Combining Tests Into A Two
Two-stage screening where the first test is relatively inexpensive, but sensitive and moderately specific is an approach that reduces the number of expensive confirmatory tests. Using imaging as the second test in a two-step process reduces costs by lowering the number of scansthat need to be performed. To have a high overall accuracy rate, the first-stage test must be at least as sensitive as imaging. As a secondary screen, imaging can weed-out false positive tests, but it cannot re-capture false-negative cases that were not referred for imaging. The primary screen must also be reasonably specific, because the number of scans that needs to be performed depends on the false positive rate of the primary screening test.
To Support The Diagnosis Your Healthcare Provider Will Also Look For Other Symptoms:
- Micrographia
- Reduced facial expression
- Decreased arm swing or leg drag on one side of the body while walking
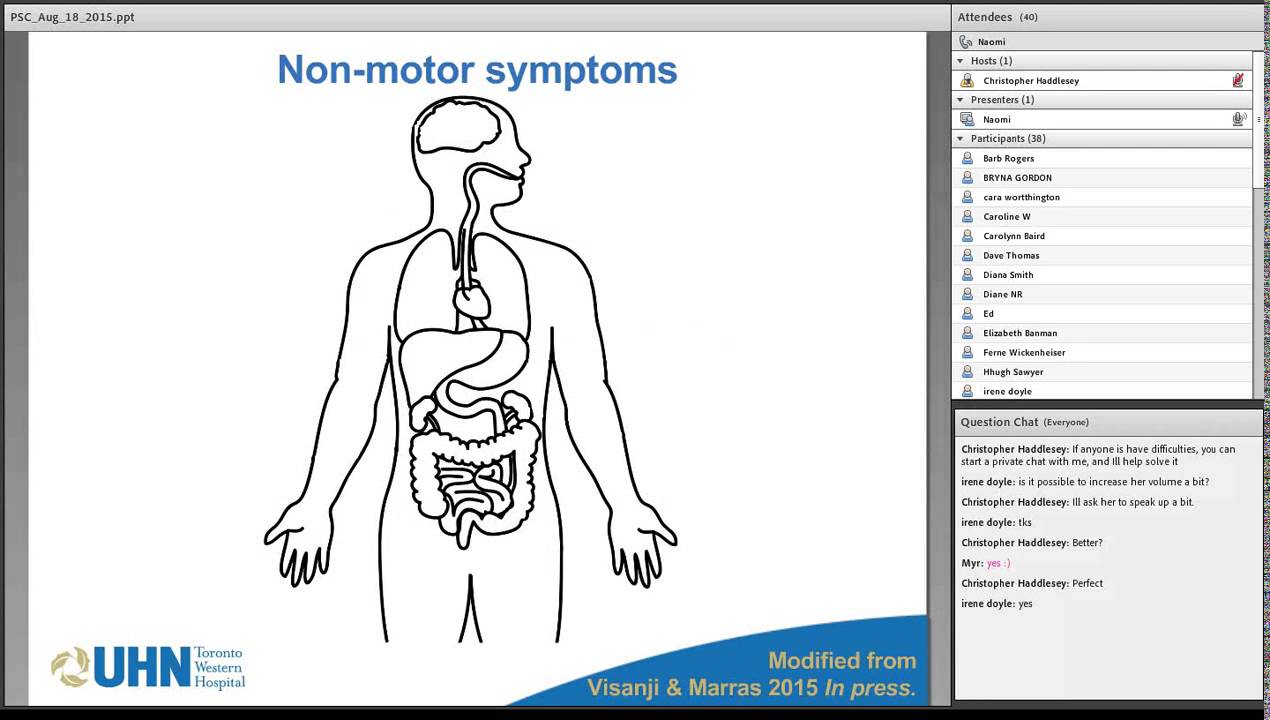
Symptoms such as shoulder pain, depression, sleep problems, constipation and loss of sense of smell can begin long before any of the motor symptoms appear. Because symptoms like these can be subtle at first, they are not always evident or meaningful before diagnosis. It is common after being diagnosed with Parkinsons to look back and realize symptoms had been coming on gradually for months or even years. Often people explore other treatment avenues for early symptoms, like physical therapy or even surgery for pain, only to discover later it was actually connected to Parkinsons.
Since doctors diagnose other medical conditions using sophisticated technology, many are surprised to learn a Parkinsons diagnosis is based on your medical history and a simple examination. While your healthcare provider may take other steps, such as order blood and urine tests, check copper levels and order a brain scan, such as an MRI or CT or DaTscan that measures dopamine, these tests do not diagnose Parkinsons. They are used to either confirm the diagnosis or determine if another medical condition is causing your symptoms.
Everyones experience of Parkinsons will be unique, and a person with YOPD may have similar symptoms as someone diagnosed later in life.
What Types Of Sleep Problems Do People With Parkinsons Disease Have
Parkinsons disease affects every person differently. It also impacts sleep in different ways. People with Parkinsons may have:
- , finding it hard to fall asleep.
- Fragmented sleep, waking up many times over the night.
- Excessive daytime sleepiness, finding it hard to stay awake during the day.
- Very vivid dreams, which may cause hallucinations or confusion after waking up.
- Emotional dreams or nightmares, which may make you feel emotionally drained after waking up.
What If You Have Parkinson’s
After Parkinson’s is diagnosed, your doctor will help you develop an individualized plan to address the symptoms that have the biggest impact on your everyday life and help slow down the progression of the disease. The first step is getting a referral to a neurologist for expert care especially one who is trained in movement disorders.
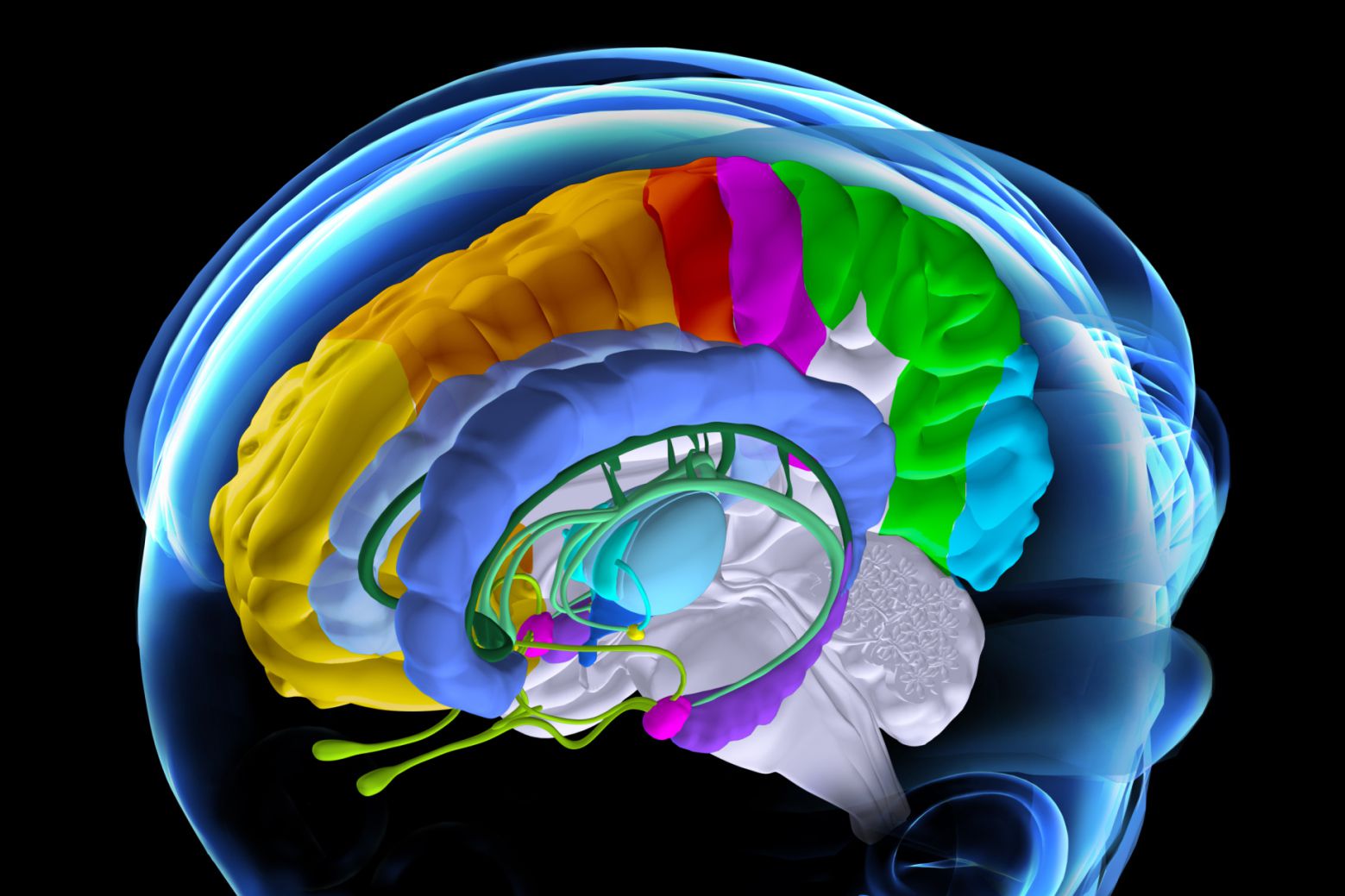
Braaks Hypothesis On How Parkinsons Disease Begins
Braaks hypothesis, named for professor Heiko Braak, MD, who outlined the theory in 2003, suggests that rather than beginning in the brain, Parkinsons disease begins in the periphery of the body. Braaks hypothesis proposes that the earliest signs of PD are found in the gut and the olfactory bulb, an area of the brain involved in the sense of smell.2-4
The accumulation of the protein is believed to begin in the gastrointestinal tract or the olfactory bulb before progressing to other areas of the brain. After the aggregates of alpha-synuclein have formed, they appear to be capable of growing and spreading from nerve cell to nerve cell across the brain.2-4
The appearance of alpha-synuclein aggregates coincides with the appearance of symptoms: alpha-synuclein aggregates in the brainstem correlates with the onset of motor symptoms. Appearance of alpha-synuclein aggregates in the cortex correlates with dementia and cognitive dysfunction.2-4
Neuropsychiatric Symptoms And Dementia
Visual hallucinations and illusions are common in PD and reportedly occur in a third to 40% of patients . Although virtually all anti-parkinsonian medications have been reported to induce hallucinations and psychosis, visual hallucinations have also been reported to occur prior to drug treatment . Neuropathological changes in the amygdala and hippocampus caused by the disease process seem to be implicated in the aetiology . Frequently, images of people, small animals or objects are conceived or the hallucinations may have multiple content. The images may be familiar or not. They last from seconds to minutes, and may recur over the day . Usually, non-demented patients retain insight and the hallucinations are usually not threatening. Less commonly, the hallucinations are olfactory , auditory and tactile . One study showed that visual component was lacking in 10% of cases . Minor visual phenomena such as sense of presence and visual illusions affect 1772% of patients and delusions about 5% . Higher load of dopaminergic treatment may be related to the hallucinations, but disease severity, cognitive impairment, depression, older age and worse visual acuity may also be important .
What Lifestyle Changes Can I Make To Ease Parkinsons Symptoms
Exercise helps improve muscle strength, balance, coordination, flexibility, and tremor. It is also strongly believed to improve memory, thinking and reduce the risk of falls and decrease anxiety and depression. One study in persons with Parkinsons disease showed that 2.5 hours of exercise per week resulted in improved ability to move and a slower decline in quality of life compared to those who didnt exercise or didnt start until later in the course of their disease. Some exercises to consider include strengthening or resistance training, stretching exercises or aerobics . All types of exercise are helpful.
Eat a healthy, balanced diet: This is not only good for your general health but can ease some of the non-movement related symptoms of Parkinsons, such as constipation. Eating foods high in fiber in particular can relieve constipation. The Mediterranean diet is one example of a healthy diet.
Preventing falls and maintaining balance: Falls are a frequent complication of Parkinson’s. While you can do many things to reduce your risk of falling, the two most important are: 1) to work with your doctor to ensure that your treatments whether medicines or deep brain stimulation are optimal; and 2) to consult with a physical therapist who can assess your walking and balance. The physical therapist is the expert when it comes to recommending assistive devices or exercise to improve safety and preventing falls.
Improve the quality of your sleep.
Living With Parkinsons Disease
Depending on severity, life can look very different for a person . As a loved one, your top priority will be their comfort, peace of mind and safety. Dr. Shprecher offered some advice, regardless of the diseases progression. Besides movement issues Parkinsons Disease can cause a wide variety of symptoms including drooling, constipation, low blood pressure when standing up, voice problems, depression, anxiety, sleep problems, hallucinations and dementia. Therefore, regular visits with a experienced with Parkinsons are important to make sure the diagnosis is on target, and the symptoms are monitored and addressed. Because changes in your other medications can affect your Parkinsons symptoms, you should remind each member of your healthcare team to send a copy of your clinic note after every appointment.
Dr. Shprecher also added that maintaining a healthy diet and getting regular exercise can help improve quality of life. Physical and speech therapists are welcome additions to any caregiving team.
Naturalremedy For Parkinsons #10 Foods You Must Avoid
There are certain foods that are known to worsen thesymptoms of Parkinsons and certain foods that are known to help. Healthadvocate, Dr Joseph Mercola, says that Parkinsons disease is primarily relatedto poor lifestyle choices, particularly poor dietary habits. Increasing yourbodys natural dopamine levels is also extremely important in your fight againstPD.
The foods and liquids you should be eating and drinkingmore of to help you along include:
· Clean Filtered Water Clean filtered water helpsto flush toxins from the body and hydrate the cells .Try and aim to drink at least two liters of water every day, and under nocircumstances drink tap water! Tap water is laced with toxic fluoride and otherchemicals and heavy metals so NEVER drink it. Buy yourself a good quality waterfilter. Its worth the investment.
· Whole Foods and Raw Foods Eat plenty oforganic mixed berries, green leafy vegetables, liver , fish,eggs, nuts and seeds such as chia and flaxseeds, along with plenty of herbs andspices. When it comes to buying any of these remember fresh is alwaysbest.
· Consume Lots of Good gutbacteria are needed for strong immunity and healthy digestive function, whichin turn produces healthy brain and nerve function. You can learn how to makeyour own probiotic rich foods such as kefir, sauerkraut, kombucha and yogurt hereCultures for Health.
The foods you should be avoiding or not eating at allinclude:
What Is The Treatment For Parkinson’s Disease
There is currently no treatment to cure Parkinson’s disease. Several therapies are available to delay the onset of motor symptoms and to ameliorate motor symptoms. All of these therapies are designed to increase the amount of dopamine in the brain either by replacing dopamine, mimicking dopamine, or prolonging the effect of dopamine by inhibiting its breakdown. Studies have shown that early therapy in the non-motor stage can delay the onset of motor symptoms, thereby extending quality of life.
The most effective therapy for Parkinson’s disease is levodopa , which is converted to dopamine in the brain. However, because long-term treatment with levodopa can lead to unpleasant side effects , its use is often delayed until motor impairment is more severe. Levodopa is frequently prescribed together with , which prevents levodopa from being broken down before it reaches the brain. Co-treatment with carbidopa allows for a lower levodopa dose, thereby reducing side effects.
In earlier stages of Parkinson’s disease, substances that mimic the action of dopamine , and substances that reduce the breakdown of dopamine inhibitors) can be very efficacious in relieving motor symptoms. Unpleasant side effects of these preparations are quite common, including swelling caused by fluid accumulation in body tissues, drowsiness, , , hallucinations, and .
Disturbances In Autonomic Function
Autonomic dysfunction may present prior to the diagnosis or become apparent with disease progression or be induced by medication . All areas of autonomic function may be affected and this has been reported to affect daily life of over 50% of patients . The autonomic dysfunction is considered because of involvement of both the central and peripheral postganglionic autonomic nervous system . Orthostatic hypotension affects 3040% of patients. This is defined as a fall in systolic blood pressure of > 20 mm Hg or in diastolic blood pressure > 10 mm Hg on either standing or head-up tilt to at least 60 degrees within 3 min . On assuming the upright posture, hypotension-induced hypoperfusion of the brain can result in dizziness, visual disturbances and impaired cognition that may precede loss of consciousness. In PD, the blood pressure drop may last several minutes . Duration of PD may be unrelated to the occurrence of orthostatic hypotension . In elderly PD patients, this may mainly occur after food intake .
Gastrointestinal symptoms are common. There is slowing of mobility of the gastrointestinal tract with symptoms such as postprandial fullness and gastric retention, but slow-transit constipation is by far the most common, occurring in 7080% . Patients may also experience difficulties in rectal evacuation because of rectal sphincter dysfunction .
Naturalremedy For Parkinsons #7 Omega
Animal based omega-3 fatty acids are a powerful weapon inthe fight against Parkinsons disease. One of the main fatty acids, DHA, is oneof the essential building blocks for the human brain. Half of your brain andeyes are made up of fat and a large proportion of this is DHA fat.
Omega-3 fatty acids have the unique ability to cross theblood-brain barrier, something most conventional drugs cannot do. They helpincrease dopamine levels and reduce neuroinflammation in the brain, while atthe same time, stimulating neuron growth. So basically, EPA and DHA help preventbrain cell damage and keep the nervous system in tip top working order!
Best sources of animal based omega-3s are either fishoil, cod liver oil or krill oil. High strength krill oil is the preferred option as thiscontains a substance called Astaxanthin. Astaxanthin is a potent brain food nutrientthat has been shown to prevent neurodegeneration and inflammation of the brain.For dosages, take AT LEAST the highest recommended amount listed on the bottle the same goes with fish oil or cod liver oil. You cant overdose on thesesupplements so theres nothing to be concerned about. In fact, the more omega-3syou can get into you the better the results!
In addition to this, try and eat some cold water fattyfish such as salmon, tuna, mackerel, sardines or herring 3-4 times a week foran extra supply of DHA and EPA.
Diagnosing Early Onset Parkinsons Disease
There is no single test to detect Parkinsons. A diagnosis may be difficult and take a while. The condition is usually diagnosed by a neurologist based on a review of your symptoms and a physical exam.
A DaTscan to visualize your brains dopamine system may help confirm diagnosis. Blood tests and other imaging tests, such as an MRI scan, dont diagnose Parkinsons. However, they may be used to rule out other conditions.
What Are The Different Stages Of Parkinsons Disease
Each person with Parkinsons disease experiences symptoms in in their own unique way. Not everyone experiences all symptoms of Parkinsons disease. You may not experience symptoms in the same order as others. Some people may have mild symptoms; others may have intense symptoms. How quickly symptoms worsen also varies from individual to individual and is difficult to impossible to predict at the outset.
In general, the disease progresses from early stage to mid-stage to mid-late-stage to advanced stage. This is what typically occurs during each of these stages:
Early stage
Early symptoms of Parkinsons disease are usually mild and typically occur slowly and do not interfere with daily activities. Sometimes early symptoms are not easy to detect or you may think early symptoms are simply normal signs of aging. You may have fatigue or a general sense of uneasiness. You may feel a slight tremor or have difficulty standing.
Often, a family member or friend notices some of the subtle signs before you do. They may notice things like body stiffness or lack of normal movement slow or small handwriting, lack of expression in your face, or difficulty getting out of a chair.
Mid stage
Mid-late stage
Standing and walking are becoming more difficult and may require assistance with a walker. You may need full time help to continue to live at home.
Advanced stage
Do People Actually Lose Their Sense Of Smell With Parkinson’s
A: Yes. It’s a condition called anosmia, and if you have it with no other disease , you have at least a 50 percent chance of developing Parkinson’s disease in the next five to 10 years. What happens is that alpha-synuclein, the protein that clumps in the part of the brain that regulates dopamine and leads to Parkinson’s disease, also aggregates in the olfactory bulb, the part of the brain responsible for your sense of smell. This happens well before the protein accumulations cause motor symptoms.
What Else Can I Do To Sleep Better With Parkinsons Disease
Practicing healthy sleep hygiene habits may also promote more restful .
Do:
- Get outside during the day. Bright light tells your body its time to be awake.
- Keep your body moving during the day. Even if all you feel up to is a short walk or two, all physical activity offers benefits.
- Try at-home remedies, such as massage or a warm bath. Relaxing your mind may help your body fall asleep.
Dont:
- Take long naps during the day.
- Use stimulants, such as , within six hours of bedtime.
- Use your bedroom for activities other than sleeping. Go to another room to read, watch TV or work.
What Is The Outlook For Persons With Parkinsons Disease
Although there is no cure or absolute evidence of ways to prevent Parkinsons disease, scientists are working hard to learn more about the disease and find innovative ways to better manage it, prevent it from progressing and ultimately curing it.
Currently, you and your healthcare teams efforts are focused on medical management of your symptoms along with general health and lifestyle improvement recommendations . By identifying individual symptoms and adjusting the course of action based on changes in symptoms, most people with Parkinsons disease can live fulfilling lives.
The future is hopeful. Some of the research underway includes:
- Using stem cells to produce new neurons, which would produce dopamine.
- Producing a dopamine-producing enzyme that is delivered to a gene in the brain that controls movement.
- Using a naturally occurring human protein glial cell-line derived neurotrophic factor, GDNF to protect dopamine-releasing nerve cells.
Many other investigations are underway too. Much has been learned, much progress has been made and additional discoveries are likely to come.
Is Parkinsons Disease Inherited
Scientists have discovered gene mutations that are associated with Parkinsons disease.
There is some belief that some cases of early-onset Parkinsons disease disease starting before age 50 may be inherited. Scientists identified a gene mutation in people with Parkinsons disease whose brains contain Lewy bodies, which are clumps of the protein alpha-synuclein. Scientists are trying to understand the function of this protein and its relationship to genetic mutations that are sometimes seen in Parkinsons disease and in people with a type of dementia called Lewy body dementia.
Several other gene mutations have been found to play a role in Parkinsons disease. Mutations in these genes cause abnormal cell functioning, which affects the nerve cells ability to release dopamine and causes nerve cell death. Researchers are still trying to discover what causes these genes to mutate in order to understand how gene mutations influence the development of Parkinsons disease.
Scientists think that about 10% to 15% of persons with Parkinsons disease may have a genetic mutation that predisposes them to development of the disease. There are also environmental factors involved that are not fully understood.
What Is And Isn’t Parkinson’s Disease
I am often asked if Parkinson’s Disease is a form of Alzheimers. is not Alzheimers, or a brain tumor, and the prognosis for Parkinson’s, though not a perfect scenario, leaves room to live a productive life.
PD is a progressive and chronic neurological disease that often begins with mild symptoms that advance gradually over time. Symptoms can be so subtle in the early stages that they go unnoticed, leaving the disease undiagnosed for years. For patients with Parkinson’s, there is a reduction in the body chemical , which controls movement and mood so simple activities like walking, talking and writing can be impacted.
Due to the complexity of PD, diagnosis is based on a variety of factors. The best diagnosis is made by an expert doing a careful history and exam followed by tracking responses to therapy. There is no blood or laboratory test to diagnose Parkinson’s disease.
While Parkinson’s reaches all demographics, the majority of people with PD are age 60 or older. Men and people with a family history of the disease have an increased risk.
What Are The Surgical Treatments For Parkinsons Disease
Most patients with Parkinsons disease can maintain a good quality of life with medications. However, as the disease worsens, medications may no longer be effective in some patients. In these patients, the effectiveness of medications becomes unpredictable reducing symptoms during on periods and no longer controlling symptoms during off periods, which usually occur when the medication is wearing off and just before the next dose is to be taken. Sometimes these variations can be managed with changes in medications. However, sometimes they cant. Based on the type and severity of your symptoms, the failure of adjustments in your medications, the decline in your quality of life and your overall health, your doctor may discuss some of the available surgical options.
Why Is Expert Care Important
Early expert care can help reduce PD complications. Findings show that 60 percent of people with Parkinson’s fall short of getting the expert care they need. The National Parkinson Foundation has estimated that about 6,400 people with Parkinson’s die unnecessarily each year due to poor care.
Trained neurologists will help you recognize, treat and manage the disease. Common approaches include , surgical treatment, lifestyle modifications , physical therapy, support groups, occupational therapy and speech therapy. The best approach is interdisciplinary care, where you are seen by multiple specialists on a regular basis and all of the specialists talk and arrange the best possible coordinated care. This is what is referred to as a patient-centric approach to Parkinson’s care.
Stooping Or Hunched Posture
People who have Parkinsons disease may notice changes in their posture due to other symptoms of the disease, such as muscle rigidity.
People naturally stand so that their weight is evenly distributed over their feet. However, people who have Parkinsons disease may start bending forward, making them appear hunched or stooped over.
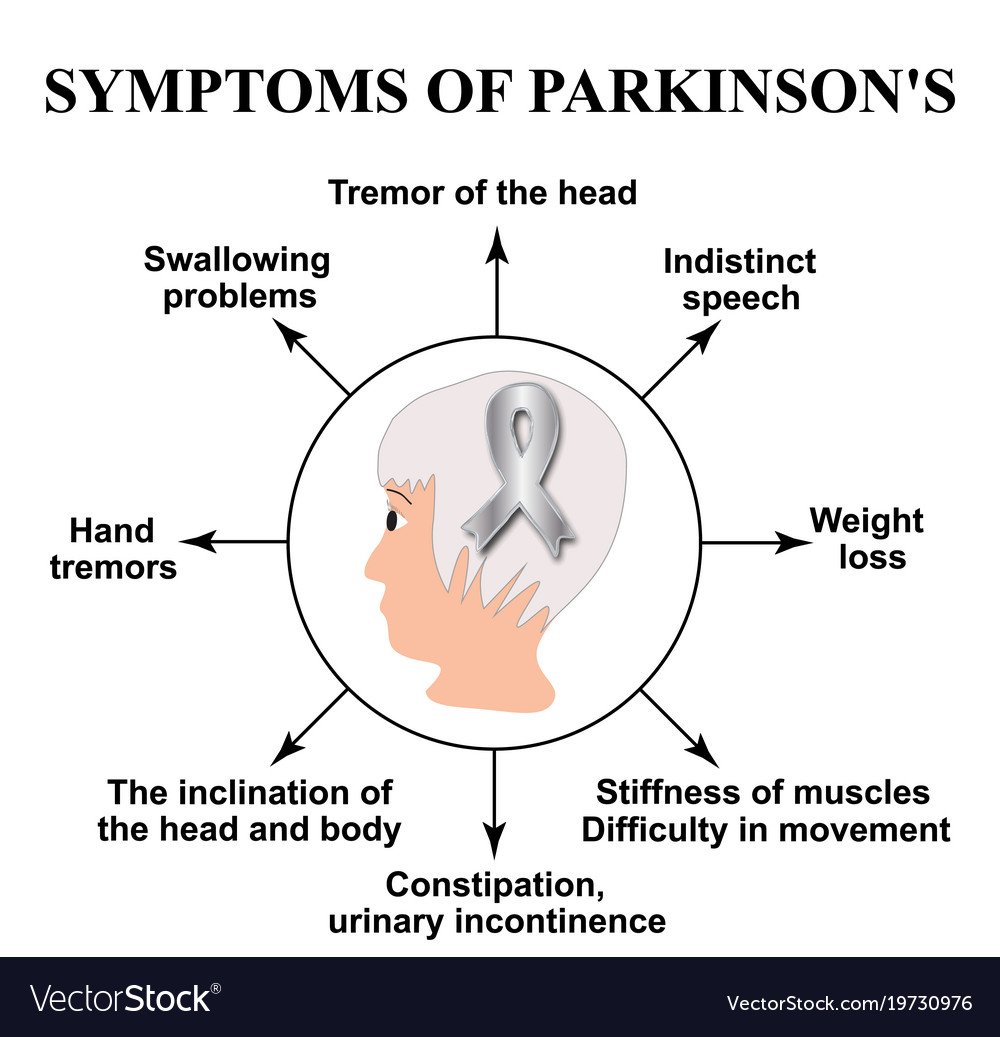
The Impacts Of Parkinsons On Movement Are Called Motor Symptoms Primary Motor Symptoms Include:
- Tremor: a rhythmic shaking in your arms, legs or chin. Most people with Parkinsons who experience tremor that is worse when relaxing and resting have rest tremor. Others experience active tremor, which means their shaking will worsen when trying to do something, like drinking out of a cup of coffee or eating with a spoon.
- Rigidity: painful stiffness, often in the arms, legs, neck or back muscles.
- Akinesia, Bradykinesia, Hypokinesia:Akinesia and bradykinesia refer to the reduction of movement, slowness of movement and sometimes even complete lack of movement that can be caused by Parkinsons. Hypokinesia refers to a loss of momentum or force in movement that can come with Parkinsons, usually in connection with akinesia, bradykinesia or both. The small, cramped handwriting that some people with Parkinsons experience is thought to be some combination of akinesia and hypokinesia.
- Postural Instability: balance problems caused by a loss of reflexes that help you stay upright. This can cause challenges with general balance as well as walking . Sometimes postural instability brings the tendency to fall backward, called retropulsion.
Early motor symptoms can also include a mask-like face or loss of facial expression, small, cramped handwriting and decreased natural arm swing.
People often complain of a heaviness feeling, dragging of one side or cramping in certain muscles. Speech can become softer and more difficult as Parkinsons progresses and swallowing can also be affected.
Whats The Relationship Between Parkinsons And Sleep
Parkinsons disease and sleep are connected in complex ways that not even scientists completely understand quite yet.
Sometimes, Parkinsons disease directly causes sleep problems. According to one study, sleep-related symptoms may be one of the earliest signs of Parkinsons disease. These signs may include things like thrashing while youre asleep.
Other factors can also play a role. One thing is clear: For many people with Parkinsons disease, a restful nights sleep can be hard to find.
Potential Precursors To Parkinson’s Disease
As part of my PhD research project on non-motor symptoms in Parkinsons disease, I often speak to patients and their families or caregivers, who always seem eager to learn more about this aspect of the disease.
Recently, a patients wife asked about a number of non-motor symptoms her husband experienced for several years before his diagnosis. She wondered whether these problems were early clues to his underlying Parkinsons disease.
The truth is that neurologists dont know for sure if these problems increase the risk for Parkinsons disease or are pre-clinical signs or symptoms of the disease itself. But, I can share what we now know about these non-motor symptoms.
1. Rapid eye movement sleep behavioral disorder : This is a sleep disorder in which people act out their dreams due to a lack of normal paralysis during the dreaming, or so-called REM, stage of sleep. RBD can be identified through a formal study called polysomnography, in which experts monitor important physiological signs such as oxygen levels during sleep. In a recent study in Neurology, about 70 percent of patients with RBD showed signs of a neurodegenerative disease 10 years later.
4. Depression and anxiety: These symptoms often occur in tandem and are associated with many different neurologic conditions, including Parkinsons disease. Excessive daytime fatigue, which can occur on its own or alongside depression, may also be a possible precursor.
Questions Remain

