What Types Of Hallucinations Can People With Parkinsons Experience
Visual hallucinations are the most common in Parkinsons disease. Auditory hallucinations occur mainly in depression. Tactile or olfactory sensations are unusual.
Often the symptom starts with lively dreams, then illusions, then hallucinations at night-time. After that hallucinations can also appear in the day. Initially the patient understands that the experience is a hallucination, but if things progress it becomes difficult to say what is real and not.
Further progression could mean that the hallucinations become scary, and patients can develop confusion or delusions . Auditive hallucinations are seldom linked to Parkinsons.
Mild hallucinations do not need to impact life very much, and can even be experienced as entertaining in some cases. But when the hallucinations become more pronounced and it is difficult to differentiate them from reality, they can have a big effect.
Per Odin is a neurologist, professor and head of the neurology department at Lund University, Sweden.
Examples Of Delusions In Pd
- Jealousy
- Belief: Your partner is being unfaithful.
- Behavior: Paranoia, agitation, suspiciousness, aggression.
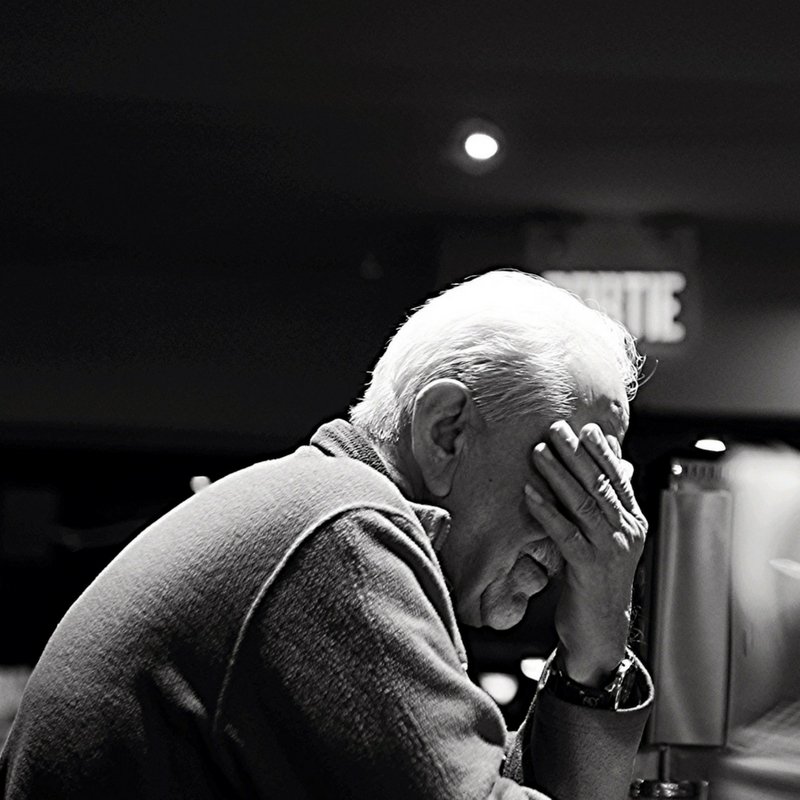
Parkinsons Disease And The Perfect Golf Swing: Reflections On My Dad
The earliest memories I have of my dad are of him practicing his golf swing in front of a mirror. It was a beautiful golf swing, perfected through hours upon hours of repetition. He loved the game. He was very physically fit, as a U.S. Marine. He would routinely do 100 push-ups and then run around the neighborhood in his black Marine Corps boots to assure he kept his callouses for reserve weekends. It was the late 1960s.
He must be a great player, I thought. It took me a few years to realize that my dad did not play golf.
My dad was the oldest son of Irish immigrants. At the age of 18, two weeks into his freshman year at Iona College, my dad received the news that he had a new sibling, a brother. This brother, his youngest, was born with Downs Syndrome. This news would impact my dads life in ways he couldnt have imagined.
Dad completed his graduate studies, began his career in public education and bought his first house. He changed the oil in his old Volkswagens and tuned up the lawnmower to save money. As he pushed the mower past the picture window at the front of our house, he would stop and practice his golf swing in the reflection, so he would be ready for the day when he had the time and resources to play.
Memory Problems And Dementia
Research shows that hallucinations and delusions often happen when someone with Parkinsons also has problems with memory, thinking problemsor dementia.
If you experience hallucinations at an early stage of Parkinsons, it could be a sign of another medical condition, such as dementia with Lewy bodies.
Should You Put Your Dog Down If Their Parkinsons Is Bad

I cannot answer that question for you. Your decision to euthanize a dog with Parkinsons disease is highly personal. If your dogs quality of life is truly poor, with no independence at all, the kinder thing may be to put them down.
Its a decision we never want to make, but sometimes it really is the best thing for them.
Consult your veterinarian for advice on how long your dog can expect to remain mobile and when euthanasia may be the sole solution.
In That Moment I Got A Glimpse Of My Dad The Real One
The one who raised three kids and taught us how to throw a football, how to use a hammer, how to treat people. The one who, in another world, would have been leading me through the airport, reciting Civil War trivia as we walked. The one who, to an outsider, would have been just a guy.
The one who, to those who knew him, was far from just a guy.
Whats The Connection Between Paraquat And Parkinsons
Paraquat is a toxic herbicide, and people exposed to paraquat can develop multiple health issues, such as pain, vomiting, and diarrhea. Paraquat exposure can lower your blood pressure, and ingesting even small amounts can cause severe health problems, including kidney failure and heart failure.
Ingesting large quantities can trigger a coma, cause muscle weakness, produce respiratory issues, or cause seizures. The U.S. Centers for Disease Control and Prevention reports that ingesting large amounts of paraquat is typically fatal. Studies indicate paraquat exposure can cause Parkinsons. These studies provide legal grounds for lawsuits against paraquat producers when exposure to paraquats linked to Parkinsons disease.
Selfcare For The Person With Parkinsons
- Join a Parkinsons support group if you dont already belong to one. Talk about your experiences, ask for help if you need it and share whats worked and not worked for you.
- Offer to have coffee with someone you know has been newly diagnosed and offer them support and encouragement.
- Make time to exercise and get out in nature every day.
- Communicate frequently with your doctors and discuss the possibility of tweaking your medications if your symptoms become worse.
- Rest when you need it.
- Plan a day trip or a vacation and get away from your normal surroundings.
- Take control where you can and keep authoring your own story.
- Practice or or Tai Chi to relax and calm your mind.
- Start a new project that youre excited to work on every day.
- Communicate with your care partners and let them know how they can best help you.
What Are The Considerations For Pain Management In The Last Days Of Life In Pd
It is important to consider that pain can be a risk factor for, and associated with, many other symptoms which might be the presenting features in a patient with complex or advanced PD. These include a new or worsened confusion, hallucinations, agitation and symptoms of depression or apathy.
As well as being an underlying cause of another symptom, pain can also be the symptom of other features of PD, such as rigidity, dyskinesia, but also non-motor features, for example, depression and fatigue.
Identifying whether pain is at the root of the presenting complaint and what might be causing the pain is therefore the most important part of the initial history from the patient and the carer. Then using the clinical examination to confirm findings from the history and identify any features not already elicited such as abnormal posturing, or dystonia.
A recent review into the pathophysiology and treatment of pain in PD suggests simple analgesia with paracetamol and non-steroidal anti-inflammatory drugs but advises caution with opiate analgesia as constipation is a recognised problem in PD patients.25The review mentions, however, the lack of evidence for many widely used analgesics specifically in PD.26
What Is A Delusion
A delusion is a thought or belief that is not based on reality, as opposed to a hallucination which involves seeing, hearing, tasting or feeling things that do not exist.
People who experience delusions may be convinced that they are true, even though they are irrational – for example paranoia – that someone is trying to cause them harm or that there is a conspiracy against them. Delusions can be difficult to overcome, particularly if they involve a carer or other close contact, as they may provoke suspicion, mistrust or jealousy and so strain relationships. Severe delusions can cause anxiety or irritability, especially if the person finds it difficult to tell whether things are real or not.
Some people with Parkinson’s experience a mixture of delusions, hallucinations and illusions which may make them feel confused and impact on daily life.
What Is The Link Between Seizures And Dementiablog
There are some symptoms of dementia that are more commonly known, such as memory loss. Seizures are a less common symptom of dementia that are not as understood. Hear from one of our dementia researchers who has been studying seizures in people with the condition.
How common are epileptic seizures in dementia? Who is most at risk of having them? What do these seizures look like? What effect do they have on how someones memory changes over time?
These are the questions that I have been researching since starting my PhD in 2016.Im astudent funded by Alzheimers Society as part of the University of Exeter doctoral training centre.
A Positive Mental Attitude
Focusing on the positive ways you can help your parent instead of worrying about how to prevent their Parkinsons from worsening can help to remove stress and anxiety from the situation.
While there are many treatments to ease your parents symptoms theyll benefit enormously from having their family and friends around them, supporting them as they face such a degenerative disease. Love, acceptance and friendship go a long way when caring for a parent with Parkinsons.
Volunteer To Help Out

Everyday responsibilities like shopping, cooking, and cleaning become much more difficult when you have a movement disorder. Sometimes people with Parkinsons need help with these and other tasks, but they may be too proud or embarrassed to ask for it. Step in and offer to run errands, prepare meals, drive to medical appointments, pick up medications at the drug store, and help with any other day-to-day tasks they have difficulty with on their own.
Demystifying Hallucinations Night Terrors And Dementia In Parkinsons
This two-hour webinar includes extensive discussion about hallucinations, delusions, illusions and other examples of Parkinsons psychosis in Parkinson’s. Presenters: Rohit Dhall, MD, MSPH and Vergilio Gerald H. Evidente, Director, Movement Disorders Center of Arizona in Scottsdale. Pay particular attention to Dr. Rohit Dhalls description of the causes of PD psychosis as well as treatment options and what to discuss with your movement disorder specialist. Dr. Evidente gives a clear description on differences in PD dementia, Alzheimer’s and other dementias.
Hallucinations Delusions And Parkinson’s
It is estimated that about 50% of people with Parkinsons will, at some point, experience hallucinations. They can affect younger people but are more often associated with those who are older and have had Parkinsons for some time.
Hallucinations experienced early in Parkinsons may also be a symptom of the condition dementia with Lewy bodies so it is important to let your doctor know if hallucinations begin at an early stage.
Parkinsons itself can be a cause of hallucinations and delusions, but very often they are a side effect of certain medications used to treat the condition. Not everyone who takes Parkinsons medications will experience hallucinations and delusions though. This varies from person to person and is often related to the particular type of medication and dosage.
Other factors may also be involved such as underlying illness, memory problems, sleep difficulties and poor eyesight.
Practical Tips For Caregivers Of People With Parkinson’s Psychosis
This 2-page tip sheet has bullet point suggestions for what to do if the person you care for experiences hallucination, delusions or confusion, or becomes agitated or aggressive. In addition, there are tips for how to best be prepared for a doctors appointment when you bring this behavior to the attention of your medical team.
How To Avoid Dip
The incidence rate of DIP has proved difficult to assess, due to the prevalence of misdiagnosis as PD. Older people and women are at higher risk of DIP, and genetic factors may also play a role.2
The only way to develop DIP is by taking a prescription drug that impacts the brains dopamine system. If you dont take those drugs, you cannot develop it.
Unfortunately, in some cases, DIP is misdiagnosed as PD. Researchers discovered that 6.8% of patients diagnosed with PD were later reclassified as having DIP.3 This mistake is particularly harmful since doctors may prescribe drugs to manage PD symptoms instead of stopping the drug thats causing DIP.
Discontinuing the responsible drug most often ends DIP. However, in some cases, the symptoms persist. In others, the parkinsonism continues to worsen along a track consistent with PD. Researchers have postulated that in these cases the drugs unmasked PD, which may have otherwise gone unexpressed.
Synopsis
If you dont take a prescription drug that causes DIP, then you cannot develop it. People experiencing DIP can usually end it by discontinuing the medication that caused it, but for some people, the symptoms persist or worsen.
Diagnosis And Treatment Of Hallucinations
First, your doctor needs to find out what’s causing your hallucinations. They’ll ask about your medical history and do a physical exam. Then they’ll ask about your symptoms.
They may need to do tests to help figure out the problem. For instance, an EEG, or , checks for unusual patterns of electrical activity in your brain. It could show if your hallucinations are due to seizures.
You might get an MRI, or magnetic resonance imaging, which uses powerful magnets and radio waves to make pictures of the inside of your body. It can find out if a brain tumor or something else, like an area that’s had a small , could be to blame.
Your doctor will treat the condition that’s causing the hallucinations. This can include things like:
- Medication for schizophrenia or dementias like Alzheimer’s disease
- Antiseizure drugs to treat epilepsy
What Are The Complications Of Parkinson Disease
Parkinson disease causes physical symptoms at first. Problems with cognitive function, including forgetfulness and trouble with concentration, may arise later. As the disease gets worse with time, many people develop dementia. This can cause profound memory loss and makes it hard to maintain relationships.
Parkinson disease dementia can cause problems with:
- Speaking and communicating with others
- Problem solving
- Forgetfulness
- Paying attention
If you have Parkinson disease and dementia, in time, you likely won’t be able to live by yourself. Dementia affects your ability to care of yourself, even if you can still physically do daily tasks.
Experts don’t understand how or why dementia often occurs with Parkinson disease. Its clear, though, that dementia and problems with cognitive function are linked to changes in the brain that cause problems with movement. As with Parkinson disease, dementia occurs when nerve cells degenerate, leading to chemical changes in the brain. Parkinson disease dementia may be treated with medicines also used to treat Alzheimer’s disease, another type of dementia.
How Can You Improve Aggressiveness And Hallucinations In Parkinsons
Hallucinations may spark anger or aggression in a person with Parkinsons disease. Some ways to help include:
- Reassure them, tell them they are safe.
- Speak slowly and calmly.
- Ask questions about the persons feelings.
- Listen to the person, dont interrupt.
- Avoid sudden movements.
- Give the person space and a way out, so they dont feel cornered or threatened.
- Make an emergency plan ahead of time for what you and others in the house will do if the person experiencing hallucinations becomes a danger to themselves, you, or anyone else.
- When it is safe, help the person speak with their healthcare provider about making a plan to address the hallucinations.
Confronting The Unspoken Truth Of My Fathers Life With Parkinsons
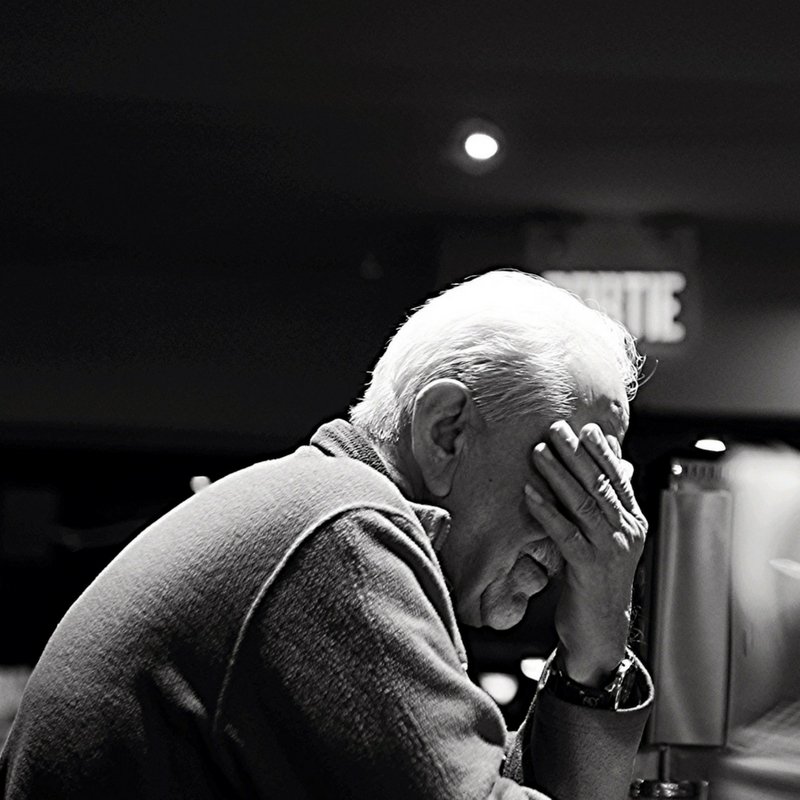
Now that I have seen and treated many people faced with chronic illness, like living with Parkinsons, I truly feel it is better not to go through it alone.
I first noticed my fathers when I came home for vacation during my first year of medical school. While we were driving back to the house from the airport, I saw something moving in the periphery of my vision. My father was sitting in the passenger seat, his left hand shaking. He saw me glancing at it and explained that the tremor had started a few weeks ago. As a physician himself, he came up with some fancy explanations for the cause. None of them included .
As the years went by, I noticed subtle changes in him. Every few months when I came home from school, he seemed a little different. His gait deteriorated, becoming more slowed and shuffled, and his posture more stooped. It was obvious that his sleeping patterns had become disrupted: I would find him napping throughout the day; at night, he would often wake up from vivid nightmares.
Even his face began to changeit seemed less expressive and animated. His speech grew softer, he mumbled, and he had to repeat himself often. In a matter of a few years, my father had transformed into a different person, a man with textbook PD symptoms. On the outside, he no longer resembled the tall, strong, bold man I knew to be my dad. But inside, his mind and his heart remained the same.
Showing Up As Your Best Self
Caring for someone with a progressive condition like Parkinsons disease can be challenging. Hallucinations only add to the stress of caregiving, especially if the person youre caring for doesnt have insight into what theyre experiencing.
The more you understand about your loved ones condition, the easier itll be to care for them. Talk to their doctor and read up on Parkinsons disease so youre better equipped to respond when hallucinations occur.
Dont forget to take care of yourself as well. Take regular breaks from caregiving to relax and do the things you enjoy. By tending to your own needs, youll have more energy to devote to your loved one.
Types Of Eye Movements
There are three kinds of eye movements that can change with PD:
- Saccadic rapid eye movements direct us to gaze at a specific object or to read lines of print.
- Pursuit eye movements allow us to follow an object as it moves.
- Vergence eye movements allow us to move our eyes in different directions2
Changes to these eye movements due to Parkinsons can also result in different kinds of visual difficulties. The inability to control eye movements can lead to involuntary blinking, double vision and other motor issues that can affect visual acuity.
Dry eyes can be treated with drops or ointments, warm wet compresses, but are not generally cured. The blink reflex can be impacted by PD. This manifests as either a slowing of the reflex, appearing as inappropriate staring, dry or burning eyes; and by reduced vision. Blepaharospasm and apraxia are two common eyelid motion issues. Blephararospasms are eyelid spasms that cannot be controlled, cause eyelids to squeeze, and can be relieved with Botox injections. Apraxia is a condition that makes it difficult to open eyes. There are specialized lid crutches and cosmetic tape that can be applied to hold the eyelids open.2
What Are Parkinsons Hallucinations
Symptoms of psychosis occur in up to 50% of people with Parkinsons disease.
Parkinsons disease psychosis is considered a neuropsychiatric condition. This means it involves neurology and psychiatry . While the psychosis involves mental health symptoms, they are caused by Parkinsons disease, which is a disease of the nervous system.
Psychosis in Parkinsons disease comes in two forms:
- Hallucinations: Sensory experiences that are not really happening
- Delusions: False beliefs not based on reality
These symptoms can be debilitating and scary for the people experiencing them. They can interfere with a persons ability to care for themselves and to relate to other people.
Psychotic symptoms in Parkinsons disease are associated with increased caregiver distress, risk of hospitalization and nursing home placement, and healthcare costs.
A study suggests the presence of hallucinations and delusions in people with Parkinsons disease is a predictor of mortality .
What Are The Symptoms Of Psychosis
Two of the most prominent symptoms are hallucinations and delusions.7 Hallucinations involve seeing, hearing, experiencing or sensing things that are not really there. Delusions are false beliefs that are not based in reality. In describing symptoms of Parkinsons disease psychosis, patients may use such common terms as: seeing things, paranoia, flashbacks, nightmares, false beliefs, or not being in touch with reality.8
What Causes Parkinson Disease
Parkinson disease arises from decreased dopamine production in the brain. The absence of dopamine makes it hard for the brain to coordinate muscle movements. Low dopamine also contributes to mood and cognitive problems later in the course of the disease. Experts dont know what triggers the development of Parkinson disease most of the time. Early onset Parkinson disease is often inherited and is the result of certain gene defects.
Do You Have Any Advice For The Family Friends And Carers Of People With Parkinsons Experiencing Hallucinations
Tell the patient that what they are experiencing is not real and do not pretend that you also experience the same thing. Be calm and friendly with the patient experiencing hallucinations can be quite stressful.
Need to know
Per Odin is a neurologist, professor and head of the neurology department at Lund University, Sweden. He also works at an outpatient clinic in Bremen, Germany. He has focused on Parkinsons disease, both clinically and in research, since 1987.
To find out more about Parkinsons disease and hallucinations, visit the EPDA website.
Read more:
Theres Something Unsettling About Someone Standing When You Feel Like They Should Be Sitting
Dad, you want to just sit here for a minute while I get us a drink?
On that, he plopped down and I positioned our bags so theyd be in his sight and reach.
A muffin would be good, too, he added.
OK. Ill see if they have muffins.
I turned and headed back to the concession stand. I couldnt have walked more than five or six steps before I glanced back over my shoulder at him. He was still sitting there. I dont know what I expected to see like he was going to erupt in flames the moment he was out of my sight or something.
I got in line, and as I waited my turn, I kept looking back.
Watch him like a hawk.
We hadnt come this far to have him fall down and break his wrist or have our bags stolen from under his nose.
Can Parkinsons Disease Make You Aggressive
Parkinsons disease Dementia or PD Dementia can make a patient very aggressive. Parkinsons Dementia Aggression germinating from Parkinsons disease Dementia can lead patients to behave erratically, experience sudden anger outbursts, feel constantly irritated, and always be in a state of restlessness. Outbursts are generally in the form of:
- Shouting
- Falling
Age And Duration Of Illness
Increased age has been associated with the presence of hallucinations. This might be explained by accerelated sensory loss or age related side effects of medication. One of the main confounders with age is duration of illness; when the non-independence of these variables was controlled, Fnelon et alfound that duration of illness was the crucial factor. Grahamet al identified two subgroups of patients with Parkinson’s disease experiencing hallucinosis: in those with disease duration of 5 years or less, visual hallucinations were associated with rapid progression of the motor but not the cognitive component of the disease. In the remainder with longer histories, visual hallucinations were associated with postural instability, global cognitive impairment, and the lack of depression. Goetz et al contrasted patients with Parkinson’s disease who experienced hallucinations within 3 months of levodopa therapy with those who experienced hallucinations after 1 year of treatment. Diagnoses in the early onset group more often changed to Lewy body or Alzheimer’s disease. Lewy bodies are present to a greater or lesser degree in all cases of Parkinson’s disease and are known to be associated with visual hallucinations.
Hallucinations According To The Duration Of The Disease
We found that the prevalence of hallucinations of all types and of visual hallucinations in the 3 months preceding inclusion in the study increased with the duration of the disease. Moreover, the duration of Parkinson’s disease was an independent predictor of visual hallucinations in the multivariate analysis. Other studies gave conflicting results on the relationship between hallucinations and disease duration. In a retrospective study of 100 patients, logistic regression analysis also showed an association between `psychosis’ and an increased duration of the disease . An association between the duration of the disease and the occurrence of hallucinations was also found by some investigators but not by others .
Table 1
I Had A Hallucination: What Next
Research has shown that for many people with PD who have them, hallucinations begin after a change in medication, more specifically, an increase in levodopa . Additional factors make a person more likely to experience hallucinations when medications are changed, such as other cognitive problems or memory issues, depression and sleep problems. Dementia|A term used to describe a group of brain disorders that cause a broad complex of symptoms such as disorientation, confusion, memory loss, impaired judgment and alterations in mood and personality.] also increases the risk of hallucinations and delusions when PD medications are changed. Dementia means cognitive changes whether in memory, judgment or attention that interfere with daily life.
One thing that does not affect the risk of hallucinations is your regular dose of levodopa. Rather, studies show that it is a change in dose an increase in a dose that has been stable that sets off hallucinations.
Tip: Experiencing a hallucination does not mean you are going crazy. Many people recognize that their hallucinations are not real. Do not react to these visions or sounds or engage them dismiss them. Bring up the topic with your doctor immediately.
