry 6410 instrument were from Agilent , and standard samples were from Sigma .
What Is The Prognosis For People With Restless Legs Syndrome
RLS is generally a lifelong condition for which there is no cure. However, current therapies can control the disorder, minimize symptoms, and increase periods of restful sleep. Symptoms may gradually worsen with age, although the decline may be somewhat faster for individuals who also suffer from an associated medical condition. A diagnosis of RLS does not indicate the onset of another neurological disease, such as Parkinson’s disease. In addition, some individuals have remissions—periods in which symptoms decrease or disappear for days, weeks, months, or years—although symptoms often eventually reappear. If RLS symptoms are mild, do not produce significant daytime discomfort, or do not affect an individual’s ability to fall asleep, the condition does not have to be treated.
Pathological Evidence Of Dopamine Dysfunction In Pd And Rls
Post-mortem studies in PD demonstrate loss of nigral neurons resulting in striatal dopamine deficiency, with differing morphological lesion patterns according to the clinical subtypes of PD. Cell loss in the ventrolateral part of the substantia nigra pars compacta projecting to the dorsal putamen is more prominent in the akinetic-rigid type, whereas tremor-dominant PD shows predominantly medial SNPC cell loss . Variability in lesion patterning might explain why some patients with PD may develop RLS. In addition, loss of dopamine 2 receptors has been documented in advanced PD .
At autopsy of 8 patients with primary RLS, there was a significant decrease in dopamine 2 receptors in the putamen compared to a neurologically normal control group. The decrease in the D2 receptors correlated to the severity of the RLS . This evidence that the nigrostriatal dopaminergic system is affected in both RLS and PD might provide a stronger argument for an etiologic link between the two. Moreover, there were significant increases in tyrosine hydroxylase in the substantia nigra, but not in the putamen of the RLS group. Phosphorylated tyrosine hydroxylase was found to be increased in both the substantia nigra and putamen. These findings are consistent with data from animal iron deficiency models demonstrating increased presynaptic dopaminergic activity .
Restless Legs Syndrome And Periodic Limb Movement Disorder
Most people who have RLS also have a condition called periodic limb movement disorder . PLMD involves repetitive flexing or twitching of the limbs while asleep at night. It is different from RLS in that these movements are not accompanied by uncomfortable sensations and because they occur during sleep, patients are often not aware of them. However, PLMD-associated movements can cause a person to wake up and therefore can compound sleep issues in patients who also have RLS.
Although most people with RLS have PLMD, many with PLMD do not have RLS.
Does Having Rls Increase The Risk Of Parkinson’s Disease
Restless Legs Syndrome is a neurologic and sleep-related condition characterized by an irresistible urge to move the legs. The symptoms respond to dopaminergic medications, which are also used to treat Parkinson’s disease , making an association between RLS and PD likely. Here we explore RLS and its potential connections with PD. This post was adapted from content originally written by Dr. J Steven Poceta, neurologist and sleep medicine specialist.
Characteristics of Restless Leg Syndrome:
The hallmark of RLS is a feeling of restlessness, usually in the legs. The restlessness is often accompanied by additional sensations such as tingling, “creepy-crawly” or electric sensations, usually located in the legs. The symptoms are usually not restricted to the toes or feet, as in peripheral neuropathy, but rather are present more generally in the legs, often the calves or thighs.
The restlessness is worse when the person is at rest or not moving. This feature makes it hard for people with RLS to get to sleep and can also interfere with the ability to sit still in order to read, relax, or do desk work.
Symptoms are improved with moving, particularly walking. Unfortunately, the relief lasts only as long as the movement continues, which makes some people “pace the floor” for hours when the condition is severe. Besides walking, sometimes providing other stimuli to the legs is helpful, such as rubbing, massage, or stretching.
Causes of Restless Leg Syndrome:
Treatment of RLS in PD:
When Should I See A Doctor About Restless Legs Syndrome
You should see a doctor to confirm the diagnosis of RLS and to exclude other conditions that may resemble RLS. The doctor can treat associated problems like iron deficiency.
If you have RLS, you should also see a doctor if you are:
- Feeling depressed or anxious
- Having trouble concentrating
You don’t have to wait until one of these things happens. If you just want to feel better, see your doctor.
Other Conditions Associated With Restless Legs Syndrome
The following medical conditions are also associated with RLS, although the relationships are not clear. In some cases, these conditions may contribute to RLS. Others may have a common cause, or they may coexist due to other risk factors:
- Osteoarthritis . About three-quarters of patients with RLS also have osteoarthritis, a common condition affecting older adults.
- Varicose veins. Varicose veins occur in about 1 in 7 patients with RLS.
- Obesity.
- Diabetes. People with type 2 diabetes may have higher rates of secondary RLS. Nerve pain related to their diabetes cannot fully explain the higher rate of RLS.
- Hypertension .
- Chronic obstructive pulmonary disease .
- Chronic alcoholism.
- Sleep apnea and snoring.
- Chronic headaches.
- Brain or spinal injuries.
- Many muscle and nerve disorders. Of particular interest is hereditary ataxia, a group of genetic diseases that affects the central nervous system and causes loss of motor control. Researchers believe that hereditary ataxia may supply clues to the genetic causes of RLS.
- Attention-deficit hyperactivity disorder .
- Psychiatric disorders, such as depression.
The Link Between Rls And Parkinsons: Dopamine Agonists
Although the cause of RLS remains unknown, we know that RLS runs in families in about one-half of the cases, and that some families have an abnormality on chromosome 12. Because RLS is well treated by medications that also treat Parkinson’s disease, it is likely that some aspect of brain dopamine function is altered in RLS. However, unlike in Parkinson’s disease, in which the deficit in substantia nigra dopamine-producing cells can be proven in many ways, no such abnormality has been shown in RLS. For example, studies show that there is no major deficit on PET or other imaging studies of the brain, as is there is in PD. The spinal fluid is normal in RLS, but shows low dopamine in PD.
Lastly, RLS does not progress to cause other major symptoms such as tremor, gait disorder, or loss of taste or smell, and does not progress to PD. In fact, one of the leading possibilities as the cause of RLS and for which there is good scientific evidence and much research is a form of iron-transport abnormality in the brain. In effect, RLS patients may have low levels of iron in brain nerve cells—just the opposite of some portions of the brain in PD.
Dr. Poceta is a Consultant in Neurology and Sleep Disorders in the Division of Neurology, Scripps Clinic, La Jolla, and the Scripps Clinic Sleep Center. His current interests include organized medicine and Internet medicine.
What Are Common Signs And Symptoms Of Restless Legs
People with RLS feel the irresistible urge to move, which is accompanied by uncomfortable sensations in their lower limbs that are unlike normal sensations experienced by people without the disorder. The sensations in their legs are often difficult to define but may be described as aching throbbing, pulling, itching, crawling, or creeping. These sensations less commonly affect the arms, and rarely the chest or head. Although the sensations can occur on just one side of the body, they most often affect both sides. They can also alternate between sides. The sensations range in severity from uncomfortable to irritating to painful.
Because moving the legs relieves the discomfort, people with RLS often keep their legs in motion to minimize or prevent the sensations. They may pace the floor, constantly move their legs while sitting, and toss and turn in bed.
A classic feature of RLS is that the symptoms are worse at night with a distinct symptom-free period in the early morning, allowing for more refreshing sleep at that time. Some people with RLS have difficulty falling asleep and staying asleep. They may also note a worsening of symptoms if their sleep is further reduced by events or activity.
People with RLS can sometimes experience remissions—spontaneous improvement over a period of weeks or months before symptoms reappear—usually during the early stages of the disorder. In general, however, symptoms become more severe over time.
Does Having Rls Increase The Risk Of Developing Pd
Since RLS affects as much as 4-10% of the US adult population, it is clear that the vast majority of those with RLS do not ever develop PD.
Despite this, it still might be the case that RLS increases the risk of subsequently developing PD. There have been many studies trying to figure this out – with conflicting results. Some studies show that there is no increased risk and others show that having RLS confers about a two-fold increased risk of developing PD over the general population.
Risk Factors For Periodic Limb Movement Disorder
About 6% of the general population has PLMD. However, the prevalence in older adults is much higher, reaching almost 60%. Studies suggest that PLMD may be especially common in older women. As with RLS, there are many conditions that are associated with PLMD. They include sleep apnea, spinal cord injuries, stroke, narcolepsy, and diseases that destroy nerves or the brain over time. Certain drugs, including some antidepressants and anti-seizure medications, may also contribute to PLMD. About a third of people with PLMD also have RLS.
What Impact Does Dbs Surgery For Pd Have On Rls
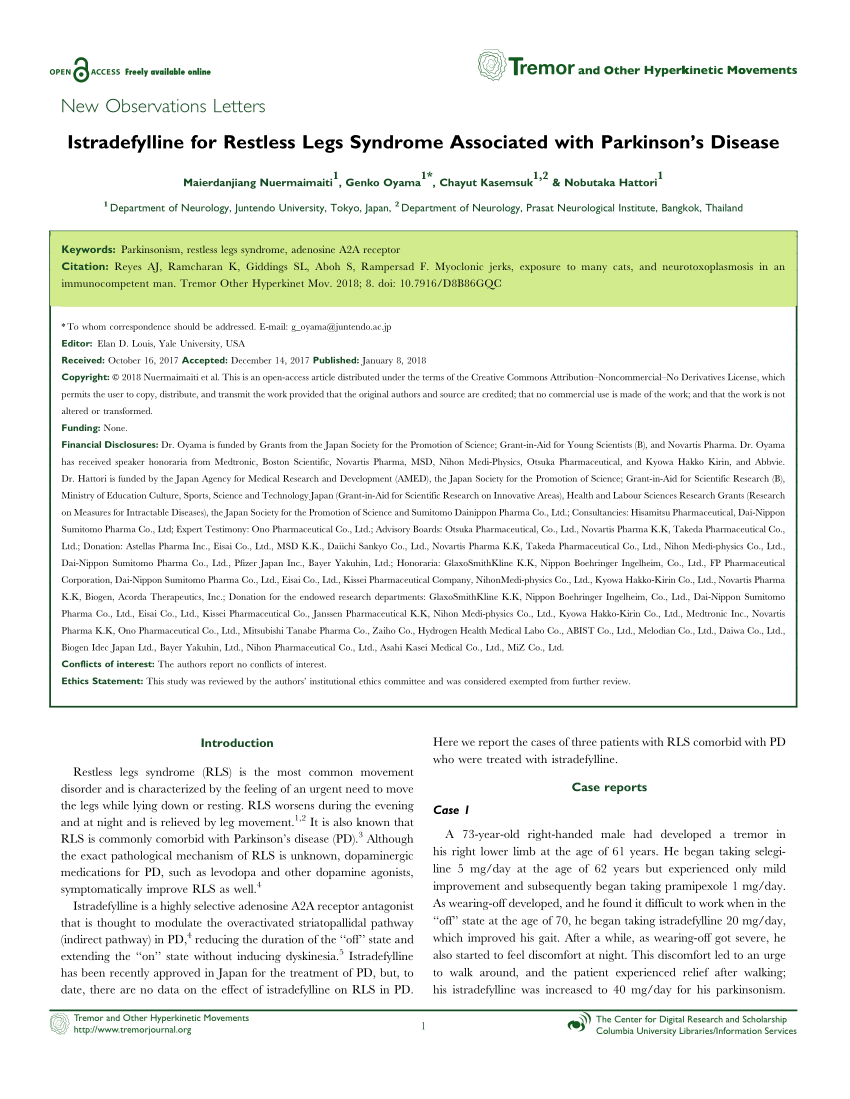
The emergence of RLS after subthalamic nucleus deep brain stimulation in patients with PD has been reported . Eleven of 195 patients with STN DBS reported new problematic symptoms of RLS after surgery. The mean reduction in antiparkinsonian medication was 74%. The authors suggested that reduction of anti-parkinsonian medication during STN DBS may unmask symptoms of RLS. However, a recent prospective study of 17 patients undergoing STN DBS identified 6 patients with RLS with a mean IRLSSG rating score of 23 preoperatively. Postoperative scores at 4 weeks and 6 months were significantly improved at 14.8 and 13.8 respectively. None of the patients developed RLS postoperatively .
Problems With The Common Pathophysiology Theory
Symptoms of RLS in PD are milder than in patients with idiopathic disease and may be difficult to differentiate from other sensory and motor symptoms in PD, in particular akathisia affecting the lower extremities . RLS symptoms may also be a manifestation of wearing-“off” phenomenon, a levodopa related complication of PD .
Prolonged dopaminergic therapy in RLS patients, in particular with levodopa use, may result in a phenomenon known as augmentation in which the severity of symptoms increases, onset of symptoms begin earlier in the day and more rapidly, and spread of distribution to other body parts occurs. In contrast, PD patients develop dyskinesias and motor fluctuations after treatment with dopaminergic agents. These complications are not seen in RLS patients.
Hypofunction of the endogenous opioid system has been postulated to be a mechanism related to the pathogenesis of RLS. Exposure to the iron chelator desferoxamine in cell cultures of rat substantia nigra resulted in DNA fragmentation while pre- administration of enkephalin significantly protected the cells from damage by iron deficiency .
What Are The Symptoms Of Restless Legs Syndrome
The sensations associated with RLS are distinct from normal sensations experienced by those who don’t have the disorder. This makes them difficult to characterize. According to the International Classification of Sleep Disorders, the words and phrases most commonly used by RLS patients to describe the feelings are:
- “Twitchy”
As a result of the sleep disturbances associated with RLS, patients often experience fatigue and daytime sleepiness. Sleep deficiency is associated with depression, anxiety, heart disease, and obesity. RLS patients are at greater risk for these issues as well. Concerns about sleep are the main reason RLS patients seek medical care for their condition.
Parkinson’s Disease And Restless Legs Syndrome Ylikoski A.
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
Iron And Its Relation To The Dopamine System
Iron is an important cofactor in several DA metabolisms and can also produce neurotoxic species.
Usually iron accumulates in the normal aging brain, in particular in the putamen, globus pallidus, red nucleus, and substantia nigra . Elemental iron plays a critical role in oxidative metabolism and it also serves as a cofactor in the synthesis of neurotransmitters .
In PD, neurodegeneration occurs mainly in SNc , while other iron-rich areas remain unaffected. In early stages of the disease the identification through the use of transcranial ultrasonography of a hyperechogenicity of the SNc correlates positively with the increase of iron and ferritin evaluated in post-mortem analysis , allowing an early identification of patients at risk for PD .
The increase in neuronal iron may be secondary to an increase in influx, facilitated by transferrin receptor-2/divalent metal transporter-1 endocytosis or the diffusion of ferric citrate , an increase in efflux, due to alteration of the activity of ceruloplasmin, or a dysregulation of iron homeostasis, mediated mainly by the iron storage protein ferritin .
Some studies have shown reduced ferritin concentrations in the SN from Parkinson’s disease brain, suggesting an alteration of this storage mechanism and a consequent increase in the level of free and potentially harmful iron .
Fatigue Sleep Difficulties And Restless Legs
Although Parkinson’s is classified as a movement disorder, it can affect people in various different ways. Sometimes the non-movement symptoms can be more troublesome and can have a bigger impact on the daily life of someone living with Parkinson’s.
Some of the more common non-movement symptoms of Parkinson’s are:
- Fatigue
- Restless legs
Evidence Of Dopaminergic Dysfunction In Rls
Observation studies of RLS in diseases which involve dopaminergic systems lend support to the hypothesis that dopaminergic dysfunction is present in RLS. One family with comorbidity of Huntington’s disease and idiopathic RLS has been reported. All family members affected by RLS also had HD, but not vice versa . Ondo and colleagues found a very high rate of undiagnosed RLS in their patients presenting with essential tremor. However, unlike other “secondary” forms of RLS, this finding was also associated with a high familial history of RLS . A study of comorbidities in Tourette syndrome including RLS investigated 144 probands with TS or chronic tics and their parents. RLS was present in 10% of probands and 23% of parents with no gender differences .
Future Prospects: Questions To Be Answered
The link between PD and RLS has yet to be clearly determined with clinical association studies differing widely in their findings, with some finding the incidence of RLS to be much greater in PD patients, and others finding no difference from that in the general population. These discrepancies could be addressed with prospective long-term clinical studies of PD patients who develop RLS and vice versa, with documentation of exposure to dopaminergic therapies.
With the exception of the parkin mutation, genetic studies have been failed to reveal any associations. We propose that population based genetic association studies of PD plus RLS and linkage studies of PD plus RLS as well as comparative studies of PD vs. PD-RLS vs. RLS should be conducted.
Sonographic studies reveal notable differences between PD and PD-RLS patients. Functional MRI studies have yet to focus on those patients with PD-RLS. Prospective functional imaging studies of PD vs. PD-RLS are needed to better understand the mechanisms involved in these disorders. To our knowledge, there have been no pathological studies looking at patients with PD-RLS. Establishing the pattern of decreased D2 receptor density in PD vs. PD and RLS vs. RLS may be valuable in understanding common pathophysiology. The reports purporting to DBS and RLS are conflicting, and more studies need to be done to clarify the effect, with attention to adjustments in dopaminergic medications.
Home Care Tips For Restless Legs Syndrome
The following approaches can reduce symptoms in patients with mild or moderate RLS and may be used in combination with medication in RLS patients who have severe symptoms.
- Sleep hygiene: Good sleep hygiene means maintaining a bedroom environment and a daily routine that supports high-quality sleep. Avoiding alcohol and caffeine is especially important for RLS patients because these substances can worsen symptoms.
- Exercise: Because physical inactivity often triggers RLS symptoms, exercise may be helpful. A research study found that RLS patients showed af 39% reduction in symptom severity after six weeks of engaging in an exercise program compared to an 8% symptom reduction in patients who did not exercise.
- Pneumatic pressure therapy: Pneumatic compression devices increase blood flow to the legs by filling with air to squeeze the legs. Researchers found that the device improved RLS symptoms, quality-of-life, and fatigue after one month of daily use compared to a control group.
- Massage and hot baths: Using massage and hot baths to stimulate the legs is widely recommended in RLS literature; however, there is limited scientific evidence supporting the effectiveness of these methods at this time.
Learn more about treating RLS here.
- Was this article helpful?
Characteristics Of Restless Leg Syndrome
There are certain features of RLS that make it a unique and specific disorder.
