Diagnosis: Parkinson’s Dementia Or Dementia With Lewy Bodies
During assessment, a specialist may look at when the dementia symptoms first appeared before reaching a diagnosis of Parkinson’s dementia or dementia with Lewy bodies.
If there have been motor symptoms for at least one year before dementia symptoms occur, specialists will often give a diagnosis of Parkinson’s dementia.
If dementia symptoms occur before or at the same time as motor symptoms, specialists will usually give a diagnosis of dementia with Lewy bodies.
However, it should be noted that in some cases of dementia with Lewy bodies, no motor symptoms develop at all.
Theres no single test – diagnosis is made through several different assessments, usually starting with an appointment with your GP or Parkinson’s nurse.
Some people find it helps to go to the appointment with someone who knows them well, who can give the GP or Parkinson’s nurse information about changes they’ve noticed.
Your GP can discuss your symptoms with you and carry out a physical examination, including blood and urine tests, to rule out other potential causes of the symptoms .
Your GP may also review your medication, in case your symptoms are side effects.
If your GP thinks you have dementia, they can refer you to a specialist, such as a neurologist, psychiatrist or geriatrician.
You might be referred to a memory clinic or memory service. In some areas of the country, you can refer yourself to these services.
But if you feel you need to see the specialist again, you can ask to be referred back.
See A Doctor If Youre Noticing Symptoms Beyond Parkinsons
Sometimes the mood or memory changes a person experiences cannot entirely be explained just by Parkinsons. If this is the case, the caregiver should explore other diagnoses, because if something cannot be explained by Parkinsons, theres certainly a risk of it being dementia, Oguh said.
She added that some signs to look for include increased memory and behavioral problems, like mood swings, anxiety or depression. Psychiatric behaviors, like hallucinations, delusions or paranoia, cannot just be explained by Parkinsons, and are more likely to be caused by a form of dementia like Lewy body dementia.
Oguh urged caregivers to be aware of changing symptoms like these.
I think sometimes family members are able to realize sooner than the patient, Oguh said. Often the patient might lack insight as to what is happening. I would encourage family members to seek expert opinion and treatment options.
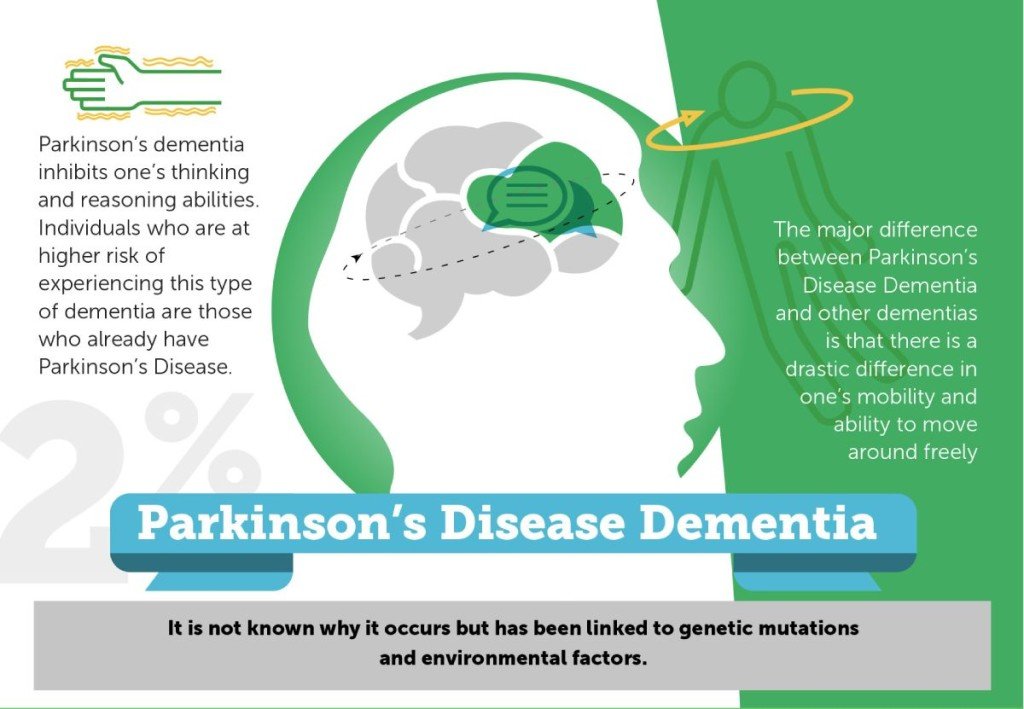
What Are Parkinson’s Disease Dementia Medical Treatment And Medications
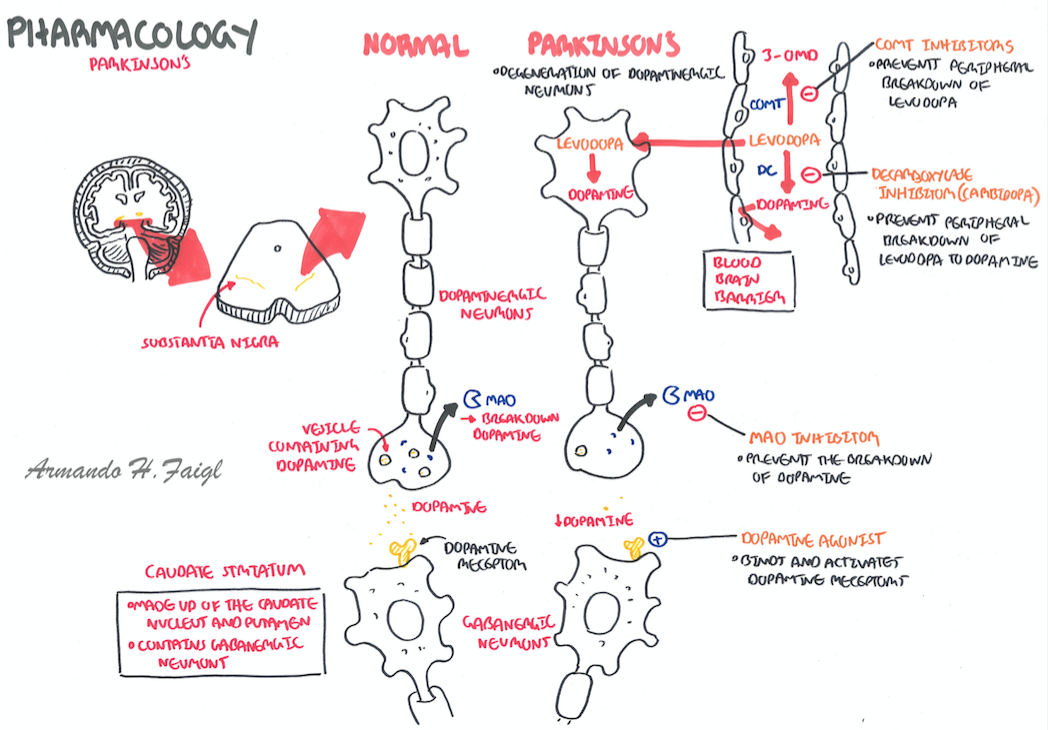
There is no specific therapy for dementia in Parkinson’s disease. Although cognitive symptoms initially may appear to respond to drugs that promote dopamine production, the improvement is mild and transient in contrast to the early responses to motor control improvement with medication in patients with Parkinson’s disease.
Parkinson’s disease dementia medications
Various medications are used to treat the movement disorders of Parkinson’s disease, some may exacerbate symptoms related to dementia.
- These include dopamine given in the form of levodopa; medications known as dopamine agonists that act on the dopamine receptor; and medications that slow down the metabolism of dopamine. They are often used in conjunction with monoamine oxidase inhibitors such as rasagiline. In addition, anticholinergic drugs are sometimes used.
- Unfortunately, these drugs may affect cognitive symptoms and mood disorders.
- The anticholinergic drugs, for example, help balance levels of dopamine and acetylcholine, another neurotransmitter, in the brain. These drugs can improve movement disorders but often make memory loss worse.
The dementia of Parkinson’s disease may respond to drugs used in patients with Alzheimer’s disease. However, these drugs, called cholinesterase inhibitors , lead to only small and temporary improvements in cognition.
Mood disorders and psychoses are usually treated with other medication.
Who Is Affected By Parkinsons Disease
Several studies have found that the incidence of PD is much more common in than women.2,4 One estimate found that PD affects about 50 percent more men than women.2 The reasons for the differences in men and women with PD are unclear, although some suggested explanations are the protective effect of estrogen in women, the higher rate of minor head trauma and exposure to occupational toxins in men, and genetic susceptibility genes on the sex chromosomes.4
People with a close family member with Parkinsons have a small increased risk of developing the disease. About 15 percent to 25 percent of people with PD have a known relative with the disease.2
It is estimated that about 10 million people worldwide are living with PD. The incidence of the disease is higher in industrialized countries.3,4
The incidence of PD increases with age: while PD affects 1 percent of the population over the age of 60, this increases to 5 percent of the population over the age of 85.1
Approximately 5 percent of people with PD are diagnosed before the age of 60.1
Urban areas have a higher prevalence and incidence of PD.5
Is There A Test To Diagnose Pd Dementia
There is no single test for PDD. The diagnosis is made clinically. If you or someone you spend time with notices cognitive changes, it is important to discuss them with your care team. If you dont have a care team in place, its important to find a specialist or physician familiar with dementia or geriatric medicine. Call the Parkinson’s Foundation Helpline 1-800-4PD-INFO for a referral.
Dementia With Lewy Bodies And Parkinson Disease Dementia
, MD, PhD, Department of Neurology, University of Mississippi Medical Center
Dementia with Lewy bodiesParkinson disease dementia
Dementia is chronic, global, usually irreversible deterioration of cognition.
Dementia with Lewy bodies is the 3rd most common dementia. Age of onset is typically > 60.
Lewy bodies are spherical, eosinophilic, neuronal cytoplasmic inclusions composed of aggregates of alpha-synuclein, a synaptic protein. They occur in the cortex of some patients who have dementia with Lewy bodies. Neurotransmitter levels and neuronal pathways between the striatum and the neocortex are abnormal.
Lewy bodies also occur in the substantia nigra of patients with Parkinson disease, and dementia may develop late in the disease. About 40% of patients with Parkinson disease develop Parkinson disease dementia, usually after age 70 and about 10 to 15 years after Parkinson disease has been diagnosed.
Because Lewy bodies occur in dementia with Lewy bodies and in Parkinson disease dementia, some experts think that the two disorders may be part of a more generalized synucleinopathy affecting the central and peripheral nervous systems. Lewy bodies sometimes occur in patients with Alzheimer disease, and patients with dementia with Lewy bodies may have neuritic plaques and neurofibrillary tangles. Dementia with Lewy bodies, Parkinson disease, and Alzheimer disease overlap considerably. Further research is needed to clarify the relationships among them.
What Happens In Pdd
People with PDD may have trouble focusing, remembering things or making sound judgments. They may develop depression, anxiety or irritability. They may also hallucinate and see people, objects or animals that are not there. Sleep disturbances are common in PDD and can include difficulties with sleep/wake cycle or REM behavior disorder, which involves acting out dreams.
PDD is a disease that changes with time. A person with PDD can live many years with the disease. Research suggests that a person with PDD may live an average of 57 years with the disease, although this can vary from person to person.
Lewy Bodies: More Than Lbd
LBD is characterized by the presence of Lewy bodies in the nerve cells of the brain, meaning that LBD patients have Lewy bodies in the brain.2 However, Lewy bodies are also common with other conditions, such as Alzheimer’s and Parkinsons disease. In fact, most people with PD also have Lewy bodies in their brain. However, even if they have Lewy bodies, not all Parkinsons patients will also develop LBD.2
What Is Aggressive Parkinsons Disease
As written above, Parkinsons dementia aggression is that form of Parkinsons which makes the patient exhibit aggressive behavior. They vent out their aggression either verbally or physically, in the various forms that have been written above. Besides verbal and physical outbursts, PD Dementia patients are also prone to hallucinating caused by the medication administered. Hallucinations in PD Dementia patients primarily occur because of the effects of dopaminergic agents for motor symptoms.
Loss of dopamine neurons in the ventral tegmental area is one of the likeliest of all neuropathological causes as changes in serotonin and norepinephrine systems are not. For the uninitiated, the ventral tegmental area is the origin of the mesolimbic dopaminergic projection. Plenty of studies have gone into analyzing the cause behind the aggression in PD Dementia patients. Depression in PD Dementia patients has been identified due to changes in the medial frontal cortex and the anterior cingulate. Akinetic-rigid variants have been found in patients showing signs of major depression.
Severity Of Motor Symptoms
Compared to those without dementia, PDD patients had more severe motor features with a greater impairment in balance. Of the 36 participants, 13 were characterised H & Y stage IV and V, whereas the others were between stages IIII. In particular, of the seven PDD participants, six were characterised by having H & Y stages IV and V.
How Can We Support The Sleep/wake Cycle Of Pdd
For people with PDD who are confused about the day-night cycle, some daily strategies can be helpful. At night, starting a lights out routine that happens at the same hour every day, where all curtains are closed and lights are turned off, can help the person understand that it is sleep time. During the day, opening the curtains, allowing the person with PDD to spend as much time in the daylight as possible, avoiding naps, and organizing stimulating activities, can be helpful. Having lots of calendars and clocks in every room might also help a person with PDD be less confused about the time of day.
How Is Parkinson Disease Treated
Parkinson disease can’t be cured. But there are different therapies that can help control symptoms. Many of the medicines used to treat Parkinson disease help to offset the loss of the chemical dopamine in the brain. Most of these medicines help manage symptoms quite successfully.
A procedure called deep brain stimulation may also be used to treat Parkinson disease. It sends electrical impulses into the brain to help control tremors and twitching movements. Some people may need surgery to manage Parkinson disease symptoms. Surgery may involve destroying small areas of brain tissue responsible for the symptoms. However, these surgeries are rarely done since deep brain stimulation is now available.
Delusions From Parkinsons Disease
Delusions affect only about 8 percent of people living with PD. Delusions can be more complex than hallucinations. They may be more difficult to treat.
Delusions often start as confusion that develops into clear ideas that arent based on reality. Examples of the types of delusions people with PD experience include:
- Jealousy or possessiveness. The person believes someone in their life is being unfaithful or disloyal.
- Persecutory. They believe that someone is out to get them or harm them in some way.
- Somatic. They believe they have an injury or other medical problem.
- Guilt. The person with PD has feelings of guilt not based in real behaviors or actions.
- Mixed delusions. They experience multiple types of delusions.
Paranoia, jealousy, and persecution are the most commonly reported delusions. They can pose a safety risk to caregivers and to the person with PD themselves.
PD isnt fatal, though complications from the disease can contribute to a shorter expected life span.
Dementia and other psychosis symptoms like hallucinations and delusions do contribute to increased hospitalizations and increased rates of death .
One study from 2010 found that people with PD who experienced delusions, hallucinations, or other psychosis symptoms were about 50 percent more likely to die early than those without these symptoms.
But early prevention of the development of psychosis symptoms may help increase life expectancy in people with PD.
What Treatments Are Available For Parkinsons Psychosis
Your doctor may first reduce or change the PD medication youre taking to see whether that reduces psychosis symptoms. This is about finding a balance.
People with PD may need higher doses of dopamine medication to help manage motor symptoms. But dopamine activity shouldnt be increased so much that it results in hallucinations and delusions. Your doctor will work with you to find that balance.
Dementia Outcomes According To Baseline Autonomic Variables
Orthostatic systolic blood pressure drop was strongly associated with dementia risk . Having a baseline systolic decrease >10 mm Hg increased dementia odds 7-fold . In addition, the mean baseline systolic blood pressure in the group with dementia was higher than in the group without dementia . Baseline occurrence of urinary symptoms , erectile dysfunction , and bowel dysfunction was higher in those with dementia but not statistically different compared with the group without dementia.
Lewy Body Dementia Vs Parkinsons Disease Dementia
Diagnoses of Lewy body dementia include dementia with Lewy bodies and Parkinsons disease dementia. Symptoms in both of these diagnoses can be similar.
Lewy body dementia is a progressive dementia caused by abnormal deposits of a protein called alpha-synuclein in the brain. Lewy bodies are also seen in Parkinsons disease.
The overlap in symptoms between Lewy body dementia and Parkinsons disease dementia include movement symptoms, rigid muscles, and problems with thinking and reasoning.
This seems to indicate that they could be linked to the same abnormalities, though more research is needed to confirm that.
The later stages of Parkinsons disease have more severe symptoms that may require help moving around, around-the-clock care, or a wheelchair. Quality of life can decline rapidly.
Risks of infection, incontinence, pneumonia, falls, insomnia, and choking increase.
Hospice care, memory care, home health aides, social workers, and support counselors can be a help in later stages.
Parkinsons disease itself isnt fatal, but complications can be.
Research has shown a median survival rate of about
Dementia Outcomes According To Baseline Sleep Disorders
Among sleep disorders , RBD at baseline dramatically increased the risk of developing dementia . All but one of the converted patients had RBD at baseline ; the only exception was 87 years old with a 22-year history of PD. Of those with RBD, the risk of developing dementia over the 4.4 years follow-up was 43%, compared with 2.5% in those without RBD. Accordingly, the mean percentage of tonic REM sleep EMG activity on baseline polysomnography was higher in dementia-converted participants than in the nonconverted group. The percentage of phasic REM sleep EMG activity was higher in the dementia-converted group, but this was not statistically different when compared with the nonconverted group . By contrast, neither daytime sleepiness, as assessed with the Epworth Sleepiness Scale, nor insomnia, as assessed with the Insomnia Severity Index, was significantly associated with dementia risk in our cohort.
Dementia Outcomes According To Baseline Motor Features
Among motor variables , the proportion of gait involvement at baseline , falls , and freezing predicted dementia. Poor performance on the Purdue Pegboard Test and alternate tap test , but not the UPDRS predicted dementia. Patients developing dementia were more likely to report bilateral onset of motor symptoms . There was no association between dementia status and PD subtype, although the dementia-converted group had slightly more patients with akinetic-rigid Schiess scores than the group without dementia . Baseline UPDRS part III scores, total UPDRS scores, Timed Up and Go, Hoehn and Yahr stage, and axial-limb ratio were not predictive of dementia status.
What Is Needed For A Parkinson’s Disease Dementia Diagnosis
There is no definitive medical test that confirms cognitive decline or dementia in Parkinson’s disease. The most accurate way to measure cognitive decline is through neuropsychological testing.
- The testing involves answering questions and performing tasks that have been carefully designed for this purpose. It is carried out by a specialist in this kind of testing.
- Neuropsychological testing addresses the individual’s appearance, mood, anxiety level, and experience of delusions or hallucinations.
- It assesses cognitive abilities such as memory, attention, orientation to time and place, use of language, and abilities to carry out various tasks and follow instructions.
- Reasoning, abstract thinking, and problem solving are tested.
- Neuropsychological testing gives a more accurate diagnosis of the problems and thus can help in treatment planning.
- The tests are repeated periodically to see how well treatment is working and check for new problems.
Imaging studies: Generally, brain scans such as CT scan and are of little use in diagnosing dementia in people with Parkinson’s disease. Positron emission tomographic scan may help distinguish dementia from depression and similar conditions in Parkinson’s disease.
What Is Parkinsons Disease
PD is a chronic, neurodegenerative movement disorder. PD affects 1 out of every 100 individuals over the age of 601, and patients commonly experience muscle rigidity, changes in speech and walking, and tremors. Some studies suggest that having PD also increases your risk of developing LBD, but most patients have only one of these conditions.2
Theres A Spectrum Of Pathologies
Scientists have been examining this linkand how the two diseases often overlapfor some time, but still arent completely certain how they contribute to one another. As a result, physicians sometimes group the diseases into different combinations when making diagnoses.
Dementia in Parkinsons patients can present itself in varying forms. In some cases, the Parkinsons pathology can trigger the dementia pathologya situation that results in whats known as Parkinsons disease dementia, says Dr. Aaron Ritter, Director of the Clinical Research Program at the Cleveland Clinic Lou Ruvo Center for Brain Health.
A substantial subset of folks with Parkinsons who live long enough, will develop dementia, Ritter said.Its separate from Alzheimers, but its likely related to Parkinsons pathology, a sort of spreading of Parkinsons.
In other cases, patients may develop a form of dementia like Alzheimers separately from their Parkinsons disease, though this isnt visible until after death, through an autopsy.
Many people with Parkinsons may also develop Lewy body dementia shortly after their diagnosis. When you have Parkinsons, and see cognitive declineor things like hallucinations and delusionsup to a year after your Parkinsons diagnosis, you may have Lewy body dementia, Oguh said.
Progression From Normal Cognition To Mci
Throughout the entire sample of 139 non-demented PD patients, the prevalence of PD-MCI at baseline was 44.6% and 39.2% considering only newly diagnosed patients; these rates were close to those reported for the whole PACOS cohort , as well as those regarding other studies .
A lower frequency of MCI at baseline was reported in the Norwegian study , while the study by Cholerton et al. reported a higher prevalence of MCI. The latter result is probably due to the lower cut-off point used for the impairment on specific neuropsychological test .
According to literature data, the most frequent type of MCI at baseline was the multiple domain , both amnestic and non-amnestic, representing the 49.1% and 20.0%, respectively.
At follow-up, 33.3% of PD-NC at the baseline developed MCI and considering only the newly diagnosed patients the frequency was 30.3%. These similar rates probably account for the short disease duration and mild motor impairment of the patients enrolled in the study. To the best of our knowledge, incidence rate of MCI among PD-NC was estimated only for the Norwegian study where an incidence rate of 68.9/1000 pyar was recorded. This rate was lower with respect to our study, but it should be underlined that also a lower frequency of MCI at baseline was reported.
Things You Should Know About The Link Between Parkinsons And Dementia
Both Parkinsons disease and dementia were ravaging the brain and behavior of actor Robin Williams before his death, but at the time, he didnt realize he had the latter.
Despite the fact that the signs of this combination can be confusing, the double diagnosis of Parkinsons and dementia impacts a large number of people. Of the one million people who have Parkinsons in the U.S., 50 to 80 percent may have dementiaeither as a result of Parkinsons pathology, or separately.
Robin Williams widow, Susan, wrote an editorial published in Neurology that was addressed to neurologists after his death. In it, she shared what it was like seeing her husband experience both Parkinsons disease and Lewy body dementia firsthand.
My hope is that it will help you understand your patients along with their spouses and caregivers a little more, Susan wrote.
Williams was first diagnosed with Parkinsons disease, which at first seemed to provide some answers for his out-of-character symptoms.
But it wasnt until after his death that an autopsy revealed he had been in the later stages of Lewy body dementiaa common form of dementia characterized by deposits of Lewy body proteins in the brain, which can impact physical movement, mood, memory and behavior.
I will never know the true depth of his suffering, nor just how hard he was fighting, Susan wrote. But from where I stood, I saw the bravest man in the world playing the hardest role of his life.
Parkinson’s Disease Dementia Surgery And Gene Therapy
- Great strides have been made in the surgical treatment of Parkinson’s disease. Several different procedures are now available, and they are successful in many patients in relieving movement symptoms. Unfortunately, surgery has no effect on cognitive symptoms. In fact, most people with dementia are not candidates for surgery.
- Gene therapy is in its infancy; there are ongoing human and animal trials with various methods to insert genes into neuronal cells to reduce or stop Parkinson’s disease symptoms by causing cells to produce dopamine coded by the newly inserted genes. Early results with the treatment termed ProSavin are encouraging. However, it is not clear if such therapy could prevent or reverse Parkinson’s disease dementia.
Why Is Proper Follow
A person with Parkinsons disease is supposed to go for regular checkups to his health care professional for the following reasons-
Treatment Progress: The check-ups help the health care professionals to check if the treatment procedure is working or not and also provides an insight about the necessary adjustments to be made.
Detecting New Issues- Regular follow-ups help in detection of new problems with cognition, behavior or mood which might need special treatment.
Planning the Care- The follow-ups provide a platform for caregivers to discuss the problems with respect to the patients care.
Presence of Dementia: It can also be known if the patient is susceptible to dementia with the help of regular checkups.
Dementia: It may happen so that the person with Parkinsons disease developing dementia may not be able to take care of himself or take decisions about his healthcare. Thus, caregivers should be extra careful and follow the regular follow-ups with the doctor.
Parkinsons Disease Lewy Body Dementia And Rem Sleep Behavior Disorder Related
Recent research has found that Parkinsons disease, Lewy body dementia and REM sleep behavior disorder are all related. When we are asleep our body goes through different sleep phases, the deepest of which is known as rapid eye movement, or REM. During normal REM our body becomes temporarily paralyzed, and this is where we beginning dreaming. People with REM sleep behavior disorder do not become paralyzed and instead act out their dreams. This can be quite dangerous, not only for the individual, but for others around them as well.
Benjamin L. Walter, M.D., director of the Parkinsons and Movement Disorders Center at University Hospitals Case Medical Center, said to Neurology Advisor, Normally, during REM sleep, reduced serotonergic activity in the brain leads to atonia or loss of muscle tone through action in a network involving brainstem nuclei including the locus subcoeruleus and magnocellularis nucleus. In RBD, this mechanism is dysfunctional, possibly due to pathology in this circuit, and there is not loss of tone during REM sleep.
It has been found that RBD and neurological disorders are related. In fact, up to 60 percent of Parkinsons disease patients suffer from RBD and between 80 to 100 percent of Lewy body dementia patients suffer from the sleep disorder as well.
Can Parkinsons Dementia Be Reversed
No specific cure has been identified for Parkinsons Disease Dementia. Rather, treatments have been aimed at reducing the symptoms of dementia and helping the patient maintain a high quality of life. Doctors treating patients of PD Dementia generally prescribe medications such as:
- Antidepressants
- Cholinesterase inhibitors
- Clonazepam and L-dopa
Serotonin reuptake inhibitors are known to reduce depression symptoms. The ones widely prescribed by doctors include:
- Prozac
- Zoloft and
- Lexapro
Cholinesterase inhibitors help reduce the effects of cognitive decline in people with dementia whereas Clonazepam helps enhance sleep quality. L-dopa helps reduce movement issues caused by PD but runs the risk of making confusion and dementia symptoms worse.
Doctors treating PD Dementia patients may also prescribe antipsychotic drugs but generally do so with caution, the reason being these reduce psychotic episodes but increase Parkinsons symptoms. The use of these drugs may also cause increased confusion and change in consciousness. For the record, Pimavanserin and Nuplazid have been identified as effective antipsychotic drugs.
