Pathophysiology Of Motor Dysfunction In Parkinsons Disease As The Rationale For Drug Treatment And Rehabilitation
Stefano Tamburin
1Department of Neurosciences, Biomedicine and Movement Sciences, University of Verona, Piazzale Scuro 10, 37134 Verona, Italy
2Neuromotor and Cognitive Rehabilitation Research Centre, University of Verona, Piazzale Scuro 10, 37134 Verona, Italy
3Rehabilitation Unit, Pederzoli Hospital, Via Monte Baldo 24, 37019 Peschiera del Garda, Italy
4Neurology Unit, Pederzoli Hospital, Via Monte Baldo 24, 37019 Peschiera del Garda, Italy
Abstract
1. Introduction
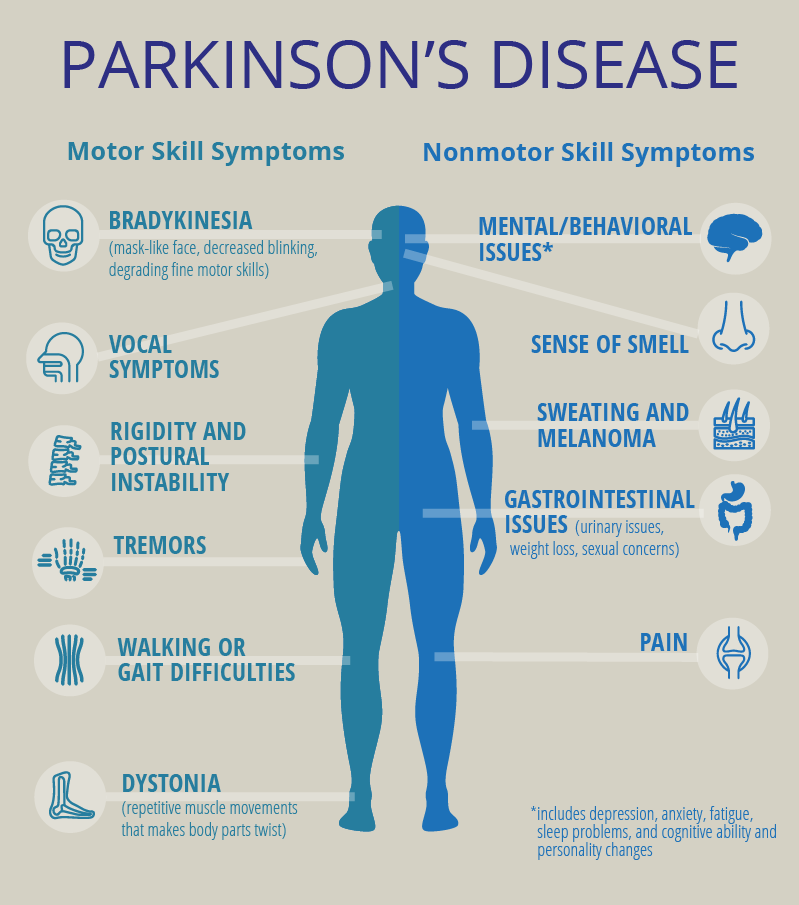
Parkinson’s disease is the second most common neurodegenerative disorder after Alzheimer’s disease , with an overall prevalence of 300 per 100,000 that rises from 41 in the 40–49 years’ age range to 1903 in people older than age of 80 years .
This review will summarize the evidence on the pathophysiology of PD motor symptoms and signs and give some insight into their neuropathological and neuropharmacological bases. These pieces of information may help the clinicians to better understand the rationale of current pharmacological and rehabilitation strategies for PD and encompass the large areas of uncertainty that should represent the focus for further studies.
2. The Functional Anatomy and Pathophysiology of the Basal Ganglia and the Role of the Cerebellum
3. The Neuropathology of PD
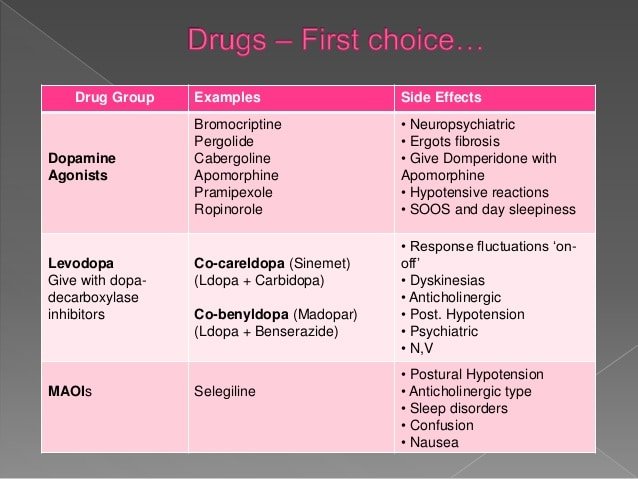
4. The Neuropharmacology of PD
| Neurotransmitter |
5. Pathophysiology of Bradykinesia in PD
6. Pathophysiology of Tremor in PD
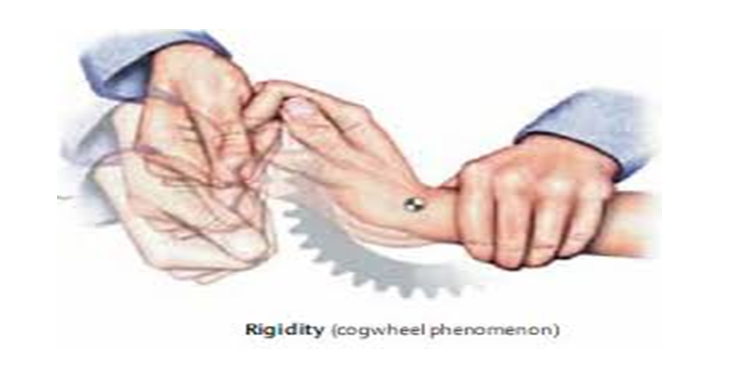
7. Pathophysiology of Rigidity in PD
8. Pathophysiology of Motor Fluctuations and Dyskinesia
Neurophysiological Studies Of The Effect Of Surgery And Deep Brain Stimulation On Bradykinesia
A large number of clinical studies have examined the effectiveness of pallidotomy; rather fewer have been published on chronic stimulation of the subthalamic nucleus or globus pallidus. However, a general rule is that, in terms of bradykinesia, pallidotomy produces an improvement of ~30% in OFF-period symptoms on the side contralateral to the lesion that is sustained for 2 years or more after the operation. There is less effect on measures of postural stability or on the best ON-therapy scores . Pallidal stimulation has similar effects, but is considered to be potentially safer in terms of adverse cognitive side-effects if bilateral procedures are performed . Chronic stimulation of the subthalamic nucleus may be more effective than pallidotomy or pallidal stimulation in improving OFF-treatment bradykinesia scores. Improvements in balance and posture are also more evident . It is usually possible to reduce the dose of l-dopa, and this ameliorates problems with dyskinesias.
Functional Imaging Studies Of The Effect Of Surgery And Deep Brain Stimulation On Bradykinesia
Many imaging studies have been driven by the model of basal ganglia function outlined in the early 1990s. Overactivity of the inhibitory output projections from the basal ganglia to the thalamus in Parkinson’s disease was supposed to remove facilitatory thalamocortical drive, particularly to midline cortical motor areas . PET and fMRI activation studies had shown that these areas were less activated during movement in patients, and therefore pallidotomy was expected to improve activation by restoring normal levels of basal ganglia output .
Most studies on movement-related changes in metabolic activity have reported similar findings both after pallidotomy and during subthalamic nucleus stimulation . In tasks in which a free-choice joystick movement is used, increased activation of preSMA and anterior cingulate cortex is usually accompanied by increased activation of the dorsolateral prefrontal cortex. Although most reports of activation-induced metabolism suggest that there is no change in the primary motor cortex, there are some suggestions that stimulation of the subthalamic nucleus may reduce activity in the resting state . Whether this is related to a general reduction in rigidity or other involuntary muscle activity or to reduced input to the cortex via pathways direct from the subthalamic nucleus is not known.
Identifying Newly Diagnosed Pd Patients And Matched Controls For Each Pd Patient
The study population comprised newly diagnosed patients with PD and their matched controls. First, we identified PD patients using the registration code for PD in the program for rare, intractable disease from January 1, 2004, to December 31, 2006, and we defined the index date as the date of the earliest claim with the V124 code. To remove any prevalent cases, we excluded patients who had PD diagnostic codes or PD registration codes before January 1, 2004. As the V124 registration criteria did not exclude atypical Parkinsonian syndromes, we excluded patients diagnosed with atypical parkinsonism during the entire study period, from 2002 to 2017. Moreover, we excluded patients under 40 years of age. Lastly, we excluded patients whose total number of days of antiparkinsonian medications was less than 180 days. The list of the antiparkinsonian medications used in this study is given in Supplementary Table S1.
Then, we selected up to four controls for each PD patient matched by sex and age at the index date. Previous studies reported that matching 4 controls to 1 patient can minimize the bias in measuring treatment effect in the maximum number of matched controls12,13. Individuals who had the registration code for rare, intractable disease for PD , had any diagnostic code for Parkinsonism , or had been prescribed an antiparkinsonian drug during the study period were not recruited as controls.
Sidebar: Morris K Udall Centers Of Excellence For Parkinson’s Disease Research

The Morris K. Udall Parkinson’s Disease Research Act of 1997 authorized the NIH to greatly accelerate and expand PD research efforts by launching the NINDS Udall Centers of Excellence, a network of research centers that provide a collaborative, interdisciplinary framework for PD research. Udall Center investigators, along with many other researchers funded by the NIH, have made substantial progress in understanding PD, including identifying disease-associated genes; investigating the neurobiological mechanisms that contribute to PD, developing and improving PD research models, and discovering and testing potential therapeutic targets for developing novel treatment strategies.
The Udall Centers continue to conduct critical basic, translational, and clinical research on PD including: 1) identifying and characterizing candidate and disease-associated genes, 2) examining neurobiological mechanisms underlying the disease, and 3) developing and testing potential therapies. As part of the program, Udall Center investigators work with local communities of patients and caregivers to identify the challenges of living with PD and to translate scientific discoveries into patient care. The Centers also train the next generation of physicians and scientists who will advance our knowledge of and treatments for PD. See the full list of Udall Centers.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25 The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
How Can I Support Someone With Parkinsons At The Advanced Or Palliative Stage
In the advanced stages of Parkinson’s, your patient’s care needs may be more complex and require careful planning along with the patient, their family and other health and social care professionals involved.
Palliative care should be holistic, considering the ‘whole person’ to support the personal, social, psychological and spiritual needs of your patient and their family. It should give your patient some control and choice over areas such as treatment options and where they will be cared for, as well as providing advice and support to all the people involved in their care.
Palliative care in Parkinson’s may be supported by a number of professionals, including a Parkinson’s nurse specialist, local hospice or specialist palliative care team, physiotherapist, occupational therapist, speech and language therapist or dietitian. Many people with Parkinson’s also find complementary therapies beneficial.
It is important that you find out whether the person has a care plan in place regarding their preferences for how the issues surrounding advanced Parkinson’s should be managed. This could include legal documentation such as a Lasting Power of Attorney and an advance care plan. Advance care plans include information on what the person’s wishes and preferences are for their care in the future. They may include decisions on any treatments the person doesn’t want to have in the future – this is called an Advance Directive, Advance Decision to Refuse Treatment or Living Will.
What Is Parkinsons Disease Symptoms Causes Diagnosis Treatment And Prevention
The causes and symptoms of Parkinson’s disease can vary from person to person. While there is no cure, there are medications and treatments to help manage the condition.
Parkinson’s disease is a movement disorder that happens when nerve cells in a certain part of the brain are no longer making the chemical dopamine.
The condition is also sometimes known as paralysis agitans or shaking palsy.
The Parkinson’s Foundation estimates that 60,000 Americans are diagnosed with Parkinson’s every year. However, the true number of people who develop the disease may be much higher.
What Other Conditions Have Similar Symptoms And Signs Of Parkinsons Disease
Other neurological diseases may cause symptoms similar to Parkinson’s disease. The term Parkinsonism refers to a patient that has symptoms similar to Parkinson’s.
Early in the disease process, it can be tough to make an assertive diagnosis and difference between Parkinson’s and Parkinson-like diseases.
Often the correct diagnosis is made after further symptoms develop, and the physician can monitor the course of the disease.
The development of additional symptoms and the course of the illness generally points towards the correct diagnosis. These are the most common neurological diseases that can produce Parkinson-like symptoms.
- Progressive Supranuclear Palsy
- Lewy Body disease or Dementia with Lewy bodies
- Corticobasal degeneration or corticobasal ganglionic degeneration
Nonetheless, doctors should think of other causes rather than Parkinson’s disease when events like this happen.
- Poor response to dopamine
- Early loss of balance or vision problems
- Prominent intellectual decline – dementia
- Rapid onset or progression of the disease
Actually, though it is a disease that is not clearly understood, there are specific organizations like Parkinson’s UK that dedicate themselves to doing research.
These organizations look forward to following the natural course of the disease and developing clinical trials for patients in an attempt to find a cure.
Quantitative Analysis Of Bradykinesia And Rigidity In Parkinsons Disease
- 1Neurology Unit, Campus Bio-Medico University of Rome, Rome, Italy
- 2NeXT: Neurophysiology and Neuroengineering of Human-Technology Interaction Research Unit, Università Campus Bio-Medico, Rome, Italy
- 3Nuffield Department of Clinical Neurosciences, University of Oxford, John Radcliffe Hospital, Oxford, United Kingdom
- 4Unit of Biomedical Robotics and Biomicrosystems, School of Engineering, Campus Bio-Medico University of Rome, Rome, Italy
- 5Brain Connectivity Laboratory, IRCCS San Raffaele Pisana, Rome, Italy
- 6IRCCS San Raffaele Pisana, Rome, Italy
Background: In the last decades, several studies showed that wearable sensors, used for assessing Parkinson’s disease motor symptoms and recording their fluctuations, could provide a quantitative and reliable tool for patient’s motor performance monitoring.
Objective: The aim of this study is to make a step forward the capability of quantitatively describing PD motor symptoms. The specific aims are: identify the most sensible place where to locate sensors to monitor PD bradykinesia and rigidity, and identify objective indexes able to discriminate PD OFF/ON motor status, and PD patients from healthy subjects .
Correlation Between Clinical Rigidity Scores And Selected Motor Network
The PCfdr method detected 227 significant connections between ROIs, and thus the X matrix in Eq. 2 was 10×227. The 227 significant connections represents ?8.6% of all possible 52×51=2,652 directional connections.
The LASSO regression operator selected nine of 227 significant connections between brain regions that significantly predicted rigidity . These regions include primary motor area , ventral premotor area, supplementary motor area, basal ganglia, areas in the temporal, parietal, and occipital lobes as well as the cerebellum. The positive and negative correlation between connectivity measures and clinical rigidity scores are demonstrated in Figure ?Figure22 and summarized in Table ?Table22.
What Are The Important Points Regarding Apomorphine At The End Of Life
Apomorphine is a dopamine agonist, which is given as a subcutaneous infusion either continuously or intermittently and also as single subcutaneous injections. An overview of studies into apomorphine use shows improvement in motor off periods and in dyskinesias.39
Apomorphine has side-effects similar to other dopaminergic medication but also notably nausea and vomiting. Ondansetron is not recommended for nausea in patients using apomorphine due to adverse effects.21
Subcutaneous apomorphine has been used at the end of life in a patient with advanced PD although with the recommendation that this is by a healthcare professional experienced in its use.40
How Can Parkinsons Affect Someone At The Advanced Or Palliative Stage
Parkinson’s progresses in stages: diagnosis, maintenance, advanced and palliative. Professionals should have talk to people with Parkinson’s about advance care planning in the earlier stages of the disease. This can allow them to express their wishes and preferences for their care in the later stages of the disease and make plans for the future.
Although the condition progresses differently and at a different speed for each person, the advanced stage can potentially cover a long period of time.
Problems that affect someone with advanced Parkinson’s may include:
- medicines being less effective at managing symptoms than before
- having to take lots of medicines to manage symptoms and side effects
- more ‘off’ periods – when the effects of medication are reduced, and people experience movement fluctuations and involuntary movements
- increased mobility problems and falls
- swallowing difficulties
- less control of their Parkinson’s symptoms, which become less predictable
- pain.
Some of the more advanced symptoms can lead to increased disability and poor health, which can make someone more vulnerable to infection, such as pneumonia. People with Parkinson’s most often die because of an infection or another condition, usually caused by Parkinson’s.
What Are The Important Points Regarding Duodopa At The End Of Life
Duodopa is a continuous infusion of dopaminergic medication administered as a gel into the gut, pumped via a percutaneously inserted gastrostomy tube . There is a requirement for care of the stoma and PEG tube together with functioning of the pump by the patient or carer.41 It reduces the time in motor off periods in advanced PD and quality of life.42 There is evidence of effective treatment up until death from within a case series.43
Correspondence Between Connectivity And Clinical Rigidity Scores
We used multivariate linear regression to determine whether or not clinical rigidity scores could be predicted from the connectivity patterns in PD subjects . Specifically, we modeled the rigidity scores as:
where Y was a vector of rigidity scores of dimensions 10 by 1, X was 10 by n and ? is a 10 by 1 vector of residuals. Since, in this case, the number of potential regressors exceeds the number of examples , we utilized LASSO regression . Unlike other methods such as ridge regression or ordinary least squares, LASSO regression puts a sparsity constraint on ? so that most values are zero and attempts to find the most informative connections to predict clinical scores . The number of regressors selected by the LASSO operator was to give the least predictive error based on a 10-fold cross-validation. Once the regressors were selected, we used robust regression to estimate the significance of the individual regressors.
Death In Patients With Parkinsons Disease An Observational Study
R. Mappilakkandy, A. Pieris, D. Miodrag, A. Chunduri
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: We aimed to analyse the major cause and contributory reasons for death in patients with Parkinson’s disease who were known to our PD service at Northampton General Hospital.
Background: PD is a progressive neuro-degenerative disorder associated with a decreased lifespan particularly for patients with dementia, a significant non motor feature. The current data provides little information for the cause of death in Parkinson’s disease. Aspiration pneumonia is often considered a leading cause of death in such patients.
Methods: An observational study was done on a series of 40 consecutive cases of patients with PD had been seen in the PD clinic previously by the Geriatric Medicine service at Northampton General Hospital between 2013 and 2015 and had subsequently died. The cause of death was obtained from the death certificates, hospital records and GP records. We also obtained data on the prior preferences of place of death and the actual place of death.
Results: The age range varied from 70 to 95 years with 62% male and 38% females. The mean Hoehn and Yahr score at the time of death was 3.66. 60% of these patients were aged from 80-89 years with 20% being very old at above 90 years.
There was also a high of incidence of dementia in this cohort of patients who died with aspiration pneumonia. There were very few cardiac, strokes, and cancer causes of death.
What Is The Prognosis And Life Expectancy For Parkinsons Disease
The severity of Parkinson’s disease symptoms and signs vary greatly from person to peson, and it is not possible to predict how quickly the disease will progress. Parkinson’s disease itself is not a fatal disease, and the average life expectancy is similar to that of people without the disease. Secondary complications, such as pneumonia, falling-related injuries, and choking can lead to death. Many treatment options can reduce some of the symptoms and prolong the quality of life.
What Are The Risks Of Not Receiving Any Dopaminergic Medication
There is the possibility of neuroleptic malignant-like syndrome , a life-threatening and distressing condition resulting in rigidity and fever, from withdrawal of therapy.31 This can also occur with sudden cessation of Deep Brain Stimulation .32,33,34 To reduce the risk of this, dopaminergic therapy at the end of life should be continued.27 It should also be noted that in a patient dying of another condition, whose PD is still responsive to dopaminergic medication, the cessation of this also risks aspiration pneumonia.35 Transdermal rotigotine can be used in patients in whom a NG tube may cause excessive distress or is not possible. The dose should be calculated with an accepted converter.36
Pathophysiology Of Rigidity And Akinesia In Parkinsons Disease
Log in to MyKarger to check if you already have access to this content.
Buy a Karger Article Bundle and profit from a discount!
If you would like to redeem your KAB credit, please log in.
Save over 20%
- Rent for 48h to view
- Buy Cloud Access for unlimited viewing via different devices
- Synchronizing in the ReadCube Cloud
- Printing and saving restrictions apply
USD 8.50
- Access to all articles of the subscribed year guaranteed for 5 years
- Unlimited re-access via Subscriber Login or MyKarger
- Unrestricted printing, no saving restrictions for personal use
The final prices may differ from the prices shown due to specifics of VAT rules.
What Is The Main Cause Of Death In Parkinsons Disease Patients
Parkinson’s is often referred to as a “bespoke” disease because it affects each patient differently. Another factor worth considering is that Parkinson’s disease generally affects people in their 60s, most of whom die of unrelated conditions such as cancer, heart disease or stroke. However, the most common cause of death in those with Parkinson’s disease is pneumonia. This is because the disease can impair your ability to swallow in the later stages, putting you at risk for aspirating food or liquid into the lungs.
Know The Causes Symptoms And Treatment Of This Nerve Disorder
Parkinson’s disease, a chronic and progressive nerve disorder, affects as many as one million Americans, with 60,000 people diagnosed each year. You might have questions like: What is Parkinson’s disease? Who gets it, what are the symptoms, and is there a cure? Here’s what you need to know.
Who Is At Risk?
Age is one of the biggest risk factors for Parkinson’s. The disease develops most often after age 60 and occurs more often in men than in women. Early-onset Parkinson’s can strike people under age 50. In very rare cases, symptoms may even appear at age 20 or younger.
Causes
Is Parkinsons Disease Fatal Life Expectancy For ParkinsonsEmma-Marie Smith
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise: Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinson’s disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didn’t exercise or didn’t start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinson’s, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments — whether medicines or deep brain stimulation — are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Which Medications Can Make Confusion And Hallucinations Worse
As PD progresses, non-motor symptoms including psychosis and hallucinations become more prominent both for the patient and caregivers.9 Dopaminergic medication can exacerbate these symptoms and this can be reduced through a “last in, first out approach.” 27,28 Medications that have an anticholinergic effect also may cause or worsen acute confusion and the anticholinergic burden in the patient’s medication history should be considered.29
Two Areas In Which Parkinsons Disease May Bring About Death
I. Falls
PD patients are at an increased risk of falling and bad falls can lead to death. This usually occurs as a complication of a fall that requires hospitalization, particularly if it involves surgery. While most people do not fracture their hips when they fall, some do, and hip surgery, while routine, is still major surgery. It carries the risk of infection, delirium related to pain medications and anesthesia, heart failure, pneumonia, blood clots in the legs that then go to the lungs, and general weakness from immobility. Hip fractures are probably the main cause for death for those who fall, but people can fracture other bones and require surgery. They may fracture their ribs, which leads to reduced coughing, because of the pain, and an increased risk of lung infections . It is surprisingly uncommon for Parkinson’s Disease patients to die from brain injuries related to falls, but it still may occur.
II. Pneumonia
PD patients also may develop pneumonias completely unrelated to difficulties with swallowing, just like their non-PD friends and relatives.
Standard Protocol Approval Registration And Patient Consent
The study protocol was assessed and determined to be exempt from review by the Institutional Review Board of Seoul National University Hospital . Furthermore, the NHIS approved the use of its database and provided data after excluding all possible patient identification information . The requirement for informed consent was waived by the Institutional Review Board of the Seoul National University, because the database was anonymized. All methods were carried out in accordance with relevant guidelines and regulations.
Do People With Parkinsons Get Priority Access To The Covid
Each state has its own process for rolling out the vaccine to different population groups. If you would like to advocate for people with Parkinson’s to be part of a priority group, we encourage you to contact your elected officials. We have created a letter that you can personalize and send them either by mail or electronically.
How Can Falls Resulting From Parkinsons Disease Be Fatal
Patients with Parkinson’s disease are seen to be at an increased risk of bad falls which can lead to death. Generally it is seen that death results from hip fractures that require hospitalization because surgery would be required. Hip surgery is a major operation which carries the risk of infection, heart failure and blood clots. Such clots become dangerous if they reach the lungs. Sometimes fall may even lead to fatal brain injuries if not taken care properly.
Janet Reno’s Death: How Does A Person Die Of Parkinson’s
Former U.S. Attorney General Janet Reno has died at age 78 from complications of Parkinson’s disease, her family announced today. But how do people die from this disease?
In patients with Parkinson’s disease, the brain cells that produce a chemical called dopamine start to die off. It’s not clear what triggers the death of these cells, but researchers do know that dopamine is important for the control of muscle movement. Parkinson’s patients experience symptoms such as tremors, slowed movements, muscle stiffness and impaired balance.
Is Parkinsons Disease Fatal Life Expectancy For Parkinsons
Worried about your Parkinson’s disease life expectancy? A Parkinson’s disease diagnosis comes with many worries and anxieties. One worry concerns the progression of the disease and whether Parkinson’s disease can be fatal. The issue is rarely straightforward, but there is no reason to think your condition is a death sentence. Many people live for years or decades with their Parkinson’s disease symptoms under control, while the illness progresses more quickly for others. It’s important that you know what to expect when you’re diagnosed with Parkinson’s disease, so don’t be afraid to ask questions and air your concerns to your doctor. For now, let’s explore the issue of life expectancy of patients with Parkinson’s disease and address some common concerns.
Correlation Of Clinical Rigidity Scores And Damping Ratio
The damping ratios of PD subjects had a linear relationship with clinical rigidity scores .3). No other model parameters significantly correlated with rigidity, including natural frequency and peak time.
There is a linear relationship between clinical rigidity scores and damping ratio . This relationship could be utilized to predict rigidity scores, which significantly correlate with actual recorded rigidity scores.
What To Do With Deep Brain Stimulation At The End Of Life
Deep brain stimulation uses an Implantable Pulse Generator, usually placed in the infraclavicular area, connected to leads within the brain. There is a remote programmer, and also a charging unit in the case of a rechargeable device, which are given to the patient and their carer. It improves dyskinesias and also has a levodopa sparing effect.37
Deactivation of DBS may lead to increased symptom burden as mentioned in the section above and so awareness of features of PHS should be considered if there is failure at the end of life. Supportive treatment should be given if possible,38 and anticipation of symptoms of distress from rigidity and fever.
After death, deactivation of the device with the patient’s handheld programmer is required before removing the pulse generator and battery in the case of a cremation.
How Can Falls Resulting From Parkinsons Disease Be Fatal

Patients with Parkinson’s disease are seen to be at an increased risk of bad falls which can lead to death. Generally it is seen that death results from hip fractures that require hospitalization because surgery would be required. Hip surgery is a major operation which carries the risk of infection, heart failure and blood clots. Such clots become dangerous if they reach the lungs. Sometimes fall may even lead to fatal brain injuries if not taken care properly.
Myth 4: Aside From Medication There Isnt Much You Can Do
Fact: This “it is what it is; there’s nothing I can do to help myself” myth is counterproductive. There is a lot you can do — chiefly, keeping as active as you can. A recent study found that patients with Parkinson’s who took part in weekly, hourlong exercise sessions were able to do more in their daily lives than those who did not.
What Diseases And Conditions Resemble Parkinsons Disease
PD is the most common form of parkinsonism, in which disorders of other causes produce features and symptoms that closely resemble Parkinson’s disease. Many disorders can cause symptoms similar to those of PD, including:
Several diseases, including MSA, CBD, and PSP, are sometimes referred to as “Parkinson ’s-plus” diseases because they have the symptoms of PD plus additional features.
In very rare cases, parkinsonian symptoms may appear in people before the age of 20. This condition is called juvenile parkinsonism. It often begins with dystonia and bradykinesia, and the symptoms often improve with levodopa medication.
Complications Related To Parkinsons Can Affect Survival
Claudia Chaves, MD, is board-certified in cerebrovascular disease and neurology with a subspecialty certification in vascular neurology.
Parkinson’s is a common neurodegenerative disease, and although it is not fatal, research suggests it may influence life expectancy.
A 2012 study in Archives of Neurology examined the six-year survival of nearly 140,000 Medicare beneficiaries with Parkinson’s disease in the United States. During the six-year period, 64% of the participants with Parkinson’s disease passed away.
The risk of death of those with Parkinson’s was then compared to Medicare beneficiaries who did not have Parkinson’s or any other common diseases, including:
When controlling for variables like age, race, and gender, the six-year risk of death among people with Parkinson’s was found to be nearly four times greater than those Medicare beneficiaries without the disease or other common diseases.
At the same time, the rate of death among those with Parkinson’s disease was similar to those with hip fracture, Alzheimer’s dementia, or a recent heart attack—although it was higher than those who had been newly diagnosed with either colorectal cancer, stroke, ischemic heart disease, or chronic obstructive pulmonary disease.
